Abstract
This case study highlights the extracranial and intracranial manifestations of severe otomastoiditis. A 35-year-old man presented with numerous symptoms, including ear and neck pain, headache, temporary vision loss, fever, malaise, and nausea and vomiting. Imaging studies led to the diagnosis of coalescent mastoiditis with septic dural sinus thrombosis, venous hemorrhagic infarctions, brain abscesses, and subdural empyema.
CASE DISCUSSION
A 35-year-old white man who transferred from an outside hospital presented to Baylor University Medical Center at Dallas with a 4-day history of headache, predominantly involving the right side of his head, “head fullness,” neck pain, right-sided temporary vision loss, fever, right ear pain with purulent discharge, neck stiffness, malaise, nausea, vomiting, and anorexia. The patient had a prior history of ear infections, but his medical history was otherwise lacking. He smoked 10 cigarettes daily, drank 4 alcoholic beverages daily, and used marijuana each week.
On arrival, his blood pressure was 180/96 mm Hg, and his temperature was normal. Purulent drainage was noted from his right ear, and his neck was rigid. His white blood cell count was 17,000 cells/μL with 86% neutrophils. Serum sodium and potassium levels were 131 and 3.1 mEq/L, respectively.
The patient underwent both axial computed tomography (CT) (Figure 1) and magnetic resonance imaging (MRI) (Figure 2). These studies prompted the diagnosis of coalescent mastoiditis with septic dural sinus thrombosis, venous hemorrhagic infarctions, brain abscesses, and subdural empyema.
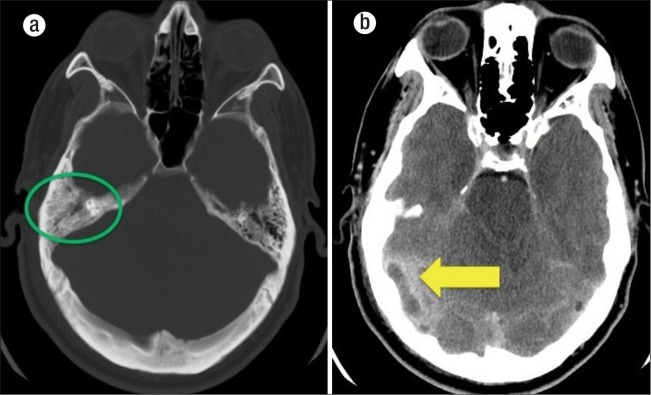
Figure 1.
CT scans of the patient showing (a) right mastoid air cell opacification (green circle) and (b) in the contrast-enhanced image, dural sinus thrombosis (yellow arrow) and surrounding inflammatory and edematous changes.
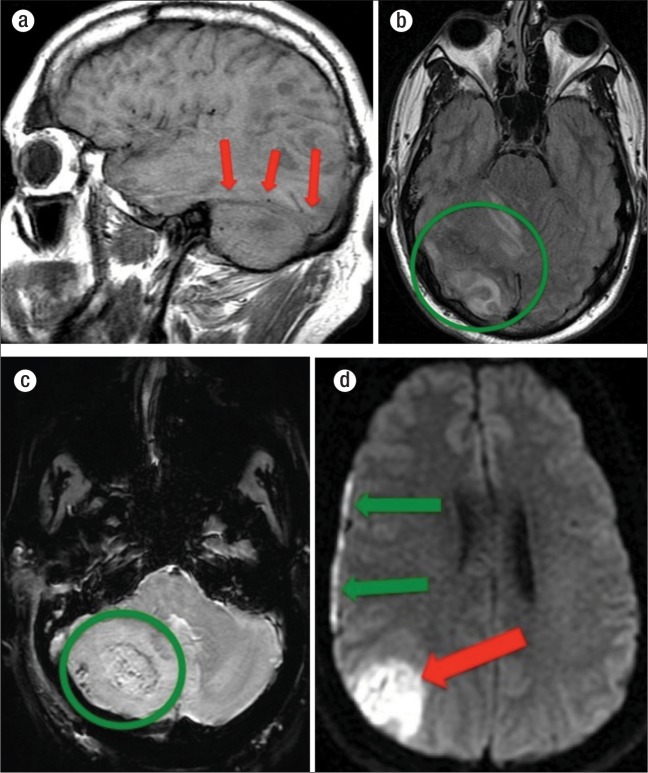
Figure 2.
MRI images of the patient. (a) An abnormally increased T1-weighted signal in the right transverse dural sinus (red arrows). (b) A T2 fluid-attenuated inversion recovery (FLAIR) image showing extensive inflammatory and edematous changes with potential ischemic injury in the right parieto-occipital lobe and superior cerebellar hemisphere (green circle). (c) A susceptibility weighted image (SWI) with an edematous mass in the right cerebellum. Blood products are shown as dark regions in the right cerebellar hemisphere (green circle). (d) A diffusion-weighted image (DWI) showing an infarction vs. abscess in the right parietal lobe (red arrow) as well as a thin right subdural empyema (green arrows). Gadolinium contrast was withheld due to acute renal impairment. Therefore, infarction versus abscesses could not be definitely characterized.
After undergoing surgery, during which a subdural empyema as well as adjacent parenchymal abscesses were identified and drained, the patient had an extended stay in the hospital on intravenous antibiotics and was subsequently transferred to a rehabilitation facility. He still has slight left-sided neurologic defects but is continuing to improve.
DISCUSSION
Radiographic findings of mastoiditis range from subtle changes of mastoid air cell opacification to the more profound changes of osseous destruction, subperiosteal abscess formation, coalescent mastoiditis, and, in some cases, venous infarctions as well as parenchymal abscesses (1–3). Middle ear infection may spread to the mastoid cells through the aditus ad antrum. Mastoid septae destruction with coalescent mastoiditis may develop with complicating intracranial and/or extracranial subperiosteal abscesses. In severe cases, there may be intracranial spread of disease. Intracranial extension has a propensity to form epi- and/or subdural empyemas.
The posterior fossa is the most common intracranial location to encounter the complications of mastoiditis, with the middle cranial fossa the next most common. Small veins that normally traverse the tympanic cavity to the overlying dura provide a conduit through which pathogens can readily spread into the subdural and subarachnoid spaces. Subdural empyemas (unlike epidural empyemas) are rarely asymptomatic and usually manifest as meningismus, as well as seizures with possible neurologic deficits. Emergent surgical decompression is often required.
In about half the cases in which epidural abscesses are seen, dural venous thrombophlebitis can occur. Symptoms may include signs of sepsis, hydrocephalus, and intracranial hypertension. Dural venous thrombophlebitis can lead to such complications as seizures, hydrocephalus, cerebral edema, and venous infarctions. Venous infarcts also have a high likelihood of hemorrhage secondary to concomitant venous hypertension.
This case shows a number of both extracranial and intracranial manifestations of severe otomastoiditis. The extracranial findings include opacification of the mastoid air cells with resultant suppuration. Acidification of the local environment under pressure causes osseous decalcification, ischemia, and osteoclastic dissolution of the pneumatic cell walls. These changes are best seen on noncontrast CT. Contrast enhancement can also help characterize subdural and epidural as well as parenchymal abscesses. Intracranial extension with complicating dural venous thrombosis, venous infarctions, subdural empyema, and parenchymal hemorrhages can be identified on CT; however, they are often better seen on contrast-enhanced MRI.
References
- 1.Vazquez E, Castellote A, Piqueras J, Mauleon S, Creixell S, Pumarola F, Figueras C, Carreño JC, Lucaya J. Imaging of complications of acute mastoiditis in children. Radiographics. 2003;23(2):359–372. doi: 10.1148/rg.232025076. [DOI] [PubMed] [Google Scholar]
- 2.Leach JL, Fortuna RB, Jones BV, Gaskill-Shipley MF. Imaging of cerebral venous thrombosis: current techniques, spectrum of findings, and diagnostic pitfalls. Radiographics. 2006;26(Suppl 1):S19–S41. doi: 10.1148/rg.26si055174. [DOI] [PubMed] [Google Scholar]
- 3.Linn J, Ertl-Wagner B, Seelos KC, Strupp M, Reiser M, Brückmann H, Brüning R. Diagnostic value of multidetector-row CT angiography in the evaluation of thrombosis of the cerebral venous sinuses. AJNR Am J Neuroradiol. 2007;28(5):946–952. [PMC free article] [PubMed] [Google Scholar]