Abstract
We present a case of a fatal toxic leukoencephalopathy following ingestion of a new psychoactive designer drug known as 2C-E or “Europa.” Recreational drugs, particularly hallucinogenic substances, appear to be growing in popularity, with increasing amounts of information available via the Internet to entice potential users. In addition, some newer “designer” psychoactive substances are available for purchase online without adverse legal consequences, therefore adding to their popularity. We describe magnetic resonance imaging (MRI) findings to include selective diffuse toxic injury of the cerebral white matter with sparing of the cortex and most of the deep gray nuclei. To our knowledge, this is the first reported description of cerebral findings on MRI that are likely related to a lethal ingestion of 2C-E.
Leukoencephalopathy is defined by a wide spectrum of neurologic deficits, including alteration of mental status, caused by pathologic changes in the cerebral white matter. After suspecting leukoencephalopathy based on history and clinical presentation, the diagnosis is typically confirmed with a magnetic resonance imaging (MRI) examination of the brain. Leukoencephalopathy can be caused by a variety of toxic insults; however, there are some widely recognized and well-defined leukoencephalopathic entities, such as those resulting from carbon monoxide inhalation and intoxication due to heroin or cocaine (1). Posterior reversible encephalopathy syndrome (PRES), a variant leukoencephalopathy, may occur as a complication of profound hypertension, toxicity due to medications such as tacrolimus or cyclosporine, and eclampsia, although there are many other etiologies. The clinical outcome varies from complete reversibility to death and depends on various factors including the type and amount of toxic exposure. The duration of exposure and the presence of underlying pathology or risk factors are also variables that alter prognosis.
2C-E (“Europa”) is a new recreational psychoactive drug related to MDMA (“ecstasy”) that has grown recently in popularity as an alternative to other psychoactive drugs due in part to its ease of legal acquisition via the Internet. Currently, there are social media websites devoted to creating and fostering experimentation with new ways of ingesting 2C-E and describing the resulting “trips” for prospective users (2).
In this case report, we discuss the MRI findings of metabolic toxic encephalopathy as a likely result of ingestion of an unknown amount of 2C-E in addition to the simultaneous ingestion of benzodiazepines and tetrahydrocannabinol (cannabis), for which there were positive toxicology test results. MRI provides insight into the possible toxic neurological effects of 2C-E.
CASE DESCRIPTION
A 26-year-old man with a history of polysubstance abuse, anxiety, and depression was brought to the emergency department after being found unconscious adjacent to an empty bottle of zolpidem. Witnesses indicated that the patient had been in his usual state of health 12 hours prior. Naloxone was administered without improvement. On presentation, the patient was unresponsive, with frothy sputum at the mouth and without focal neurological deficits. Brain stem reflexes remained intact. An initial brain computed tomography scan and lumbar puncture results were unremarkable. A urine toxicology screen was positive for benzodiazepines and tetrahydrocannabinol, but was otherwise negative. Serum testing was negative for alcohol, salicylates, and acetaminophen. Blood cultures were obtained, and the patient was placed on broad-spectrum antibiotics. A friend disclosed that the patient recently received 2C-E from an Internet website and had likely consumed it. Although testing for 2C-E is limited, a urine sample was positive for this substance.
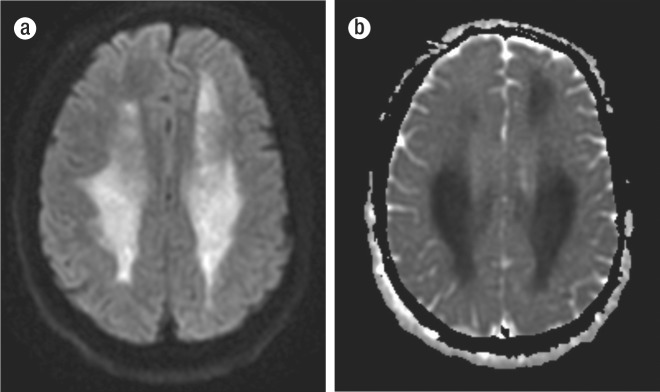
MRI of the brain showed large symmetric areas of restricted diffusion within the subcortical white matter, genu, splenium of the corpus callosum, and minimally within the globus pallidi (Figures 1 and 2). The patient's neurological status did not improve. Life support was curtailed at the request of the family, and the patient died.
Figure 1.
(a) Single axial image from a diffusion-weighted sequence MRI at the level of the centrum semiovale demonstrates extensive restricted diffusion throughout the subcortical white matter of the frontal, temporal, and parietal lobes. Notice the complete sparing of the cortex. There was minimal restricted diffusion of the bilateral globus pallidi, with sparing of the other deep gray nuclei. (b) Associated apparent diffusion coefficient (ADC) map at the same level demonstrates signal dropout, indicating true restricted diffusion.
Figure 2.
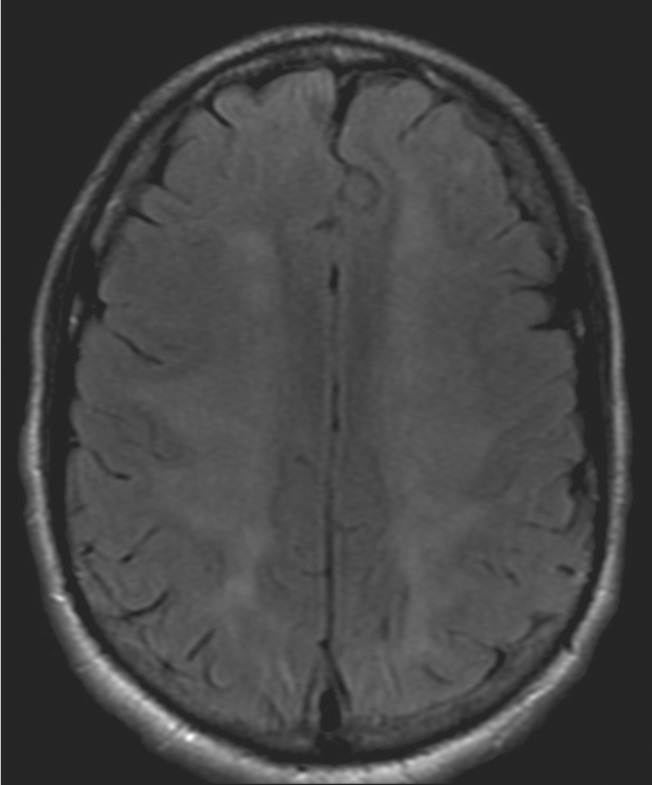
Fluid-attenuated inversion recovery (FLAIR) sequences demonstrate mild signal hyperintensity in a pattern similar to that of the restricted diffusion. While this is nonspecific, findings are most consistent with preferential ischemia of the subcortical white matter, with sparing of the cortex and most of the deep gray nuclei.
DISCUSSION
2C-E or “Europa” is known chemically as 2,5-dimethoxy-4-ethylphenethylamine. Like its analogs, 2C-E causes auditory, visual, and temporal distortions, which are often user dependent and related to both mood and location. Use is via inhalation or ingestion concomitantly with other substances. It is not yet considered explicitly illegal in the United States, as it is in Europe (3); therefore, it is available for order on the Internet, where it is listed as a “research chemical.” However, it may be considered an analog to other psychoactive amines that are scheduled by the Drug Enforcement Agency (DEA), and as such prosecution may be possible for sale or possession with intent for consumption under the Federal Analog Act. Due to the increasing availability of these substances on the Internet, the DEA launched Operation Web Tryp in 2004, which targets individuals and companies illegally selling phenethylamines (3). Nevertheless, since it is not scheduled, websites often sell 2C-E through a loophole by labeling it “not for human consumption.”
Deaths related to 2C-E overdose have been reported, with an unknown additional number of hospitalizations (4). With the patient's history of polysubstance abuse and his positive urine toxicology screen for benzodiazepines and tetrahydrocannabinol, it cannot be concluded that his metabolic injury was the consequence of 2C-E alone. In light of other reported 2C-E deaths, however, it is likely that this agent contributed to the toxic brain injury with selective destruction of white matter.
Like many drugs similar to 2C-E, overdose can cause a selective toxic leukoencephalopathy, as was evidenced on MRI in this case. Toxic leukoencephalopathy may be caused by exposure to a wide variety of agents, including cranial irradiation, therapeutic agents, drug abuse, and environmental toxins. The use of MRI has led to a greater appreciation of the damage that leukotoxic agents can inflict on the brain's white matter (5). As MRI continues to become more sophisticated, newer possibilities are sure to offer more insight into this type of injury as well as the degree of overall compromised brain function. Diffusion tensor MRI tractography may offer such information in the foreseeable future. Kim et al have recently described the use of diffusion tractography in the successful evaluation of tacrolimus-induced encephalopathy. As this methodology becomes more available, it may have a role in the treatment and prognosis of white matter encephalopathies (6).
While MRI findings are consistent in this case with bilateral diffuse toxic leukoencephalopathy, a hypoxic mechanism was considered given the patient's history of being unconscious for an unknown period of time. Fortunately, there are methods of differentiating the etiologies of brain insults, which include assessing the particular distribution of injury. For example, the brain regions thought to be most sensitive to hypoxic/ischemic injury are the CA1 and CA3 regions of the hippocampus, cortical layers 3 and 5, medium spiny neurons of the striatum, and the Purkinje layer of the cerebellum (7). Upon review of the imaging for this patient, there was minimal restricted diffusion in the bilateral globus pallidi, which can be seen in hypoxia. However, there was sparing of the striatum, cortices, and hippocampus, which is consistent with a toxic metabolic encephalopathy.
Other substances are also capable of causing toxic leukoencephalopathy, including cocaine and heroin. With the patient's history of polysubstance abuse, these drugs were an etiologic consideration, although they were reliably excluded based on the toxicology screening. The patient's MRI findings had many features similar to those of cocaine overdose, including injury of the centrum ovale. In addition to causing toxic injury to cerebral white matter, cocaine typically injures portions of the basal ganglia, particularly the globus pallidi, which were minimally affected in this case (8). The use of heroin in this case was not considered a contributor, since the toxicology screen was negative and the imaging findings of heroin differ from those in this case. With heroin overdose, destruction of cerebellar white matter is frequently seen, along with involvement of the corticospinal tract and sparing of the dentate nuclei (9).
The exact pathophysiologic mechanism for toxic leukoencephalopathy is unknown; however, it is likely related to the pharmacodynamics of the inciting substance. In the case of heroin overdose, it has been suggested that heroin or its metabolite may be deposited in lipid-rich myelin, where it resides and is slowly released, resulting in ongoing tissue destruction and symptom progression (10). Perhaps a similar mechanism occurs with 2C-E.
With the continuing use by the public of recreational drugs, the number of potential leukotoxins is likely to grow (9). This case represents the first known case of 2C-E overdose at our institution and perhaps the first MRI description of its lethal consequences. Although the exact cause and effect of 2C-E on the brain remains less than certain in the setting of presumed polypharmacy abuse in this patient's case, we feel there is value in alerting the medical community as a whole as to the potential lethality of this recreational agent. Given the relatively recent introduction of this designer drug to the United States, future cases are likely to follow. Larger case series will be needed to best determine if 2C-E is indeed a leukotoxin and to further describe its potential effects on the brain and other organ systems.
References
- 1.Tormoehlen LM. Toxic leukoencephalopathies. Neurol Clin. 2011;29(3):591–605. doi: 10.1016/j.ncl.2011.05.005. [DOI] [PubMed] [Google Scholar]
- 2.Boyer EW, Shannon M, Hibberd PL. The Internet and psychoactive substance use among innovative drug users. Pediatrics. 2005;115(2):302–305. doi: 10.1542/peds.2004-1199. [DOI] [PubMed] [Google Scholar]
- 3.Sanders B, Lankenau SE, Bloom JJ, Hathazi D. “Research chemicals”: tryptamine and phenethylamine use among high-risk youth. Subst Use Misuse. 2008;43(3-4):389–402. doi: 10.1080/00952990701202970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pham S. Man arrested in mass drug overdose that killed 1 teen and left 10 people hospitalized. ABC News. Available at http://abcnews.go.com/US/man-arrested-minnesota-deadly-mass-drug-overdose/story?id=13166375&singlePage=true.
- 5.Filley CM, Kleinschmidt-DeMasters BK. Toxic leukoencephalopathy. N Engl J Med. 2001;345(6):425–432. doi: 10.1056/NEJM200108093450606. [DOI] [PubMed] [Google Scholar]
- 6.Kim MU, Kim SY, Son SM, Park YH. A case of tacrolimus-induced encephalopathy after kidney transplantation. Korean J Pediatr. 2011;54(1):40–44. doi: 10.3345/kjp.2011.54.1.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bianchi MT, Sims JR. Restricted diffusion in the splenium of the corpus callosum after cardiac arrest. Open Neuroimag J. 2008;2:1–4. doi: 10.2174/1874440000802010001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sharma P, Eesa M, Scott JN. Toxic and acquired metabolic encephalopathies: MRI appearance. AJR Am J Roentgenol. 2009;193(3):879–886. doi: 10.2214/AJR.08.2257. [DOI] [PubMed] [Google Scholar]
- 9.Offiah C, Hall E. Heroin-induced leukoencephalopathy: characterization using MRI, diffusion-weighted imaging, and MR spectroscopy. Clin Radiol. 2008;63(2):146–152. doi: 10.1016/j.crad.2007.07.021. [DOI] [PubMed] [Google Scholar]
- 10.Ryan A, Molloy FM, Farrell MA, Hutchinson M. Fatal toxic leukoencephalopathy: clinical, radiological, and necropsy findings in two patients. J Neurol Neurosurg. Psychiatry. 2005;76(7):1014–1016. doi: 10.1136/jnnp.2004.047134. [DOI] [PMC free article] [PubMed] [Google Scholar]