Abstract
The authors present the case of a 45-year-old lady who presented to the emergency department with sudden onset of right hemiparesis, numbness, dysarthria, dysmetria, left upper motor neuron facial palsy and left extensor plantar. Initial laboratory investigations, ECG and MR angiography were normal. MRI brain revealed multiple ischaemic strokes in middle cerebral artery and posterior cerebral artery territory. Transthoracic echocardiography revealed large mobile mass in left atrium which was resected and the patient remained well postoperatively. Anticoagulants do not play any protective role making resection as the only effective treatment.
Background
At least 20% of all ischaemic strokes are cardioembolic. Cardiac myxoma is a source of emboli to the central nervous system and elsewhere in the vascular tree.1 It is a well-described cause of stroke that usually occurs in young people and is a potential treatable condition.2 Therefore, it is important for the clinicians to detect the myxoma and prevent its complications like syncope, recurrent strokes or sudden cardiac death. In this case, a middle aged lady with no known co-morbids presented with acute stroke and her investigation revealed atrial myxoma on transesophageal echocardiography which was successfully resected.
Case presentation
A 45-year-old female with no known comorbids, was brought to our emergency department with sudden onset of left hemiparesis and numbness for 1 day after an episode of nausea and vomiting. Neurological examination revealed that she was drowsy but arousable and was following two steps commands. Neck was supple and speech was dysarthric. She had left upper motor neuron facial palsy and rest of the cranial nerves was normal. Motor examination revealed left-sided hemiparesis with a power of 4/5 in left upper and lower limbs with left extensor plantar. Reflexes were +1 in all over the limbs. Cerebellar examination revealed bilateral finger nose dysmetria. Sensory examination were normal. On cardiovascular examination, S1 and S2 were audible in all four areas with no added sounds and pulse of 90 beats per min. Rest of the systemic examination was unremarkable.
Investigations
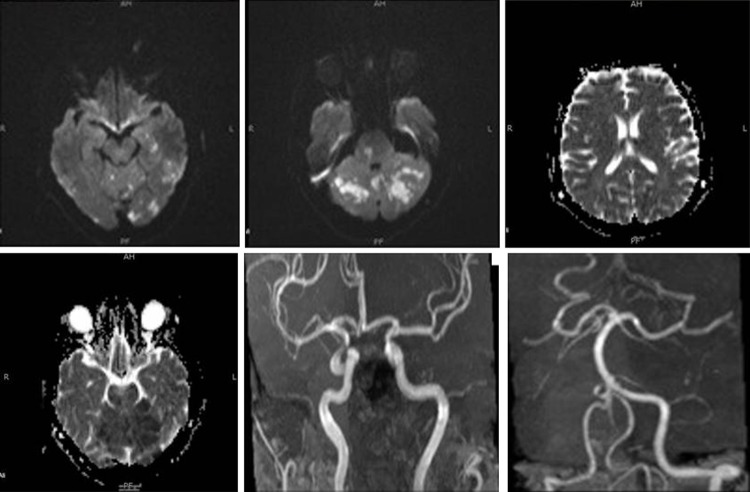
Her initial laboratory investigations including complete blood count, electrolytes, renal and liver functions were normal. ECG revealed normal sinus rhythm. MRI brain with time of flight MR angiography (MRA), was done which showed diffusion restricted infarctions in bilateral cerebellar hemisphere, vermis, bilateral pons, left-sided occipital, parietal and basal ganglia. These areas appeared dark on apparent diffusion coefficient mapping, thus confirming acute stroke in the territory of bilateral middle cerebral artery and posterior cerebral artery (figure 1). The results of MRA were unremarkable. Her carotid doppler ultrasound and lipid profile were unremarkable. Transthoracic echocardiography (TTE) was thereby done to find out a cardiac source of embolism which revealed large (4.5×3×2.5 cm) mobile echogenic density noted in the left atrium attached to the interatrial septum and was consistent with an atrial myxoma of size. She was diagnosed as a case of cardioembolic infarction secondary to atrial myxoma.
Figure 1.
(A, B) Multiple areas of diffusion restricted in middle cerebral artery and posterior cerebral artery territories. (C, D) Subsequent areas that are dark on apparent diffusion coefficient mapping. (E) Normal anterior and posterior circulation vessels.
Differential diagnosis
-
▶
Acute cardioembolic stroke
-
▶
Acute thrombotic stroke
-
▶
Cerebral venous thrombosis
-
▶
Intracerebral haemorrhage
-
▶
Subarachnoid haemorrhage
-
▶
Cerebral abscess
-
▶
Chronic central nervous system infection
Treatment
The patient was managed on the line of acute stroke care. She was admitted to the highly specialised stroke unit and the supportive management including intravenous fluids, oxygen, deep vein thrombosis stockings, antacids, antiemetics etc along with antiplatelets and statins were given. Investigation of stroke revealed atrial myxoma. Cardiothoracic team was involved and they planned to resect the lesion. She underwent the surgery after 7 days of admission and was well postoperatively. Later histopathology confirmed the diagnosis.
Outcome and follow-up
She remained in the hospital 4 days after the surgery and was discharged without any poststroke complication. Rehabilitation was started including physiotherapy, speech therapy and occupational therapy for her residual deficits. Postoperatively, she remained well without any surgical complication.
Discussion
Atrial myxoma is a benign neoplasm of mesenchymal origin. Histologically, these tumours are composed of scattered cells within a mucopolysaccharide stroma. It is the most frequent (70%) primary cardiac tumour in adults3 and its incidence is reported to be between 0.0017% and 0.19%.4 About 75%–90% of the cardiac myxomas occurs in the left atrium, and is found more commonly between 3rd to 6th decades of life.5 Tumours vary widely in size, ranging from 1 to 15 cm in diameter, and weigh between 15 and 180 g.6 About 35% of myxomas are friable or villous, and these tend to present with emboli. Larger tumours are more likely to have a smooth surface and to be associated with cardiovascular symptoms. In at least half of the cases, cerebral arteries are affected, leading to embolic ischemic stroke.6 The male to female ratio is 1:2 with a slight female preponderance. Delay in the diagnosis after presentation is usually variable and may range from 1 to 126 months.7
Most cases (90%) of atrial myxoma are sporadic with no known cause.8 In remaining (10%), a familial pattern occurs having an autosomal dominant pattern known as Carney complex which is characterised by multiple tumors, including atrial and extracardiac myxomas, cutaneous spotty pigmentation, non-myxomatous extracardiac tumours, schwannomas and various endocrine tumours, through a causative mutation of the PRKAR1α gene located on the long arm of chromosome 17 (17q22-24 region).7 9
Patients with cardiac myxoma presents characteristically with a triad of obstructive symptoms (30%), constitutional symptoms (60%) and embolic phenomenon (30–40%).8 Obstructive symptoms include atrioventricular valve obstruction, dyspnoea, orthopnea, paraoxysmal nocturnal dyspnoea, oedema, dizziness, syncope, atrial fibrillation or sudden cardiac death. Embolic phenomenon such as systemic embolisation presents with stroke, pulmonary embolism or paradoxical embolism while constitutional symptoms presents as fever, weight loss, arthralgia or Raynaud’s phenomena.2 10
Neurological manifestations of atrial myxoma vary widely ranging from embolic,6 haemorrhagic or recurrent infarctions11 and progressive multi-infarct dementia12 to massive embolic stroke causing sudden death.13 Since tumour fragments may embolise, early anticoagulation may not be protective in reducing disability and mortality.1
Laboratory investigations may reveal anaemia, polycythaemia, thrombocytopenia with raise erythrocyte sedimentation rate, C reactive protein and imunoglobulins.14 Echocardiography is widely available and provides a simple, non-invasive technique for the initial evaluation. Echocardiography images both the myocardium and the cardiac chambers and can usually identify the presence of a mass and its mobility. Transesophageal echocardiography which has been reported as having 100% sensitivity for cardiac myxoma,7 15 is preferred over TTE. Cardiac MRI can help out in demarcating tumour size, attachment and its mobility7 16 and this information may be further used during surgical resection. Surgery should not be delayed even in asymptomatic cases which are revealed incidentally because of the risk of having further embolisation. Neurological sequelae after resection are usually rare but possiblity exist.7 Positron emission tomography scan has been useful in identifying cardiac involvement in patients with metastatic tumours17 and atrial myxoma.18
Once a presumptive diagnosis of myxoma has been made on imaging studies, prompt resection is required because of the risk of embolisation or cardiovascular complications including sudden death.19 The results of surgical resection are generally very good, with most series reporting an operative death rate of <5%.20
There is a recurrence rate of 1%–3% which is associated with sporadic cases of atrial myxoma, often because of inadequate resection.8 These patients require annual review for a period of 3–4 years with echocardiography, when the risk of recurrence is greatest.21 For Carney complex, which has a recurrence rate of up to 25%, lifetime annual review with familial screening is recommended.22
Learning points.
-
▶
Cardiac echocardiography should always be considered in young patients presenting with embolic ischaemic stroke with usually normal MRA of neck vessels.
-
▶
Patients with cardiac myxoma can present with symptoms of atrioventricular valvular dysfunction, stroke and neurological disorder or with any other constitutional symptoms.
-
▶
Transesophageal echocardiography should be preffered over transthoracic echocardiography.
-
▶
Once the diagnosis is made, surgery should not be delayed.
Footnotes
Competing interests: None.
Patient consent: Obtained.
References
- 1.Paciaroni M, Agnelli G, Micheli S, et al. Efficacy and safety of anticoagulant treatment in acute cardioembolic stroke: a meta-analysis of randomized controlled trials. Stroke 2007;38:423–30. [DOI] [PubMed] [Google Scholar]
- 2.Ekinci EI, Donnan GA. Neurological manifestations of cardiac myxoma: a review of the literature and report of cases. Intern Med J 2004;34:243–9. [DOI] [PubMed] [Google Scholar]
- 3.Vermeulen T, Conraads VM, Vrints C, et al. Recurrent left ventricular myxoma presenting as cerebrovascular accidents in a teenage girl. Acta Cardiol 2009;64:811–4. [DOI] [PubMed] [Google Scholar]
- 4.Uner A, Dogan M, Sal E, et al. Stroke and recurrent peripheral embolism in left atrial myxoma. Acta Cardiol 2010;65:101–3. [DOI] [PubMed] [Google Scholar]
- 5.Reynen K. Cardiac myxomas. N Engl J Med 1995;333:1610–7. [DOI] [PubMed] [Google Scholar]
- 6.Pinede L, Duhaut P, Loire R. Clinical presentation of left atrial cardiac myxoma. A series of 112 consecutive cases. Medicine (Baltimore) 2001;80:159–72. [DOI] [PubMed] [Google Scholar]
- 7.O’Rourke F, Dean N, Mouradian MS, et al. Atrial myxoma as a cause of stroke: case report and discussion. CMAJ 2003;169:1049–51. [PMC free article] [PubMed] [Google Scholar]
- 8.McCarthy PM, Piehler JM, Schaff HV, et al. The significance of multiple, recurrent, and “complex” cardiac myxomas. J Thorac Cardiovasc Surg 1986;91:389–96. [PubMed] [Google Scholar]
- 9.Kirschner LS, Carney JA, Pack SD, et al. Mutations of the gene encoding the protein kinase A type I-alpha regulatory subunit in patients with the Carney complex. Nat Genet 2000;26:89–92. [DOI] [PubMed] [Google Scholar]
- 10.Knepper LE, Biller J, Adams HP, Jr, et al. Neurologic manifestations of atrial myxoma. A 12-year experience and review. Stroke 1988;19:1435–40. [DOI] [PubMed] [Google Scholar]
- 11.Kassab R, Wehbe L, Badaoui G, et al. [Recurrent cerebrovascular accident: unusual and isolated manifestation of myxoma of the left atrium]. J Med Liban 1999;47:246–50. [PubMed] [Google Scholar]
- 12.Hutton JT. Atrial myxoma as a cause of progressive dementia. Arch Neurol 1981;38:533. [DOI] [PubMed] [Google Scholar]
- 13.Bienfait HP, Moll LC. Fatal cerebral embolism in a young patient with an occult left atrial myxoma. Clin Neurol Neurosurg 2001;103:37–8. [DOI] [PubMed] [Google Scholar]
- 14.Mendoza CE, Rosado MF, Bernal L. The role of interleukin-6 in cases of cardiac myxoma. Clinical features, immunologic abnormalities, and a possible role in recurrence. Tex Heart Inst J 2001;28:3–7. [PMC free article] [PubMed] [Google Scholar]
- 15.Engberding R, Daniel WG, Erbel R, et al. Diagnosis of heart tumours by transoesophageal echocardiography: a multicentre study in 154 patients. European Cooperative Study Group. Eur Heart J 1993;14:1223–8. [DOI] [PubMed] [Google Scholar]
- 16.Damásio H, Seabra-Gomes R, da Silva JP, et al. Multiple cerebral aneurysms and cardiac myxoma. Arch Neurol 1975;32:269–70. [DOI] [PubMed] [Google Scholar]
- 17.Gates GF, Aronsky A, Ozgur H. Intracardiac extension of lung cancer demonstrated on PET scanning. Clin Nucl Med 2006;31:68–70. [DOI] [PubMed] [Google Scholar]
- 18.Agostini D, Babatasi G, Galateau F, et al. Detection of cardiac myxoma by F-18 FDG PET. Clin Nucl Med 1999;24:159–60. [DOI] [PubMed] [Google Scholar]
- 19.Keeling IM, Oberwalder P, Anelli-Monti M, et al. Cardiac myxomas: 24 years of experience in 49 patients. Eur J Cardiothorac Surg 2002;22:971–7. [DOI] [PubMed] [Google Scholar]
- 20.Bakaeen FG, Reardon MJ, Coselli JS, et al. Surgical outcome in 85 patients with primary cardiac tumors. Am J Surg 2003;186:641–7; discussion 647. [DOI] [PubMed] [Google Scholar]
- 21.Semb BK. Surgical considerations in the treatment of cardiac myxoma. J Thorac Cardiovasc Surg 1984;87:251–9. [PubMed] [Google Scholar]
- 22.Basson CT, Aretz HT. Case records of the Massachusetts General Hospital. Weekly clinicopathological exercises. Case 11-2002. A 27-year-old woman with two intracardiac masses and a history of endocrinopathy. N Engl J Med 2002;346:1152–8. [DOI] [PubMed] [Google Scholar]