Abstract
The past characterisations of breastfeeding as being only at the breast of the mother may no longer be applicable in the United States as mothers now frequently express their milk. We conducted a retrospective cohort study with women who visited the Cincinnati Children's Breastfeeding Medicine Clinic to understand breast milk feeding behaviours of healthy mothers and infants, which included questions specifically about breast milk expression. All 40 mothers in the cohort expressed their milk and all 40 infants were fed expressed milk. One infant was fed another mother's milk for 30 days. Two‐thirds (13/40) of infants received their mother's expressed milk at least a week after it was first expressed and 25% (10/40) of infants continued to be fed expressed breast milk after mothers had stopped expressing milk. There were 14 sequences of breast milk production by the mothers and 16 sequences of consumption by the infants. Early in the post‐partum period, mothers started expressing milk even though their infants were consuming all of the breast milk that they needed at the breast. As a result of breast milk expression by all mothers in this cohort, we observed highly variable patterns of maternal breast milk production and infant breast milk consumption, which were not necessarily synchronous within a dyad. It is now time to develop appropriate ways to characterise the production and consumption of breast milk more accurately and investigate whether these behaviours have consequences for the health of mothers and infants.
Keywords: human milk, breastfeeding, breast milk pumping, breast milk expression
Background
The definitions of ‘breastfeeding’ traditionally characterise a mother as breastfeeding and an infant as being breastfed for as long as the infant is fed at the breast of the mother. Labbok and Krasovec recommended that breastfeeding for both mothers and infants be defined as ‘full, partial, or token’, as determined by the estimated breast milk intake of the infant (Labbok & Krasovec 1990). Although introduced two decades ago, this nomenclature is still widely accepted today. Breastfeeding for both the mother and the child traditionally has been understood to be a coordinated, synchronous event.
While there have been calls to update and further refine the definitions of breastfeeding, these primarily have been in the context of breastfeeding exclusivity and of breast milk content (World Health Organization 2008; Binns et al. 2009; Thulier 2010; United States Breastfeeding Committee 2010; Hector 2011). Now that mothers in the United States frequently express their milk, however, this adds to the complexity of collecting infant feeding data, and method of feeding (at the breast vs. expressed milk) needs to be considered as well (Geraghty & Rasmussen 2010; Leonard et al. 2011; Rasmussen & Geraghty 2011). Breast pumps, equipment and milk storage containers can be rented or purchased at many local retail outlets without a health care provider's prescription or instruction. A post‐partum woman with a double‐sided, electric pump can easily and painlessly extract milk from her breasts in about 15 min (Becker et al. 2008). A mother may then transport and store her milk in a variety of places to be fed to the infant at a later time (Geraghty 2011). In the Infant Feeding Practices Study II, the most comprehensive data collection available to date on milk expression by American mothers, 85% of 1564 breastfeeding mothers of healthy, singleton infants aged 1.5–4.5 months expressed their milk (Labiner‐Wolfe et al. 2008) and 6% of the mothers expressed milk only and never fed their infants at the breast at all (Shealy et al. 2008). As ‘breastfeeding’ is no longer only at the breast feeding, the increased physical challenges and amplified complexity of emotions which pumping contributes to women's infant feeding experiences are now being recognised (Kelleher 2006; Boswell‐Penc & Boyer 2007; Johnson et al. 2009; Flaherman et al. 2012).
In this research study, our goals were to examine the methods of breast milk production by the mother and consumption of breast milk by the infant, either directly at the breast or by incorporating expressed milk feeding. We wanted to ascertain the number of ways mothers and infants participated in these methods of breast milk feeding and determine if mothers produced and infants consumed breast milk concomitantly. The seminal studies that established the benefits of breastfeeding compared outcomes of infants directly feeding at the mothers' breast vs. the feeding of a breast milk substitute from a bottle or cup (Leon‐Cava et al. 2002; Ip et al. 2009). With breast milk expression, breast milk is now in a bottle or cup. The consequences of this change in behaviour for the health of mothers and their infants are unknown at present. Before these health outcomes are determined, however, the scientific community needs to develop more accurate ways to describe and measure these behaviours.
Key messages
-
•
Past characterisations of breastfeeding as being only at the breast of the mother may no longer be applicable in the United States as mothers now frequently express their milk.
-
•
As a result of breast milk expression, we observed highly variable patterns of maternal breast milk production and infant breast milk consumption, which were not necessarily synchronous within a dyad.
-
•
Accurately characterising the production and consumption of breast milk to include expressed milk feeding is necessary to determine whether these behaviours have consequences for the health of mothers and infants.
Methods
This retrospective cohort study was conducted with women who visited the Cincinnati Children's Breastfeeding Medicine Clinic. Our clinic is an outpatient practice in which three lactation‐trained physicians and one lactation‐trained nurse see mother–infant dyads referred by primary‐care physicians, maternity hospitals, home health care agencies and community lactation consultants. Challenges for the mother usually consist of latch difficulties, low milk supply, breast infections and latching multiple gestation infants. Problems for the infant usually are related to latch difficulties, ankyloglossia, failure to gain weight, transition to the breast associated with prematurity or prolonged illness, congenital abnormalities and infants of a multiple gestation. Unless there is an ongoing complication, each dyad is typically seen once, with referral back to the primary‐care physician.
Dyads selected to be in this cohort were seen in the Breastfeeding Medicine Clinic from October to December 2008, approximately 20–23 months before the start of the study. We chose this period because it is a similar time interval used by the widely accepted breastfeeding data collection method of the National Immunization Survey [Centers for Disease Control and Prevention (CDC) 2011], and recall of breastfeeding initiation and duration is more accurate during this early post‐partum time period (Li et al. 2010). Questions for the study were based on the clinical history format used in our breastfeeding medicine clinic. Eligible dyads included those where the mother was over 18 years old, English‐speaking, and both mother and infant were generally healthy. Dyads were excluded if the pregnancy was shorter than 37 weeks, was a multiple gestation or there were any medical problems for the mother or baby precluding feeding directly at the breast.
There were a total of 80 pairs of mother–infant clinical charts from the specified period. Fifty‐nine of these dyads met the eligibility criteria. The mother's address, maternal birth date, race, marital status and insurance status were extracted from the registration data file. The research assistant sent an introductory letter explaining the study, a one‐page survey and a return‐mail envelope. If the survey was not returned after 4 weeks, a second letter was sent in an attempt to contact the non‐respondents. Mothers who returned the completed survey were sent a $20 gift card to a local retail store as compensation for their time.
Survey questions
The one‐page survey questions sent to the mothers and used for this analysis are listed in Table 1 (Geraghty & Rasmussen 2010). If a mother answered to the timing of a question in weeks or months, her answer was converted to days.
Table 1.
Survey questions utilised for this study
| Questions pertaining to start of breast milk production and consumption | Questions pertaining to end of breast milk production and consumption |
|---|---|
| How many days old was your child when he/she was first fed breast milk? | How many days old was your child when he/she completely stopped breastfeeding or being fed breast milk? |
| How many days old was your child when you first fed him/her directly at the breast? | How many days old was your child when you stopped feeding him/her directly at the breast? |
| How many days old was your child when he/she was first fed another mother's breast milk? | How many days old was your child when he/she was no longer fed another mother's breast milk? |
| On what post‐partum day did you first begin to hand‐express or pump your milk? | On what post‐partum day did you stop hand‐expressing or pumping your milk? |
| How many days old was your child when he/she was first fed any of your hand‐expressed or pumped breast milk? | How many days old was your child when he/she was no longer fed any of your hand‐expressed or pumped breast milk? |
Statistical analysis
We used clinic registration data to determine study participants' mean age, race (white vs. non‐white), marital status (married vs. not married) and insurance (private vs. public/self‐pay).
We determined the days at which the mothers and infants started and stopped producing or consuming breast milk and the number of days the infants were only fed at the breast vs. at least some expressed milk. We also determined the number of days an infant was fed another mother's milk. We calculated the percentage of infants who were concurrently fed both at the breast and expressed milk feedings at any point during the breast milk consumption period. We calculated the number of days after mothers first expressed milk until the infants received expressed milk. We also determined the number of days that a child was fed breast milk if the mother previously had stopped lactating.
We examined the method of breast milk production by each mother to determine if it was by directly feeding the infant only at the breast or by also expressing milk. We also determined if the method that the infant was fed breast milk was either only at the breast or expressed milk fed.
We chose to examine the methods of breast milk feeding production and consumption in closer detail at post‐partum days 2, 90 and 180 because these are benchmarks used by the Centers for Disease Control and Prevention (Centers for Disease Control and Prevention 2011); day 14 as the time when mothers may have been more settled in their breast milk feeding routine; and day 42 (6 weeks) when maternity leave typically concludes in the United States. We determined the frequencies of mothers' breast milk production methods and infants' breast milk consumption methods at each time point. At each time point, we compared the proportion of mothers who reported producing milk by feeding the baby only at the breast to the proportion of infants who consumed milk only at the breast using a McNemar's test.
All data were analysed with SAS®, version 9.2 (SAS Institute, Cary, NC, USA). Differences were determined to be significant at P < 0.05. This study was approved by the Cincinnati Children's Hospital Medical Center's Institutional Review Board.
Results
Forty‐two of the 59 (71%) eligible mothers returned the mailed survey. One mother put a zero for days when asked when she stopped feeding her baby at the breast, although she said that she had started doing so, and another mother put no time frame after several of her responses. These two surveys were excluded from the data analysis. The average age of the 40 mothers who participated was 32 (±4.4) years. Thirty‐four (87%) were white, 25 (68%) were married and 32 (80%) had private insurance.
All 40 respondents reported putting their baby to the breast within the first day of life (Fig. 1). All 40 mothers expressed their milk and all 40 infants were fed expressed milk. The infant fed breast milk for the shortest length of time also was fed another mother's milk for 30 days longer than he received his own mother's milk. Ninety‐five per cent (38 out of 40) of infants were fed at the breast and expressed milk concurrently during the breast milk consumption period. Thirty‐seven per cent (15 out of 40) of the infants were fed the milk that their mothers expressed on the day they started expressing it (not shown), 30% (12 out of 40) were fed expressed milk within the first week, 25% (8 out of 40) waited 1–4 weeks after they started before feeding their infant their expressed breast milk and 13% (5 out of 40) of mothers waited more than 4 weeks to feed their infants their expressed milk. Twenty‐five per cent (10 out of 40) of infants continued to be fed expressed breast milk for 7–230 days longer than their mothers expressed milk, albeit it is not necessarily everyday, and 13% of the infants (5 out of 40) continued to be fed expressed breast milk after the mother had stopped lactating completely (Fig. 1).
Figure 1.
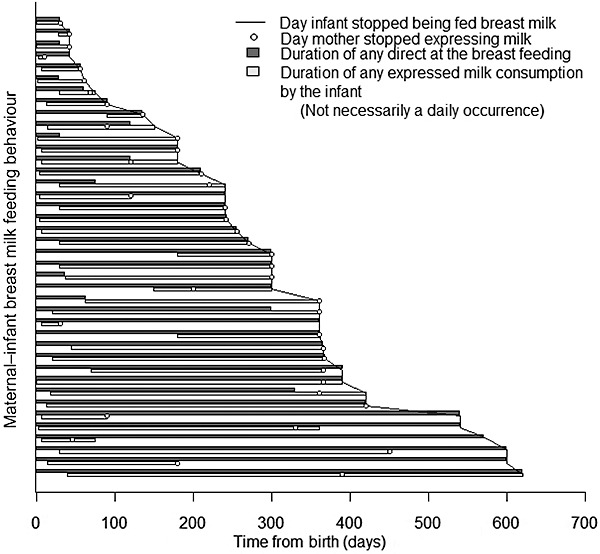
Maternal–infant breast milk feeding behaviour by time since birth.
The methods of breast milk production by the mothers and breast milk consumption by the infants at 2, 14, 42, 90 and 180 days are shown in Table 2. There were 14 different sequences of breast milk production by the 40 mothers and 16 different sequences of consumption by the 40 infants. The most frequent combination of milk production methods by 11 out of 40 mothers (28%) was feeding the infant at the breast at the second day and then including at least some milk expression until at least 6 months. Infants were most commonly fed at the breast at 2 and 14 days and then were fed at least some expressed milk until at least 180 days. Six of the sequences were not practised by both a mother and an infant.
Table 2.
Mothers' breast milk production and infants' breast milk consumption categorised as at the breast, at least some expressed milk feeding, or none at 2, 14, 42, 90 and 180 days
| Number (%) of mothers producing breast milk following sequence (n = 40) | Number (%) of infants consuming breast milk following sequence (n = 40) | Sequence | ||||
|---|---|---|---|---|---|---|
| 2 days | 14 days | 42 days | 90 days | 180 days | ||
| 0 | 0 | B | B | B | B | B |
| 1 (2) | 1 (2) | B | B | B | – | – |
| 0 | 3 (8) | B | B | B | B | E |
| 0 | 3 (8) | B | B | B | E | E |
| 6 (15) | 11 (28) | B | B | E | E | E |
| 11 (28) | 7 (18) | B | E | E | E | E |
| 8 (20) | 2 (5) | E | E | E | E | E |
| 1 (2) | 1 (2) | E | E | – | – | – |
| 2 (5) | 2 (5) | E | E | E | – | – |
| 1 (2) | 0 | E | E | E | E | – |
| 1 (2) | 0 | E | E | E | E | B |
| 0 | 1 (2) | B | B | B | E | – |
| 2 (5) | 1 (2) | B | B | E | – | – |
| 3 (8) | 1 (2) | B | E | E | E | – |
| 0 | 2 (5) | B | B | E | E | – |
| 1 (2) | 1 (2) | B | E | E | – | – |
| 1 (2) | 1 (2) | B | E | B | B | B |
| 1 (2) | 1 (2) | B | E | E | B | B |
| 1 (2) | 2 (5) | B | E | E | E | B |
B, milk production or consumption only at the breast; E, milk production or consumption including at least some expressed breast milk; –, no longer any breast milk production or consumption.
The proportions of mothers producing milk by feeding their infant only at the breast and the proportions of infants consuming breast milk only at the breast at 2, 14, 42, 90 and 180 days are shown in Table 3. The proportion of mothers producing milk by only at the breastfeeding was significantly lower than the proportion of infants who consumed milk only at the breast at 2 (P < 0.01) and 14 (P < 0.01) days. This discrepancy demonstrates that the mothers had already started expressing milk during those times, even though the infants were consuming all of the breast milk that they received only at the breast. Although not significantly different, this trend of mothers expressing milk beyond at the breastfeeding was similar at days 42 and 90. At day 180, four mothers and infants were reported to be feeding breast milk only at the breast, yet all of these mothers had expressed milk previously and all infants already had been fed expressed milk (Table 3).
Table 3.
The concordance between mothers producing breast milk by only feeding their infants at the breast compared to infants consuming breast milk only at the breast of the mother at 2, 14, 42, 90 and 180 days
| 2 days | 14 days | 42 days | 90 days | 180 days | |
|---|---|---|---|---|---|
| Percent (95% CI) of mothers producing breast milk by only feeding their infants at the breast | 68 (52, 85) | 23 (8, 37) | 5 (0, 13) | 5 (0, 13) | 10 (0, 20) |
| Percent (95% CI) of infants consuming breast milk by only feeding at the breast of the mother | 88 (76, 99) | 55 (38, 72) | 23 (8, 37) | 13 (1, 24) | 10 (0) |
| P‐value | <0.01 | <0.01 | 0.07 | 0.39 | 0.80 |
CI, confidence interval.
Discussion
The challenge of properly measuring and accurately defining breastfeeding behaviour for mothers and their infants culminates in the task scientists now face, namely relating expressed milk feeding to health outcomes. The seminal studies that established the benefits of breastfeeding for both mothers and infants compared outcomes of infants directly feeding at the mothers' breast vs. the feeding of a breast milk substitute from a bottle or cup. Breast milk expression creates a combination of these two once‐distinct behaviours because breast milk is now in a bottle or cup. In our study, all mothers expressed milk and all of their infants were fed expressed milk. Almost all infants were fed expressed milk concurrently while feeding directly at the breast. One infant in the cohort was fed another mother's milk. Mothers expressed milk sometimes weeks before their infants received that milk and mothers stopped expressing milk or even lactating at all while their infants were still being fed expressed milk. There were multiple sequences of breast milk production by mothers and breast milk consumption by infants, which were not necessarily the same within a dyad. Starting at the immediate post‐partum period, mothers began ‘overproducing’ their milk by starting milk expression, while their infants were only fed breast milk at the breast. In our study, ‘breastfeeding’ by no means could be described as simply ‘at the breast’ feeding.
This complexity of infant feeding behaviours illustrates the need for improvement in the measurement of ‘breastfeeding’. For example, national breastfeeding rates in the United States currently are determined by responses to a set of questions assessing a child's breast milk intake (Centers for Disease Control and Prevention 2011). These questions do not distinguish the method of the breast milk intake by the infant, yet the CDC reports them as the ‘percent of children who were “breastfed” by birth year’. Although this statement implies that these infants were fed directly at the breast of their mothers, they may not have been. Moreover, the CDC's data, which are collected from the perspective of the infant, are used to describe the breastfeeding behaviours of mothers in the recent Surgeon General's ‘Call to Action to Support Breastfeeding’ (U.S. Department of Health and Human Services 2011). Our study was small, but it documents clearly that when an infant receives breast milk, he may not always be fed at his mother's breast, and, in turn, that his mother even may not be lactating. The feeding of another mother's milk, which has unidentified consequences, (Geraghty et al. 2011) is not captured by the CDC's questions either; thus, the national incidence of milk sharing is currently unknown.
Results of this study also showed that mothers made more milk than their infants needed at the time. At days 2 and 14, while over half of the infants in our study were being fed the entire amount of breast milk which they consumed only at the breast, several mothers were making extra milk by also expressing it. Although we did not ask mothers why they were ‘overproducing’ milk, they may have been attempting to make extra milk so that someone else could feed the infant [as seen in the IFPS II (Labiner‐Wolfe et al. 2008)] or to have a store of milk before returning to work. Outcomes related to this behaviour are unknown. While these findings obviously need to be repeated with a much larger group, we caution that Labbok and Krasovec's categorisation (Labbok & Krasovec 1990) or any other categorisation of breastfeeding based on the estimated proportion of an infant's daily intake may be inadequate to accurately quantify the amount of maternal milk production. As we previously recommended, both clinical history‐taking and research data‐gathering around maternal and infant breast milk production and consumption behaviours would best be recorded separately. This study is a demonstration of our previous work in this area, showing how to actually collect data separately from mothers and infants and how disparate the results can be. Although this study was on a small scale with a cohort of mothers who were having some type of breastfeeding problem for which they sought help, the same questions can be asked in a larger cohort to determine more generalisable results.
Limitations of our study include small size, retrospective data collection relaying on mothers' ability to accurately recall their feeding choices and the fact that all mothers were seen in our breastfeeding referral practice. These mothers may have been more determined to provide human milk for their infants longer than the general population. Although we were not studying the prevalence or duration of breast milk expression in this group, we know that these mothers may have chosen to express their milk earlier and longer because of problems feeding their infants directly at the breast. While reasons for breast milk expression are now being studied (Binns et al. 2009; Clemons & Amir 2010), we do not know specifically why women in our study expressed their milk or why they sometimes waited weeks to feed their infants stored breast milk. We also do not know why some women may have ‘overproduced’ their milk during certain periods of time. These are questions that need careful study. Ethical considerations to the practice of breast milk expression should include analysis as to what advice mothers are getting about breast milk expression and if it is ultimately beneficial to the mother–infant dyad. Moreover, the determination needs to be made as to who is giving mothers the message that it is advantageous to make more milk than their child needs when the medical community does not support this behaviour. By choosing these varied methods of breast milk feeding, women may be shifting the outcomes previously thought to be associated with ‘breastfeeding’ for both themselves and their infants.
Conclusions
As a result of breast milk expression by all mothers in this cohort, we observed highly variable patterns of maternal breast milk production and infant breast milk consumption, which were not necessarily synchronous within a dyad. These distinct maternal and infant behaviours challenge traditional definitions of ‘breastfeeding’ as well as our understanding of the benefits of breastfeeding for both mothers and their infants. It is now time to develop appropriate ways to characterise the production and consumption of breast milk more accurately and investigate whether these behaviours have consequences for the health of mothers and infants.
Source of funding
This study was funded by NIH K23ES014691 (SRG).
Conflicts of interest
The authors declare that they have no conflicts of interest.
Contributors
All authors originated the study, and wrote and revised the drafts.
Acknowledgement
The authors are grateful to Ms. Leslie Kemper for the help in carrying out the study.
References
- Becker G.E., McCormick F.M. & Renfrew M.J. (2008) Methods of milk expression for lactating women. Cochrane Database of Systematic Reviews (4), CD006170. [DOI] [PubMed] [Google Scholar]
- Binns C.W., Fraser M.L., Lee A.H. & Scott J. (2009) Defining exclusive breastfeeding in Australia. Journal of Paediatrics and Child Health 45, 174–180. [DOI] [PubMed] [Google Scholar]
- Boswell‐Penc M. & Boyer K. (2007) Expressing anxiety? Breast pump usage in American wage workplaces. Gender, Place, Culture 14, 551–567. [Google Scholar]
- Centers for Disease Control and Prevention (CDC) (2011) Breastfeeding among U.S. children born 1999–2007 CDC National Immunization Survey. Available at: http://www.cdc.gov/breastfeeding/data/NIS_data/ (Accessed 1 November 2011).
- Clemons S.N. & Amir L.H. (2010) Breastfeeding women's experience of expressing: a descriptive study. Journal of Human Lactation 26, 258–265. [DOI] [PubMed] [Google Scholar]
- Flaherman V.J., Gay B., Scott C., Aby J., Stewart A.L. & Lee K.A. (2012) Development of the breast milk expression experience measure. Maternal & Child Nutrition. DOI:10.111/j.1740‐8709.2011.00390.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geraghty S.R. (2011) Photo album of pumped breastmilk. Breastfeeding Medicine 6, 433–434. [DOI] [PubMed] [Google Scholar]
- Geraghty S.R. & Rasmussen K.M. (2010) Redefining ‘breastfeeding’ initiation and duration in the age of breastmilk pumping. Breastfeeding Medicine 5, 135–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geraghty S.R., Heier J.E. & Rasmussen K.M. (2011) Got milk? Sharing human milk via the Internet. Public Health Reports 126, 161–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hector D.J. (2011) Complexities and subtleties in the measurement and reporting of breastfeeding practices. International Breastfeeding Journal 6, 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ip S., Chung M., Raman G., Trikalinos T.A. & Lau J. (2009) A summary of the Agency for Healthcare Research and Quality's evidence report on breastfeeding in developed countries. Breastfeeding Medicine 4 (Suppl. 1), S17–S30. [DOI] [PubMed] [Google Scholar]
- Johnson S., Williamson I., Lyttle S. & Leeming D. (2009) Expressing yourself: a feminist analysis of talk around expressing breast milk. Social Science & Medicine 69, 900–907. [DOI] [PubMed] [Google Scholar]
- Kelleher C.M. (2006) The physical challenges of early breastfeeding. Social Science & Medicine 63, 2727–2738. [DOI] [PubMed] [Google Scholar]
- Labbok M. & Krasovec K. (1990) Toward consistency in breastfeeding definitions. Studies in Family Planning 21, 226–230. [PubMed] [Google Scholar]
- Labiner‐Wolfe J., Fein S.B., Shealy K.R. & Wang C. (2008) Prevalence of breast milk expression and associated factors. Pediatrics 122 (Suppl. 2), S63–S68. [DOI] [PubMed] [Google Scholar]
- Leonard S.A., Labiner‐Wolfe J., Geraghty S.R. & Rasmussen K.M. (2011) Associations between high prepregnancy body mass index, breast‐milk expression, and breast‐milk production and feeding. The American Journal of Clinical Nutrition 93, 556–563. [DOI] [PubMed] [Google Scholar]
- Leon‐Cava N., Lutter C., Ross J. & Martin L. (2002) Quantifying the Benefits of Breastfeeding: A Summary of the Evidence. PAHO: Washington, DC. [Google Scholar]
- Li R., Fein S.B. & Grummer‐Strawn L.M. (2010) Do infants fed from bottles lack self‐regulation of milk intake compared with directly breastfed infants? Pediatrics 125, e1386–e1393. [DOI] [PubMed] [Google Scholar]
- Rasmussen K.M. & Geraghty S.R. (2011) The quiet revolution: breastfeeding transformed with the use of breast pumps. American Journal of Public Health 101, 1356–1359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shealy K.R., Scanlon K.S., Labiner‐Wolfe J., Fein S.B. & Grummer‐Strawn L.M. (2008) Characteristics of breastfeeding practices among US mothers. Pediatrics 122 (Suppl. 2), S50–S55. [DOI] [PubMed] [Google Scholar]
- Thulier D. (2010) A call for clarity in infant breast and bottle‐feeding definitions for research. Journal of Obstetric, Gynecologic, and Neonatal Nursing 39, 627–634. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services (2011) The Surgeon General's Call to Action to Support Breastfeeding. U.S. Department of Health and Human Services, Office of the Surgeon General: Washington, DC. [Google Scholar]
- United States Breastfeeding Committee (2010) Implementing the Joint Commission Perinatal Care Core Measure on Exclusive Breast Milk Feeding (ed. Ed R.). United States Breastfeeding Committee: Washington, DC. [Google Scholar]
- World Health Organization (2008) Indicators for Assessing Infant and Young Child Feeding Practices: Conclusions of a Consensus Meeting Held 6–8 November 2007 (ed. Geneva S.). World Health Organization: Washington, DC. [Google Scholar]


