Abstract
Objective
To examine trends in disparities in children's mental health care.
Data
2002–2007 Medical Expenditure Panel Survey.
Study Design
We used the Institute of Medicine (IOM) definition of health care disparities and estimated two-part expenditure models to examine disparity trends in any mental health care use, any outpatient care, and psychotropic drug use, as well as expenditures in these three categories, conditional on use. We used 2-year longitudinal panel data to determine disparities in care initiation among children with unmet need.
Principal Findings
Assessing trends over time between 2002 and 2007, we identified that disparities persist for blacks and Latinos in receipt of any mental health care, any outpatient care, and any psychotropic drug use. Among those with positive mental health care expenditures, Latino–white disparities in overall mental health care expenditures increased over time. Among children with unmet need, significant disparities in initiation of an episode of mental health care were found, with whites approximately twice as likely as blacks and Latinos to initiate care.
Conclusions
Disparities in children's mental health care use are persistent and driven by disparities in initiation, suggesting policies to improve detection or increase initial access to care may be critical to reducing disparities.
Keywords: Racial disparities, children's mental health, health care expenditures, psychotropic drug use
Noting significant racial/ethnic disparities in mental health care, the U.S. Surgeon General promoted a vision for reducing these disparities in 2001 (U.S. Department of Health and Human Services 2001). Evidence indicated that African American children were less likely than white children to use mental health services, even after adjustment for socioeconomic, family, and regional factors (Cuffe et al. 1995; Cunningham and Freiman 1996; Zahner and Daskalakis 1997). Limited findings for Latino children were mixed. Puerto Ricans received less mental health care than mainland Latino children (Leaf et al. 1996), and Latino children reported fewer lifetime counseling visits than whites (Pumariega et al. 1998). On the other hand, Latino children with both mental health disorder and impairment had less unmet need for care than white children (Flisher et al. 1997).
Since then, other studies have emerged documenting disparities in children's mental health care, finding black–white disparities in psychotropic drug use nationwide (Chen and Chang 2002) and in the Medicaid population (Zito et al. 2005), and Latino–white and black–white disparities in psychotropic drug use in the child welfare population (Raghavan et al. 2005). Latino–white and black–white disparities were also found in children's antidepressant use (Kirby, Hudson, and Miller 2010) and stimulant use (Olfson et al. 2003; Hudson, Miller, and Kirby 2007). To our knowledge, previous studies have not assessed disparities in children's overall mental health care expenditures or outpatient mental health care use, or tracked trends in children's mental health care use and spending over time.
To understand how disparities in children's mental health care use have changed since the Surgeon General's report, we use the Andersen behavioral model of health care utilization as a conceptual framework (Andersen 1995), recognizing the importance of predisposing factors (e.g., age and gender), enabling factors (e.g., income, education, and insurance), and need-based factors (e.g., mental health status and comorbid physical health status) on mental health care utilization.
The IOM Definition of Health Care Disparities
Health care disparities have been measured using multiple methods and disparity definitions, including assessing differences in unadjusted means as is done in the National Health care Disparities Reports (AHRQ 2008b), interpreting race coefficients in models that increasingly add available covariates in a regression context (Fiscella et al. 2002; Trivedi et al. 2005; Vaccarino et al. 2005; Guevara et al. 2006), and model-based estimations of disparities that adhere to the Institute of Medicine (IOM) definition of health care disparities (McGuire et al. 2006; Cook, McGuire, and Miranda 2007; Cook et al. 2010b). We use the latter approach in this article, building on the IOM definition put forth in Unequal Treatment (IOM 2002), that defines disparity to be any difference in health care not due to clinical appropriateness, need, or patient preferences for health care services (see Figure 1).
Figure 1.
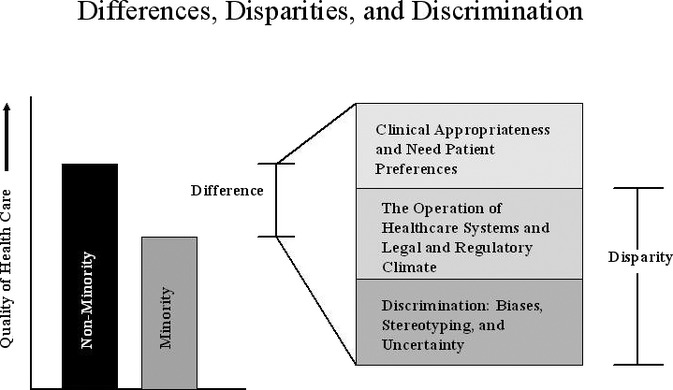
The Institute of Medicine Definition of Racial/Ethnic Health Care Disparities
Ideally, implementation of the IOM definition of racial/ethnic health care disparities in national health care datasets requires the identification of survey variables that match the constructs of clinical appropriateness, need, and patient preferences. To compute disparities, an analyst would adjust for differences due to clinical appropriateness, need, and patient preferences but include differences due to other variables (Cook, McGuire, and Zaslavsky 2012). Mental and physical health status variables are strong proxies for need for services, as are age and sex given large differences across these categories in prevalence of mental illness (Merikangas et al. 2010; Kessler et al. 2012). Differences due to patient preferences (e.g., perceived value of medical care and tolerance of risk) should also be adjusted for to the extent they are available in the data. Clinical appropriateness may be more difficult to account for in studies that use observational data, and we are unable to account for this in our analysis.
Although clinical appropriateness, need, and patient preference variables should be equalized or adjusted across racial/ethnic groups according to the IOM definition, differences due to the operation of health care systems and the legal and regulatory climate should be considered part of the disparity (see Figure 1). In survey data, differences due to measures of socioeconomic status (SES) (e.g., income and education) can be considered to fit into the operation of health care systems category. For example, if lower SES families are less able to navigate the health care system or pay for their children's mental health care, and racial/ethnic minority families are disproportionately represented in lower SES categories, then the operation of the health care system may be affecting disparities through SES. Differences due to discrimination should also be considered to be part of the disparity according to the IOM definition (see Figure 1). In regression models of survey data, the independent effect of race/ethnicity on health care can be considered a proxy for discrimination (National Research Council 2004).
Using Longitudinal Data to Assess Disparities in Mental Health Care
Analysis of longitudinal data can identify underlying care-seeking behaviors and correlates of treatment behaviors that drive disparities in mental health care, fulfilling in part the need for research that is more directly translatable into disparities reduction policies (Alegria 2009). Unlike cross-sectional data analysis, longitudinal data analysis can distinguish whether disparities in any use of mental health care are due to whites’ greater initiation of care or whites’ longer treatment episodes. The policy implications will differ depending on the result. Also important, individual characteristics in cross-sectional data can be endogenous to the decision to seek treatment. For example, being insured may affect whether an individual seeks treatment, but once treatment is initiated, children may be more likely to be insured (either because providers encourage enrolling children in public programs or parents choose to enroll their children), thus biasing the effect of insurance on treatment downward. In longitudinal data, patient characteristics can be observed in the time period prior to treatment initiation, reflecting the circumstances of individuals when deciding to seek treatment.
New Contribution
This study measures recent national trends in disparities in children's mental health care and is the first study that we are aware of to measure disparities in children's use of outpatient mental health care. In addition, this article makes two important contributions over and above the prior literature. First, we ground our method of measuring disparities conceptually in the IOM definition of racial/ethnic health care disparities. Second, we capitalize on longitudinal panel data from the Medical Expenditure Panel Surveys (MEPS) and model the initiation of treatment among youth with unmet need for mental health care. This analysis allows us to identify mechanisms associated with disparities in initiation of mental health care.
Methods
Data
Data are from the Household Component of the 2002–2007 MEPS for youth age 5–21. Models were fit using MEPS cross-sectional data from two pooled time periods (2002–2003 and 2006–2007). Two years were combined for each time period to increase the precision of estimates. We assessed disparities for overall mental health care, outpatient mental health care, and psychotropic drug use. Each of these outcomes is separated into (1) any use (> $0 expenditure) and (2) expenditures conditional on any use. We considered a visit to involve mental health care if there was an outpatient or office-based visit (hereafter referred to as outpatient visits) or a prescription fill associated with a diagnosis of mental disorder using codes 291, 292, and 295–314 (ICD-9/DSM-IV), or if the treatment was coded as psychotherapy or mental health counseling (Zuvekas 2001). Prices were adjusted to 2007 dollars using the Consumer Price Index (CPI).
Longitudinal analyses were conducted using six merged two-year panels (Panels 6–11). Each panel's respondents were surveyed at five time periods (Rounds 1–5). We assessed mental and physical health status, sociodemographic characteristics, and mental health care in Rounds 1 and 2 (“preperiod”) and Rounds 3, 4, and 5 (“postperiod”).
The MEPS contain a large number of missing values on certain variables. Our initial sample of 35,574 non-Latino white, black, and Latino individuals ages 5–21 for the 2002–2003 and 2006–2007 data was trimmed to 30,171 to exclude those with missing data. To account for differential missingness by race/ethnicity, and to maintain generalizability of the data to the white, black, and Latino youth population, we reweighted the included individuals to represent their propensity to be like individuals with missing values (Brick and Kalton 1996; Wooldridge 2002).
Measures
Individuals of any race claiming to be of Latino or Hispanic origin were identified as Latino in our study. Other respondents were classified as black or white by responses to the question about race. Other covariates used in our model were classified into two broad categories to implement the IOM definition of disparity: (1) variables indicating need and patient preferences (as mentioned above, we were unable to account for clinical appropriateness in these data) and (2) SES variables. SES variables include family income, parents’ highest level of education, region of the country, urban or rural location, and insurance coverage (see Table 1 for more detail on categorizations). Variables representing need are parent-assessed mental health and physical health scores (rated in four categories as excellent, very good, good, fair/poor), having any functional limitation, gender, and age (5–9, 10–13, 14–18, 19–21). Sensitivity analyses were conducted for the sample age 5–17 to control for a more detailed mental health measure, the Columbia Impairment Scale (CIS) (Bird et al. 1996). Although no specific item measured preferences for mental health care in the MEPS, we proxied for preferences using parents’ responses to items asking whether the parent believes illness can be overcome without medical help and whether the parent was more likely to take risks than the average individual.
Table 1.
Weighted Population Characteristics for Blacks, Latinos, and Non-Latino Whites Ages 5–21† 2002–2003 and 2006–2007 Medical Expenditure Panel Survey (MEPS)
| White | Black | Latino | ||||
|---|---|---|---|---|---|---|
| 2002–2003 (N = 7,448) | 2006–2007 (N = 5,899) | 2002–2003 (N = 2,911) | 2006–2007 (N = 2,748) | 2002–2003 (N = 5,457) | 2006–2007 (N = 5,035) | |
| Dependent variables | ||||||
| Any mental health care use (%) | 10.2 | 9.9 | 5.2 ** | 6.1 ** | 4.4 ** | 5.5 ** |
| Mental health expenditure given use | $ 1,126.57 | $ 1,544.89 | $ 1,016.42 | $ 1,219.71 | $ 1,891.46 | $ 1,828.14 |
| Any outpatient MH use (%) | 8.2 | 7.5 | 4.4 ** | 4.6 ** | 3.7 ** | 4.4 ** |
| Outpatient MH expenditure given use | $ 655.81 | $ 797.26 | $ 544.61 | $ 552.01 ** | $ 1,062.00 | $ 693.00 |
| Any psychotropic drug use (%) | 7.5 | 7.3 | 2.8 ** | 4.3 **,‡ | 2.9 ** | 3.4 ** |
| Psychotropic drug expenditure given use | $ 628.87 | $ 806.10 | $ 555.72 | $ 567.59 | $ 821.66 | $ 574.22 |
| Need and preferences | ||||||
| Age (%) | ||||||
| 5–9 | 27.6 | 27.9 | 28.5 | 26.5 | 32.2 ** | 31.7 ** |
| 10–13 | 24.0 | 22.3 | 26.8 ** | 24.4 ** | 24.7** | 23.5 ** |
| 14–18 | 31.4 | 31.6 | 29.4 ** | 32.7 **,‡ | 26.5 ** | 28.4 ** |
| 19–21 | 17.0 | 18.2 | 15.4 | 16.4 | 16.6 | 16.4 |
| Gender (%) | ||||||
| Female | 49.1 | 48.7 | 48.4 | 49.9 | 48.9 | 47.8 |
| MH status (%)(Parent report) | ||||||
| Excellent | 53.9 | 54.9 | 52.6 | 52.6 | 43.1** | 47.3 ** |
| Very good | 28.6 | 27.8 | 26.9 | 24.1 | 32.3** | 30.9 ** |
| Good | 14.7 | 14.6 | 16.9 ** | 19.8 ** | 21.7** | 19.3 ** |
| Fair | 2.4 | 2.3 | 2.9 ** | 2.8 ** | 2.4 | 2.1 |
| Poor | 0.4 | 0.5 | 0.7 | 0.7 | 0.5 | 0.4 |
| Limitation of activity (%) | ||||||
| Any | 4.7 | 4.1 | 3.8 | 3.6 | 4.6 | 3.5 |
| Psychological impairment (%) (age <18 only) | ||||||
| Columbia impairment scale > 16 | 11.3 | 11.6 | 11.0 | 10.4 | 6.5 ** | 5.2 ** |
| Health status (%) (parent report) | ||||||
| Excellent | 51.8 | 54.5 | 48.3 ** | 48.3 ** | 39.2 ** | 42.1 ** |
| Very good | 30.3 | 29.1 | 26.9 | 26.7 | 31.9 | 31.0 |
| Good | 15.1 | 13.9 | 21.8 ** | 20.4 ** | 24.2 | 23.4 |
| Fair | 2.4 | 2.1 | 2.8 | 4.1 | 4.3 ** | 3.1 ** |
| Poor | 0.4 | 0.4 | 0.3 | 0.5 | 0.5 | 0.4 |
| Parent preferences (%) | ||||||
| More likely to take risks | 28.1 | 30.0 | 26.4 | 22.9 | 27.7 | 31.4 |
| Feel child can overcome illness without medical help | 37.4 | 37.9 | 26.4 | 23.6 | 26.5** | 27.7 ** |
| Socioeconomic status/system factors | ||||||
| Family income level (%) % FPL | ||||||
| <100% FPL | 10.0 | 10.0 | 29.5 ** | 30.3 ** | 25.8 ** | 25.4 ** |
| 100–125% FPL | 3.6 | 3.2 | 6.4 ** | 6.9 ** | 9.2 ** | 8.5 ** |
| 126–200% FPL | 11.9 | 12.1 | 19.6 ** | 18.8 ** | 24.4 ** | 23.0 ** |
| 201–400% FPL | 36.4 | 35.7 | 29.7 ** | 28.4 ** | 28.3 ** | 30.2 ** |
| > 400% FPL | 38.1 | 39.1 | 14.8 ** | 15.5 ** | 12.3 ** | 12.9 ** |
| Parent's education (%) | ||||||
| <High school education | 6.7 | 5.2 | 18.0 | 14.6 | 41.4 | 38.4 |
| High school graduate | 93.3 | 94.8 | 82.0 ** | 85.4 ** | 58.6 ** | 61.6 ** |
| Insurance status (%) | ||||||
| Private | 77.8 | 74.0 | 49.6 ** | 50.8 ** | 42.5 ** | 37.1 **,‡ |
| Medicaid/SCHIP | 17.2 | 19.4 | 48.2 ** | 47.7 ** | 41.3 ** | 46.6 **,‡ |
| Other public insurance | 0.3 | 0.4 | 2.4 ** | 0.8 ** | 1.2 ** | 1.0 ** |
| Uninsured | 7.4 | 7.9 . | 6.7 | 7.2 | 20.1 ** | 18.9 ** |
| Region (%) | ||||||
| Northeast | 20.2 | 19.7 | 16.3 | 16.5 | 12.6 ** | 12.6 ** |
| Midwest | 27.7 | 27.3 | 19.1 ** | 19.0 ** | 8.4 ** | 9.2 ** |
| South | 32.6 | 34.0 | 55.2 ** | 56.1 ** | 33.8 | 34.6 |
| West | 19.5 | 19.0 | 9.5 ** | 8.4 ** | 45.1** | 43.6 ** |
| Urbanicity (%) | ||||||
| Urban area: population > 250K | 77.0 | 77.7 | 87.6 ** | 88.2 ** | 91.1 ** | 92.9 ** |
Overall difference between minority group and whites is significant at α < .05 level.
Calculations are weighted to be representative of the entire U.S. population.
Difference in trends for minority group is significantly different from difference in trends for whites at p < .05 level.
Data: Combined yearly cross-sectional data from 2002/2003 and 2006/2007 Medical Expenditure Panel Survey (MEPS). FPL, federal poverty level; MH, mental health.
Statistical Analysis
We first examined characteristics of the 2002–2003 and 2006–2007 MEPS sample, providing racial/ethnic group means for our main dependent and independent variables. We then assessed disparity trends in a multivariate setting. To examine expenditures, we used two-part generalized linear models (GLMs) (Blough, Madden, and Hornbrook 1999) to account for a large mass of zeros and extremely skewed expenditure data. Two-part models separately analyze the likelihood of receiving care using logistic regression and the level of expenditure conditional on any use (McCullagh and Nelder 1989). Using diagnostics in Manning and Mullahy (2001) and Buntin and Zaslavsky (2004), we identified the optimal generalized linear model for the expenditure variables to have a log link, and a gamma distribution to correspond to the conditional variance. All model estimates were weighted to reflect sample design and survey nonresponse.
Because we estimated differences in racial/ethnic disparities over two pooled time periods (2002–2003 and 2006–2007), main effects of race/ethnicity and year, as well as a race by year interaction term, were used as predictors. Other predictors were a vector of need variables and a vector of SES variables relevant to the Andersen behavioral model of health care utilization (Andersen 1995) and racial/ethnic mental health care disparities (Cook, McGuire, and Miranda 2007; Kirby, Hudson, and Miller 2010). We also inserted Need by Race and SES by Race interaction terms into the model because previous studies have identified that the association between SES and health care use varies by racial/ethnic group, as does the relationship between need variables and health care use (e.g., Cook, McGuire, and Zuvekas 2009). The model is as follows:
| (1) |
where Yi is the utilization by individual, Needi is the vector of need indicator variables, SESi is the vector of SES characteristics, including poverty status, education, and insurance status, and Yeart is the indicator of whether the information was collected in 2006–2007. For conditional expenditures, we estimated the above-described GLM using the same covariates in Equation (1).
Implementing the IOM Definition of Disparity
To apply the IOM definition of racial/ethnic disparities, we built on the model estimation described above as step one in a four-step process: (1) model estimation; (2) adjustment for need and preference variables (hereafter abbreviated as “need variables”); (3) estimation of minority group predicted use and expenditures using coefficients from the model and the distributions of variables for each racial/ethnic group (including the adjusted need variables); and (4) comparison of the mean of these adjusted minority group predictions with unadjusted white means.
To implement the adjustment of need variables, we used a rank-and-replace method described in McGuire et al. (2006) and Cook, McGuire, and Zuvekas (2009) that creates a counterfactual population of black or Latino individuals with the white distribution of need without adjustment for SES covariates. First, multivariate indicators of need were summarized with a univariate need-based linear predictor defined as the sum of the terms (coefficient times covariate) of the fitted model corresponding to need variables. Individuals were then assigned survey-weighted ranks within their race based on this need predictor, and the need variable values of each minority individual were replaced by those of the equivalently ranked white individual. Thus, a black individual with a need-based predictor at the p-th percentile for blacks would be reassigned the need variable values of the white individual at the p-th percentile for whites.
Predicted use and expenditure for each minority individual were then calculated using the coefficients and SES values from the original two-part model and the adjusted need covariate values. The means of these predictions were then subtracted from the corresponding white group's unadjusted mean to estimate an IOM-concordant disparity.
Longitudinal Data Analysis
To better understand determinants of treatment initiation, we focused on youth with probable need (parent-reported mental health of good, fair, or poor) but no mental health care in the preperiod. We estimated a logistic regression of postperiod initiation of mental health care conditional on a similar set of covariates as that described in (1), except we intentionally used baseline or preperiod values for covariates. Panel indicators were included to account for secular changes over time.
Variance Estimation
Variance estimates account for the complex sample design. Stratum and primary sampling unit variables were standardized across pooled years (AHRQ 2008a) using publicly available strata and psu variables that specify a common variance structure for MEPS respondents across multiple years of data. Variance estimates for predicted expenditures, rates, and disparities were calculated using a balanced-repeated-replication (BRR) procedure (Wolter 1985).
Results
Unadjusted Analyses
Unadjusted black–white and Latino–white differences existed in both 2002–2003 and 2006–2007 for any mental health care use, any outpatient mental health care, and any psychotropic drug use with black–white differences in any psychotropic drug use in 2006–2007 being significantly smaller than black–white differences in 2002–2003 (Table 1). Fewer significant differences in level of use, conditional on any use, were found in either time period studied. Black–white differences in conditional outpatient mental health care expenditures were identified in 2006–2007. Summarizing population characteristics, compared with whites, black youth were in worse physical and mental health, had lower SES, were more likely to live in the South, and to be enrolled in Medicaid or other public insurance. Compared with whites, Latino children were younger, less likely to report excellent mental health status but also less likely to have psychological impairment, had lower SES, and were more likely to be uninsured, enrolled in Medicaid and other public insurance, and to live in the West. A significant shift in these characteristics was that Latinos, compared with whites, had a greater increase over time in rates of Medicaid insurance and a greater decrease in rates of private insurance.
Mental Health Care Use
In Table 2, we present disparity predictions using the IOM-concordant method. We found that black–white and Latino–white disparities existed in both periods (2002–2003 and 2006–2007) for all three of the any use outcomes studied (see Appendix Table A1 for regression results); disparity trends were insignificant for all these measures, suggesting few changes in disparities over the time period studied. Among those that initiated mental health care, no significant differences in black–white disparities were found in either time period. Latino–white disparities existed in overall and outpatient mental health care expenditures in 2006–2007, but not in 2002–2003, with Latino–white disparities in overall mental health care expenditures significantly increasing between 2002–2003 and 2006–2007. Results were identical in sensitivity analyses using only youth 5–17 including the CIS measure of mental health impairment to further control for need.
Table 2.
Disparities in Mental Health Care Use Implementing the IOM Definition†, MEPS 2002–2007
| Any MH Care Use (n = 29,948) | Any Outpatient MH Care Use (n = 29,948) | Any Psychotropic Drug Use (n = 29,948) | ||||
|---|---|---|---|---|---|---|
| Disparity | SE* | Disparity | SE* | Disparity | SE* | |
| Black–white | ||||||
| 2006–2007 | −5.6% | (0.7%) | −4.2% | (0.6%) | −4.3% | (0.6%) |
| 2002–2003 | −6.6% | (0.8%) | −5.0% | (0.7%) | −5.5% | (0.7%) |
| Difference in disparity | 1.0% | (0.8%) | 0.8% | (0.8%) | 1.2% | (0.7%) |
| Latino–white | ||||||
| 2006–2007 | −5.4% | (0.8%) | −3.8% | (0.7%) | −4.4% | (0.8%) |
| 2002–2003 | −6.5% | (0.8%) | −4.9% | (0.7%) | −4.9% | (0.8%) |
| Difference in disparity | 1.1% | (0.9%) | 1.1% | (0.8%) | 0.6% | (0.7%) |
| Expenditures Given Any MH Care Use (n = 2,184) | Outpatient Expenditures Given Use (n = l,743) | Psychotropic Drug Expenditures Given Use (n = l,517) | ||||
|---|---|---|---|---|---|---|
| Disparity ($) | SE* | Disparity ($) | SE* | Disparity ($) | SE* | |
| Black–white | ||||||
| 2006–2007 | −474.25 | (343.76) | 146.48 | (378.94) | −364.99 | (522.28) |
| 2002–2003 | −379.64 | (282.23) | 166.64 | (389.50) | −83.40 | (300.67) |
| Difference in disparity | −94.62 | (216.43) | −20.16 | (185.49) | −281.60 | (321.20) |
| Latino–white | ||||||
| 2006–2007 | −664.63 | (272.43) | −347.96 | (124.55) | −232.96 | (209.86) |
| 2002–2003 | −161.00 | (332.22) | −176.05 | (138.92) | −28.38 | (216.62) |
| Difference in disparity | −503.63 | (222.35) | −171.91 | (118.36) | −204.58 | (149.62) |
Standard errors are calculated using balanced-repeated-replication (BRR) methodology.
Need- and preference-related variables used in adjustments concordant with the IOM definition were parent-reported mental health status, physical and mental health components of the SF-12, age, sex, marital status, activity limitation, and whether the parent was more likely to take risks than the average individual. Numbers in bold indicate differences in disparities that are significant at the α <.05 level.
Data: Combined yearly cross-sectional data from 2002/2003 and 2006/2007 Medical Expenditure Panel Survey (MEPS).
Longitudinal Data Analysis
Using longitudinal MEPS panel data and focusing on a population with probable unmet mental health care need (parent-reporting good, fair, or poor mental health in the postperiod and having no mental health care in the preperiod), we identified large racial/ethnic disparities in postperiod initiation of mental health care (Figure 2; see Appendix Table A2 for regression results). IOM-concordant predictions of initiation of mental health care for this group found that whites (10.1 percent) were approximately twice as likely as blacks (5.3 percent) and Latinos (4.3 percent) to initiate care in the postperiod.
Figure 2.
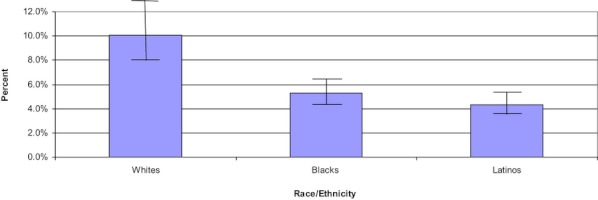
Predicted Probability of Individuals with Probable Unmet Mental Health Care in Preperiod Initiating Mental Health Care in Postperiod Data: Medical Expenditure Panel Survey Panels 6–11 (2002–2007): Sample Includes Individuals Age 5–21 with Probable Unmet Mental Health Care Need (i.e., Parent-Reported Good, Fair, or Poor Mental Health in the Preperiod (Rounds 1 and 2 of the MEPS) with No Preperiod Mental Health Care
Discussion
Trends in children's mental health care from 2002 to 2007 indicate persistent racial/ethnic disparities in our three measures of access to mental health care (i.e., any mental health care, any outpatient mental health care, and any psychotropic drug use). Yet we found fewer significant disparities in expenditures, conditional on use, with the exception that Latino–white disparities in conditional mental health care expenditures increased significantly over time. These findings build on previous literature that identified black–white and Latino–white disparities in youth psychotropic drug use (e.g., Chen and Chang 2002; Raghavan et al. 2005; Kirby, Hudson, and Miller 2010). Our findings provide further evidence of these disparities in any psychotropic drug use and additionally identified disparities in access to mental health care overall and access to outpatient mental health care. Our findings of black–white disparities in any mental health care but no disparities in expenditures conditional on any use are consistent with patterns identified in the adult population (Cook et al. 2010b). Our results imply that policies focused on reducing barriers to access for blacks and Latinos should be prioritized.
In the longitudinal analysis, we limited our sample to those with probable need for care and no mental health care in the preperiod, to ensure that covariates controlled for were not in fact caused by treatment initiation. In doing so, we found that the magnitude of disparities in any mental health care use was greater in relative terms than disparities in any mental health care use among the general youth population, with blacks and Latinos initiating care in the postperiod half as much as whites. Furthermore, sensitivity analyses among those with psychological impairment (CIS≥16) identified similar trends to our main disparity trends analyses.
Disparities in treatment may have far-reaching effects. Recent literature suggests that presence of mental health conditions in youth may lead to worse educational attainment and academic performance (Currie and Stabile 2006; Ding et al. 2009; Fletcher 2010), poorer social outcomes in adulthood (Cook, Carson, and Alegria 2010a), and pose greater risk for alcohol or drug abuse (Substance Abuse and Mental Health Services Administration 2007). To the extent black children are less likely to be treated and treatment reduces symptoms of mental health conditions improving educational outcomes (Busch, Golberstein, and Meara 2011), these disparities may lead to long-term differences in earnings.
A limitation of this study is the absence of a full set of parent- and child-reported exogenous, fully informed preferences for mental health care. This is typical of other disparities studies (Braddock et al. 1999; Ashton et al. 2003; Armstrong, Hughes-Halbert, and Asch 2006). We believe our preference measures (parent's overall risk and parent's belief that illness can be overcome without medical help) are less likely than more targeted mental health services preferences measures to be influenced by limited information or previous discriminatory practices. However, we also recognize that these general measures may be poor proxies for preferences relevant to children's mental health care. We think the bias introduced from omission of additional preference measures is minimal given the strong likelihood that preferences are driven by previous experiences with the health care system, which may be the result of disparate treatment by race/ethnicity. To the extent that unobserved preferences do represent a realistic response to past experiences of discrimination or inferior access to and quality of health care, rather than an exogenously determined preference, our analysis treats these preferences in accordance with the IOM definition. These unobserved racial/ethnic differences will load into the race/ethnicity indicator coefficients and be included in disparity calculations.
A second limitation is the lack of more specific measures of mental health status than those available in the MEPS. Lack of information on diagnoses of mental illness among individuals that do not utilize care necessitates reliance on a brief measure (parent-reported mental health) and a scale (CIS). However, the MEPS is the sole data source with sufficient numbers of ethnic and racial minority cases to estimate nationally representative trends in mental health service disparities with precision with a very short lag time between data collection and public release. In addition, the parent-reported mental health and CIS measures have been shown to predict psychological distress, depressed mood, and functioning (Fleishman and Zuvekas 2007), and to correspond with psychiatric symptoms and diagnosed mental illness (Hoff et al. 1997). One caveat is that Zuvekas and Fleishman (2008) found the SRMH differentially predicted emotional functioning (measured using the mental health component of the SF-12 (Ware, Kosinski, and Keller 1996) across racial/ethnic groups of adults, with blacks and Latinos reporting good, fair, or poor mental health at more severe levels of emotional functioning than whites. If these same patterns are true in the SRMH when parents are reporting on their children's mental health, then the greater severity of blacks and Latinos in the good, fair, or poor group makes our initiation disparities findings even more striking. Related to this limitation, because we used observational data, and did not have access to medical records for survey respondents, we were unable to control for clinical appropriateness of treatment. There is evidence of a misallocation of treatment in mental health care and disparities may be due to overtreatment of whites or undertreatment of blacks or Latinos or both (Shaffer et al. 1996; Alegria et al. 2008) and we cannot distinguish among these in this study.
The MEPS data did not contain a sufficient sample to assess how more expensive and potentially less appropriate mental health care factored into disparities (or lack of disparities) in mental health care expenditures. Less than 0.5 percent of our sample reported inpatient or emergency room mental health care use. Future research using datasets with greater samples of individuals using these types of mental health services is needed to identify the relationship between cost, severity of illness upon access, and disparities in mental health care expenditures. In addition, because the MEPS identifies youth mental health service use through parent reporting, there is the possibility that parents may have been unwilling to reveal that their children received care from a provider for mental health reasons. Given that stigma may be a barrier to receiving mental health care within minority communities (Pumariega, Rogers, and Rothe 2005), it is possible that differential underreporting by racial/ethnic minorities bias results toward identifying greater disparities in parent-reported survey data compared with administrative data. A final limitation is that cost information in the MEPS reflects charges, which may be higher than actual payments to providers. However, charges may be a more relevant measure of actual resource use given that payments may be distorted in health care markets which are not perfectly competitive.
In conclusion, our findings suggest that improving initiation of care is critical for targeting future efforts. Thus, policies to increase detection of childhood mental health disorders, perhaps through improved screening efforts, will potentially be effective in reducing disparities.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: This research was supported by grants R01 MH080883 (PI Busch) and R01 MH082312 (PI Cook) from the National Institute of Mental Health. We also are grateful for comments and suggestions received from Noelia Duchovny, who was a reviewer of this paper as part of the 2010 Meeting of the American Society of Health Economists.
Disclosures: None.
Disclaimers: None.
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Table A1: Regression Coefficients from Models of Mental Health Care Use and Expenditures.
Table A2: Regression Coefficients from Model of Initiation of Mental Health Care among Those At Risk for Mental Illness with No Pre-Period Mental Health Care Visits.
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
References
- AHRQ. MEPS HC-036BRR: 1996-2006 Replicates for Calculating Variances File. Rockville, MD: Agency for Healthcare Research and Quality; 2008a. [Google Scholar]
- AHRQ. National Healthcare Quality Report, 2008. Rockville, MD: Agency for Healthcare Research and Quality; 2008b. [Google Scholar]
- Alegria M. “Academy Health 25th Annual Research Meeting Chair Address: From a Science of Recommendation to a Science of Implementation”. Health Services Research. 2009;44(1):5–14. doi: 10.1111/j.1475-6773.2008.00936.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegria M, Chatterji P, Wells K, Cao Z, Chen C, Takeuchi D, Jackson J, Meng XL. “Disparity in Depression Treatment among Racial and Ethnic Minority Populations in the United States”. Psychiatric Services. 2008;59(11):1264–72. doi: 10.1176/appi.ps.59.11.1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen RM. “Revisiting the Behavioral Model and Access to Medical Care: Does It Matter?”. Journal of Health and Social Behavior. 1995;36(1):1–10. [PubMed] [Google Scholar]
- Armstrong K, Hughes-Halbert C, Asch D. “Patient Preferences Can Be Misleading as Explanations for Racial Disparities in Health Care”. Archives of Internal Medicine. 2006;166(9):950–4. doi: 10.1001/archinte.166.9.950. [DOI] [PubMed] [Google Scholar]
- Ashton CM, Haidet P, Paterniti DA, Collins TC, Gordon HS, O'Malley K, Petersen LA, Sharf BF, Suarez-Almazor ME, Wray NP, Street RL., Jr “Racial and Ethnic Disparities in the Use of Health Services: Bias, Preferences, or Poor Communication?”. Journal of General Internal Medicine. 2003;18(2):146–52. doi: 10.1046/j.1525-1497.2003.20532.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bird HR, Andrews HF, Schwab-Stone M, Goodman SH, Dulcan MK, Richters J, Rubio-Stipec M, Moore RE, Chiang PH, Hoven CW, Canino G, Fisher P, Gould MS. “Global Measures of Impairment for Epidemiologic and Clinical Use with Children and Adolescents”. International Journal of Methods in Psychiatric Research. 1996;6(4):295–307. [Google Scholar]
- Blough DK, Madden CW, Hornbrook MC. “Modeling Risk Using Generalized Linear Models”. Journal of Health Economics. 1999;18(2):153–71. doi: 10.1016/s0167-6296(98)00032-0. [DOI] [PubMed] [Google Scholar]
- Braddock CH, 3rd, Edwards KA, Hasenberg NM, Laidley TL, Levinson W. “Informed Decision Making in Outpatient Practice: Time to Get Back to Basics”. Journal of the American Medical Association. 1999;282(24):2313–20. doi: 10.1001/jama.282.24.2313. [DOI] [PubMed] [Google Scholar]
- Brick JM, Kalton G. “Handling Missing Data in Survey Research”. Statistical Methods in Medical Research. 1996;5(3):215–38. doi: 10.1177/096228029600500302. [DOI] [PubMed] [Google Scholar]
- Buntin MB, Zaslavsky AM. “Too Much Ado about Two-Part Models and Transformation? Comparing Methods of Modeling Medicare Expenditures”. Journal of Health Economics. 2004;23(3):525–42. doi: 10.1016/j.jhealeco.2003.10.005. [DOI] [PubMed] [Google Scholar]
- Busch S, Golberstein E, Meara E. Cambridge, MA: National Bureau of Economic Research; 2011. The FDA and ABCs: The Unintended Consequences of Antidepressant Warnings on Human Capital. NBER Working Paper Series. No: 17426. [Google Scholar]
- Chen AY, Chang RKR. “Factors Associated with Prescription Drug Expenditures among Children: An Analysis of the Medical Expenditure Panel Survey”. Pediatrics. 2002;109(5):728–32. doi: 10.1542/peds.109.5.728. [DOI] [PubMed] [Google Scholar]
- Cook B, Carson N, Alegria M. “Assessing Racial/Ethnic Differences in the Social Consequences of Early-Onset Psychiatric Disorder”. Journal of Health Care for the Poor and Underserved. 2010a;21(2):49–66. doi: 10.1353/hpu.0.0289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook B, McGuire T, Miranda J. “Measuring Trends in Mental Health Care Disparities, 2000–2004”. Psychiatric Services. 2007;58(12):1533–9. doi: 10.1176/ps.2007.58.12.1533. [DOI] [PubMed] [Google Scholar]
- Cook B, McGuire TG, Zaslavsky AM. “Measuring Racial/Ethnic Disparities in Health Care: Methods and Practical Issues”. Health Services Research. 2012;47 (3 part 2):1232–54. doi: 10.1111/j.1475-6773.2012.01387.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook BL, McGuire TG, Zuvekas SH. “Measuring Trends in Racial/Ethnic Health Care Disparities”. Medical Care Research and Review. 2009;66(1):23–48. doi: 10.1177/1077558708323607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook BL, McGuire T, Lock K, Zaslavsky A. “Comparing Methods of Racial and Ethnic Disparities Measurement across Different Settings of Mental Health Care”. Health Services Research. 2010b;45(3):825–47. doi: 10.1111/j.1475-6773.2010.01100.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuffe S, Waller J, Cuccaro M, Pumariega A, Garrison C. “Race and Gender Differences in the Treatment of Psychiatric Disorders in Young Adolescents”. Journal of the American Academy of Child & Adolescent Psychiatry. 1995;34(11):1536–43. doi: 10.1097/00004583-199511000-00021. [DOI] [PubMed] [Google Scholar]
- Cunningham P, Freiman M. “Determinants of Ambulatory Mental Health Services Use for School-Age Children and Adolescents”. Health Services Research. 1996;31(4):409–25. [PMC free article] [PubMed] [Google Scholar]
- Currie J, Stabile M. “Child Mental Health and Human Capital Accumulation: The Case of ADHD”. Journal of Health Economics. 2006;25:1094–118. doi: 10.1016/j.jhealeco.2006.03.001. [DOI] [PubMed] [Google Scholar]
- Ding W, Lehrer SF, Rosenquist J, Audrain-McGovern J. “The Impact of Poor Health on Academic Performance: New Evidence from Genetic Markers”. Journal of Health Economics. 2009;29:578–97. doi: 10.1016/j.jhealeco.2008.11.006. [DOI] [PubMed] [Google Scholar]
- Fiscella K, Franks P, Doescher MP, Saver BG. “Disparities in Health Care by Race Ethnicity, and Language among the Insured: Findings from a National Sample”. Medical Care. 2002;40(1):52–9. doi: 10.1097/00005650-200201000-00007. [DOI] [PubMed] [Google Scholar]
- Fleishman JA, Zuvekas SH. “Global Self-Rated Mental Health: Associations with Other Mental Health Measures and with Role Functioning”. Medical Care. 2007;45(7):602–9. doi: 10.1097/MLR.0b013e31803bb4b0. [DOI] [PubMed] [Google Scholar]
- Fletcher JM. “Adolescent Depression and Educational Attainment: Results Using Sibling Fixed Effects”. Health Economics. 2010;19(7):855–71. doi: 10.1002/hec.1526. [DOI] [PubMed] [Google Scholar]
- Flisher A, Kramer R, Grosser R, Alegria M, Bird H, Bourdon K, Goodman S, Greenwald S, Horwitz S, Moore R, Narrow W, Hoven C. “Correlates of Unmet Need for Mental Health Services by Children and Adolescents”. Psychological Medicine. 1997;27(5):1145–54. doi: 10.1017/s0033291797005412. [DOI] [PubMed] [Google Scholar]
- Guevara JP, Mandell DS, Rostain AL, Zhao H, Hadley TR. “Disparities in the Reporting and Treatment of Health Conditions in Children: An Analysis of the Medical Expenditure Panel Survey”. Health Services Research. 2006;41(2):532–49. doi: 10.1111/j.1475-6773.2005.00484.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoff RA, Bruce ML, Kasl SV, Jacobs SC. “Subjective Ratings of Emotional Health as a Risk Factor for Major Depression in a Community Sample”. The British Journal of Psychiatry. 1997;170(2):167–72. doi: 10.1192/bjp.170.2.167. [DOI] [PubMed] [Google Scholar]
- Hudson JL, Miller GE, Kirby JB. “Explaining Racial and Ethnic Differences in Children's Use of Stimulant Medications”. Medical Care. 2007;45(11):1068–75. doi: 10.1097/MLR.0b013e31806728fa. [DOI] [PubMed] [Google Scholar]
- IOM. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academies Press; 2002. [PubMed] [Google Scholar]
- Kessler RC, Avenevoli S, Costello EJ, Georgiades K, Green JG, Gruber MJ, He J, Koretz D, McLaughlin KA, Petukhova M. “Prevalence, Persistence, and Sociodemographic Correlates of DSM-IV Disorders in the National Comorbidity Survey Replication Adolescent Supplement”. Archives of General Psychiatry. 2012;69(4):372–80. doi: 10.1001/archgenpsychiatry.2011.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirby JB, Hudson J, Miller GE. “Explaining Racial and Ethnic Differences in Antidepressant Use among Adolescents”. Medical Care Research and Review. 2010;67(3):342–63. doi: 10.1177/1077558709350884. [DOI] [PubMed] [Google Scholar]
- Leaf P, Alegría M, Cohen P, Goodman S, Horowitz S, Hoven C, Narrow W, Vaden-Kiernan M, Regier D. “Mental Health Service Use in the Community and Schools: Results from the Four-Community MECA Study”. Journal of the American Academy of Child & Adolescent Psychiatry. 1996;35:889–97. doi: 10.1097/00004583-199607000-00014. [DOI] [PubMed] [Google Scholar]
- Manning W, Mullahy J. “Estimating Log Models: To Transform or Not to Transform?”. Journal of Health Economics. 2001;20(4):461–94. doi: 10.1016/s0167-6296(01)00086-8. [DOI] [PubMed] [Google Scholar]
- McCullagh P, Nelder JA. Generalized Linear Models. London: Chapman & Hall; 1989. [Google Scholar]
- McGuire TG, Alegria M, Cook BL, Wells KB, Zaslavsky AM. “Implementing the Institute of Medicine Definition of Disparities: An Application to Mental Health Care”. Health Services Research. 2006;41(5):1979–2005. doi: 10.1111/j.1475-6773.2006.00583.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, He JP, Brody D, Fisher PW, Bourdon K, Koretz DS. “Prevalence and Treatment of Mental Disorders among US Children in the 2001-2004 NHANES”. Pediatrics. 2010;125(1):75–81. doi: 10.1542/peds.2008-2598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Research Council. Measuring Racial Discrimination. Panel on Methods for Assessing Discrimination. Washington, DC: National Academy Press; 2004. pp. 121–8. [Google Scholar]
- Olfson M, Gameroff M, Marcus S, Jensen P. “National Trends in the Treatment of Attention Deficit Hyperactivity Disorder”. American Journal of Psychiatry. 2003;160(6):1071–7. doi: 10.1176/appi.ajp.160.6.1071. [DOI] [PubMed] [Google Scholar]
- Pumariega AJ, Rogers K, Rothe E. “Culturally Competent Systems of Care for Children's Mental Health: Advances and Challenges”. Community Mental Health Journal. 2005;41(5):539–55. doi: 10.1007/s10597-005-6360-4. [DOI] [PubMed] [Google Scholar]
- Pumariega A, Glover S, Holzer C, Nguyen H. “Administrative Update: Utilization of Services. II. Utilization of Mental Health Services in a Tri-Ethnic Sample of Adolescents”. Community Mental Health Journal. 1998;34(2):145–56. doi: 10.1023/a:1018788901831. [DOI] [PubMed] [Google Scholar]
- Raghavan R, Zima BT, Andersen RM, Leibowitz AA, Schuster MA, Landsverk J. “Psychotropic Medication Use in a National Probability Sample of Children in the Child Welfare System”. Journal of Child & Adolescent Psychopharmacology. 2005;15(1):97–106. doi: 10.1089/cap.2005.15.97. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Dulcan MK, Davis D, Piacentini J, Schwab-Stone M, Lahey B, Bourdon K, Jensen P, Bird HR, Canino G, Regier D. “The NIMH Diagnostic Interview Schedule for Children (DISC 2.3): Description, Acceptability, Prevalences, and Performance in the MECA Study”. Journal of the American Academy of Child & Adolescent Psychiatry. 1996;35(7):865–77. doi: 10.1097/00004583-199607000-00012. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2007. Depression and the Initiation of Alcohol and Other Drug Use among Youths Aged 12 to 17. No: May 3, 2007. [Google Scholar]
- Trivedi AN, Zaslavsky AM, Schneider EC, Ayanian JZ. “Trends in the Quality of Care and Racial Disparities in Medicare Managed Care”. New England Journal of Medicine. 2005;353(7):692–700. doi: 10.1056/NEJMsa051207. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Culture, Race, and Ethnicity: A Supplement to Mental Health a Report of the Surgeon General. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service Office of the Surgeon General; 2001. [Google Scholar]
- Vaccarino V, Rathore SS, Wenger NK, Frederick PD, Abramson JL, Barron HV, Manhapra A, Mallik S, Krumholz HM. “Sex and Racial Differences in the Management of Acute Myocardial Infarction, 1994 through 2002”. New England Journal of Medicine. 2005;353(7):671–82. doi: 10.1056/NEJMsa032214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ware JE, Kosinski M, Keller SD. “A 12-Item Short-Form Health Survey: Construction of Scales and Preliminary Tests of Reliability and Validity”. Medical Care. 1996;34(3):220–33. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- Wolter K. Introduction to Variance Estimation. New York: Springer-Verlag; 1985. [Google Scholar]
- Wooldridge JM. Econometric Analysis of Cross Section and Panel Data. Cambridge, MA: The MIT press; 2002. “Sample Selection, Attrition, and Stratified Sampling”; pp. 587–90. [Google Scholar]
- Zahner G, Daskalakis C. “Factors Associated with Mental Health, General Health, and School-Based Service Use for Child Psychopathology”. American Journal of Public Health. 1997;87(9):1440–8. doi: 10.2105/ajph.87.9.1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zito JM, Safer DJ, Zuckerman IH, Gardner JF, Soeken K. “Effect of Medicaid Eligibility Category on Racial Disparities in the Use of Psychotropic Medications among Youths”. Psychiatric Services. 2005;56(2):157–63. doi: 10.1176/appi.ps.56.2.157. [DOI] [PubMed] [Google Scholar]
- Zuvekas SH. “Trends in Mental Health Services Use and Spending, 1987-1996”. Trends in Mental Health. 2001;20(2):214–24. doi: 10.1377/hlthaff.20.2.214. [DOI] [PubMed] [Google Scholar]
- Zuvekas SH, Fleishman JA. “Self-Rated Mental Health and Racial/Ethnic Disparities in Mental Health Service Use”. Medical Care. 2008;46(9):915–23. doi: 10.1097/MLR.0b013e31817919e5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


