Abstract
Aniridia is a rare congenital disorder in which there is a variable degree of hypoplasia or the absence of iris tissue associated with multiple other ocular changes, some present from birth and some arising progressively over time. Most cases are associated with dominantly inherited mutations or deletions of the PAX6 gene. This article will review the clinical manifestations, the molecular basis including genotype–phenotype correlations, diagnostic approaches and management of aniridia.
Keywords: aniridia, PAX6, eye, iris, foveal hypoplasia, WAGR syndrome
In Brief
Aniridia is a rare, sight-threatening disorder that affects the iris, retina, optic nerve, lens and cornea.
The major diagnostic feature is congenital absence or hypoplasia of the iris; foveal hypoplasia with reduced visual acuity is almost always present and is usually associated with nystagmus.
Progressive sight-threatening complications include keratopathy, cataract and glaucoma.
Aniridia patients may have other sensory deficits including reduced olfaction and hearing difficulties.
In the vast majority of cases, aniridia is caused by the loss of function of one copy (haploinsufficiency) of the PAX6 gene at 11p13 by intragenic mutation or chromosomal rearrangement.
The PAX6 gene encodes a transcription factor with multiple roles in the development of the eye and other tissues.
Familial aniridia cases show autosomal dominant inheritance with high penetrance but considerable phenotypic heterogeneity.
Newborns with sporadic aniridia are at greatly increased risk of the paediatric nephroblastoma Wilms tumour if they have a deletion encompassing PAX6 and the nearby Wilms tumour predisposition gene (WT1 gene). Such deletions may manifest as Wilms tumour-aniridia-genital anomalies-retardation (WAGR) syndrome.
Missense mutations in the PAX6 paired domain often cause atypical phenotypes ranging from mild iris hypoplasia to Peters anomaly and microphthalmia.
INTRODUCTION
Aniridia (MIM 106210) is a condition of complete or partial iris hypoplasia and foveal hypoplasia, resulting in reduced visual acuity and nystagmus.1, 2 It usually presents in early infancy. Frequently associated ocular abnormalities, generally with later onset, include cataract, glaucoma and corneal abnormalities. About two-thirds of cases are familiar with dominant inheritance; the remainders are sporadic. Aniridia occurs either as an isolated ocular abnormality without obvious systemic involvement or as part of the WAGR (Wilms tumour-aniridia-genital anomalies-retardation) contiguous gene syndrome.3 Individuals with WAGR have a significant risk of developing Wilms tumour, a childhood kidney malignancy. The prevalence of aniridia is 1:40 000 to 1:100 000 with no known influence of race or gender.1, 4
CLINICAL OVERVIEW
Aniridia is a panocular disorder affecting tissues throughout the eye, in addition to the iris abnormalities for which it is named.1, 2, 5 Affected individuals characteristically have absent or altered iris tissue and foveal hypoplasia, which generally leads to nystagmus and impaired visual acuity (usually 20/100–20/200). Later onset cataracts, glaucoma and corneal opacification are responsible for progressive visual failure (Figure 1).1, 2, 5, 6, 7, 8, 9 The phenotype can vary between and within families, but affected individuals usually show little difference between the two eyes. Most cases present within six weeks of birth with an obvious iris or pupillary abnormality or nystagmus. Despite their many ocular problems, most aniridia patients can retain useful vision with appropriate ophthalmic care.
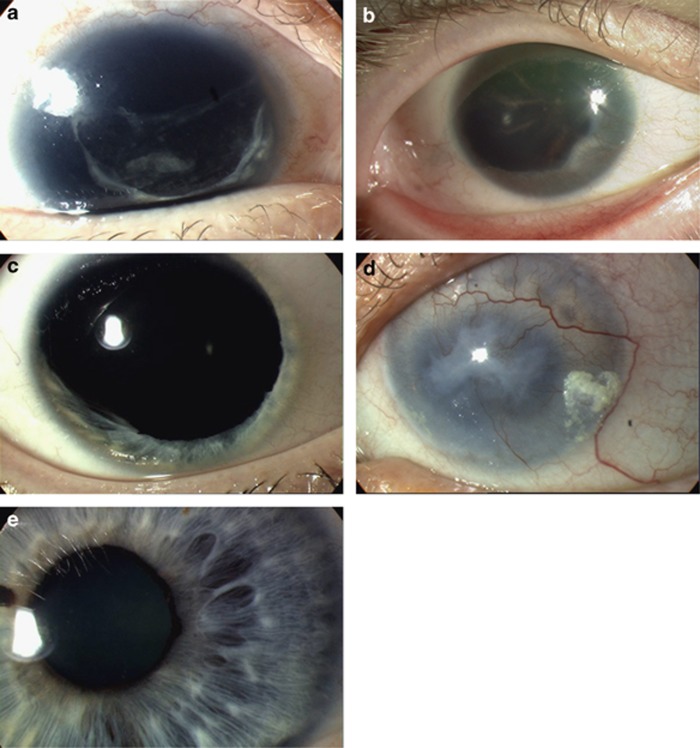
Figure 1.
Heterozygous PAX6 mutations cause a range of eye phenotypes. (a) Total absence of iris tissue with surgical aphakia (removal of natural lens) and remnant of opaque lens capsule (CTE mutation). (b) Almost complete absence of iris tissue obscured by peripheral corneal changes with opacification and neovasularisation, and unusual partly pigmented cortical lens opacities (PTC mutation). (c) Partial absence of iris tissue (missense mutation). (d) Severe aniridic keratopathy with total loss of transparency and neovasularisation of the cornea (PTC mutation). (e) Full iris demonstrating substantial area of abnormal iris architecture (missense mutation). Panels (c) and (e) are reproduced from Hingorani et al.7 Association for Research in Vision and Ophthalmology.
Iris
The most characteristic ocular abnormality is iris hypoplasia (Figure 1). In the most severe cases, the iris may be reduced to a small stump of residual tissue, visible only on gonioscopy or ultrasound biomicroscopy; in the mildest cases, the iris may be present but abnormal on transillumination or for surface architecture.6, 7, 10 Other changes include partial iris defects (resembling a coloboma), eccentric or misshapen pupils and iris ectropion (ectropion uveae).
Lens
Congenital lens opacities (especially polar) are common.1, 2, 6, 7 Occasionally there are remnants of the foetal vascularisation of the anterior lens capsule (tunica vasculosa lentis) or a persistent pupillary membrane. Cataracts are rare in infancy, but visually significant lens opacities eventually develop in 50–85% of aniridics, often in the teens or early adulthood. Lens subluxation or dislocation also occurs but infrequently.
Intraocular pressure
Elevated intraocular pressure without optic disc and visual field changes (ocular hypertension) and glaucoma (intraocular pressure-related optic disc cupping and visual field reduction) are common, with an eventual prevalence of 30–50%.1, 2, 5, 6, 7 Glaucoma usually develops in later childhood or adulthood but may be present in infancy with a large corneal diameter and corneal oedema (buphthalmos).
Cornea
Keratopathy (corneal abnormality) is a relatively late and often progressive manifestation mainly due to limbal stem cell failure. Changes vary from mild peripheral vascularisation to pancorneal vascularisation, opacification and keratinisation (Figure 1).1, 2, 6, 7 Corneal deterioration may be triggered by surgical intervention for cataract or glaucoma. Inadequate tear production is common, exacerbating the ocular surface problems. Central corneal thickness is often increased and this may cause under-estimation of intraocular pressure on tonometry and failure to diagnose glaucoma.
Fovea
Foveal hypoplasia is usually present and manifests as reduced foveal reflex, macular hypopigmentation and crossing of the usual foveal avascular zone by retinal vessels.2, 7
Optic nerve
Optic nerve hypoplasia (small, malformed optic nerve) occurs in up to 10% of cases; optic nerve colobomata are also seen occasionally.7, 8
Refractive error, strabismus and ptosis
Myopia, hypermetropia, astigmatism, as well as squints are commonly seen in aniridics.5, 7, 11 Up to 10% of patients may have ptosis (drooping eyelid).
Aniridic fibrosis syndrome
Multiple intraocular surgeries sometimes trigger a fibrotic membrane to grow from the root of the iris tissue remnant behind the lens and cornea, causing displacement or entrapment of the intraocular lens (IOL) and corneal opacification.12
Systemic features
There is growing realisation that aniridia patients may have non-ocular sensory and neurological deficits. Thus, even ‘isolated' aniridia may have characteristic systemic features.
Central nervous system
In patients with isolated aniridia, reduced olfaction appears to be the most common functional deficit.13 MRI studies have demonstrated abnormalities of the anterior commissure, anterior cingulate cortex, cerebellum, temporal and occipital lobes, corpus callosum, pineal gland and olfactory bulb.13, 14, 15 Nevertheless, cognitive function is generally normal.16 Behavioural difficulties and developmental delay are rare.17, 18
Hearing
Aniridics may have central auditory processing deficits owing to abnormal interhemispheric transfer, which can cause hearing difficulties. Diagnosis requires detailed audiological assessment, but is important in patients, especially children, who already have a visual impairment.15
WAGR syndrome
Sporadic aniridia must be investigated to determine whether it is caused by a chromosomal deletion of PAX6 that also includes WT1, the Wilms tumour predisposition gene. Such cases are at strongly increased risk (up to 50%) of the paediatric nephroblastoma known as Wilms tumour (MIM 194070). Classical WAGR syndrome (MIM 194072) includes Wilms tumour with Aniridia, genitourinary abnormalities and mental Retardation, but the phenotype is highly variable.3, 4, 19, 20 Aniridia is the most consistent symptom.3 The term ‘WAGR syndrome' is generally used even if a patient does not exhibit all four classical features. Similarly, ‘WAGR deletion' describes a deletion involving PAX6 and WT1 even if Wilms tumour is absent. WAGR Wilms tumours are more likely to be bilateral, and present earlier than other Wilms tumours.3, 21 Developmental kidney abnormalities, including focal segmental glomerulosclerosis, are more common, as is end-stage renal disease.22 Genitourinary abnormalities include cryptorchidism (in 60% of males), hypospadias and ambiguous genitalia, uterine abnormalities, streak ovaries, ureteric abnormalities and gonadoblastoma.3 Mental retardation (IQ<74) has been documented in 70% of WAGR patients and tends to be associated with larger deletions.3, 4 A variety of dysmorphic features and behavioural, neurological and metabolic abnormalities, including obesity, may also be present.3, 23, 24
MOLECULAR AND GENETIC BASIS OF ANIRIDIA
Loss of function of one copy of the PAX6 gene can be identified in about 90% of aniridia cases, with intragenic mutations accounting for two-thirds and chromosomal rearrangements for one-third of cases.4, 25 About two-thirds of all cases are familial and show dominant inheritance with very-high penetrance.4, 5 In the remaining sporadic cases, the new mutation (which presumably arose de novo in the germ line of one parent) will be dominantly inherited in subsequent generations.1, 9
Structure and function of the PAX6 gene
The 14 exon PAX6 gene, located at 11p13, encodes a highly conserved transcriptional regulator with two DNA binding domains (a paired domain and a homeodomain) and a transcriptional trans-activation domain.2, 26, 27 PAX6 is expressed in the developing eye, multiple brain regions, olfactory bulb, neural tube, gut and pancreas. It is active early in ocular morphogenesis, fulfilling multiple roles in development of the retina, lens, cornea and iris.26, 27 Its targets include PAX6 itself and genes encoding other developmental regulators, such as SOX2, cell adhesion molecules and structural proteins including lens crystallins and corneal keratins.2, 26, 27
PAX6 mutation spectrum
The PAX6 locus-specific database (http://lsdb.hgu.mrc.ac.uk/home.php?select_db=PAX6) currently contains 334 unique sequence changes scattered throughout the gene. Over 90% of these are predicted to disrupt transcription or translation and likely to be pathological mutations; the remainder are probably neutral polymorphisms. Ninty-four percent of all intragenic point mutations lead to the introduction of a premature termination codon (PTC), or to C-terminal extensions (CTE), or amino acid substitutions (missense changes).
PTC mutations
Predicted protein truncations in the open reading frame arise through different mechanisms: nonsense mutations, frame-shifting insertions and deletions and most splice mutations.6, 7, 25, 28, 29, 30 Mutant mRNAs containing a PTC are generally degraded by nonsense-mediated decay (unless the PTC is very close to the stop codon).31 Synthesis of a truncated protein is prevented and a mutant null allele is effectively produced.28, 29 Nearly a fifth of the 552 records currently in the database are accounted for by just four common nonsense mutations: p.Arg203* (24 reports), p.Arg240* (40 reports), p.Arg261* (15 reports) and p.Arg317* (29 reports). Most mutations, however, have been reported only once or twice. The large number of unique mutations reflects the many paths to PAX6 gene disruption.
PTC (null) mutations usually cause classical aniridia with iris aplasia and progressive sight-threatening ocular changes.2, 7 Even with null alleles, however, the degree of iris hypoplasia can vary greatly, potentially complicating the diagnosis.6, 7
CTE mutations
These cause the open reading frame to continue into the 3′ untranslated region and appear to cause a phenotype towards the severe end of the spectrum.7, 32 Nonsense-mediated decay is not predicted for CTE transcripts, which probably produce an extended protein with impaired function.29 The CTE mutation (c.1267dupT), in which the termination codon is replaced by a leucine codon, is the fourth most common intragenic PAX6 mutation (20 reports).
Missense mutations
Intragenic changes predicted to lead to single-amino acid substitutions will produce a full-length protein that may fold and function subnormally or abnormally.7, 29 Fifty five percent of missense mutations cause variant phenotypes ranging from very mild iris defects with well-preserved visual acuity, to phenotypes more severe than classical aniridia, including optic nerve malformations, Peters anomaly and microphthalmia.6, 7, 26, 33, 34, 35 Mild missense mutations often lead to a partial set of classical aniridia symptoms, such as nystagmus, cataract, glaucoma and/or keratopathy.6, 7 Four-fifths of missense mutations are located in the paired domain; these may affect binding of the PAX6 protein to its target genes.26, 34, 35 Phenotypic severity is probably correlated with functional impairment of the mutant protein.36
Compound heterozygous PAX6 mutations
There are three published cases of children inheriting two pathological PAX6 mutations, one from each affected parent. Two of these compound heterozygous infants died soon after birth with anophthalmia and brain abnormalities.37, 38 The third child survived with severe microphthalmia and microcephaly.39
Chromosomal rearrangements in isolated aniridia and WAGR syndrome
Isolated aniridia can also be caused by chromosomal deletions affecting all or part of the PAX6 region, or translocations and inversions that disrupt the transcription unit or control elements.4, 19, 25, 30 PAX6 is associated with a downstream cluster of highly conserved transcriptional regulatory elements, located in introns of the adjacent ELP4 gene.26, 40 If these elements are removed by a deletion or separated from the PAX6 transcription unit by an inversion or translocation break point, the typical outcome is classical aniridia.25, 26
A proportion of sporadic aniridia cases is caused by contiguous deletion of PAX6 and WT1, which are about 700 kb apart on 11p13.3, 4 The deletion provides the first of two ‘hits' needed to inactivate both WT1 alleles. Somatic loss of both alleles in kidney, or more rarely gonad, triggers tumour development. Cells susceptible to malignancy are only present early in life, so if Wilms tumour has not arisen in a deletion patient by the age of 8 years, it is very unlikely to occur.20, 22
Gillespie syndrome
Gillespie syndrome (MIM 206700) is characterised by circumpupillary aplasia, cerebellar ataxia and developmental delay. Owing to its rarity, the inheritance pattern is unclear. PAX6 intragenic mutations have been reported in two individuals with phenotypes overlapping Gillespie syndrome, but these cases probably have atypical aniridia.41, 42 The molecular basis of classical Gillespie syndrome is unidentified.
Other genes
Aniridia-like phenotypes can result from FOXC1, PITX2 and PITX3 mutations.43, 44, 45, 46 FOXC1 and PITX2 mutations usually cause Axenfeld–Rieger syndrome (MIM 602482 and 180500), characterised by iris hypoplasia (thinning), corectopia (displaced pupil) and polycoria (multiple holes).47 PITX3 mutations typically cause anterior segment dysgenesis and cataracts.46
DIAGNOSTIC APPROACHES
Clinical diagnosis
Aniridia is usually first diagnosed at the clinical level by a paediatrician, often following parental concerns about the baby's vision. An ophthalmologist should verify the diagnosis, although the final decision may require molecular genetic confirmation. Differential diagnoses include anterior segment developmental abnormalities (eg, Axenfeld–Rieger syndrome and Peters anomaly), iris coloboma, albinism (oculocutaneous and ocular), Gillespie syndrome and other causes of infantile nystagmus and reduced vision without iris changes, such as retinal dysplasia, retinal dystrophy, congenital cataracts, optic nerve hypoplasia and congenital infections.
The most important clinical assessment method is slit-lamp examination to identify iris and pupillary abnormalities; corneal opacification and vascularisation and cataract or glaucoma can also be detected if present. Infants will benefit from use of a hand-held slit lamp. Fundoscopy can demonstrate foveal hypoplasia and any associated optic nerve malformations, but for infants an indirect ophthalmoscope will be required. Small children may need to be examined under anaesthesia. Optical coherence tomography may be used to document foveal hypoplasia,48 but is difficult to perform in the presence of nystagmus and in young children. In infants with corneal opacity or severe corneal oedema due to congenital glaucoma, high frequency anterior segment ultrasound examination can demonstrate iris hypoplasia or aplasia.
Genetic diagnosis
Following clinical diagnosis of aniridia in an infant, it is important to assess family history. If there is an affected parent, it is unlikely that the child will have a deletion extending to WT1, although rare cases have been reported.25, 49, 50 Even without obvious family history, ophthalmological examination of the parents should be undertaken for PAX6 spectrum anomalies.
Molecular assessment of PAX6 status
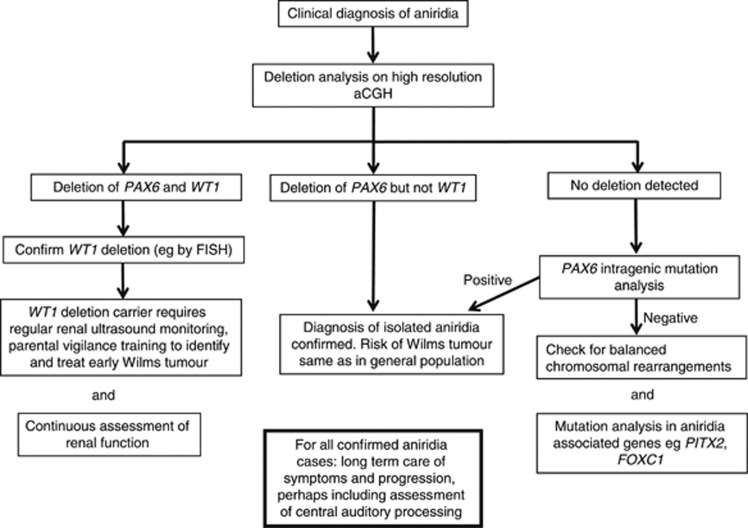
Although intragenic mutations are more common in aniridia patients than deletions, deletion analysis is recommended first because of the clinical importance of detecting WAGR deletions. High-resolution CGH arrays require small amounts of DNA and are increasingly cost-effective. By identifying deletion patients first, sequence analysis, using a variety of established or emerging new generation methods, can be focused on patients who are more likely to have intragenic mutations (Figure 2). However, a small subset of chromosomal disruptions that do not lead to copy number change will not be picked up by arrays. Some molecular service labs still offer fluorescence in situ hybridisation (FISH) to identify rearrangements that might disrupt PAX6 function without copy number change.19, 25 In the future, however, whole-genome sequencing with paired-end sequencing will probably supersede FISH for identifying balanced rearrangements.51, 52 Targeted local deletion analysis is also possible using multiplex ligation-dependent probe amplification (MLPA).30 Some balanced chromosomal rearrangements, such as insertional translocations may lead to recurrent deletions and duplications in a family.53, 54
Figure 2.
Flow-chart illustrating a suggested strategy for molecular analysis of aniridia cases. The priority is to determine whether there is an underlying WAGR deletion (involving both the PAX6 and WT1 loci), which strongly predisposes to Wilms tumour. In cases where WT1 is not deleted, detection of a PAX6 mutation is less urgent but provides a sound basis for genetic counselling. This diagram is intended to show general principles only – molecular techniques are evolving quickly and the specific approaches mentioned here may be superseded by more efficient and cost-effective methods.
Cases without deletions (sporadic and familial) should then undergo intragenic PAX6 mutation analysis. This may be requested by parents or patients themselves, depending on their perception of how useful knowledge of the exact mutation is. Intragenic point mutations are detected by direct sequencing of exons and splice junctions. Small local deletions can be identified by aCGH or MLPA.30
The following step-by-step genetic testing strategy is suggested (see also Figure 2):
First evaluate newly diagnosed aniridia case for the presence of a genomic deletion using high-resolution CGH array.
If a deletion is observed, determine the exact extent.
Identification of a deletion of PAX6 and WT1 confirms the diagnosis of WAGR.
Such a result should trigger surveillance for Wilms tumour (see below). aCGH will also define chromosomal sex, which is important as XY sex reversal to female phenotypic sex can be a feature of WT1 deletion and requires clinical attention.55 If the deletion involves PAX6 but spares WT1, a diagnosis of isolated aniridia is confirmed. The Wilms tumour risk is the same as in the general population.6
If deletion is absent, evaluate for intragenic mutations within the PAX6 coding region, using sequence analysis.
If there are affected relatives, confirm that they carry the same mutation as the proband.
If there is no family history, check parental DNA to determine whether mutation is de novo. Exclude parental mosaicism35 and partial- or non-penetrance, all of which could lead to unexpected familial recurrence if not identified.
Identification of a deleterious PAX6 sequence alteration confirms the diagnosis of isolated aniridia. Individuals that are negative in these tests may have mutations deep in introns or in regulatory elements. Alternatively patients may have mutations in FOXC1, PITX2 or PITX3 (or other candidate genes, yet to be identified), which cause overlapping phenotypes (Figure 2).43, 44, 45, 46
MANAGEMENT
Clinical workup
Risk of WT
Children with clinical WAGR or sporadic aniridia and a confirmed WT1 deletion require regular renal ultrasound examinations every three months and follow-up by a paediatric oncologist until the age of eight years. Cryptorchidism and other genital anomalies also require monitoring and treatment.56
Severity of ocular condition
This can be assessed by measuring the visual acuity (not always easy in infants), determining the degree of iris tissue deficiency and the presence of foveal and optic nerve hypoplasia, in order to predict future visual function. Patients should also be evaluated for corneal involvement, cataract and glaucoma but these are usually of later onset. If surgery is required, special approaches may help to avoid problems due to limbal stem cell insufficiency.9
Genetic counselling
Isolated aniridia
Seventy percent of individuals diagnosed with isolated aniridia have an affected parent.5 Those with no family history may have a de novo gene mutation or deletion. Phenotypic severity can vary greatly among family members, so the parents of anyone with an apparent de novo mutation should be examined for subtle aniridic changes. The risk to siblings depends upon the genetic status of the proband's parents.9 If a parent has isolated aniridia the risk to each child is 50%. When the parents are unaffected, the risk to the sibs of a proband is low, although germ line mosaicism in the parent should be considered.35
WAGR syndrome
Genitourinary system abnormalities, particularly in males, are pleiotropic when WT1 is deleted. Additional abnormalities are also seen in cases with larger deletions. The phenotypic spectrum is determined by the identity of the genes in the deletion.3, 23, 24 Reproductive transmission is thus significantly reduced. Larger WAGR deletions therefore generally arise de novo in each case, and siblings are unlikely to be affected, although rare cases of balanced translocations in a parent can lead to recurrent larger deletions.54 Small WAGR deletions with milder phenotypes are occasionally transmitted vertically.25, 49 These rare fertile WAGR deletion carriers will transmit their deletion to 50% of their offspring. Such cases, which may mimic familial aniridia, will be identified by the strategy presented in Figure 2. Deletion analysis is also informative in rare cases where an asymptomatic parent is mosaic for a deletion.19, 25
Prenatal diagnosis
Prenatal diagnosis by amniocentesis (usually at 15–18 weeks' gestation) or chorionic villus sampling (10–12 weeks' gestation) is possible for:
Isolated aniridia if the disease-causing PAX6 mutation or regulatory region deletion has been identified in the family.57
WAGR caused by a cytogenetic deletion if a balanced chromosome rearrangement has been identified in a parent or a cryptic deletion identified by FISH or deletion testing in the family.
Rare germ line mosaicism for point mutations or deletions – usually identified through somatic mosaicism in an unaffected parent.
Treatment and care
During childhood, simple measures are often the most important. Patients should have regular eye examinations and correction of refractive errors usually using spectacles.5 Tinted or photochromic lenses can reduce light sensitivity. Contact lenses in older patients can be difficult due to corneal changes and dry eyes. Occlusion therapy may be required for anisometropic or strabismic amblyopia. Optical low-vision aids and other devices such as closed-circuit television systems can be crucial for those with significant visual impairment and advice and help with schooling and social support should be offered. As there may be abnormal hearing, detailed audiological evaluation is recommended15 for children reaching school age. Children with WAGR deletions will require surveillance for Wilms tumour (see above) and will need non-ophthalmic medical care with regular evaluation of renal function.
Intraocular pressure and glaucoma
Individuals with aniridia should undergo annual glaucoma screening throughout life, including measurement of intraocular pressure, optic disc examination and visual field assessment, when possible. Glaucoma is initially treated with topical medication and surgery is usually reserved for eyes that do not respond to medical therapy.9 Surgery may involve trabeculectomy with or without antimetabolites (such as 5-fluorouracil or mitomycin C) or drainage tube surgery or cyclodiode laser treatment.2, 9 Glaucoma in infancy, although rare, usually requires early surgery such as goniotomy, trabeculotomy or trabeculectomy with antimetabolites.
Cornea
Corneal problems can be treated medically using lubricants, mucolytics and lacrimal punctal occlusion.2 Drops without preservatives may be beneficial. Corneal surgery carries a poor prognosis and is usually only undertaken when corneal opacification causes significant visual reduction. Penetrating keratoplasty or anterior lamellar keratoplasty may be considered but the significant limbal stem cell deficiency will usually also need addressing by limbal stem cell transplantation, either tissue transplant or cultured stem cells.2 Rarely, a keratoprosthesis (artificial cornea) offers the only hope of some functional vision in cases with severe keratopathy,2 particularly if traditional corneal transplanting has repeatedly failed, but the surgery is fraught with difficulty.
Lens
Cataract extraction (lens aspiration, lensectomy or phacoemulsification depending on age) can significantly improve visual acuity in patients with severe lens opacities.2 However, visual improvement after surgery is limited by other aniridic ocular changes and mild to moderate lens opacities may not benefit from surgery.
Many individuals with aniridia have poor zonular stability that increases the risk of intraoperative complications and influences the choice of surgical technique and options for IOL implantation.9 Black diaphragm aniridic IOLs may reduce glare or light sensitivity, but may be associated with a slightly higher rate of surgical complications.
Aniridic fibrosis syndrome
Early surgical removal of the membrane is required.
CONCLUSION
Aniridia is rare but can significantly and progressively impair vision. Better surgical therapy for glaucoma and, in particular, corneal and limbal stem cell abnormalities is required. Greater awareness of the huge variation in severity is required in the ophthalmic world, as subtle variants of the disorder are often missed or misdiagnosed. Genetic testing has a very important role in confirming the involvement of a PAX6 mutation and determining whether an affected individual is at risk of Wilms tumour.
Web resources
Aniridia Network UK: http://aniridia.org.uk/
Aniridia Foundation International: http://www.aniridia.net/
PAX6 mutation database: http://lsdb.hgu.mrc.ac.uk/home.php?select_db=PAX6
The authors declare no conflict of interest.
References
- Nelson LB, Spaeth GL, Nowinski TS, Margo CE, Jackson L. Aniridia. A review. Surv Ophthalmol. 1984;28:621–642. doi: 10.1016/0039-6257(84)90184-x. [DOI] [PubMed] [Google Scholar]
- Lee H, Khan R, O'Keefe M. Aniridia: current pathology and management. Acta Ophthalmol. 2008;86:708–715. doi: 10.1111/j.1755-3768.2008.01427.x. [DOI] [PubMed] [Google Scholar]
- Fischbach BV, Trout KL, Lewis J, Luis CA, Sika M. WAGR syndrome: a clinical review of 54 cases. Pediatrics. 2005;116:984–988. doi: 10.1542/peds.2004-0467. [DOI] [PubMed] [Google Scholar]
- Gronskov K, Olsen JH, Sand A, et al. Population-based risk estimates of Wilms tumor in sporadic aniridia. A comprehensive mutation screening procedure of PAX6 identifies 80% of mutations in aniridia. Hum Genet. 2001;109:11–18. doi: 10.1007/s004390100529. [DOI] [PubMed] [Google Scholar]
- Valenzuela A, Cline RA. Ocular and nonocular findings in patients with aniridia. Can J Ophthalmol. 2004;39:632–638. doi: 10.1016/s0008-4182(04)80028-0. [DOI] [PubMed] [Google Scholar]
- Gronskov K, Rosenberg T, Sand A, Brondum-Nielsen K. Mutational analysis of PAX6: 16 novel mutations including 5 missense mutations with a mild aniridia phenotype. Eur J Hum Genet. 1999;7:274–286. doi: 10.1038/sj.ejhg.5200308. [DOI] [PubMed] [Google Scholar]
- Hingorani M, Williamson KA, Moore AT, van Heyningen V. Detailed ophthalmologic evaluation of 43 individuals with PAX6 mutations. Invest Ophthalmol Vis Sci. 2009;50:2581–2590. doi: 10.1167/iovs.08-2827. [DOI] [PubMed] [Google Scholar]
- McCulley TJ, Mayer K, Dahr SS, Simpson J, Holland EJ. Aniridia and optic nerve hypoplasia. Eye (Lond) 2005;19:762–764. doi: 10.1038/sj.eye.6701642. [DOI] [PubMed] [Google Scholar]
- Khaw PT. Aniridia. J Glaucoma. 2002;11:164–168. doi: 10.1097/00061198-200204000-00013. [DOI] [PubMed] [Google Scholar]
- Okamoto F, Nakano S, Okamoto C, Hommura S, Oshika T. Ultrasound biomicroscopic findings in aniridia. Am J Ophthalmol. 2004;137:858–862. doi: 10.1016/j.ajo.2003.12.014. [DOI] [PubMed] [Google Scholar]
- Hewitt AW, Kearns LS, Jamieson RV, Williamson KA, van H,V, Mackey DA. PAX6 mutations may be associated with high myopia. Ophthalmic Genet. 2007;28:179–182. doi: 10.1080/13816810701356676. [DOI] [PubMed] [Google Scholar]
- Tsai JH, Freeman JM, Chan CC, et al. A progressive anterior fibrosis syndrome in patients with postsurgical congenital aniridia. Am J Ophthalmol. 2005;140:1075–1079. doi: 10.1016/j.ajo.2005.07.035. [DOI] [PubMed] [Google Scholar]
- Sisodiya SM, Free SL, Williamson KA, et al. PAX6 haploinsufficiency causes cerebral malformation and olfactory dysfunction in humans. Nat Genet. 2001;28:214–216. doi: 10.1038/90042. [DOI] [PubMed] [Google Scholar]
- Mitchell TN, Free SL, Williamson KA, et al. Polymicrogyria and absence of pineal gland due to PAX6 mutation. Ann Neurol. 2003;53:658–663. doi: 10.1002/ana.10576. [DOI] [PubMed] [Google Scholar]
- Bamiou DE, Free SL, Sisodiya SM, et al. Auditory interhemispheric transfer deficits, hearing difficulties, and brain magnetic resonance imaging abnormalities in children with congenital aniridia due to PAX6 mutations. Arch Pediatr Adolesc Med. 2007;161:463–469. doi: 10.1001/archpedi.161.5.463. [DOI] [PubMed] [Google Scholar]
- Thompson PJ, Mitchell TN, Free SL, et al. Cognitive functioning in humans with mutations of the PAX6 gene. Neurology. 2004;62:1216–1218. doi: 10.1212/01.wnl.0000118298.81140.62. [DOI] [PubMed] [Google Scholar]
- Malandrini A, Mari F, Palmeri S, et al. PAX6 mutation in a family with aniridia, congenital ptosis, and mental retardation. Clin Genet. 2001;60:151–154. doi: 10.1034/j.1399-0004.2001.600210.x. [DOI] [PubMed] [Google Scholar]
- Heyman I, Frampton I, van Heyningen V, et al. Psychiatric disorder and cognitive function in a family with an inherited novel mutation of the developmental control gene PAX6. Psychiatr Genet. 1999;9:85–90. doi: 10.1097/00041444-199906000-00006. [DOI] [PubMed] [Google Scholar]
- Crolla JA, van Heyningen V. Frequent chromosome aberrations revealed by molecular cytogenetic studies in patients with aniridia. Am J Hum Genet. 2002;71:1138–1149. doi: 10.1086/344396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Heyningen V, Hoovers JM, de KJ, Crolla JA. Raised risk of Wilms tumour in patients with aniridia and submicroscopic WT1 deletion. J Med Genet. 2007;44:787–790. doi: 10.1136/jmg.2007.051318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslow NE, Norris R, Norkool PA, et al. Characteristics and outcomes of children with the Wilms tumor-Aniridia syndrome: a report from the National Wilms Tumor Study Group. J Clin Oncol. 2003;21:4579–4585. doi: 10.1200/JCO.2003.06.096. [DOI] [PubMed] [Google Scholar]
- Breslow NE, Collins AJ, Ritchey ML, Grigoriev YA, Peterson SM, Green DM. End stage renal disease in patients with Wilms tumor: results from the National Wilms Tumor Study Group and the United States Renal Data System. J Urol. 2005;174:1972–1975. doi: 10.1097/01.ju.0000176800.00994.3a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu S, Han JC, Morales A, Menzie CM, Williams K, Fan YS. Characterization of 11p14-p12 deletion in WAGR syndrome by array CGH for identifying genes contributing to mental retardation and autism. Cytogenet Genome Res. 2008;122:181–187. doi: 10.1159/000172086. [DOI] [PubMed] [Google Scholar]
- Han JC, Liu QR, Jones M, et al. Brain-derived neurotrophic factor and obesity in the WAGR syndrome. N Engl J Med. 2008;359:918–927. doi: 10.1056/NEJMoa0801119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson DO, Howarth RJ, Williamson KA, van Heyningen V, Beal SJ, Crolla JA. Genetic analysis of chromosome 11p13 and the PAX6 gene in a series of 125 cases referred with aniridia. Am J Med Genet A. 2008;146A:558–569. doi: 10.1002/ajmg.a.32209. [DOI] [PubMed] [Google Scholar]
- van Heyningen V, Williamson KA. PAX6 in sensory development. Hum Mol Genet. 2002;11:1161–1167. doi: 10.1093/hmg/11.10.1161. [DOI] [PubMed] [Google Scholar]
- Simpson TI, Price DJ. Pax6; a pleiotropic player in development. Bioessays. 2002;24:1041–1051. doi: 10.1002/bies.10174. [DOI] [PubMed] [Google Scholar]
- Vincent MC, Pujo AL, Olivier D, Calvas P. Screening for PAX6 gene mutations is consistent with haploinsufficiency as the main mechanism leading to various ocular defects. Eur J Hum Genet. 2003;11:163–169. doi: 10.1038/sj.ejhg.5200940. [DOI] [PubMed] [Google Scholar]
- Tzoulaki I, White IM, Hanson IM. PAX6 mutations: genotype-phenotype correlations. BMC Genet. 2005;6:27. doi: 10.1186/1471-2156-6-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redeker EJ, de Visser AS, Bergen AA, Mannens MM. Multiplex ligation-dependent probe amplification (MLPA) enhances the molecular diagnosis of aniridia and related disorders. Mol Vis. 2008;14:836–840. [PMC free article] [PubMed] [Google Scholar]
- Bhuvanagiri M, Schlitter AM, Hentze MW, Kulozik AE. NMD:RNA biology meets human genetic medicine. Biochem J. 2010;430:365–377. doi: 10.1042/BJ20100699. [DOI] [PubMed] [Google Scholar]
- Aggarwal S, Jinda W, Limwongse C, Atchaneeyasakul LO, Phadke SR. Run-on mutation in the PAX6 gene and chorioretinal degeneration in autosomal dominant aniridia. Mol Vis. 2011;17:1305–1309. [PMC free article] [PubMed] [Google Scholar]
- Hanson IM, Fletcher JM, Jordan T, et al. Mutations at the PAX6 locus are found in heterogeneous anterior segment malformations including Peters' anomaly. Nat Genet. 1994;6:168–173. doi: 10.1038/ng0294-168. [DOI] [PubMed] [Google Scholar]
- Azuma N, Yamaguchi Y, Handa H, et al. Mutations of the PAX6 gene detected in patients with a variety of optic-nerve malformations. Am J Hum Genet. 2003;72:1565–1570. doi: 10.1086/375555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanson I, Churchill A, Love J, et al. Missense mutations in the most ancient residues of the PAX6 paired domain underlie a spectrum of human congenital eye malformations. Hum Mol Genet. 1999;8:165–172. doi: 10.1093/hmg/8.2.165. [DOI] [PubMed] [Google Scholar]
- Alibes A, Nadra AD, De MF, Bulyk ML, Serrano L, Stricher F. Using protein design algorithms to understand the molecular basis of disease caused by protein-DNA interactions: the Pax6 example. Nucleic Acids Res. 2010;38:7422–7431. doi: 10.1093/nar/gkq683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glaser T, Jepeal L, Edwards JG, Young SR, Favor J, Maas RL. PAX6 gene dosage effect in a family with congenital cataracts, aniridia, anophthalmia and central nervous system defects. Nat Genet. 1994;7:463–471. doi: 10.1038/ng0894-463. [DOI] [PubMed] [Google Scholar]
- Schmidt-Sidor B, Szymanska K, Williamson K, et al. Malformations of the brain in two fetuses with a compound heterozygosity for two PAX6 mutations. Folia Neuropathol. 2009;47:372–382. [PubMed] [Google Scholar]
- Solomon BD, Pineda-Alvarez DE, Balog JZ, et al. Compound heterozygosity for mutations in PAX6 in a patient with complex brain anomaly, neonatal diabetes mellitus, and microophthalmia. Am J Med Genet A. 2009;149A:2543–2546. doi: 10.1002/ajmg.a.33081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleinjan DA, Seawright A, Mella S, et al. Long-range downstream enhancers are essential for Pax6 expression. Dev Biol. 2006;299:563–581. doi: 10.1016/j.ydbio.2006.08.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ticho BH, Hilchie-Schmidt C, Egel RT, Traboulsi EI, Howarth RJ, Robinson D. Ocular findings in Gillespie-like syndrome: association with a new PAX6 mutation. Ophthalmic Genet. 2006;27:145–149. doi: 10.1080/13816810600976897. [DOI] [PubMed] [Google Scholar]
- Graziano C, D'Elia AV, Mazzanti L, et al. A de novo nonsense mutation of PAX6 gene in a patient with aniridia, ataxia, and mental retardation. Am J Med Genet A. 2007;143A:1802–1805. doi: 10.1002/ajmg.a.31808. [DOI] [PubMed] [Google Scholar]
- Perveen R, Lloyd IC, Clayton-Smith J, et al. Phenotypic variability and asymmetry of Rieger syndrome associated with PITX2 mutations. Invest Ophthalmol Vis Sci. 2000;41:2456–2460. [PubMed] [Google Scholar]
- Khan AO, Aldahmesh MA, Al-Amri A. Heterozygous FOXC1 mutation (M161K) associated with congenital glaucoma and aniridia in an infant and a milder phenotype in her mother. Ophthalmic Genet. 2008;29:67–71. doi: 10.1080/13816810801908152. [DOI] [PubMed] [Google Scholar]
- Ito YA, Footz TK, Berry FB, et al. Severe molecular defects of a novel FOXC1 W152G mutation result in aniridia. Invest Ophthalmol Vis Sci. 2009;50:3573–3579. doi: 10.1167/iovs.08-3032. [DOI] [PubMed] [Google Scholar]
- Semina EV, Ferrell RE, Mintz-Hittner HA, et al. A novel homeobox gene PITX3 is mutated in families with autosomal-dominant cataracts and ASMD. Nat Genet. 1998;19:167–170. doi: 10.1038/527. [DOI] [PubMed] [Google Scholar]
- Tumer Z, Bach-Holm D. Axenfeld-Rieger syndrome and spectrum of PITX2 and FOXC1 mutations. Eur J Hum Genet. 2009;17:1527–1539. doi: 10.1038/ejhg.2009.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas MG, Kumar A, Mohammad S, et al. Structural grading of foveal hypoplasia using spectral-domain optical coherence tomography a predictor of visual acuity. Ophthalmology. 2011;118:1653–1660. doi: 10.1016/j.ophtha.2011.01.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fantes JA, Bickmore WA, Fletcher JM, Ballesta F, Hanson IM, van Heyningen V. Submicroscopic deletions at the WAGR locus, revealed by nonradioactive in situ hybridization. Am J Hum Genet. 1992;51:1286–1294. [PMC free article] [PubMed] [Google Scholar]
- Nicholson HS, Blask AN, Markle BM, Reaman GH, Byrne J. Uterine anomalies in Wilms' tumor survivors. Cancer. 1996;78:887–891. doi: 10.1002/(SICI)1097-0142(19960815)78:4<887::AID-CNCR28>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- Slade I, Stephens P, Douglas J, et al. Constitutional translocation breakpoint mapping by genome-wide paired-end sequencing identifies HACE1 as a putative Wilms tumour susceptibility gene. J Med Genet. 2010;47:342–347. doi: 10.1136/jmg.2009.072983. [DOI] [PubMed] [Google Scholar]
- Hormozdiari F, Hajirasouliha I, McPherson A, Eichler EE, Sahinalp SC. Simultaneous structural variation discovery among multiple paired-end sequenced genomes. Genome Res. 2011;21:2203–2212. doi: 10.1101/gr.120501.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nowakowska BA, de Leeuw N, Ruivenkamp CA, et al. Parental insertional balanced translocations are an important cause of apparently de novo CNVs in patients with developmental anomalies. Eur J Hum Genet. 2012;20:166–170. doi: 10.1038/ejhg.2011.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolan M, Berry SA, Rubin KR, Hirsch B. Deletion and duplication of 11p13-11p14: reciprocal aberrations derived from a paternal insertion. Am J Med Genet A. 2011;155A:2775–2783. doi: 10.1002/ajmg.a.34232. [DOI] [PubMed] [Google Scholar]
- Le Caignec C, Delnatte C, Vermeesch JR, et al. Complete sex reversal in a WAGR syndrome patient. Am J Med Genet A. 2007;143A:2692–2695. doi: 10.1002/ajmg.a.31997. [DOI] [PubMed] [Google Scholar]
- Clericuzio C, Hingorani M, Crolla JA, van H, Verloes V. A. Clinical utility gene card for: WAGR syndrome. Eur J Hum Genet. 2011. p. 19. [DOI] [PMC free article] [PubMed]
- Churchill AJ, Hanson IM, Markham AF. Prenatal diagnosis of aniridia. Ophthalmology. 2000;107:1153–1156. doi: 10.1016/s0161-6420(00)00093-2. [DOI] [PubMed] [Google Scholar]