Abstract
Compromised respiratory sinus arrhythmia (RSA, i.e., low cardiac vagal control) frequently characterizes clinically depressed adults and also has been detected in infants of depressed mothers; however, its existence has not been established in older at-risk offspring. We investigated developmental patterns of RSA in a sample of 163 5-14 year-old children, who were either at high risk for depression (due to having a parent with a childhood-onset mood disorder) or low-risk for depression. We hypothesized that high-risk children have lower resting RSA than do low-risk children, which could reflect atypical developmental trajectories. Children's RSA was assessed during resting baseline periods on multiple occasions, typically one-year apart. Linear growth modeling indicated a group by age interaction. Low-risk children (but not the high-risk children) exhibited a significantly increasing trajectory in resting RSA with age. Mood disorders in offspring did not account for the Group X Age interaction effect. Our study provides new evidence that children at high risk for depression have an atypical developmental trajectory of RSA across late childhood.
Keywords: respiratory sinus arrhythmia, vagal tone, depression, risk, developmental, children, adolescents
Low respiratory sinus arrhythmia (RSA) is often found in clinically depressed adults (see Rottenberg, 2007, for a review). Such findings could signify that low resting RSA covaries with clinical depression, or that it predates the disorder and is a vulnerability factor for it. Consistent with the latter possibility, lower resting RSA has been detected in the infants of depressed mothers as compared to infants of control mothers (see Field & Diego, 2008). To our knowledge however, low resting RSA has not been documented in older children with a parental history of depression. In the present study, we tested the hypothesis that offspring (spanning from middle childhood to early adolescence) of parents with childhood-onset mood disorder (COMD) have lower resting RSA than do offspring of comparison parents.
RSA is the beat-to-beat variability in heart rate that is synchronized with the breathing cycle, such that heart rate accelerates during inspiration, and decelerates with expiration. RSA is indexed by measuring this high-frequency heart rate variability, which is considered to reflect vagal influence on the heart (e.g., Berntson et al., 1997; Porges, 1995; Porges, Doussard-Roosevelt, Portales, & Greenspan, 1996). Specifically, the myelinated branch of the vagus nerve, which originates in the nucleus ambiguus and ends on the sino-atrial node in the heart, affects patterns of heart rate (Porges, 2007). During resting conditions, higher RSA is generally considered adaptive as it reflects resource conservation (e.g., heart rate is slowed). According to Porges (e.g., Porges, 2007; Porges, et al., 1996), under resting conditions higher cardiac vagal control serves as a brake and inhibits cardiovascular arousal. However, as environmental demands increase, this brake is removed (i.e., vagal withdrawal), enabling the individual to respond flexibly to situational demands with, for example, increased sympathetic activity.
RSA and Depression
While the association between depression and compromised RSA has not yet been verified in children, low RSA is reliably associated with a current diagnosis of major depressive disorder in adults, with a modest effect size (Licht, et al., 2008; see Rottenberg, 2007 for a quantitative review and discussion of factors that influence effect size estimates). Furthermore, with adults, there is some evidence that changes in RSA may co-occur with changes in depression. For example, individuals whose depressive symptoms decrease in response to pharmacotherapy, acupuncture, or cognitive-behavioral therapy exhibit concurrent increases in RSA (Balogh, Fitzpatrick, Hendricks, & Paige, 1993; Carney, Freedland, Stein, Skala, Hoffman, & Jaffe, 2000; Chambers & Allen, 2002). However, the research on adult depression and RSA has sometimes resulted in nonsignificant or contradictory findings (e.g., Bosch, Riese, Ormel, Verhulst, & Oldehinkel, 2009; Rottenberg, Wilhelm, Gross, & Gotlib, 2002), possibly because investigators have often been inattentive to potential confounds which can inflate effect sizes (e.g., medication, body weight).
Another issue has been the causal relationship between RSA and episodes of depression: is low RSA a precursor of depression or simply a correlate of the depressed state? One way to address this issue is to examine RSA in children who are at high risk for, but have not yet developed a depressive disorder. High risk can be defined as the presence of elevated depression symptoms (e.g., Keenan et al., 2008; Kovacs & Lopez-Duran, 2010). But there is only indirect evidence that lower RSA and higher symptom levels may be associated; namely, low RSA children who were exposed to stressors developed more internalizing symptoms than did high RSA peers (e.g., El-Sheikh, 2005a; El-Sheikh, Harger, & Whitson, 2001).
High depression risk also can be conferred by having a positive family history of depression. It has been shown that high-risk infants (i.e., those whose mothers had depression during pregnancy or postpartum) have lower vagal tone than do infants of nondepressed mothers (Field, Healy, Goldstein, & Perry, 1988; Field et al., 2004; Jones, Field, Fox, Davalos, Lundy, & Hart, 1998). Further, infants of depressed mothers do not show the normative vagal tone increase from 3 to 6 months that are evident in infants of nondepressed mothers (Field, Pickens, Fox, Nawrocki, et al., 1995). However, associations between at-risk status and compromised RSA in children beyond the infancy period have not been detected. For example, Ashman, Dawson, and Panagiotides (2008) found that 6 year-olds who had a mother with a history of depression (at some point since the child's birth) did not differ from children of nondepressed mothers in their level of resting RSA.
Notably, reports of children's RSA and depression-risk have concerned the relationship of RSA and indices of functioning within high-risk offspring. For instance, Forbes, Fox, Cohn, Galles, and Kovacs (2006) found that lower resting RSA was linked to higher internalizing symptoms among 3-9 year old offspring of parents with COMD, but not among comparison offspring. Similarly, Shannon, Beauchaine, Brenner, Neuhaus, and Gatzke-Kopp (2007) found that higher resting RSA might protect 8-12 year old children against elevated depressive symptoms when their mothers have melancholic symptoms. Finally, preschoolers with higher resting RSA, whose mothers reported clinical levels of depressive symptoms, did not show increases in emotion regulation by age 7 years that other children did (Blandon, Calkins, Keane, & O'Brien, 2008). Overall, the limited and inconsistent evidence for group-level differences in RSA in children also raises the possibility that the link between RSA and depression risk may be moderated by various factors.
RSA and Children's Age
Age is among the most important potential moderator variables in studies of RSA in youth. As mentioned, infants of depressed mothers do not show the normative vagal tone increase from 3 to 6 months (Field, et al., 1995). Age also may affect the link between RSA and behavior (oppositional defiant/conduct, or attention deficit hyperactivity) disorders. Specifically, children with behavioral disorders in middle childhood had lower resting RSA compared to control youth, while RSA differences were absent in preschoolers (Beauchaine, Gatzke-Kopp, & Mead, 2007). Possibly, abnormalities in RSA among at-risk children may only be evident at certain ages, perhaps when the nervous system is undergoing relatively substantial development (e.g., early in infancy, Pereyra, Zhang, Schmidt, & Becker, 1992) or when mastery of self-regulatory skills is especially important (e.g., in mid-late childhood).
The present study adds to the limited body of research on RSA and age effects during the childhood and adolescence period. One longitudinal study found that the mean-level of resting RSA increased across the age span from 4.5 to 7 years (Marshall and Stevenson-Hinde, 1998), whereas another study of 8-17 year olds found no difference across two time points (Salomon, 2005). Cross-sectional studies similarly found that age is positively associated with resting HF-HRV across childhood (Galeev, Igisheva, & Kazin, 2002; Kazuma, Otsuka, Wakamatsu, Shirase, & Matsuoka, 2002; Massin & von Bernuth, 1997; Silvetti, Drago, & Ragonese, 2001) or that children between 6 -15 years of age have higher HF-HRV compared to younger children (Pikkujämsä et al., 1999; though for exceptions see Finley & Nugent, 1995 and Goto et al., 1997). A recent study with 8 year olds followed up at ages 9 and 10 years indicated that age effects were moderated by race in that European American children showed an increase in resting RSA with age, whereas African-American children had higher RSA at age 8 but no change with age (Hinnant, Elmore-Staton, & El-Sheikh, 2011). The overall pattern of findings may suggest that resting RSA increases across early childhood but that by late childhood there is more inter-individual variability in how RSA changes. We can investigate this possibility in the current study as one aspect of comparing children at high and low risk for depression.
RSA and Children's Sex
Children's sex also may moderate group differences in RSA. In adults, the association between RSA and depression varies by sex, with depressed men but not women showing lower resting heart rate variability (Thayer, Smith, Rossy, Sollers, & Friedman, 1998). No comparable information exists for children who have a depression history or a high future risk for developing depression. However, there are indications that RSA relates differently to emotional responses or adjustment for boys and girls (e.g., Eisenberg, Fabes, Murphy, Maszk, Smith, & Karbon, 1995), and that boys and girls vary in mean levels of RSA in childhood or adolescence (Allen & Matthews, 1997; Ashman, et al., 2008; El-Sheikh, 2005b). Thus we tested for sex differences in RSA and examined whether RSA differences between high- and low-risk children vary by children's sex.
The Present Study and Hypotheses
The main goal of the study was to determine whether high-risk offspring (whose parent had COMD) exhibit lower resting RSA than low-risk comparison offspring (whose parents did not have a history of major psychopathology). Because of the availability of multiple assessments for most children, we were able to test the hypothesis, namely, that high-risk children may show an atypical trajectory of resting RSA. We examined children's sex as a potential moderator because it may be the case that the group effect is detectable only in boys or girls. Finally, given that the high-risk children are more likely to have diagnosed psychiatric disorders, we investigated whether the presence of a mood disorder could account for any difference between high- and low-risk children's level of RSA at rest.
Method
Sample
Our sample included 163 children (88 boys and 75 girls) who had completed at least one psychophysiology assessment between the ages of 5 and 14 years of age. There were 107 high-risk offspring (78 had a parent with unipolar depression disorder and 29 had a parent with bipolar disorder) and 56 low-risk offspring. The children's age ranged from 4.69 to 13.62 years at their first appointment. Children with 2 or more assessments were 5.86 to 14.17 years of age at their last appointment. Most children had multiple assessments across the years (M = 2.16) for a total of 352 appointments. Specifically, 49 children had one assessment, 53 had two, 47 had three, and 14 had four assessments. The racial distribution of this sample was 56% White, 22% African-American, 18% Biracial, 1% Asian, and 4% other.
At the psychophysiology assessment, parents reported on children's current medication at 242 appointments. No child was taking an anti-depressant, and six children (all high-risk) were taking a psychostimulant. Psychostimulant use was unrelated to levels of resting RSA, t (1, 157) = .90, p = .370 and thus we do not consider it further. Also, we calculated children's body-mass index (BMI) from their height and weight measured on the day of their psychophysiology session. Using children's BMI from their last appointment, we found that high-risk (M = 18.69, SD = 3.96) and low-risk children (M = 18.12, SD = 4.41) did not differ on BMI, t (149) = -.81, p = .42, and that BMI was not significantly correlated with resting RSA levels, r (149) = -.09, p = .30. Our reported results below therefore do not include BMI as a covariate.
Procedure and measures
Recruitment and case ascertainment of parents
The children in the sample are offspring of adult participants in a Program Project; the parents either were diagnosed with a COMD (probands) or were control subjects. COMD was operationally defined as onset of depression (MDD and/or dysthymic disorder) before age 15 or bipolar spectrum (bipolar I or II or cyclothymic disorder) before age 18. Also, to be included in the study, participants had to be free of preexisting major systemic medical disorders, and without evidence of mental retardation. Trained professional-level clinical evaluators from the Psychiatric Evaluation Core of the program project conducted the diagnostic interviews. Clinicians’ assessments were then evaluated by independent psychiatrists to verify diagnostic status. Diagnoses were based on rules specified in the DSM (DSM-III, DSM-IV; American Psychiatric Association, 1980, 1994).
Adult COMD participants were recruited for the program project in multiple ways: by accessing individuals who had participated in clinical research when they were children, through adult mental health clinics, or by advertising in the general community. A portion had been enrolled in a longitudinal, naturalistic follow-up study of childhood-onset depression when they were young (Kovacs, Feinberg, Crouse-Novak, Paulauskas, & Finkelstein, 1984; Kovacs, Obrosky, Gatsonis, & Richards, 1997). During childhood and adolescence, their diagnoses were based on the Interview Schedule for Children and Adolescents or its Young Adult version administered separately to the child and one parent (Sherrill & Kovacs, 2000). During adulthood, participants were assessed via the Structured Clinical Interview for DSM-IV Axis I disorders (SCID, First, Spitzer, Gibbon, & Williams, 1995), which was modified to include a few childhood-onset and Axis II disorders. A second informant (e.g., parent or partner) also was interviewed. Participants recruited as adults from other research studies, clinics, or the community also were given the SCID; second informants and pediatric medical records served to document mood problems in childhood.
At intake, control participants had to be free of any lifetime major psychiatric disorder. Controls also were recruited in various ways: from other studies during childhood or adolescence wherein they served as ‘normal controls’, by using the Cole directory to target neighborhoods matching probands’ socioeconomic status, or through community advertisements (e.g., at a Women, Infants, and Children Center).
Children's psychiatric assessment
Children aged seven years and older also received direct psychiatric examinations at yearly intervals; those below this age (n = 20) are generally considered too young for a direct psychiatric examination and thus were excluded from analyses examining children's mood disorders. As part of the psychiatric assessment, the parent and child were separately interviewed about the child using the “Kiddie” version of the Schedule for Affective Disorders and Schizophrenia, Lifetime (K-SADS-PL). This semi-structured interview yields diagnoses of current and past episodes of disorders according to DSM criteria (DSM-IV; American Psychiatric Association, 1994), and has established reliability and validity (Kaufman, Birmaher, Brent, & Rao, 1997). Interviewers’ ratings and diagnoses were subsequently reviewed by independent psychiatrists using the “best-estimate” diagnostic procedure. For this paper, we focused on mood disorders that included major depressive disorder, dysthymic disorder, depressive disorder not otherwise specified (NOS), and bipolar NOS. In this sample, 10 children had a lifetime diagnosis of a mood disorder.
Children's psychophysiological assessment
At all study appointments, children participated in a multi-component psychophysiological assessment (only some of these data are reported herein). The protocol included a series of behavioral tasks (which varied slightly by child age and the number of previous assessments) that were interspersed with 1-minute inter-task intervals. Electrocardiogram (ECG) data were collected across the entire protocol. Each session started with an approximately 30-minute period during which experimenters fastened electrodes to children's chest, head, and face (for the acquisition of data on electroencephalographic [EEG] and facial electromyographic activity). During this hook-up period, children were given a variety of distractors (e.g., videogames, toys) and completed questionnaires. Children's weight and height measurements also were obtained at the session.
In this paper, we report on RSA determined during the resting baseline period that occurred at the beginning of every psychophysiology protocol. The periods were divided into six alternating segments. In each segment, children were asked to either keep their eyes closed or to open their eyes and focus on a toy spaceship being held by an experimenter or on an object on a computer screen. The baseline was 3 minutes in length (with 30-second segments) most of the time, although in one age-specific protocol (completed by some 10-13 year olds), the baseline was 6 minutes (with 1-minute alternating segments).1 All resting RSA scores were computed by averaging the six RSA scores for the baseline segments. The mean for the eyes-open baseline (M = 7.03, SD = 1.14) was significantly higher than for the eyes-closed baseline (M = 6.92, SD = 1.15), t (344) = 2.84, p < .01. However, because all children had the same proportion of eyes-open and closed segments, these would not impact our current investigation. The alternating eyes open and closed sequence was used to meet standards of resting baselines for EEG data acquisition.
ECG of child participants was recorded using electrodes placed on children's rib cage at heart level. Data were recorded and processed using software/equipment from James Long Company (Caroga Lake, NY). A bandpass filter of .01 – 1000 Hz was used and the data were amplified by a gain of 500. The signal was digitized with a sampling rate of 512 Hz (Berntson et al., 1997), and was re-sampled offline at 1000 Hz. The processing of ECG data off-line involved a multi-pass algorithm to detect R-waves. Data were later manually checked for missed R-waves or peaks misidentified as R-waves. The times between R-waves were converted to interbeat intervals (IBIs) and resampled into equal time intervals of 125 ms. Prorated IBI values were saved for an analysis of the mean and variance of heart period as well as for further processing. Using the James Long software program, a 30-second cubic polynomial was used to detrend the prorated IBI data. Data were tapered with a Hanning window. For the present study, RSA was computed using Fast Fourier transform analysis within the .15 - .50 Hz frequency band for the 6-14 year olds and in the .20 – 1.00 Hz range for the 4-5 year olds.2 These ranges reflect high frequency heart rate variability that is within the range of likely respiration for children in these age ranges (9 to 30 breaths per minute for the older group, and 12 to 60 breaths per minute for the younger group; see Bar-Haim, Marshall, & Fox, 2000; Marshall & Stevenson-Hinde, 1998). Note however that researchers also have used a wider band of .12 – 1.00 Hz to quantify RSA across a wide age range of youth (e.g., Bal et al., 2010; Van Hecke et al., 2009). Power scores were log-transformed to normalize the distribution. In Table 1, we report IBI values in ms and RSA in log [ms2] for each age and group.
Table 1.
Descriptive Information for Resting IBI (Interbeat interval), RSA (Respiratory Sinus Arrhythymia), and Lifetime History of Mood Disorder by Children's Age
| Age | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 |
|---|---|---|---|---|---|---|---|---|---|---|
| Low Risk | ||||||||||
| N | 25 | 14 | 26 | 23 | 11 | 8 | 8 | 7 | 1 | 2 |
| IBI (ms) | ||||||||||
| Mean | .61 | .62 | .69 | .68 | .75 | .69 | .73 | .83 | .61 | .92 |
| SD | .06 | .04 | .07 | .09 | .08 | .08 | .07 | .11 | - | .18 |
| RSA (log ms2) | ||||||||||
| Mean | 6.85 | 6.41 | 7.32 | 6.94 | 7.76 | 6.83 | 7.12 | 7.37 | 6.04 | 7.94 |
| SD | 1.18 | .71 | .92 | .93 | 1.03 | 1.27 | .82 | .80 | - | .98 |
| High Risk | ||||||||||
| N | 37 | 25 | 40 | 29 | 21 | 17 | 11 | 22 | 11 | 4 |
| IBI (ms) | ||||||||||
| Mean | .59 | .67 | .68 | .69 | .68 | .71 | .68 | .74 | .69 | .73 |
| SD | .06 | .12 | .09 | .10 | .06 | .12 | .07 | .10 | .09 | .12 |
| RSA (log ms2) | ||||||||||
| Mean | 6.61 | 7.25 | 7.30 | 7.16 | 6.90 | 7.07 | 6.84 | 7.15 | 6.06 | 6.37 |
| SD | 1.10 | 1.11 | .97 | 1.30 | .74 | 1.06 | 1.17 | 1.05 | 1.43 | 1.28 |
| Mood disorder | ||||||||||
| n | 1 | 1 | 1 | 1 | 3 | 0 | 2 | 6 | 2 | 0 |
| % | 2.7% | 4.0% | 2.4% | 3.6% | 15.0% | 0% | 20.0% | 30.0% | 25.0% | 0% |
Note. For descriptive purposes, children's age was rounded to the nearest integer. Children with multiple assessments are represented in multiple columns. No child in the low-risk group had a diagnosed mood disorder.
Analyses
We sought to model resting RSA as the dependent variable, with children's parental group (high-risk vs. low-risk), sex, and age (centered at the age of 10 years, so that parameters could easily be interpreted) as predictors. We fit an unconditional linear growth model of annual assessments of resting RSA, which allowed us to determine if high-risk and low-risk youth had different mean slopes or intercepts (fixed effects), or if individual or family-specific variation in slope or intercept (random effect after accounting for fixed effects) was significantly different across the groups. This model accommodates the staggered ages at which children entered and left the study and the repeated measures (up to 4) on children, and although children with a single appointment contribute less to the results than those with multiple appointments, all participants’ data can be retained in these analyses (Luke, 2004).
In a linear growth model, each individual is assumed to have his or her own growth curve with parameters (in our case, intercept and slope random effects per child and per family) that vary from the population mean. This allows inferences about the mean trajectory in the two groups and also about differential variation from that mean. We used the maximum likelihood method to estimate model parameters; in so doing we could evaluate model fit by comparing Akaike's information criterion (AIC) of the full model to models without specific fixed effects. We tested the models using the covariance structure of compound symmetry to account for within-subject variation. Finally, we examined whether a history of mood disorder could account for any significant difference in resting levels of RSA between high and low risk children. The SAS program, PROC MIXED, was used, following examples of unconditional growth curve models (DeLucia & Pitts, 2006).
Results
Preliminary Analyses
Table 1 presents descriptive information about the physiological variables (resting IBI, RSA) as well as rates of mood disorder by chronological age. Specifically, 11.6% of high-risk children had a lifetime history of a mood disorder by the time of their last psychophysiology appointment (n = 10) whereas no low-risk children were diagnosed with a mood disorder, χ2 (1, N = 137) = 6.40, p < 0.05.
In Table 2, we reported Spearman Rho correlations for children by age. Only children who had another appointment within 2 rounded years were included so that the estimate of inter-individual stability is more comparable to other studies’ results with similarly aged samples (Hinnant et al., 2010; El-Sheikh, 2005b; Salomon, 2005). Significant correlations for children aged 5, 6, and 9 years indicated some stability in resting RSA. However, because the group sizes were quite small and tended to decrease with child age, these values must be interpreted cautiously.
Table 2.
Spearman Rho correlations for Respiratory Sinus Arrhythmia by children's age by integer and only including those with an appointment within the next 2 years (rounded)
| Age | 5-7 | 6-8 | 7-9 | 8-10 | 9-11 | 10-12 | 11-13 | 12-14 |
|---|---|---|---|---|---|---|---|---|
| N with a second assessment | 24 | 28 | 30 | 19 | 13 | 8 | 11 | 10 |
| Spearman rho | .57** | .38* | .08 | .26 | .58* | .05 | -.32 | .10 |
Linear Mixed Models
To test our hypothesis that high-risk and low-risk children differ in their resting RSA and that the group effect would be moderated by children's sex or age, we used all available RSA data from the initial resting baseline for children aged 4.5 years onward. The initial model included children's sex but we found that boys and girls did not differ significantly in resting RSA (F (1, 15) = 0.22, p = 0.644), nor did sex interact with child group (F (1, 15) = 2.55, p = 0.131) or age (F (1, 222) = 0.83, p = 0.363). Thus, children's sex was not included as a predictor variable in the final model.
As shown in Table 3, the final, full factorial model (Model 1) indicated a fixed effect of group, no overall age effect, and a significant Age X Group interaction. Examination of fixed-effect coefficients by group showed a higher intercept (at age 10) in the low risk than in the high risk group (B = 7.319, SE = 0.132 vs. B = 6.972, SE = 0.112) and a positive slope in the low-risk group (B = 0.102, SE = 0.039) that significantly increased with age, t (226) = 2.59, p < .05. However, the slope in the high-risk group (B = -.004, SE = .032) was not significantly different from zero, t (226) = -.11, p = .909. In other words, high-risk children had lower RSA than low-risk children, and while RSA increased in low-risk children with age, this effect was not evident in the high-risk offspring.3
Table 3.
Modeling Developmental Trends in Respiratory Sinus Arrhythmia in Children at High- and Low-Familial Risk for Mood Disorder
|
Model 1 (N = 163) |
Model 2 (N = 143) |
|||
|---|---|---|---|---|
| Parameter | Coefficient (SE) | t-value | Coefficient (SE) | t-value |
| Intercept (high risk, age 10) | 6.972 (.112) | 62.37*** | 7.121 (.319) | 22.30*** |
| Child's parental group | .346 (.173) | 2.00* | .370 (.180) | 2.06* |
| Child's age (change per year) | -.004 (.032) | -0.11 | .004 (.036) | 0.10 |
| Group × Age | .105 (.050) | 2.08* | .102 (.054) | 1.87+ |
| Depressive disorder (lifetime) | --- | --- | -.182 (.339) | -0.54 |
Coefficients reflect parameter estimates for fixed effects in the models. SE= Standard Error. Because the reference group is the high-risk group, the intercept and age parameters reflect this group. The Group and Group × Age effects reflect the difference for the low risk group.
p = .063.
p < .05.
p < .001.
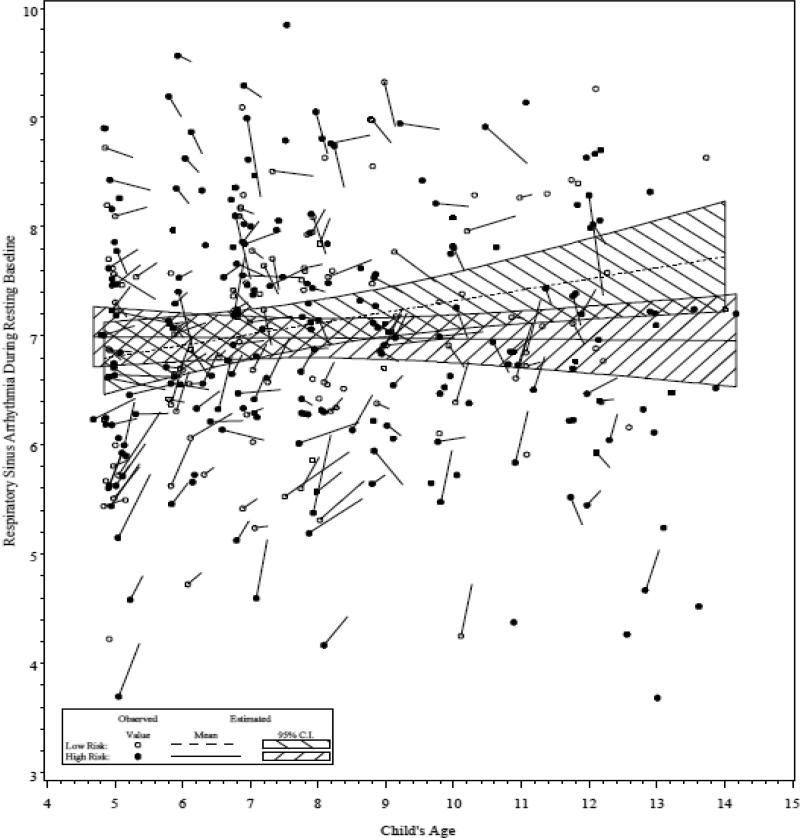
Examining fitted curves (see Figure 1) of the mean model for each group reveals overlap of 95% confidence intervals across ages (with resting RSA slightly but not significantly higher in COMD children at age 5, and identical in both groups at age 6) and divergence in adolescence (with estimated mean RSA lower in the high risk group after age 10). A slight overlap of confidence intervals at the age of 10 years and older is consistent with a statistically significant difference in means at p < 0.05 (Schenker & Gentleman, 2001).
Figure 1.
Respiratory Sinus Arrhythmia in Children at High- and Low-Familial Risk for Mood Disorders by Children's Age
Note. Means are estimates from a linear growth curve model accounting for family-level and child-level variability; vectors from points lead to the next measurement in the same child.
We then examined if children's mood disorder history could account for the group by age effect on RSA. Model 2 (see Table 3) includes a variable indicating whether a child had a mood disorder diagnosis by the time of each particular psychophysiology session. Results showed that while mood disorder history was unrelated to resting RSA, the group effect remained significant, but the Group X Age interaction dropped in significance to p = .063. The slope for low-risk youth remained significantly positive (B = 0.105, SE = 0.041), t (217) = 2.55, p < .05, and close to zero for high-risk youth (B = 0.004, SE = 0.036), t (217) = .10, p = .920. Overall, given that children's history of mood disorder was not associated with resting RSA and that the pattern of findings were in the same direction as our original model, these results provide preliminary evidence that the different trajectories for the high and low risk children are not attributable to children's diagnosed mood disorders.
Discussion
To our knowledge, this study is the first to document that offspring of depressed parents have different developmental trajectories of respiratory sinus arrhythmia across late childhood than do offspring of comparison parents. Our finding complements and extends previous reports that infant offspring of depressed mothers have low vagal tone (Field, et al., 2004; Jones, et al., 1998) and importantly, that they fail to show the typical developmental trend of increasing vagal tone (Field, et al., 1995). In our study, the availability of longitudinal assessments provided critical evidence that the interindividual difference between high- and low-risk youth resulted in part from intra-individual change. However, we did not find evidence that children's own mood disorders could account for the lower resting RSA by late childhood in those at higher risk for depression.
Our study indicated that RSA functioning appeared to be similar in high-risk and low-risk children in early childhood, which echoes some reports from studies of young children that failed to find compromised vagal tone among those at high depression risk. Our own earlier investigations using younger samples did not reveal any differences in resting RSA between high-risk and low-risk youth even though results indicated that lower RSA (either at rest, or in terms of less reactivity or recovery) was associated with elevated symptoms or dysfunctional emotion regulation (Forbes et al., 2006; Gentzler, Santucci, Kovacs, & Fox, 2009; Santucci, Silk, Shaw, Gentzler, Fox, & Kovacs, 2008). In light of prior findings that high-risk infants do differ from control infants with regard to RSA (Field et al., 1995), and results that high- and low-risk children are indistinguishable with regard to RSA in early childhood, it is reasonable to wonder why the groups in our study started to diverge as they got older.
One consideration of the varying chronological ages at which children's RSA differs as a function of depression risk is that there may be particular developmental periods at which children are more sensitive to external influences of stress. For example, in infancy when the nervous system is undergoing marked development (Pereyra et al., 1992), the high-risk infants of currently-depressed mothers likely experience acute stress during interactions with their mothers (Pickens & Field, 1995). In relation to our findings, children whose mothers have a history of depression also may have experienced less supportive parenting (Feng, Shaw, Skuban, & Lane, 2007; Shaw, et al., 2006). Further, children with lower resting RSA may be more susceptible to parenting influences than those with higher resting RSA (Hastings & De, 2008; Hastings, Sullivan, McShane, Coplan, Utendale, & Vyncke, 2008). However, perhaps a cumulative effect of this type of stress on RSA is more readily detectable as youth approach adolescence when perceived stress within peer and school domains may be increasing (e.g., Roeser & Eccles, 1998; Rudolph & Hammen, 1999), which could further challenge their self-regulatory skills.
We expected that children's own depressive disorders might account for a portion of the group difference in resting RSA, particularly since the group difference emerged later in childhood. Our results did indicate that mood disorders were more prevalent among high-risk children, which is consistent with our expectations and other findings (Weissman, et al., 2006). However, children's lifetime history of a mood disorder was not related to resting RSA levels. Thus, the reason that parental history of mood disorder predicts lower resting RSA in the offspring is not simply due to disorders in the offspring themselves. In our sample, however, very few children were diagnosed with a mood disorder, which is not surprising given their age (83% of the sample was younger than 11 years old). Considering that the rates of depressive disorders increase substantially by mid-adolescence (Kessler, Avenevoli, & Merikangas, 2001; Weissman, et al. 2006), determining whether lower resting RSA predicts an adolescent onset of depression is a crucial next step.
The origin of across-group differences in the developmental trajectory of resting RSA remains an important question. High-frequency heart rate variability shows moderate heritability (Dubreuil, et al., 2003; Sinnreich, Friedlander, Sapoznikov, & Kark, 1998; Snieder, Boomsma, Van Doornen, & De Geus, 1997). The group effect may be partially due to genetic transmission, though clearly there are other influences. Additional explanatory factors of the age effect could be maturational changes or physical characteristics that may not be independent of children's risk status for depression. Although one likely candidate is children's weight (Kaufman, Kaiser, Steinberger, Kelly, & Dengal, 2007), in our sample high-risk children did not have higher BMI than low-risk children, and BMI was not significantly associated with RSA. Thus, the flat developmental trajectory of RSA for youth at high risk for depression does not appear to be due to the presence of higher BMI among them as they reach adolescence.
One factor that we are unable to rule out with our data is pubertal status, which may be a consideration since a history of mood disorders in mothers may be related to earlier pubertal onset in females (Ellis & Garber, 2000). To our knowledge, however, direct effects of puberty on RSA have not been found (El-Sheikh, 2005b) even though puberty is acknowledged as an important variable to consider (e.g., Allen & Matthews, 1997; Galeev, Igisheva, & Kazin, 2002). Thus, not having pubertal status is a limitation of this study, and the relationship between puberty and RSA requires further investigation.
This study also contributes to the literature on the stability of RSA. First, our findings suggested little rank order stability in RSA over time. Specifically, a portion of the correlations reached significance, indicating moderate stability for a subset of the children at ages 5, 6, and 9 years. However, the estimates were lower and inconsistent at the other ages. Because our group sizes were small, we are cautious in making cross-age comparisons. Other researchers have found more robust stability in resting RSA (Calkins & Keane, 2004; Kennedy, Rubin, Hastings, & Maisel, 2004; Marshall & Stevenson-Hinde, 1998). For instance, El-Sheikh (2005b) reported a Spearman Rho of .36, p <.001, for baseline RSA with 9 year olds assessed two years later. Salomon (2005) and Hinnant et al. (2010), who also included youth within this middle childhood or adolescence period, report slightly higher stability estimates. However, their samples were not high risk and in fact included exclusionary criteria for all or some disorders. Thus, to the extent that we observed lower rank order stability, it may be attributable to sampling differences. Also, stability rates of resting RSA in adulthood tend to be higher (e.g., r = .74, Bornstein & Suess), which might suggest that vagal influences on the heart are more dynamic during childhood.
Second, our findings indicate that mean level stability appears to differ as a function of children's depression risk status. We found that low-risk comparison children showed a significantly increasing trajectory in resting RSA with age, whereas high-risk children had a flat trajectory that did not differ from zero across their study visits. The normative trend in RSA appears to be a linear increase across childhood (Galeev et al., 2002; Kazuma et al., 2002; Massin & von Bernuth, 1997; Pikkujämsä et al., 1999; Silvetti et al., 2001) particularly for White youth (Hinnant et al., 2011), though different methods for collecting RSA (short-term versus long-term recordings) as well as variations in ages across samples make across-study comparisons difficult (Task Force, 1996). Nevertheless, given that a positive trajectory in resting RSA was only evident in low-risk youth, the impact of parental history of depression on children's RSA across time needs to be further investigated.
Overall, our study has several notable strengths. Psychiatric disorders in parents and children were determined by clinical interviews and ratings were reviewed by independent psychiatrists, underscoring diagnostic accuracy. Also, most children completed multiple physiological assessments allowing us to examine the trajectory of resting RSA. These data would be unique in a normative sample, but are even more valuable because they include offspring of parents with a depressive or bipolar disorder. Finally, our investigation of potential confounds, such as BMI and medication, helped to address and rule out less interesting explanations of why high depression risk status in children may affect the developmental trajectory of resting RSA. However, we caution against reliance on a linear model for extrapolation beyond the range of observed ages. For example, it would be a mistake to assume that differences would increase with age or that RSA trajectory would continue to be independent of mood disorder diagnosis. Even within the age range we examined, the “true” mean trajectories may be more complex. However, a larger sample with longer and more frequent follow-up would be required to fit nonlinear trajectories. Also given that the group by age effect was small, independent replication of these findings by others will be important. If replicated, our finding may suggest that low RSA is a risk factor for first-onset of depression given that it is detectable in children who are at high risk for mood disorders as they approach adolescence.
Acknowledgments
This study was supported by the NIMH Program Project Grant #MH56193, HHSA, Washington, DC, USA. Authors would like to thank the families who participated in this project, and Nathan Fox, Ph.D., who was Principal Investigator of the psychophysiology study.
Footnotes
Note that the analyses reported here include all usable data, but we did test our model when excluding the 39 observations from the protocol with the 6-minute baseline. However, the results were the same when only retaining youth (n = 157) who had 3-minute baselines. Thus we report on all usable data and conclude that baseline length does not account for our pattern of findings.
We had originally used the same frequency range for all children of .15 - .50 Hz due to the expectation that 4 year old children were not expected to be breathing faster than 30 times a minute at rest and due to the caution provided by Bar-Haim, Marshall and Fox (2000) that with some 4-year olds, high-frequency heart-rate variability may fall below .24 Hz. However, because we did not measure respiration, we cannot be certain that no child was indeed breathing faster than 30 times a minute. Therefore we used the .20-1.00 Hz band for 4-5 year olds, and the .15-.50 Hz band for the older children. However, it is important to note that our major results were identical (i.e., the significant Group X Age interaction) regardless of which frequency band was used for the younger children.
Random effect parameters had little effect on the mean inferences. The estimated family-level variance parameter for the intercept was 0.09 (SE = 0.09, p = 0.16) and for the slope, 0, indicating that family effects did not account for much individual variation. The child-level covariance parameters for the intercept were 0.24 (SE = 0.14, p < 0.05) in the high-risk group and 0.05 (SE = 0.14, p = 0.36) in the low-risk group while covariance parameters for slope were at or near zero in both groups. Upon examining other covariance structures for the repeated assessments, it was found that a compound symmetry within-subject covariance structure improved the model. Therefore, the standard errors on fixed effect parameters in Table 2 were adjusted under the assumption of an overall compound symmetric correlation of residuals. The compound symmetry parameter (i.e., correlation between RSA measured at one visit and any other visit) was small (0.01, SE = 0.001, p < 0.001) relative to the residual variance (0.83, SE = 0.09, p < 0.001) indicating that some individual variation in RSA remained unexplained by either the fixed effects or within-subject correlation.
Contributor Information
Amy L. Gentzler, West Virginia University, Department of Psychology Amy.gentzler@mail.wvu.edu
Jonathan Rottenberg, University of South Florida, Department of Psychology jrottenb@cas.usf.edu.
Maria Kovacs, University of Pittsburgh School of Medicine, Department of Psychiatry kovacs@pitt.edu.
Charles J. George, Western Psychiatric Institute and Clinic, University of Pittsburgh Medical Center qqq@pitt.edu
Jennifer Morey, West Virginia University, Department of Psychology Jennifer.morey@mail.wvu.edu.
References
- Allen M, Matthews K. Hemodynamic responses to laboratory stressors in children and adolescents: The influences of age, race, and gender. Psychophysiology. 1997;34:329–339. doi: 10.1111/j.1469-8986.1997.tb02403.x. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 3rd ed. Author; Washington, DC: 1980. [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed. Author; Washington, DC: 1994. [Google Scholar]
- Ashman S, Dawson G, Panagiotides H. Trajectories of maternal depression over 7 years: Relations with child psychophysiology and behavior and role of contextual risks. Development and Psychopathology. 2008;20:55–77. doi: 10.1017/S0954579408000035. [DOI] [PubMed] [Google Scholar]
- Bal E, Harden E, Lamb D, Van Hecke AV, Denver JW, Porges SW. Emotion recognition in children with autism spectrum disorders: Relations to eye gaze and autonomic state. Journal of Autism & Developmental Disorders. 2010;40:358–370. doi: 10.1007/s10803-009-0884-3. [DOI] [PubMed] [Google Scholar]
- Balogh S, Fitzpatrick D, Hendricks S, Paige S. Increases in heart rate variability with successful treatment in patients with major depressive disorder. Psychopharmacology Bulletin. 1993;29:201–206. [PubMed] [Google Scholar]
- Bar-Haim Y, Marshall PJ, Fox NA. Developmental changes in heart period and high-frequency heart rate variability from 4 months to 4 years of age. Developmental Psychobiology. 2000;37:44–56. doi: 10.1002/1098-2302(200007)37:1<44::aid-dev6>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- Beauchaine T, Gatzke-Kopp L, Mead H. Polyvagal theory and developmental psychopathology: Emotion dysregulation and conduct problems from preschool to adolescence. Biological Psychology. 2007;74:174–184. doi: 10.1016/j.biopsycho.2005.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berntson GG, Bigger JT, Jr., Eckberg DL, Grossman P, Kaufmann PG, Malik M, Nagaraja HN, Porges SW, Saul JP, Stone PH, van der Molen MW. Heart rate variability: Origins, methods, and interpretive caveats. Psychophysiology. 1997;34:623–648. doi: 10.1111/j.1469-8986.1997.tb02140.x. [DOI] [PubMed] [Google Scholar]
- Blandon A, Calkins S, Keane S, O'Brien M. Individual differences in trajectories of emotion regulation processes: The effects of maternal depressive symptomatology and children's physiological regulation. Developmental Psychology. 2008;44:1110–1123. doi: 10.1037/0012-1649.44.4.1110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bornstein M, Suess P. Child and mother cardiac vagal tone: Continuity, stability, and concordance across the first 5 years. Developmental Psychology. 2000;36:54–65. [PubMed] [Google Scholar]
- Bosch NM, Riese H, Ormel J, Verhulst F, Oldehinkel AJ. Stressful life events and depressive symptoms in young adolescents: Modulation by respiratory sinus arrhythmia? The TRAILS study. Biological Psychology. 2009;81:40–47. doi: 10.1016/j.biopsycho.2009.01.005. [DOI] [PubMed] [Google Scholar]
- Calkins SD, Keane SP. Cardiac vagal regulation across the preschool period: Stability, continuity, and implications for childhood adjustment. Developmental Psychobiology. 2004;45:101–112. doi: 10.1002/dev.20020. [DOI] [PubMed] [Google Scholar]
- Carney R, Freedland K, Stein P, Skala J, Hoffman P, Jaffe A. Change in heart rate variability during treatment for depression in patients with coronary heart disease. Psychosomatic Medicine. 2000;62:639–647. doi: 10.1097/00006842-200009000-00007. [DOI] [PubMed] [Google Scholar]
- Chambers A, Allen J. Vagal tone as an indicator of treatment response in major depression. Psychophysiology. 2002;39:861–864. doi: 10.1111/1469-8986.3960861. [DOI] [PubMed] [Google Scholar]
- DeLucia C, Pitts S. Applications of individual growth curve modeling for pediatric psychology research. Journal of Pediatric Psychology. 2006;31:1002–1023. doi: 10.1093/jpepsy/jsj074. [DOI] [PubMed] [Google Scholar]
- Dubreuil E, Ditto B, Dionne G, Pihl R, Tremblay R, Boivin M, Perusse D. Familiality of heart rate and cardiac-related autonomic activity in five-month-old twins: The Quebec newborn twins study. Psychophysiology. 2003;40:849–862. doi: 10.1111/1469-8986.00103. [DOI] [PubMed] [Google Scholar]
- Eisenberg N, Fabes R, Murphy B, Maszk P, Smith M, Karbon M. The role of emotionality and regulation in children's social functioning: A longitudinal study. Child Development. 1995;66:1360–1384. [PubMed] [Google Scholar]
- Ellis B, Garber J. Psychosocial antecedents of variation in girls’ pubertal timing: Maternal depression, stepfather presence, and marital and family stress. Child Development. 2000;71:485–501. doi: 10.1111/1467-8624.00159. [DOI] [PubMed] [Google Scholar]
- El-Sheikh M. Does poor vagal tone exacerbate child maladjustment in the context of parental problem drinking? A longitudinal examination. Journal of Abnormal Psychology. 2005a;114:735–741. doi: 10.1037/0021-843X.114.4.735. [DOI] [PubMed] [Google Scholar]
- El-Sheikh M. Stability of respiratory sinus arrhythmia in children and young adolescents: A longitudinal examination. Developmental Psychobiology. 2005b;46:66–74. doi: 10.1002/dev.20036. [DOI] [PubMed] [Google Scholar]
- El-Sheikh M, Harger J, Whitson S. Exposure to interparental conflict and children's adjustment and physical health: The moderating role of vagal tone. Child Development. 2001;72:1617–1636. doi: 10.1111/1467-8624.00369. [DOI] [PubMed] [Google Scholar]
- Feng X, Shaw D, Skuban E, Lane T. Emotional exchange in mother-child dyads: Stability, mutual influence, and associations with maternal depression and child problem behavior. Journal of Family Psychology. 2007;21:714–725. doi: 10.1037/0893-3200.21.4.714. [DOI] [PubMed] [Google Scholar]
- Field T, Diego M. Vagal activity, early growth and emotional development. Infant Behavior & Development. 2008;31:361–373. doi: 10.1016/j.infbeh.2007.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field T, Diego M, Dieter J, Hernandez-Reif M, Schanberg S, Kuhn C, Yando R, Bendell D. Prenatal depression effects on the fetus and the newborn. Infant Behavior & Development. 2004;27:216–229. [Google Scholar]
- Field T, Healy B, Goldstein S, Perry S. Infants of depressed mothers show ‘depressed’ behavior even with nondepressed adults. Child Development. 1988;59:1569–1579. doi: 10.1111/j.1467-8624.1988.tb03684.x. [DOI] [PubMed] [Google Scholar]
- Field T, Pickens J, Fox N, Nawrocki T. Vagal tone in infants of depressed mothers. Development and Psychopathology. 1995;7:227–231. [Google Scholar]
- First M, Spitzer R, Gibbon M, Williams J. Structured Clinical Interview for DSM IV Axis I Disorders - Patient Edition (SCID-I/P, Version 2.0) Biometrics Research Department, New York State Psychiatric Institute; New York: 1995. [Google Scholar]
- Finley J, Nugent S. Heart rate variability in infants, children and young adults. Journal of the Autonomic Nervous System. 1995;51:103–108. doi: 10.1016/0165-1838(94)00117-3. [DOI] [PubMed] [Google Scholar]
- Forbes E, Fox N, Cohn J, Galles S, Kovacs M. Children's affect regulation during a disappointment: Psychophysiological responses and relation to parent history of depression. Biological Psychology. 2006;71:264–277. doi: 10.1016/j.biopsycho.2005.05.004. [DOI] [PubMed] [Google Scholar]
- Galeev A, Igisheva L, Kazin E. Heart rate variability in healthy six- to sixteen year old children. Human Physiology. 2002;28(4):54–58. [PubMed] [Google Scholar]
- Gentzler AL, Santucci AK, Kovacs M, Fox N. Respiratory sinus arrhythmia reactivity predicts emotion regulation and depressive symptoms in at-risk and control children. Biological Psychology. 2009;82:156–163. doi: 10.1016/j.biopsycho.2009.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goto M, Nagashima M, Baba R, Nagano Y, Yokota M, Nishibata K, Tsuji A. Analysis of heart rate variability demonstrates effects of development on vagal modulation of heart rate in healthy children. The Journal of Pediatrics. 1997;130:725–729. doi: 10.1016/s0022-3476(97)80013-3. [DOI] [PubMed] [Google Scholar]
- Hastings P, De I. Parasympathetic regulation and parental socialization of emotion: Biopsychosocial processes of adjustment in preschoolers. Social Development. 2008;17:211–238. [Google Scholar]
- Hastings PD, Sullivan C, McShane KE, Coplan RJ, Utendale WT, Vyncke JD. Parental socialization, vagal regulation, and preschoolers’ anxious difficulties: Direct mothers and moderated fathers. Child Development. 2008;79:45–64. doi: 10.1111/j.1467-8624.2007.01110.x. [DOI] [PubMed] [Google Scholar]
- Hinnant JB, Elmore-Staton L, El-Sheikh M. Developmental trajectories of respiratory sinus arrhythmia and preejection period in middle childhood. Developmental Psychobiology. 2011;53(1):59–68. doi: 10.1002/dev.20487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones N, Field T, Fox N, Davalos M, Lundy B, Hart S. Newborns of mothers with depressive symptoms are physiologically less developed. Infant Behavior & Development. 1998;21:537–541. [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U. Schedule for affective disorders and schizophrenia for school-age children- present and lifetime version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Kaufman C, Kaiser D, Steinberger J, Kelly A, Dengel D. Relationships of cardiac autonomic function with metabolic abnormalities in childhood obesity. Obesity. 2007;15:1164–1171. doi: 10.1038/oby.2007.619. [DOI] [PubMed] [Google Scholar]
- Kazuma N, Otsuka K, Wakamatsu K, Shirase E, Matsuoka I. Heart rate variability in normotensive healthy children with aging. Clinical and Experimental Hypertension. 2002;24(1-2):83–89. doi: 10.1081/ceh-100108718. [DOI] [PubMed] [Google Scholar]
- Keenan K, Hipwell A, Feng X, Babinski D, Hinze A, Rischall M, Henneberger A. Subthreshold symptoms of depression in preadolescent girls are stable and predictive of depressive disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47:1433–1442. doi: 10.1097/CHI.0b013e3181886eab. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy AE, Rubin KH, Hastings PD, Maisel B. Longitudinal relations between child vagal tone and parenting behavior: 2 to 4 years. Developmental Psychobiology. 2004;45:10–21. doi: 10.1002/dev.20013. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Avenevoli S, Merikangas KR. Mood disorders in children and adolescents: An epidemiologic perspective. Biological Psychiatry. 2001;49:1002–1014. doi: 10.1016/s0006-3223(01)01129-5. [DOI] [PubMed] [Google Scholar]
- Kovacs M, Feinberg T, Crouse-Novak M, Paulauskas S, Finkelstein R. Depressive disorders in childhood. I. A longitudinal prospective study of characteristics and recovery. Archives of General Psychiatry. 1984;41:229–237. doi: 10.1001/archpsyc.1984.01790140019002. [DOI] [PubMed] [Google Scholar]
- Kovacs M, Lopez-Duran NL. Prodromal symptoms and atypical affectivity as predictors of major depression in juveniles: implications for prevention. Journal of Child Psychology and Psychiatry. 2010;51:472–496. doi: 10.1111/j.1469-7610.2010.02230.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovacs M, Obrosky DS, Gatsonis C, Richards C. First episode major depressive and dysthymic disorder in childhood: Clinical and sociodemographic factors in recovery. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:777–784. doi: 10.1097/00004583-199706000-00014. [DOI] [PubMed] [Google Scholar]
- Licht CMM, de Geus EJC, Zitman FG, Hoogendijk WJG, van Dyck R, Penninx BWJH. Association between major depressive disorder and heart rate variability in the Netherlands Study of Depression and Anxiety (NESDA). Archives of General Psychiatry. 2008;65:1358–1366. doi: 10.1001/archpsyc.65.12.1358. [DOI] [PubMed] [Google Scholar]
- Luke DA. Multilevel Modeling. Sage Publications; Thousand Oaks, CA: 2004. [Google Scholar]
- Marshall PJ, Stevenson-Hinde J. Behavioral inhibition, heart period, and respiratory sinus arrhythmia in young children. Developmental Psychobiology. 1998;33:283–292. [PubMed] [Google Scholar]
- Massin M, von Bernuth G. Normal ranges of heart rate variability during infancy and childhood. Pediatric Cardiology. 1997;18:297–302. doi: 10.1007/s002469900178. [DOI] [PubMed] [Google Scholar]
- Pereyra P, Zhang W, Schmidt M, Becker L. Development of myelinated and unmyelinated fibers of human vagus nerve during the first year of life. Journal of the Neurological Sciences. 1992;110:107–113. doi: 10.1016/0022-510x(92)90016-e. [DOI] [PubMed] [Google Scholar]
- Pickens JN, Field T. Facial expressions and vagal tone of infants of depressed and non-depressed mothers. Early Development and Parenting. 1995;4:83–89. [Google Scholar]
- Pikkujämsä S, Mäkikallio T, Sourander L, Räihä I, Puukka P, Skyttä J, Peng C, Goldberger A, Huikuri H. Cardiac interbeat interval dynamics from childhood to senescence: Comparison of conventional and new measures based on fractals and chaos theory. Circulation. 1999;100:393–399. doi: 10.1161/01.cir.100.4.393. [DOI] [PubMed] [Google Scholar]
- Porges S. Cardiac vagal tone: A physiological index of stress. Neuroscience & Biobehavioral Reviews. 1995;19:225–233. doi: 10.1016/0149-7634(94)00066-a. [DOI] [PubMed] [Google Scholar]
- Porges SW. The polyvagal perspective. Biological Psychology. 2007;74:116–143. doi: 10.1016/j.biopsycho.2006.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porges S, Doussard-Roosevelt J, Portales A, Greenspan S. Infant regulation of the vagal ‘brake’ predicts child behavior problems: A psychobiological model of social behavior. Developmental Psychobiology. 1996;29:697–712. doi: 10.1002/(SICI)1098-2302(199612)29:8<697::AID-DEV5>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- Roeser RW, Eccles JS. Adolescents’ perceptions of middle school: Relation to longitudinal changes in academic and psychological adjustment. Journal of Research on Adolescence. 1998;8:123–158. [Google Scholar]
- Rottenberg J. Cardiac vagal control in depression: A critical analysis. Biological Psychology. 2007;74:200–211. doi: 10.1016/j.biopsycho.2005.08.010. [DOI] [PubMed] [Google Scholar]
- Rottenberg J, Wilhelm F, Gross J, Gotlib I. Respiratory sinus arrhythmia as a predictor of outcome in major depressive disorder. Journal of Affective Disorders. 2002;71:265–272. doi: 10.1016/s0165-0327(01)00406-2. [DOI] [PubMed] [Google Scholar]
- Rudolph K, Hammen C. Age and gender as determinants of stress exposure, generation, and reactions in youngsters: A transactional perspective. Child Development. 1999;70(3):660–677. doi: 10.1111/1467-8624.00048. [DOI] [PubMed] [Google Scholar]
- Salomon K. Respiratory sinus arrhythmia during stress predicts resting respiratory sinus arrhythmia 3 years later in a pediatric sample. Health Psychology. 2005;24(1):68–76. doi: 10.1037/0278-6133.24.1.68. [DOI] [PubMed] [Google Scholar]
- Santucci A, Silk J, Shaw D, Gentzler A, Fox N, Kovacs M. Vagal tone and temperament as predictors of emotion regulation strategies in young children. Developmental Psychobiology. 2008;50:205–216. doi: 10.1002/dev.20283. [DOI] [PubMed] [Google Scholar]
- Schenker N, Gentleman JF. On judging the significance of differences by examining the overlap between confidence intervals. The American Statistician. 2001;55:182–186. [Google Scholar]
- Shannon K, Beauchaine T, Brenner S, Neuhaus E, Gatzke-Kopp L. Familial and temperamental predictors of resilience in children at risk for conduct disorder and depression. Development and Psychopathology. 2007;19:701–727. doi: 10.1017/S0954579407000351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw D, Schonberg M, Sherrill J, Huffman D, Lukon J, Obrosky D, Kovacs M. Responsivity to offspring's expression of emotion among childhood-onset depressed mothers. Journal of Clinical Child and Adolescent Psychology. 2006;35:490–503. doi: 10.1207/s15374424jccp3504_1. [DOI] [PubMed] [Google Scholar]
- Sherrill J, Kovacs M. Interview schedule for children and adolescents (ISCA). Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39:67–75. doi: 10.1097/00004583-200001000-00018. [DOI] [PubMed] [Google Scholar]
- Silvetti M, Drago F, Ragonese P. Heart rate variability in healthy children and adolescents is partially related to age and gender. International Journal of Cardiology. 2001;81:169–174. doi: 10.1016/s0167-5273(01)00537-x. [DOI] [PubMed] [Google Scholar]
- Sinnreich R, Friedlander Y, Sapoznikov D, Kark J. Familial aggregation of heart rate variability based on short recordings--the kibbutzim family study. Human Genetics. 1998;103:34–40. doi: 10.1007/s004390050779. [DOI] [PubMed] [Google Scholar]
- Snieder H, Boomsma D, Van Doornen L, De Geus E. Heritability of respiratory sinus arrhythmia: Dependency on task and respiration rate. Psychophysiology. 1997;34:317–328. doi: 10.1111/j.1469-8986.1997.tb02402.x. [DOI] [PubMed] [Google Scholar]
- Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology Heart rate variability: Standards of measurement, physiological interpretation and clinical use. Circulation. 1996;93:1043–1065. [PubMed] [Google Scholar]
- Thayer J, Smith M, Rossy L, Sollers J, Friedman B. Heart period variability and depressive symptoms: Gender differences. Biological Psychiatry. 1998;44:304–306. doi: 10.1016/s0006-3223(98)00008-0. [DOI] [PubMed] [Google Scholar]
- Van Hecke AV, Lebow J, Bal E, Lamb D, Harden E, Kramer A, Porges SW. Electroencephalogram and heart rate regulation to familiar and unfamiliar people in children with autism spectrum disorders. Child Development. 2009;80(4):1118–1133. doi: 10.1111/j.1467-8624.2009.01320.x. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Wickramaratne P, Nomura Y, Warner V, Pilowsky D, Verdeli H. Offspring of depressed parents: 20 years later. American Journal of Psychiatry. 2006;163:1001–1008. doi: 10.1176/ajp.2006.163.6.1001. [DOI] [PubMed] [Google Scholar]