Abstract
Objective: The efficacy and acceptability of existing psychological interventions for health anxiety (hypochondriasis) are limited. In the current study, the authors aimed to assess the impact of mindfulness-based cognitive therapy (MBCT) on health anxiety by comparing the impact of MBCT in addition to usual services (unrestricted services) with unrestricted services (US) alone. Method: The 74 participants were randomized to either MBCT in addition to US (n = 36) or US alone (n = 38). Participants were assessed prior to intervention (MBCT or US), immediately following the intervention, and 1 year postintervention. In addition to independent assessments of diagnostic status, standardized self-report measures and assessor ratings of severity and distress associated with the diagnosis of hypochondriasis were used. Results: In the intention-to-treat (ITT) analysis (N = 74), MBCT participants had significantly lower health anxiety than US participants, both immediately following the intervention (Cohen's d = 0.48) and at 1-year follow-up (d = 0.48). The per-protocol (PP) analysis (n = 68) between groups effect size was d = 0.49 at postintervention and d = 0.62 at 1-year follow-up. Mediational analysis showed that change in mindfulness mediated the group changes in health anxiety symptoms. Significantly fewer participants allocated to MBCT than to US met criteria for the diagnosis of hypochondriasis, both immediately following the intervention period (ITT 50.0% vs. 78.9%; PP 47.1% vs. 78.4%) and at 1-year follow-up (ITT 36.1% vs. 76.3%; PP 28.1% vs. 75.0%). Conclusions: MBCT may be a useful addition to usual services for patients with health anxiety.
Keywords: mindfulness-based cognitive therapy, mindfulness, health anxiety, hypochondriasis
Severe health anxiety, also described as hypochondriasis (Diagnostic and Statistical Manual of Mental Disorders; 4th ed., text rev., or DSM–IV–TR; American Psychiatric Association, 2000) or hypochondriacal disorder (ICD–10 Classification of Mental and Behavioural Disorders; World Health Organization, 1992), is characterized by the preoccupation with the fear of having a serious disease, which persists in spite of appropriate medical reassurance. Up to 9% of patients in general medical practice clinics and up to 5% of the general population meet diagnostic criteria for hypochondriasis (Creed & Barsky, 2004; Gureje, Üstun, & Simon, 1997). Health anxiety not only causes great suffering for the patient and those around him or her but is also costly in terms of higher medical care utilization (Barsky, Ettner, Horsky, & Bates, 2001; Noyes et al., 1994) and occupational disability (Mykletun et al., 2009). Hence, it is a priority for the sake of both patients and health care service providers to develop effective treatments for health anxiety.
Patients with health anxiety have a preference for psychological treatments over drug treatments (Walker, Vincent, Furere, Cox, & Kjernisted, 1999). However, to date, the effects of psychological treatments on health anxiety have been limited. Thomson and Page's (2007) Cochrane review concluded that the strongest evidence for a psychological treatment that was effective for hypochondriasis was for cognitive behavioral therapy (CBT), with several studies reporting positive outcomes (e.g., Barsky & Ahern, 2004; Clark et al., 1998; Greeven et al., 2007; Visser & Bouman, 2001). However, they noted several limitations of the existing trial data on the psychological treatment of health anxiety. First, the possibility that improvements seen were due to nonspecific factors involved in regular therapist contact cannot be ruled out, emphasizing the need for mediational analyses. Second, it was not possible to determine what proportion of patients were “cured” by the treatments, highlighting the need to give diagnostic outcomes as well as scores on continuous variables. And third, data on the longer term outcome from psychological treatments for health anxiety are limited, highlighting the need for extended follow-up periods. This paucity of follow-up data is especially concerning given the low natural recovery rate of health anxiety (Olde Hartman et al., 2009). Furthermore, in some studies of psychological treatments for health anxiety, as few as 30% of eligible participants agreed to participate (Barsky & Ahern, 2004), and dropout rates of 25%–30% have been reported (Greeven et al., 2007; Visser & Bouman, 2001), suggesting that existing psychological interventions are not always acceptable to patients with health anxiety. Taken together, these data suggest that the efficacy and acceptability of existing psychological treatments for health anxiety could be improved.
Given the limitations of existing interventions, it remains a priority to investigate novel treatments for health anxiety. Recent developments in novel psychological interventions have included mindfulness-based cognitive therapy (MBCT; Segal, Williams, & Teasdale, 2002). MBCT is a cost-effective 8-week class-based program in which participants are taught to observe their thoughts and feelings through the repeated practice of intentionally returning attention to an object (e.g., the breath or body sensations). Participants are taught how to cultivate direct experiential awareness and nonjudgmental acceptance of whatever arises in each moment (including negative mood states that trigger anxiety and negative thinking). The cultivation of awareness during mindfulness practice enables participants to recognize when negative and ruminative responses are being triggered and facilitates decentering from such patterns of thought, seeing them as mental events rather than as valid reflections of reality. Unlike standard cognitive–behavioral therapy (CBT), where the focus has traditionally been on changing the content of thoughts, MBCT focuses on fostering meta-cognitive awareness and the modification of meta-cognitive processes that maintain unhelpful reactive or ruminative mind states.
MBCT was designed to target the cognitive processes that render depressed individuals vulnerable to repeated relapse and recurrence, such as rumination and high cognitive reactivity (Teasdale, Segal, & Williams, 1995). MBCT has been shown to reverse processes hypothesized to underlie depressive psychopathology (e.g., Hargus, Crane, Barnhofer, & Williams, 2010; Kuyken et al., 2010; Raes, Dewulf, van Heeringen, & Williams, 2009) and to reduce the risk of relapse of depression (Teasdale et al., 2000) as much as maintenance antidepressant medication (Kuyken et al., 2008; Segal et al, 2010). Although originally designed for depressed patients in remission, preliminary data suggest that MBCT may be helpful for a broad range of mental health problems including bipolar disorder, generalized anxiety disorder, panic disorder, chronic fatigue syndrome, and psychosis, as well as chronic, treatment-resistant, and suicidal forms of depression (see Hofmann, Sawyer, Witt, & Oh, 2010, and Piet & Hougaard, 2011, for reviews of the efficacy of MBCT interventions).
There are several reasons to hypothesize that MBCT may be particularly applicable to the treatment of health anxiety. First, unlike standard CBT, MBCT does not aim to change the content of the patient's thoughts by disconfirming the feared predictions, but to reduce their impact by changing the individual's relationship to their thoughts. This may circumvent the difficulty of disconfirming health anxious fears, which often relate to the distant future and thus are not so amenable to disconfirmation via standard CBT methods such as thought challenging or behavioral experiments. Second, rumination has been shown to maintain health anxiety (Marcus, Hughes, & Arnau, 2008), and MBCT can reduce maladaptive rumination (Heeren & Philippot, 2011; Michalak, Hölz, & Teismann, 2011). Hence, it is hypothesized that MBCT may help health anxious patients to learn generic skills of attentional control to enable them to break the pattern of excessive attending to somatic sensations, which leads to an escalation of anxiety via rumination on the potential negative meanings of sensations.
However, note that cognitive–behavioral conceptualizations have emphasized the role of heightened bodily focused attention in the maintenance of health anxiety (e.g., Warwick & Salkovskis, 1990), and this is supported by experimental studies of attentional bias in health anxiety (Rassin, Muris, Franken, & van Straten, 2008). Thus, MBCT's focus on attentional awareness of the body may be problematic for patients with health anxiety. The preliminary evidence that training in attentional control strategies can be beneficial to patients with health anxiety excludes attention to the body for this reason (Papageorgiou & Wells, 1998). On the other hand, a central tenet of MBCT is changing the mode of mind within which a person views him- or herself and the world, leading the individual away from the problem-solving mode that seeks as its first priority to change or “get rid of” unwanted experiences (Williams, 2008). To this end, patients are taught to see more clearly the patterns of mind that exacerbate and maintain emotional disturbance. This involves seeing directly the distinction between the raw body sensations as actually experienced and the meaning that has become associated with those sensations. Thus, rather than refocusing attention away from body sensations, MBCT encourages the person to bring curiosity toward the sensations themselves, to register their affective quality, and to observe how the mind and body react to this information (most often with negative and ruminative responses). Despite these intentions, it is possible that MBCT may fail to break into the hypothesized maintenance cycles of health anxiety because patients may find body focus too aversive.
Preliminary results are encouraging, however. A recent pilot study (N = 10) reported MBCT produced significant improvements in health anxiety, disease-related thoughts, and somatic symptoms; the improvements were sustained at 3-month follow-up (Lovas & Barsky, 2010). In addition, both Lovas and Barsky's pilot study and a qualitative study of MBCT for health anxiety (Williams, McManus, Muse, & Williams, 2011) reported MBCT to be an acceptable treatment to patients with health anxiety. However, to date, there have been no controlled evaluations of the impact of MBCT for health anxiety. The current study reports on the outcome from a randomized clinical trial in which MBCT in addition to unrestricted services (US) was compared with US alone.
Method
Study Objectives and Design
Our objective was to assess the impact of MBCT on health anxiety by comparing the impact of MBCT plus US with US alone in a single center randomized trial conducted in a university setting in the United Kingdom. It was hypothesized that participants who received MBCT in addition to US would have lower levels of health anxiety than those who received US alone, both immediately following the intervention, and at 1-year follow-up.
Participants were assessed prior to intervention (MBCT or US), immediately following the 8-week intervention period, and at 1 year postintervention. Allocation status was concealed from the independent assessors, and the trial adhered to established procedures to maintain separation between staff who administered outcome measurements and staff who delivered the intervention. Given that previous treatment trials in health anxiety have been criticized for failing to assess diagnostic status as a primary outcome (Thomson & Page, 2007), the primary outcome measures in our study were the diagnosis of hypochondriasis and assessor ratings of interference and distress associated with the diagnosis of hypochondriasis, as well as self-report scores on standardized measures of health anxiety.
Participants
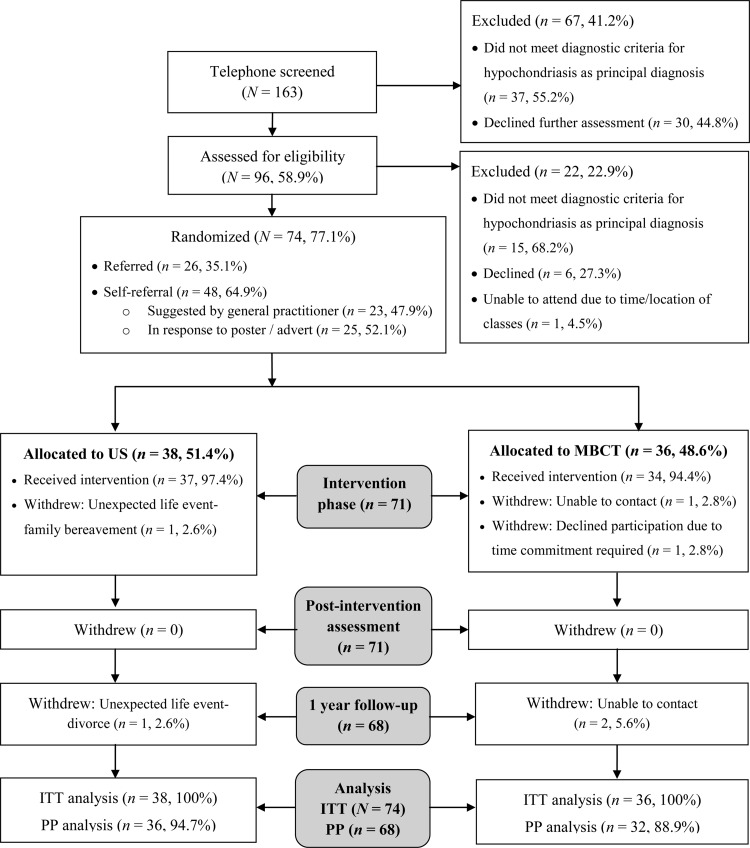
Participants were recruited between July 2008 and September 2009 via referrals from health professionals and self-referral in response to posters placed in local medical and psychiatric services and a local press release. Potential participants were screened via telephone interviews for (a) the presence of the symptoms of hypochondriasis using the DSM–IV–TR (American Psychiatric Association, 2000) and probe questions outlined in Taylor and Asmundson (2004) and (b) study inclusion/exclusion criteria, such as age and acceptance of random allocation. Those who reported symptoms in line with DSM–IV–TR criteria for hypochondriasis and meeting the study inclusion criteria were invited for assessment. During the assessment, we established diagnoses using the Structured Clinical Interview for DSM–IV–TR Axis I disorders (SCID–I; First, Gibbon, Spitzer, & Williams, 2002) by a trained assessor. Inclusion criteria were (a) being between the ages of 18 and 65, (b) meeting DSM–IV–TR criteria for the diagnosis of hypochondriasis as the principal diagnosis, and (c) having adequate skills in written and spoken English. Exclusion criteria were (a) meeting DSM–IV–TR criteria for the diagnosis of a psychotic illness or for substance dependence or (b) having severity of symptoms or suicidality such that allocation to US (delayed MBCT) would be unethical. Participants were not excluded for being in receipt of other forms of treatment (psychological or drug), but if they were taking psychotropic medication, they were required to have been on a stable dose for 6 weeks prior to inclusion in the study. The flow of participants through the trial, including reasons for exclusion or withdrawal, is depicted in Figure 1.
Figure 1. Consolidated Standards of Reporting Trials (CONSORT) diagram showing the flow of participants through the trial and reasons for dropout. US = unrestricted services; MBCT = mindfulness-based cognitive therapy; ITT = intention to treat; PP = per protocol.
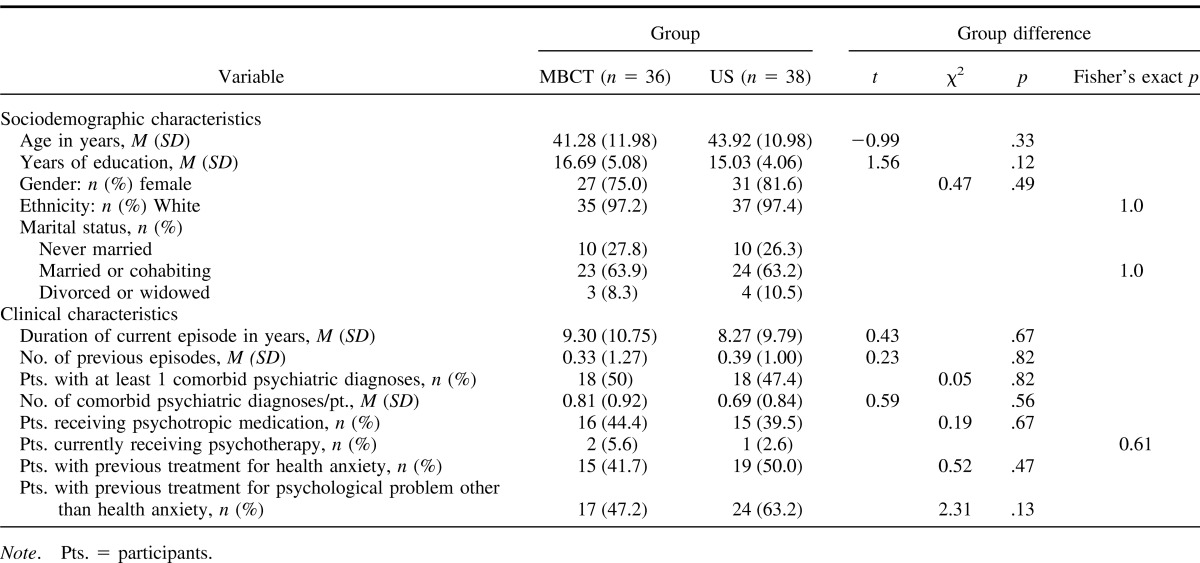
Characteristics of the MBCT and US groups are shown in Table 1 along with the results of t tests for continuous variables and chi-square or Fisher's exact tests for categorical variables. There were no significant differences between the two groups in their clinical and sociodemographic characteristics or scores on self-report measures (see Table 1 for means and SDs of self-report measures, all ts ≤ 1.15, all ps ≥ .37).
Table 1. Demographic and Clinical Characteristics of Participants (N = 74) Allocated to Mindfulness-Based Cognitive Therapy (MBCT) and Unrestricted Services (US).
The participants constituted a relatively chronic sample, with up to seven previous episodes and a mean duration of the current episode of hypochondriasis of 8.77 years (SD = 10.21; range = 6 months–41 years). The mean severity of health anxiety on the Short Health Anxiety Inventory (SHAI; Salkovskis, Rimes, Warwick, & Clark, 2002) was 32.85 (SD = 8.22) and on the Whiteley Index (WI; Pilowsky, 1967) 49.34 (SD = 11.64), which is comparable to scores reported for other samples of patients diagnosed with hypochondriasis (e.g., Barsky & Ahern, 2004; Nakao, Shinozaki, Ahern, & Barsky, 2011; Wattar et al., 2005). Thirty-six participants (48.7%) had one or more comorbid diagnoses; 19 had one comorbid diagnosis, 15 had two comorbid diagnoses, and two participants had three comorbid diagnoses, making a total of 55 comorbid diagnoses across the 74 participants. Participants' comorbid diagnoses were as follows: depression (n = 13), obsessive–compulsive disorder (n = 5), dysthymic disorder (n = 2), panic disorder (n = 6), social phobia (n = 6), alcohol abuse (n = 1), generalized anxiety disorder (n = 9), specific phobia (n = 10), binge eating disorder (n = 2), and pain disorder (n = 1). Of the 74 participants, 34 (46.0%) had previously had psychological treatment for health anxiety, including the three (4.1%) who were engaged in psychological treatment at the time of the initial assessment. Furthermore, 41 (55.4%) had previously had treatment for a psychological problem other than health anxiety. Although previous experience with yoga or meditation was not assessed, no participants had previously participated in a mindfulness-based psychological intervention.
Procedure
The study was approved by the local National Health Service Research Ethics Committee and was carried out in the University of Oxford's Department of Psychiatry from September 2008 to January 2010, with follow-up assessments continuing until January 2011.
Allocation Strategy
Participants were allocated by an independent statistician to either US alone or MBCT plus US using Pocock's (1983) minimization method in random block sizes, whereby each patient was randomized to the group (MBCT vs. US) that minimizes any existing imbalance between the groups in severity, comorbidity, age, and gender. The randomization method was successful in that there were no significant differences between the two groups on any clinical or demographic characteristic at intake to the study (see Table 1).
Measures
Diagnoses
The Structured Clinical Interview for DSM–IV Axis I Disorders (SCID–I; First et al., 1997) was used to establish diagnoses and to make the judgment that hypochondriasis was the principal diagnosis. In line with DSM–IV–TR criteria, participants were not judged to meet diagnostic criteria for hypochondriasis if we could not exclude the possibility that their health anxiety was realistic concern about a medical condition.
Diagnostic assessments were carried out “blind” to treatment status by an independent assessor who was trained and experienced in use of the SCID–I in patients with anxiety disorders. All SCID–I assessments were audio recorded, and 20.0% (n = 45 across three assessment times) were selected at random and rated by a different assessor for reliability, with high agreement between assessors (κ = .924, p < .001).
Health anxiety
All measures of health anxiety were significantly correlated with each other, with the correlation between the two standardized self-report scales (SHAI and WI) being .84, p < .001, and between the two assessor ratings (of distress and interference) being .76, p < .001. Hence, a composite measure, the Health Anxiety Composite, was used as the primary outcome. This was created by combining the assessor and self-report measures of health anxiety, using Rosenthal and Rosnow's (1991) procedure, which has been adopted in several previous trials of psychological treatments (e.g., Clark et al., 2003, 2006). Patients' scores on each scale were standardized (M = 0, SD = 1) by converting to Z scores. The composite at each assessment occasion (preintervention, postintervention, and follow-up) was the mean of the Z scores on that occasion. The individual scales that made up the composite were as follows:
Assessor ratings
Independent assessors, blind to treatment allocation, rated the degree of distress and interference associated with participants' health anxiety (on visual analogue scales from 0 = not at all to 10 = extremely). As with diagnostic assessments, 20% (n = 45) were rated by a different assessor to establish reliability of ratings. Intraclass correlation coefficients (two-way random-effects model, absolute agreement on single measures) were equal to or greater than .95 for both distress and interference ratings, indicating good agreement between raters.
Standardized self-report measures of health anxiety
The Short Health Anxiety Inventory (SHAI: Salkovskis et al., 2002)
The SHAI is widely seen as the primary self-report measure of health anxiety symptoms. It consists of 18 self-report items, each rated on a Likert scale from 0 to 3. This scale has been shown to have high internal consistency (α = .89 in the current sample) and to have good sensitivity and specificity (Salkovskis et al., 2002).
The Whiteley Index (WI: Pilowsky, 1967)
Although it has been criticized in recent years (e.g., Salkovskis et al., 2002), the WI was included because its historical widespread use allows comparison of results from the current study with those from earlier treatment studies. The WI is a 14-item self-report questionnaire measure of health anxiety with demonstrated psychometric properties (Pilowsky, 1967). We used a Likert scale version of the WI (Welch, Carleton, & Asmundson 2009), on which each item is scored on a scale from 1 (not at all) to 5 (a great deal). The WI had high internal consistency (α = .92) in the current sample.
General Symptom Measures
The Beck Anxiety and Depression Inventories (BAI: Beck, Epstein, Brown, & Steer, 1988; BDI–II: Beck, Steer & Brown, 1996) were used to measure general symptoms levels. The BAI and BDI are widely used 21-item self-report measures of the cognitive, affective, behavioral and somatic symptoms of anxiety and depression respectively. Both have been demonstrated to have good psychometric properties (Beck et al., 1996; Beck & Steer, 1993) and internal consistency was good in the current sample (α = .90 and α = .93 respectively).
Mindfulness
The Five Facet Mindfulness Questionnaire (FFMQ: Baer et al., 2008) is a 39-item self-report questionnaire designed to measure the constructs central to mindfulness: observing, describing, nonreactivity to experience, nonjudgment of experience, and acting with awareness. Items are rated on a Likert scale ranging from 1 to 5, and the scale has been shown to have good internal consistency (α = .91 in the current sample) and construct validity (Baer et al., 2008).
Interventions
There was no difference between the MBCT and US groups in the mean time between attending the initial assessment of suitability and allocation/commencement of the intervention period; respective means (SD) were 42.33 (24.02) versus 43.53 (29.11) days, t(72) = 0.19, p = .85. The mean delay between assessment and the commencement of the intervention period (allocation to MBCT or US) in this study was comparable to that reported in other trials of group interventions (e.g., Barnhofer et al., 2009). During the time between participants' initial assessment of suitability and allocation to MBCT or US, the assessor maintained telephone contact with participants to assess any changes in their levels of health anxiety. Those who reported any change in their level of health anxiety were reassessed immediately prior to the beginning of the intervention period, with those scores being used as the preintervention scores. For those who were reassessed (n = 10), there was a trend toward exacerbation of health anxiety, which did not reach significance: SHAI means (SD) 30.70 (5.87) versus 32.90 (6.84), t(9) = −1.91, p = .09.
MBCT intervention
MBCT is a manualized, group-based skills training program (Segal, Williams, & Teasdale, 2002) that begins with an individual “preclass assessment” in which the MBCT teacher lets the participants know what to expect during the course and discusses how mindfulness might help them, given their particular history, current symptoms, and maintaining factors. The remaining sessions are delivered in a class format over 8 weekly sessions of 2 hr each. Each of the four MBCT classes of between seven and 11 participants was led by an experienced MBCT teacher assisted by a clinician with less MBCT experience. In addition to the weekly classes, participants were asked to engage in homework, including regular meditation practices and related exercises for about I hr per day for 6 days a week. The MBCT treatment in this study followed the manual by Segal, Williams, and Teasdale (2002) with some adaptations to focus on health anxiety and address the presence of acute symptoms (see McManus, Muse, & Surawy, 2011, for more detail on the implementation of MBCT for health anxiety).
Unrestricted services (US) intervention
In the current literature, there is considerable variation in treatment-as-usual (TAU) comparison conditions, with some studies using the term TAU to reflect a standardized intervention that is comparable to the active intervention and others using the term to describe unconstrained services, which varied across participants and sites. For clarity, the term unrestricted services (US) is used to describe the comparison condition in our study. Those allocated to US were informed that the purpose of the study was to assess the impact of MBCT in comparison to the provision of usual services and that they would be offered the MBCT intervention after the 60-week duration of the study. They were not directed toward any specific services but were encouraged to continue any current medication or other interventions and advised to seek help from their family doctor or other sources, as they normally would, over the duration of the study. The treatment that participants received as US was monitored at the assessment sessions and is reported in the section titled US alone.
MBCT + US
Of the 34 MBCT participants who completed the postintervention assessment, four (11.8%) received additional psychological treatment during this period: one received CBT for health anxiety, one received nonspecific counseling, and two received CBT for anxiety (although one of these only received two sessions). Of the four participants who received additional psychological treatment during the MBCT intervention, one continued to receive treatment (CBT for anxiety) during the 1-year follow-up period. An additional six MBCT participants received additional psychological treatment between the postintervention assessment and the 1-year follow-up assessment: three received CBT for health anxiety, one received nonspecific counseling, one received CBT for anxiety, and one received CBT for depression. Thus, of the 32 participants who completed the 1-year follow-up assessment, 10 (31.2%) had received additional psychological treatment at some point during the 60 weeks of the study. Of the 36 participants allocated to MBCT, 16 had been taking psychotropic medication at intake. Of these 16, two had stopped taking medication by the postintervention assessment, and another one had stopped taking medication by the 1-year follow-up assessment. None of the 20 participants allocated to MBCT who had not been taking psychotropic medication at the initial assessment began to take it during the study.
US alone
Of the 37 US participants who completed the postintervention assessment, seven (18.9%) had received psychological treatment during the 8-week US period: two received CBT for health anxiety, one received counseling focused on health anxiety, one received psychiatric treatment for depression, one received two sessions of management advice for chronic fatigue syndrome, one received CBT for pain management, and one received computerized CBT for depression. Of the seven participants who received psychological treatment during the 8-week US period, five continued to receive treatment during the 1-year follow-up period: one received CBT for pain management, one received management advice for chronic fatigue syndrome, one received psychiatric treatment for depression, one received CBT for health anxiety, and one received counseling for health anxiety. An additional four US participants received additional psychological treatment between the postintervention and 1-year follow-up assessments: two received CBT for health anxiety, one received pain management advice, and one received nonspecific counseling. Thus, of the 36 participants who completed the 1-year follow-up assessment, 11 (30.6%) received additional psychological treatment at some point during the 60 weeks of the study (comparable to the 31.2% in the MBCT group). Of the 38 participants allocated to US, 15 had been taking psychotropic medication at intake. Of these 15, one had stopped taking medication by the postintervention assessment, and another one had stopped taking medication at the 1-year follow-up. Of the 23 participants in the US group who were not taking psychotropic medication at the initial assessment, five (21.7%) began taking psychotropic medication during the course of the study, two by the postintervention assessment, and an additional three by the 1-year follow-up.
Treatment Adherence
MBCT classes were led by a qualified CBT therapist [CS] who has extensive training and experience in delivering MBCT. Supervision was provided by of one of the developers of MBCT [JMGW], who monitored both adherence to the MBCT treatment protocol and competence in delivering it. All MBCT sessions were videorecorded, and a random selection of 16 (50.0%) were assessed by independent psychologists for adherence using the Mindfulness-Based Cognitive Therapy Adherence Scale (MBCT–AS; Segal, Teasdale, Williams, & Gemar, 2002). The MBCT–AS is a 17-item measure of observable therapist behaviors (rated 0 = no evidence, 1 = slight evidence, 2 = definite evidence). The MBCT–AS was modified to replace the word “depression” with “health anxiety” as this was the focus of treatment. The mean MBCT-AS score was 22.56 (SD = 5.78) which is comparable to scores reported in the psychometric evaluation of the scale (Segal, Teasdale, Williams, & Gemar, 2002) and in other trials of MBCT (Kuyken et al., 2008) and indicates good adherence to protocol.
Of the 36 participants allocated to MBCT, two (5.5%) did not attend any classes (see Figure 1). The 34 participants who took part in MBCT classes attended a mean of 6.5 (SD = 1.58) classes.
Power Calculation
In a recent meta-analytic review, Hofmann et al. (2010) reported MBCT interventions to have effect sizes ranging from Hedges's g = 0.59–0.97 for patients with anxiety or anxiety and mood disorders, and similar effect sizes have been reported for CBT interventions for health anxiety (e.g., Buwalda, Bouman, & van Duijn, 2007). Given a conservative estimated effect size of d = 0.7, a two-tailed power calculation (using G*Power) shows that a sample size of 68 (34 per group) has 80.0% power to detect at p < .05 an effect size of d = 0.7. Thus the sample of 74 should give sufficient power for the primary comparisons.
Results
Data Analytic Strategy
Analyses were conducted on both per-protocol (PP)1 and intention-to-treat (ITT) samples (see Figure 1 for details of attrition), but for the sake of parsimony, PP analyses are reported only where results differ from the ITT analysis. For the ITT sample, we used the conservative method of including all participants who were entered into the trial (N = 74), regardless of whether they received the intervention, with the last observation carried forward for missing data (4.1% of participants at postintervention and 8.1% at 1-year follow-up). As a manipulation check, we used a repeated-measures analysis of variance (ANOVA) with group (MBCT vs. US) as a between-participants factor and time (preintervention vs. postintervention vs. follow-up] as a within-participants factor to determine if the MBCT intervention had been successful in increasing mindfulness (the core construct it aims to impact). Health anxiety outcomes were analyzed using a repeated-measures ANOVA2 for the health anxiety composite measure with group (MBCT vs. US) as a between-participants factor and time (preintervention, postintervention, 1-year follow-up) as a within-participants factor. This was followed by corresponding univariate repeated-measures Group × Time ANOVAs3 for each dependent measure separately (results are reported in Table 2). When the assumption of homogeneity of variance was violated, we adjusted the degrees of freedom using the Welch–Satterthwaite method. Significant interactions were followed up with comparison by independent t tests of the MBCT and US groups at each time point. Chi-square tests were used to compare binary variables (e.g., diagnosis of hypochondriasis).
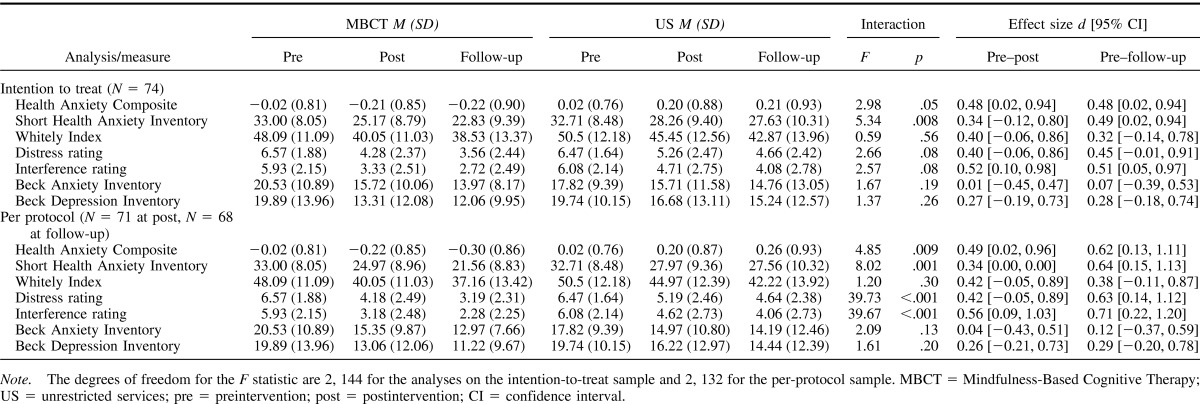
Table 2. Mean Scores (and Standard Deviations) on Symptom Measures, Results of Analyses of Variance and Between-Group Effect Sizes (Per-Protocol and Intention-to-Treat Samples).
Manipulation Check
To assess the effectiveness of the MBCT intervention on mindfulness, participants' scores on the FFMQ were analyzed (ITT analysis N = 74) using a 2 (treatment: MBCT vs. US) × 3 (time: preintervention vs. postintervention vs. 1-year follow-up) repeated-measures ANOVA. There was a significant effect of time, F(1.77, 127.37) = 10.84, p < .001, η2 = .13, and a significant Time × Group interaction, F(1.77, 127.37) = 3.66, p = .03,η2 = .05. Post hoc tests revealed a significant increase from pre- to post-intervention in FFMQ scores in the MCBT group, t(35) = −3.62, p = .001, but not in the US group, t(37) = 0.84, p = .41. There were no further significant changes between the postintervention assessment and the 1-year follow-up assessment in FFMQ scores in either the MBCT or US groups: MCBT group, t(35) = 0.32, p = .75; US group, t(37) = 1.42, p = .16.
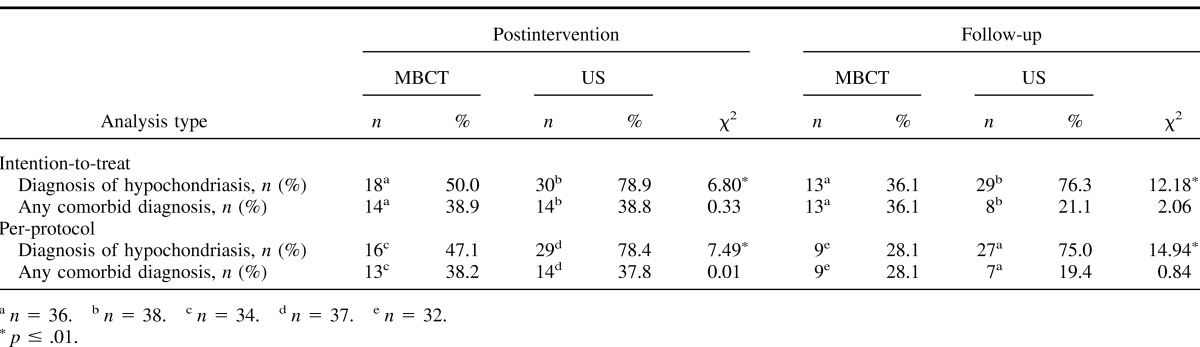
Diagnosis of Hypochondriasis and Comorbid Diagnoses
Chi-square tests showed that a significantly smaller proportion of participants allocated to MBCT, as compared with those allocated to US, continued to meet criteria for the diagnosis of hypochondriasis, both immediately following the MBCT/US period and at 1-year follow-up (see Table 3). However, chi-square tests showed no significant differences in the proportion of participants with a comorbid diagnosis in the MBCT and US groups at either postintervention or 1-year follow-up. Similarly, a repeated-measures ANOVA for the mean number of comorbid diagnoses per participant with group (MBCT vs. US) as a between-participants factor and time (preintervention vs. postintervention vs. 1-year follow-up) as a within-participants factor on the ITT sample (N = 74) showed a significant effect of time, F(1.67, 120.25) = 16.37, p > .001, η2 = .19, but no significant effect of group, F(1, 72) = 0.27, p = .61, η2 = .004, or significant Group × Time interaction, F(1.67, 120.25) = 0.74, p = .46 η2 = .01.
Table 3. Intention-to-Treat and Per-Protocol Analyses of the Proportion of Participants in the Mindfulness-Based Cognitive Therapy (MBCT) and Unrestricted Services (US) Groups Meeting Criteria for Diagnosis of Hypochondriasis or Other Psychiatric Disorders at Postintervention and Follow-Up.
Health Anxiety Measures
Health anxiety composite
A repeated-measures ANOVA for the health anxiety composite measure with group (MBCT vs. US) as a between-participants factor and time (preintervention vs. postintervention vs. 1-year follow-up) as a within-participants factor on the ITT sample (N = 74) showed no significant effect of time, F(2, 144) = 0.002, p > .99, η2 < .01, or group, F(1, 72) = 2.99, p = .09, η2 = .04, but a significant Group × Time interaction, F(2, 144) = 2.98, p = .05, η2 = .04. Post hoc t tests showed that the MBCT group scored significantly lower than the US group, both immediately following the intervention, t(72) = −2.02, p < .05, and at the 1-year follow-up, t(72) = −2.03, p < .05 (see Table 2 for means and SDs), with a between-groups effect size (d) 0.48, 95% confidence interval (CI) d [0.02, 0.94], at both time points.
Individual health anxiety measures
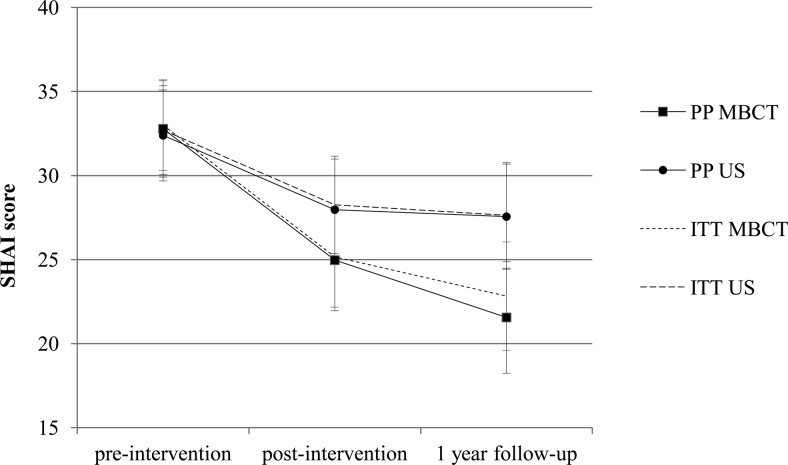
To facilitate comparison with previous trials, here we report outcomes on symptom measures individually, analyzed using 2 (treatment: MBCT vs. US) × 3 (time: preintervention vs. postintervention vs. 1-year follow-up) repeated-measures ANOVAs for each measure. Means, standard deviations, results of Group × Time interactions, and between-group effect sizes are shown in Table 2. Figure 2 shows MBCT and US participants' scores on the SHAI at the three time points, with 95% CIs.
Figure 2. Score for the mindfulness-based cognitive therapy (MBCT) group and unrestricted services (US) group on the Short Health Anxiety Inventory (SHAI) at preintervention, postintervention, and 1-year follow-up (PP = per-protocol sample; ITT = intention-to-treat sample) with 95% confidence intervals.
Impact on General Levels of Anxiety and Depression
Scores on measures of general levels of anxiety and depression were analyzed with a multivariate analysis of variance (MANOVA), which showed a significant effect of time, F(4, 69) = 6.89, p > .001, η2 = 0.29, but no significant effect of group, F(2, 71) = 1.13, p = .33, η2 = 0.03, or significant Group × Time interaction, F(4, 69) = 0.77, p = .55, η2 = 0.04, in the ITT sample. See Table 2 for means, standard deviations, results of Group × Time interactions, and between-group effect sizes.
Mediation Analysis
A mediational analysis was conducted to determine whether changes in health anxiety were due to changes in mindfulness. Following MacKinnon, Lockwood, and Williams's (2004) recommendations for directly examining mediation in small samples, we used a nonparametric, resampling approach (bootstrapping procedure; Preacher & Hayes, 2008) to test the significance of the hypothesized mediation model. The SPSS script provided by Preacher and Hayes (Hayes, n.d.) was used to implement the nonparametric resampling method (bias-corrected bootstrap) with 5,000 resamples to derive the 95% CIs for the indirect effect of group (MBCT vs. US) via the hypothesized mediator (change in mindfulness as measured by FFMQ scores from preintervention to postintervention) on change in health anxiety (change in SHAI scores from preintervention to postintervention) to determine the statistical significance of the indirect effect (MacKinnon et al., 2004; Preacher & Hayes, 2008). The total indirect effect of group on health anxiety was significant, Z = −2.20, p = .028, and the true indirect effect was estimated to lie between −3.49 and −0.57 with 95% CI. Because zero is not in the 95% CI, it can be concluded that the indirect effect is significantly different from zero at p < .05 and, thus, that change in mindfulness mediated the relationship between group (MBCT vs. US) and change in health anxiety. The direct effect of group was not significant (p = .49). The reverse model was also tested, wherein change in mindfulness would be mediated by changes in health anxiety (which would not be predicted by the theoretical model of change). The same nonparametric resampling method was used but with change in mindfulness as the dependent variable and change in health anxiety as the mediator in the model. The total indirect effect was not significant, Z = 1.59, p = .11, and the true indirect effect was estimated to lie between −0.19 and 6.40 with 95% CI. Because zero is in the 95% CI, it can be concluded that the indirect effect is not significantly different from zero at p < .05 and that, in line with expectations, change in health anxiety did not mediate the relationship between group (MBCT vs. US) and change in mindfulness. In line with this finding, the direct effect of group in this model was significant (p = .03).
Discussion
The present study is the first randomized controlled trial examining the impact of MBCT on health anxiety. One previous pilot study (Lovas & Barsky, 2010 [N = 10]) and a qualitative study (Williams et al., 2011 [N = 9]) both reported positive impacts and acceptability, but the conclusions that can be drawn from these studies are limited by their uncontrolled designs and small sample sizes. The present study compared the impact of MBCT in addition to usual (unrestricted) services (US) with US alone in a relatively chronic sample of patients diagnosed with hypochondriasis. In addition to meeting diagnostic criteria for hypochondriasis, almost half of the participants met criteria for another psychiatric disorder, and over half had previously received psychological treatment for an emotional problem other than health anxiety. Furthermore, almost half of the participants had had previous psychological treatment for health anxiety, and 41.0% were currently taking psychotropic medication.
While there were no significant differences between the MBCT and US groups in levels of general anxiety or depression, or in the number or presence of comorbid diagnoses, the composite measure of health anxiety showed that the MBCT group's score was significantly lower than the US group's, both immediately following the intervention period and at the 1-year follow-up. This suggests that the MBCT intervention, adapted to focus on symptoms of health anxiety, added significant advantage to US in terms of reducing symptoms of health anxiety. The magnitude of change on measures of health anxiety found here is similar to that reported in Lovas and Barsky's (2010) pilot study of MBCT for hypochondriasis, and the effect sizes (ds) fall within the range 0.28–0.78 reported in Vøllestad, Sivertsen, and Høstmark's (2011) trial of MBCT versus waitlist for anxiety disorders. However, it is also worth noting that while symptoms of general anxiety and depression improved over time, there was no significant advantage of MBCT over US for either general anxiety or depression. This is in contrast to previous studies showing MBCT to have a significant positive impact on depression and anxiety symptoms (e.g., see Hofmann et al., 2010, for a review). This may be due to the MBCT program being adapted to focus on symptoms of hypochondriasis or to lower power to detect differences in these symptoms as there was greater variability in participants' levels of depression and general anxiety. However, future research should examine carefully the issue of generic versus specific changes when the MBCT protocol is adapted to focus on a specific condition.
As regards the impact on health anxiety symptoms, in comparison to those who had received US alone, significantly fewer participants who received the MBCT intervention met criteria for the diagnosis of hypochondriasis, both immediately following the intervention and at 1-year follow-up. In the ITT sample, 50.0% of MBCT participants no longer met diagnostic criteria for hypochondriasis immediately following the intervention, and this increased to 63.9% by the 1-year follow-up, as compared with rates of 21.1% at postintervention and 23.7% at 1-year follow-up in the US group. In the PP sample, 52.9% of MBCT participants no longer met criteria for hypochondriasis immediately following the intervention, and this increased to 71.9% by the 1-year follow-up, as compared with rates of 21.6% and 25.0%, respectively, in the US group.
A criticism of previous trials is that the better outcomes achieved by the active treatment might have been due to the nonspecific effects of therapy. However, our analysis showed that there were large and significant changes in the supposed mediator of change (mindfulness) that were maintained at 1-year follow-up. Mediational analysis showed that these changes in mindfulness significantly mediated the group changes in health anxiety, whereas the reverse analysis (whereby changes in health anxiety would mediate changes in mindfulness) was not significant.
The MBCT treatment seemed highly acceptable to those participants who entered into the trial, in that all 34 of the participants who began the MBCT treatment continued through to the postintervention assessment. However, two of the 36 participants allocated to MBCT did not take up the intervention. Of the 34 participants who did attend the classes, attendance was good, with participants attending an average of 6.5 out of eight sessions. While it is encouraging that there was little drop out once the intervention had been initiated, it is also worth noting that 37 potential participants (22.7% of those telephone screened or assessed) declined either further assessment or inclusion in the study. These patients' refusal could have many reasons (e.g., the patient did not wish to participate in a research trial, or the patient accessed alternative treatment elsewhere), and it is not possible to know whether the acceptability of the intervention was a factor in this. However, it is encouraging that 91.4% of the 81 participants assessed as eligible for participation in the study entered into the trial and that the overall attrition rate from MBCT was less than 6%, which is noticeably lower than rates reported in some other studies of psychological treatments of health anxiety (e.g., 25.0% from CBT in Greeven et al., 2007, and 28.2% from cognitive therapy or exposure and response prevention in Visser & Bouman, 2001).
The surprising element of these results is that mindfulness interventions involve focusing on the body, and yet such bodily focus is seen as one of the primary maintaining factors in health anxiety. On the face of it, MBCT should make people feel worse. However, the theory on which MBCT is based distinguishes two modes of self-focus (Williams, 2008). In the first problem-solving (doing) mode, a person attends to external or internal stimuli through representations (thoughts or images), with the motivation to change the current state being the highest priority using standard discrepancy-based processing. Such motivation drives two “slave” processes—rumination and avoidance—both of which are intended to help reduce the perceived discrepancy between current and desired state but which actually increase the discrepancy, leading to a rapid escalation of distress. MBCT teaches patients to see these maladaptive patterns as they begin and then to “decenter” from them, switching instead into an experiential mode in which the thoughts and body sensations are seen as passing events.
The positive outcomes reported should be viewed within the limitations of the study. Participants were predominantly female, highly educated, and White. While this is not the case in all studies of patients with hypochondriasis, other trials of psychological treatments for hypochondriasis have also reported more than 70% of participants to be female and White (e.g., 74.5–78.8% female and 70.6–74.1% White in Barsky & Ahern, 2004, and 76.4% female and 72.0% White in Nakao et al., 2011). In addition, the group nature of the MBCT-based intervention meant that there was a delay between being assessed for inclusion in the study and the time at which sufficient numbers had been recruited to allocate participants to a MBCT group and equivalent numbers to US, which meant that participants had a variable length of delay between the initial assessment and commencement of the MBCT/US period. However, the mean length of delay was not different between those allocated to MBCT or US, so it is unlikely that this could have accounted for the differences between the groups found at the postintervention assessment. A further limitation is that in order to complete the trial within time scales, the sample was actively recruited, with 33.8% of participants self-referring in response to advertisements and 31.1% initiating contact at the suggestion of their general practitioner. Self-referral rates in the current study are consistent with those reported for other trials of psychological treatments for hypochondriasis (e.g., 57.2% in Barsky & Ahern's 2004 trial of CBT for hypochondriasis), and the sample appears to be comparable to other samples of patients diagnosed with hypochondriasis in terms of having comparable scores on standardized measures of health anxiety, a mean duration of the current episode of over 8 years, and high rates of comorbidity and of previous treatment. Nevertheless, as noted by Lovas and Barsky (2010), it remains a priority to investigate the dissemination of such novel treatment procedures into routine clinical practice. A final important limitation of the current study is that it employed only a US control as the first step to establishing whether MBCT has a role to play in a diagnosis in which excessive focus on the body is central. It will be a priority for future studies to compare the impact of MBCT with alternative interventions that are matched for therapist time and attention and to compare the comparative cost effectiveness of different approaches to treating health anxiety. Despite these limitations, this trial provides reason for optimism that the effects of MBCT are mediated by change in the mechanisms hypothesized to underlie it and that MBCT has potential as an adjunctive class-based psychological approach to treating severe health anxiety.
Acknowledgments
We are grateful to the Lupina Foundation for funding the current study and to Christie Leung and Marco Cheng for help with data collection and entry. J. Mark G. Williams is supported by Programme Grant G067797 from the Wellcome Trust.
Footnotes
The PP analysis excluded the three participants who discontinued participation at postintervention (N = 71) and the additional three who discontinued at 1-year follow-up (N = 68, 91.9%).
Hierarchical linear modeling (HLM) is an alternative method for analyzing longitudinal data, and HLM analyses revealed a similar pattern to the ANOVAs/multivariate analyses of variance reported here, with improvement over time in both groups and significantly lower scores or percentages on health anxiety measures, but not general measures of anxiety and depression, in the MBCT group.
Group (MBCT vs. US) × Time (preintervention vs. postintervention vs. 1-year follow-up) repeated-measures multivariate analyses of variance on the measures of health anxiety (Short Health Anxiety Inventory and Whitely Index scores and assessor's ratings of interference and distress) showed an identical pattern of results (ITT analysis N = 74): a significant effect of time, F(8, 65) = 13.86, p < .001, η2 = .63, and a significant interaction between time and group, F(8, 65) = 2.28, p = .03, η2 = .22. See Table 2 for results of univariate repeated-measures ANOVAs on the individual measures.
References
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Washington, DC: Authors. [Google Scholar]
- Baer R. A., Smith G. T., Lykins E., Button D., Krietemeyer J., Sauer S., . . . Williams J. M. G. (2008). Construct validity of the Five Facet Mindfulness Questionnaire in meditating and non-meditating samples. Assessment, 15, 329–342. doi:10.1177/1073191107313003 [DOI] [PubMed] [Google Scholar]
- Barnhofer T., Crane C., Hargus E., Amarasinghe M., Winder R., & Williams J. M. G. (2009). Mindfulness-based cognitive therapy for chronic depression: A preliminary study. Behaviour Research and Therapy, 47, 366–373. doi:10.1016/j.brat.2009.01.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barsky A. J., & Ahern D. K. (2004). Cognitive behavior therapy for hypochondriasis. A randomized trial. Journal of the American Medical Association, 291, 1464–1470. doi:10.1001/jama.291.12.1464 [DOI] [PubMed] [Google Scholar]
- Barsky A J., Ettner S., Horsky J., & Bates D. (2001). Resource utilization of patients with hypochondriacal health anxiety and somatization. Medical Care, 39, 705–715. doi:10.1097/00005650-200107000-00007 [DOI] [PubMed] [Google Scholar]
- Beck A. T., Epstein N., Brown G., & Steer R. A. (1988). An inventory for measuring clinical anxiety: Psychometric properties. Journal of Consulting and Clinical Psychology, 56, 893–897. [DOI] [PubMed] [Google Scholar]
- Beck A. T., & Steer R. A. (1993). Beck Anxiety Inventory manual. San Antonio, TX: Psychological Corporation. [Google Scholar]
- Beck A. T., Steer R. A., & Brown G. K. (1996). Manual for the Beck Depression Inventory–II. San Antonio, TX: Psychological Corporation. [Google Scholar]
- Buwalda F. M., Bouman T., & van Duijn M. (2007). Psychoeducation for hypochondriasis: A comparison of a cognitive-behavioural approach and a problem–solving approach. Behaviour Research and Therapy, 45, 887–899. doi:10.1016/j.brat.2006.08.004 [DOI] [PubMed] [Google Scholar]
- Clark D. M., Ehlers A., Hackmann A., McManus F., Fennell M., Grey N., . . . Wild J. (2006). Cognitive therapy versus exposure and applied relaxation in social phobia: A randomized controlled trial. Journal of Consulting and Clinical Psychology, 74, 568–578. doi:10.1037/0022-006X.74.3.568 [DOI] [PubMed] [Google Scholar]
- Clark D. M., Ehlers A., McManus F., Hackmann A., Fennell M., Campbell H., . . . Louis B. (2003). Cognitive therapy versus fluoxetine in generalized social phobia: A randomized placebo-controlled trial. Journal of Consulting and Clinical Psychology, 71, 1058–1067. doi:10.1037/0022-006X.71.6.1058 [DOI] [PubMed] [Google Scholar]
- Clark D. M., Salkovskis P. M., Hackmann A., Wells A., Fennell M., Ludgate J., . . . Gelder M. (1998). Two psychological treatments for hypochondriasis. A randomised controlled trial. British Journal of Psychiatry, 173, 218–225. doi:10.1192/bjp.173.3.218 [DOI] [PubMed] [Google Scholar]
- Creed F., & Barsky A. J. (2004). A systematic review of the epidemiology of somatisation disorder and hypochondriasis. Journal of Psychosomatic Research, 56, 391–408. doi:10.1016/S0022-3999(03)00622-6 [DOI] [PubMed] [Google Scholar]
- First M. B., Spitzer R. L., Gibbon M., & Williams J. B. W. (2002). User's guide for the Structured Clinical Interview for DSM–IV–TR Axis I disorders–Research version, patient edition (SCID-I/P). New York: Biometrics Research Department, New York State Psychiatric Institute. [Google Scholar]
- Greeven A., van Balkom A. J., Visser S., Merkelbach J. W., van Rood Y. R., van Dyck R., . . . Spinhoven P. (2007). Cognitive behavior therapy and paroxetine in the treatment of hypochondriasis: A randomized controlled trial. The American Journal of Psychiatry, 164, 91–99. doi:10.1176/appi.ajp.164.1.91 [DOI] [PubMed] [Google Scholar]
- Gureje O., Üstun T. B., & Simon G. E. (1997). The syndrome of hypochondriasis: A cross-national study in primary care. Psychological Medicine, 27, 1001–1010. doi:10.1017/S0033291797005345 [DOI] [PubMed] [Google Scholar]
- Hargus E., Crane C., Barnhofer T., & Williams J. M. G. (2010). Effects of mindfulness on meta-awareness and specificity of describing prodromal symptoms in suicidal depression. Emotion, 10, 34–42. doi:10.1037/a0016825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes A. F. (n.d.). My macros and code for SPSS and SAS. Retrieved July 13, 2011, from http://www.afhayes.com/spss-sas-and-mplus-macros-and-code.html [Google Scholar]
- Heeren A., & Philippot P. (2011). Changes in ruminative thinking mediate the clinical benefits of mindfulness: Preliminary findings. Mindfulness, 2, 8–13, doi:10.1007/s12671-010-0037-y [Google Scholar]
- Hofmann S. G., Sawyer A. T., Witt A. A., & Oh D. (2010). The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. Journal of Consulting and Clinical Psychology, 78, 169–183. doi:10.1037/a0018555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuyken W., Byford S., Taylor R. S., Watkins E., Holden E., White K., . . . Teasdale J. D. (2008). Mindfulness-based cognitive therapy to prevent relapse in recurrent depression. Journal of Consulting and Clinical Psychology, 76, 966–978. doi:10.1037/a0013786 [DOI] [PubMed] [Google Scholar]
- Kuyken W., Watkins E., Holden E., White K., Taylor R. S., Byford S., . . . Dalgleish T. (2010). How does mindfulness-based cognitive therapy work? Behaviour Research and Therapy, 48, 1105–1112. doi:10.1016/j.brat.2010.08.003 [DOI] [PubMed] [Google Scholar]
- Lovas D. A., & Barsky A. J. (2010). Mindfulness-based cognitive therapy for hypochondriasis, or severe health anxiety: A pilot study. Journal of Anxiety Disorders, 24, 931–935. doi:10.1016/j.janxdis.2010.06.019 [DOI] [PubMed] [Google Scholar]
- MacKinnon D. P., Lockwood C. M., & Williams J. (2004). Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research, 39, 99–128. doi:10.1207/s15327906mbr3901_4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcus D. K., Hughes K. T., & Arnau R. C. (2008). Health anxiety, rumination, and negative affect: A mediational analysis. Journal of Psychosomatic Research, 64, 495–501. doi:10.1016/j.jpsychores.2008.02.004 [DOI] [PubMed] [Google Scholar]
- McManus F., Muse K., & Surawy C. (2011). Mindfulness- based cognitive therapy (MBCT) for severe health anxiety: An overview of principles and practices. Healthcare Counselling and Psychotherapy Journal, 11, 19–23. [Google Scholar]
- Michalak J., Hölz A., & Teismann T. (2011). Rumination as a predictor of relapse in mindfulness-based cognitive therapy for depression. Psychology and Psychotherapy: Theory, Research and Practice, 84, 230–236. doi:10.1348/147608310X520166 [DOI] [PubMed] [Google Scholar]
- Mykletun A., Heradstveit O., Eriksen K., Glozier N., Øverland S., Maeland J. G., & Wilhelmsen I. (2009). Health anxiety and disability pension award: The HUSK Study. Psychosomatic Medicine, 71, 353–360. doi:10.1097/PSY.0b013e31819cc772 [DOI] [PubMed] [Google Scholar]
- Nakao M., Shinozaki Y., Ahern D. K., & Barsky A. J. (2011). Anxiety as a predictor of improvements in somatic symptoms and health anxiety associated with cognitive–behavioral intervention in hypochondriasis. Psychotherapy and Psychosomatics, 80, 151–158. doi:10.1159/000320122 [DOI] [PubMed] [Google Scholar]
- Noyes R., Kathol R. G., Fisher M. M., Phillips B. M., Suelzer M. T., & Woodman C. L. (1994). One-year follow-up of medical outpatients with hypochondriasis. Psychosomatics, 35, 533–545. doi:10.1016/S0033-3182(94)71722-9 [DOI] [PubMed] [Google Scholar]
- Olde Hartman T. C., Borghuis M. S., Lucassen P. L. B. J., van de Laar F. A., Speckens A. E., & van WeeL C. V. (2009). Medically unexplained symptoms, somatisation disorder, and hypochondriasis: Course and prognosis. A systematic review. Journal of Psychosomatic Research, 66, 363–377. doi:10.1016/j.jpsychores.2008.09.018 [DOI] [PubMed] [Google Scholar]
- Papageorgiou C., & Wells A. (1998). Effects of attention training on hypochondriasis: A brief case series. Psychological Medicine, 28, 193–200. doi:10.1017/S0033291797005825 [DOI] [PubMed] [Google Scholar]
- Piet J., & Hougaard E. (2011). The effect of mindfulness-based cognitive therapy for prevention of relapse in recurrent major depressive disorder: A systematic review and meta-analysis. Clinical Psychology Review, 31, 1032–1040. doi:10.1016/j.cpr.2011.05.002 [DOI] [PubMed] [Google Scholar]
- Pilowsky I. (1967). Dimensions of hypochondriasis. The British Journal of Psychiatry, 113, 89–93. doi:10.1192/bjp.113.494.89 [DOI] [PubMed] [Google Scholar]
- Pocock S. J. (1983). Clinical trials: A practical approach. Chichester, England: Wiley. [Google Scholar]
- Preacher K. J., & Hayes A. F. (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behaviour Research Methods, 40, 879–891. doi:10.3758/BRM.40.3.879 [DOI] [PubMed] [Google Scholar]
- Raes F., Dewulf D., van Heeringen C., & Williams J. M. G. (2009). Mindfulness and reduced cognitive reactivity to sad mood: Evidence from a correlational study and a non-randomized waiting list controlled study. Behaviour Research and Therapy, 47, 623–627. doi:10.1016/j.brat.2009.03.007 [DOI] [PubMed] [Google Scholar]
- Rassin E., Muris P., Franken I., & van Straten M. (2008). The feature-positive effect and hypochondriacal concerns. Behaviour Research and Therapy, 46, 263–269. doi:10.1016/j.brat.2007.11.003 [DOI] [PubMed] [Google Scholar]
- Rosenthal R., & Rosnow R. L. (1991). Essentials of behavioral research: Methods and data analysis (2nd ed.). New York, NY: McGraw-Hill. [Google Scholar]
- Salkovskis P. M., Rimes K. A., Warwick H. M. C., & Clark D. M. (2002). The Health Anxiety Inventory: Development and validation of scales for the measurement of health anxiety and hypochondriasis. Psychological Medicine, 32, 843–853. doi:10.1017/S0033291702005822 [DOI] [PubMed] [Google Scholar]
- Segal Z. V., Bieling P., Young T., MacQueen G., Cooke R., Martin L., . . . Levitan R. D. (2010). Antidepressant monotherapy vs. sequential pharmacotherapy and mindfulness-based cognitive therapy, or placebo, for relapse prophylaxis in recurrent depression. Archives of General Psychiatry, 67, 1256–1264. doi:10.1001/archgenpsychiatry.2010.168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segal Z. V., Teasdale J. T., Williams J. M. G., & Gemar M. C. (2002). The Mindfulness-Based Cognitive Therapy Adherence Scale: Inter-rater reliability, adherence to protocol, and treatment distinctiveness. Clinical Psychology & Psychotherapy, 9, 131–138. doi:10.1002/cpp.320 [Google Scholar]
- Segal Z. V., Williams J. M. G., & Teasdale J. D. (2002). Mindfulness-based cognitive therapy for depression: A new approach to preventing relapse. London, England: Guilford Press. [Google Scholar]
- Taylor S. T., & Asmundson G. J. G. (2004). Appendix 1: Health Anxiety Interview. In Treating health anxiety: A cognitive–behavioral approach (pp. 245–249). New York, NY: Guilford Press. [Google Scholar]
- Teasdale J. D., Segal Z., & Williams J. M. G. (1995). How does cognitive therapy prevent depressive relapse and why should attentional control (mindfulness) training help. Behavior Research and Therapy, 33, 25–39. doi:10.1016/0005-7967(94)E0011–7 [DOI] [PubMed] [Google Scholar]
- Teasdale J. D., Segal Z., Williams J. M. G., Ridgeway V. A., Soulsby J. M., & Lau M. A. (2000). Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. Journal of Consulting and Clinical Psychology, 68, 615–923. doi:10.1037/0022-006X.68.4.615 [DOI] [PubMed] [Google Scholar]
- Thomson A. B., & Page L. A. (2007). Psychotherapies for hypochondriasis. Cochrane Database of Systematic Reviews, 4, 1–43. doi:10.1002/14651858.CD006520.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Visser S., & Bouman T. K. (2001). The treatment of hypochondriasis: Exposure plus response prevention vs. cognitive therapy. Behaviour Research and Therapy, 39, 423–442. doi:10.1016/S0005-7967(00)00022-X [DOI] [PubMed] [Google Scholar]
- Vøllestad J., Sivertsen B., & Høstmark G. H. (2011). Mindfulness-based stress reduction for patients with anxiety disorders: Evaluation in a randomized controlled trial. Behaviour Research and Therapy, 49, 281–288. doi:10.1016/j.brat.2011.01.007 [DOI] [PubMed] [Google Scholar]
- Walker J., Vincent N., Furere P., Cox B., & Kjernisted K. (1999). Treatment preference in hypochondriasis. Journal of Behavior Therapy and Experimental Psychiatry, 30, 251–258. doi:10.1016/S0005-7916(99)00027-0 [DOI] [PubMed] [Google Scholar]
- Warwick H. M. C., & Salkovskis P. M. (1990). Hypochondriasis. Behaviour, Research and Therapy, 28, 105–117. doi:10.1016/0005-7967(90)90023-C [DOI] [PubMed] [Google Scholar]
- Wattar U., Sorensen P., Buemann I., Birket-Smith M., Salkovskis P. M., Albertsen M., & Strange S. (2005). Outcome of cognitive-behavioural treatment for health anxiety (hypochondriasis) in a routine clinical setting. Behavioural and Cognitive Psychotherapy, 33, 165–175. doi:10.1017/S1352465804002000 [Google Scholar]
- Welch P. G., Carleton R. N., & Asmundson G. J. G. (2009). Measuring health anxiety: Moving past the dichotomous response option of the original Whiteley Index. Journal of Anxiety Disorders, 23, 1002–1007. doi:10.1016/j.janxdis.2009.05.006 [DOI] [PubMed] [Google Scholar]
- Williams J. M. G. (2008). Mindfulness, depression, and modes of mind. Cognitive Therapy and Research, 32, 721–733. doi10.1007/s10608-008-9204-z [Google Scholar]
- Williams M. J., McManus F., Muse K., & Williams J. M. G. (2011). Mindfulness-based cognitive therapy for severe health anxiety (hypochondriasis): An interpretative phenomenological analysis of patients' experiences. British Journal of Clinical Psychology, 50, 379–397. doi:10.1111/j.2044-8260.2010.02000.x [DOI] [PubMed] [Google Scholar]
- World Health Organization. (1992). The ICD–10 classification of mental and behavioural disorders: Clinical descriptions and diagnostic guidelines. Geneva, Switzerland: Author. [Google Scholar]