Abstract
Background
Physician counselling may help patients increase physical activity, improve nutrition and lose weight. However, physicians have low outcome expectations that patients will change. The aims are to describe the accuracy of physicians' outcome expectations about whether patients will follow weight loss, nutrition and physical activity recommendations. The relationships between physician outcome expectations and patient motivation and confidence also are assessed.
Methods
This was an observational study that audio recorded encounters between 40 primary care physicians and 461 of their overweight or obese patients. We surveyed physicians to assess outcome expectations that patients will lose weight, improve nutrition and increase physical activity after counselling. We assessed actual patient change in behaviours from baseline to 3 months after the encounter and changes in motivation and confidence from baseline to immediately post-encounter.
Results
Right after the visit, ∼55% of the time physicians were optimistic that their individual patients would improve. Physicians were not very accurate about which patients actually would improve weight, nutrition and physical activity. More patients had higher confidence to lose weight when physicians thought that patients would be likely to follow their weight loss recommendations.
Conclusions
Physicians are moderately optimistic that patients will follow their weight loss, nutrition and physical activity recommendations. Patients might perceive physicians' confidence in them and thus feel more confident themselves. Physicians, however, are not very accurate in predicting which patients will or will not change behaviours. Their optimism, although helpful for patient confidence, might make physicians less receptive to learning effective counselling techniques.
Keywords: Counselling, outcome expectations, physicians, weight loss
Over 60% of Americans are overweight or obese.1 Physician counselling may help patients increase physical activity, improve nutrition and lose weight.2–6 Unfortunately, few physicians are trained how to counsel and thus, tend to have low outcome expectations for their counselling.7–9 Outcome expectations and self-efficacy are a key components of social cognitive theory,10 which explains behaviour as the reciprocal interaction of the person and his/her environment. Self-efficacy, confidence to counsel about weight, and outcome expectations, the belief that counselling will improve patient health, affect whether and how physicians counsel.11,12 Physicians who have low outcome expectations may not counsel at all, may do so in a cursory manner or may use a tone that conveys their lack of expectation. In a reciprocal manner as suggested by social cognitive theory, physician low outcome expectations can lead to patients being less likely to improve their behaviours, which then confirms physicians' low outcome expectations and in essence becomes a self-fulfilling prophecy.
Physician outcome expectations for specific patients following recommendations are understudied; most researchers have surveyed physicians about their patients in general, not about patients immediately after an office visit. None has examined whether physician outcome expectations are accurate. Namely, when physicians think patients will change, do they actually change or if they do not think patient will change, do they not change? Accurate outcome expectations might indicate better insight among physicians of the efficacy of their counselling. Inaccurate outcome expectations might indicate reliance on stereotypes about certain patients.13
The aims of this paper are to (i) examine physicians' outcome expectations about whether their overweight and obese patients will follow their recommendations to lose weight, improve nutrition and increase physical activity; (ii) examine the association of physicians' outcome expectations with actual patient weight loss, improvement in nutrition, increases in physical activity, increases in motivation and increases in confidence and (iii) examine the association of physicians' outcome expectations and patient changes in motivation and confidence to lose weight, improve nutrition and increase physical activity.
Methods
Recruitment
Project CHAT (Communicating Health: Analyzing Talk) was approved by the Duke University Medical Center IRB. Methods are described in detail elsewhere.2 In brief, 40 primary care physicians were told that the study would examine how they address disease prevention with their patients, not about weight specifically. Physicians gave written consent, completed a baseline questionnaire, had 11–12 encounters audio recorded and completed post-encounter questionnaires.
Study staff identified patients who had appointments at least 3 weeks in advance to exclude acute visits. Staff sent patients a letter signed by the patient's physician. In the letter, patients were informed that the study was about how physicians discuss disease prevention, not weight specifically. Staff called patients who did not refuse via calling an 800 number. Staff obtained verbal consent, screened patients and administered a telephone survey. Patients were >18 years old, English speaking, not pregnant and had a body mass index (BMI) >25. At the visit, patients provided written consent. Staff assessed patient weight and vital signs immediately and 3 months after the encounter.
Outcomes
Patient outcomes.
We assessed patient weight, nutrition and physical activity at baseline and 3 months after the encounter. With single item measures, we assessed motivation and confidence to lose weight, improve nutrition and increase physical activity at baseline and immediately after the encounter. To mask the focus on weight, these same measures were assessed for smoking and alcohol use; only 7 of the 461 patients guessed the study was about weight.
Weight.
Weight was assessed on a calibrated scale with shoes, outwear and pocket contents removed.
Nutrition.
Nutrition was assessed using the 22-item Fat- and Fibre-related Diet Behavior Questionnaire.14,15 Questions about frequency of food selections included: ‘When you ate dessert, how often did you eat only fruit?’ and ‘When you ate chicken, how often did you take off the skin?’ Responses were averaged into a total score where ‘1’ reflected higher fibre, lower fat food choices and a score of ‘4’ reflected lower fibre, higher fat choices (Cronbach’s α = 0.74 at baseline and α = 0.77 at 3-month follow-up). Patients were considered to have improved their nutrition significantly if they decreased their overall fat and fibre score by ≥0.2 points. In this 22-item scale, this represents a small, yet meaningful change in at least one fat- or fibre-related eating behaviour. As fat contains twice as many calories as protein or carbohydrates, changes in fat reduction of this magnitude could result in significant weight change. For example, responses going from ‘sometimes’ to ‘always’ for just three questions: (i) eating bread/rolls ‘without butter or margarine’, (ii) eating low-fat cheese and (iii) drinking non-fat or 1% milk would reduce the summary score by 0.22. The caloric equivalent of this score could be interpreted as a reduction of ∼5719 cal (or 1.5 pounds) per month [(change from 2% to non-fat milk = −30 kcal, no butter = −100 kcal, regular to reduced fat cheese = −60 kcal) = −190 cal/day = −1330 cal/week = −5719 cal/month].
Physical activity.
Physical activity was measured using the Framingham physical activity index.16 Participants recalled the average number of hours spent engaged in various levels of occupational and leisure activity (sleep, sedentary, slight, moderate and heavy) over a 24-hour period. From this, we estimated energy expenditure in metabolic equivalent of task (MET)-minutes (range 1440–7200). A score of 1440 represents 24 hours of sleep, while 7200 is 24 hours of heavy activity, such as running. Consistent with others,17,18 we categorized patients as having clinically significant changes in physical activity level if they showed an improvement of at least 5 METS hours/week. A change of this magnitude is the equivalent of adding ∼1 hour of brisk walking or a 30-minute jog/week.19
Motivation.
Motivation was assessed using a 7-level Likert scale with the following question: ‘With 1 being “not at all” and 7 being “very much,” how much do you want to lose weight at this time?’
Confidence.
Confidence was assessed with a 5-level Likert scale: ‘With 1 being “not at all” and 5 being “very much,” how confident are you that you can lose weight at this time?’ Motivation and confidence to improve nutrition and increase exercise were measured similarly. Because of skewness and little variability in motivation and confidence scores, baseline and post-visit motivation and confidence scores were dichotomized for analysis as follows: motivated (5–7) or not motivated (1–4); confident (4–5) or not confident (1–3).
Outcome expectations.
After each encounter, physicians reported whether they discussed weight loss, nutrition and physical activity (among other topics like smoking and alcohol to mask the focus on weight; only one of 40 physicians guessed the study was about weight). They also were asked three questions, one for each topic, ‘How likely will the patient follow your (weight loss/nutrition/physical activity) recommendations as a result of your discussion?’ (1 = not at all likely; 5 = extremely likely).
Accuracy of outcome expectations.
To create the accuracy outcome for weight, nutrition and physical activity discussions, outcome expectations were dichotomized into 1–3 versus 4–5 (‘likely’ or ‘extremely likely’). Patients were considered to have lost a clinically significant amount of weight if they lost >1 kg at the 3-month follow-up.20 A >1 kg change in weight over 3 months is what the primary analysis of this study was powered to detect. Patients were considered to have improved nutrition if they reduced their fat and fibre scale by 0.2; to have increased physical activity if their score increased by 5 points. ‘Accurate’ was defined for each behaviour (weight loss, nutrition and physical activity) as physician predicted patient would follow weight loss recommendations AND patient lost >1 kg; would follow nutrition recommendation AND decreased fat and fibre score by ≥0.2 or would follow physical activity recommendation AND physical activity increased by ≥5 points OR physician said patient would not follow weight loss recommendations AND patient did not lose >1 kg; would not follow nutrition recommendations AND fat and fibre score decreased <0.2 points or would not follow physical activity recommendations AND physical activity score increased <5 points. Any other combinations of outcome expectation and change in behaviour were considered ‘inaccurate’.
Covariates assessed at baseline
Patient level.
Gender, age, race, co-morbidities (diabetes, hypertension, arthritis and hyperlipidaemia), high school education, economic security, overweight (BMI 25.0–29.9) or obese (BMI ≥ 30), actively trying to lose weight, comfortable discussing weight, motivated to lose weight, improve nutrition or increase physical activity and confident about losing weight, improving nutrition or increasing physical activity.
Physician level.
Gender, race, years since medical school, specialty (family versus internal medicine), self-efficacy about weight counselling, barriers to weight counselling, comfort discussing weight, insurance reimbursement concerns and prior training in behavioural counselling. ‘Confidence’ (four items): sample item, ‘How confident are you that you can advise patients to lose weight?’ (1 = not at all confident to 5 = extremely confident, scored mostly/extremely versus other); α = 0.78. ‘Comfort’ (one item), ‘In your previous visits, how comfortable have you been discussing weight?’ (1 = very uncomfortable to 5 = very comfortable, scored very comfortable versus other). ‘Outcome expectations’ (three items): sample item is, ‘Your overweight or obese patients will listen to your healthy weight advice’ (1 = not at all likely to 5 = extremely likely, scored very/extremely likely versus other); α = 0.76. ‘Barriers’ (five items): sample items are ‘too much time is required’ and ‘overweight or obese patients may not be interested in discussing weight’ (1 = strongly agree and 5 = strongly disagree, scored agree/strongly agree versus other); α = 0.72.
Visit level.
Minutes spent addressing weight issues, explicit discussion of patient BMI (i.e. physician said ‘weight’), type of visit (preventive or chronic) and who initiated the weight discussion (coded from audio recordings, Kappa = 0.1.0).
Analyses
Analyses were performed using SAS v. 9.2 (SAS Institute, Inc.). Descriptive statistics of outcome expectations and accuracy of outcome expectations were calculated by physician. Using linear mixed models,21 we adjusted for physician clustering to examine the association between outcome expectation and each patient outcome of 3-month weight change, nutrition change or physical activity change in the full sample (n = 461). In the mixed model, a physician random effect was used to account for extra variance due to patients having more similar weight, nutrition or physical activity changes when they saw the same physician. For this analysis, an outcome expectation variable with three categories was used that included a category for ‘no discussion of topic’ depending on which outcome we were examining and then the dichotomization of the outcome expectation for each of the behaviours: 1–3 versus 4–5 (‘likely’ or ‘extremely likely’ to follow recommendations). In these models, we included baseline outcome and variables that were defined a priori at the patient (e.g. age, gender, race), physician (e.g. gender, specialty, years since medical school) and visit level (e.g. type of visit). We examined the association between the dichotomous outcomes post-visit motivation and confidence and each of the three-level outcome expectation variables described above using generalized estimating equation models22 adjusting for clustering and including baseline motivation and/or confidence variables for either weight loss, nutrition or physical activity and patient, physician and visit level factors.
Results
Outcome expectations
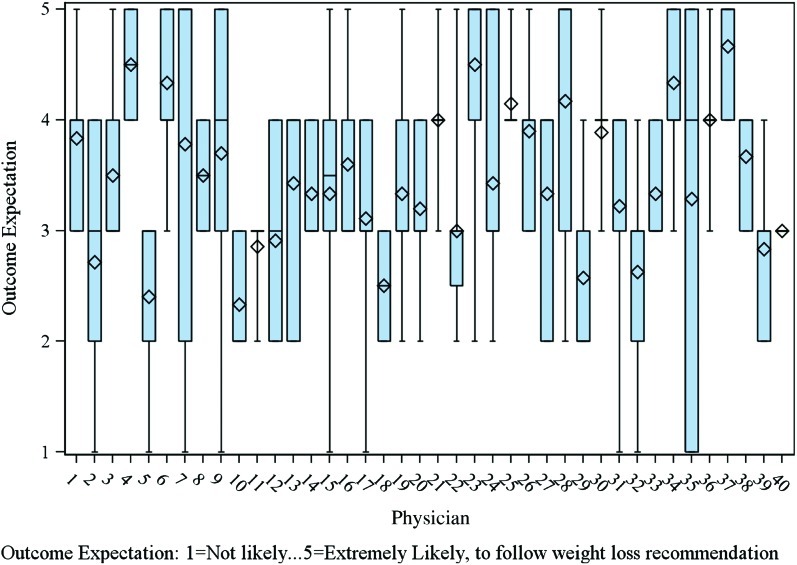
Table 1 lists sample characteristics. The mean rates of physicians discussing weight, nutrition and exercise in encounters were 58% (range 17–92%; SD = 20%), 63% (range 18–100%; SD = 21%) and 74% (range 8–100%; SD = 18%), respectively. In encounters when physicians discussed weight loss, nutrition or physical activity, the mean rates of physician outcome expectations that patients were likely or extremely likely to follow weight loss, nutrition and physical activity recommendations were each ∼55%. The mean outcome expectation (SD) for following weight loss recommendation per physician was 3.5 (0.6) with means ranging from 2.3 to 4.7 on the 1–5 scale (Fig. 1). The distribution of outcome expectations for nutrition and physical activity followed similar patterns as shown for weight in Figure 1. Similarly, for encounters with weight, nutrition or physical activity discussion, physicians outcome expectations about whether patients would follow the specific recommendations for weight, nutrient or physical activity were more similar within physicians than between physicians [Intraclass Correlation Coefficient (ICC) = 0.20 for weight, ICC = 0.16 for nutrition and ICC = 0.16 for physical activity]. At baseline, when asked whether ‘their’ overweight and obese patients would follow their weight loss recommendations, using the same scale, only 8% said very or extremely likely. Physicians had equally low outcome expectations for patients following their nutrition and physical activity advice, 8% and 8%, respectively.
Table 1.
Patient and physician characteristics for total sample and sample of patients that physicians reported a discussion of weight
| Patients | Total (N = 461); M (SD) or % (N) |
| Baseline weight (kg) | 91.7 (21.1) |
| Obese (BMI ≥ 30) | 54% (248) |
| Race | |
| White/Asian | 65% (300) |
| African American | 35% (161) |
| Male | 34% (158) |
| Age | 59.8 (13.9) |
| More than high school education (missing = 1, 1)a | 67% (306) |
| Economic security: pay bills easily (missing = 13, 7) | 86% (387) |
| Medical history | |
| Diabetes | 31% (142) |
| Hypertension (missing = 1, 0) | 69% (316) |
| Hyperlipidaemia (missing = 1, 1) | 56% (257) |
| Arthritis | 47% (215) |
| Very motivated to lose weight versus somewhat to not at allb | 52% (241) |
| Very confident can lose weight versus somewhat to not at all confident (missing = 1, 0)c | 36% (165) |
| Very comfortable discussing weight with MD versus somewhat to not at all (missing = 1, 0)d | 76% (350) |
| Tried to lose weight in past month | 47% (217) |
| Visit factors | |
| Total patient-medical personnel in room time (minutes) | 25.4 (10.3) |
| Total time spent discussing weight (minutes) (missing = 15, 0) | 3.3 (3.3) |
| Who initiated the weight discussion | |
| Physician | 35% (163) |
| Patient | 55% (254) |
| Weight not discussed | 10% (44) |
| Type of encounter (missing = 3, 2) | |
| Preventive | 36% (163) |
| Chronic care | 64% (295) |
| Explicit weight discussion (missing = 15, 0) | 64% (286) |
| Physicianse | N = 40 |
| Race | |
| White/Asian/Pacific Islander | 85% (34) |
| Male | 40% (16) |
| Years since medical school graduation | 22.1 (8.0) |
| Specialty | |
| Family physician | 46% (19) |
| Internist | 54% (21) |
| Prior training in behavioural counselling | 38% (15) |
| Self-efficacy to address weightc | 4.0 (0.7) |
| Comfort discussing weightd | 4.4 (0.9) |
| Barriers to discussing weight with patientsf | 2.5 (0.8) |
| Concerns about reimbursementg | 3.0 (1.6) |
Note: Forty primary care physicians and 461 of their overweight or obese patient visits were audio recorded between December 2006 and June 2008 in Durham and Oxford, NC.
Missing data at baseline (total sample and counselled sample).
Motivation to lose weight/address weight (1 = not at all to 7 = very much).
Self-efficacy to lose weight/address weight (1 = not at all confident to 5 = very confident).
Comfort discussing weight (1 = not at all comfortable to 5 = very comfortable).
Same number of physicians in discussed weight group; all physicians discussed weight with at least one patient.
Barriers (1 = strongly disagree to 5 = strongly agree).
Concerns about reimbursement (1 = not very concerned to 5 = very concerned).
Figure 1.
Boxplot of outcome expectation for weight loss by physicians (n = 40) of patients who had weight discussions during the encounter; a diamond represents the mean score for physician and a dash represents the median score. Number of patients per physician varies from 2 to 11. A colour version of this image is available in Family Practice online.
Outcome expectations and actual change
Overall, 28% of patients lost at least 1 kg of weight in the 3-month time period, 34% of patients improved their fat and fibre intake by 0.2 points and only 6% of patients increased their physical activity by 5 points. For all three outcomes, these rates of change in outcomes were the same in the subgroup of patients where weight, nutrition or physical activity was discussed. Three-month follow-up was completed on 426 patients (follow-up rate 92%).
Physician outcome expectations about weight loss, nutrition or physical activity discussions were not associated with 3-month weight (ICC = 0; P = 0.15), nutrition (ICC = 0.0; P = 0.24) or physical activity (ICC = 0; P = 0.08) change adjusting for baseline outcome and patient, physician and visit-level factors. For both change in weight and physical activity, we found no physician clustering effect (ICC = 0). In a sensitivity analysis for weight using a cut-off based on no weight gain instead of losing >1 kg, we found similar results. Mean observed and estimated 3-month changes in weight, nutrition and physical activity by outcome expectation category are shown in Table 2.
Table 2.
Observed means and estimated means and 95% CI for 3-month weight loss (3 month—baseline weight) from linear mixed model adjusted for baseline outcome, patient, physician and visit factorsa (n = 389 in model for weight and physical activity; 72 observations deleted due to missing data; n = 390 in model for nutrition; 71 observations deleted due to missing data)
| Main predictor | N a | Outcomes | P-valuec | |
| Observed 3-month change | Estimated mean 3-month change (95% CI)b | |||
| Weight outcome expectation | Weight change | 0.15 | ||
| No weight discussion | 188 | 0.6 | 0.6 (−0.1 to 1.2) | |
| Somewhat to not at all likely to follow weight recommendation | 134 | −0.0 | −0.1 (−0.8 to 0.5) | |
| Likely to extremely likely to follow weight recommendation | 134 | −0.5 | −0.4 (−1.1 to 0.2) | |
| Nutrition outcome expectation | Fat change | 0.24 | ||
| No nutrition discussion | 167 | −0.1 | −0.1 (−0.0 to −0.1) | |
| Somewhat to not at all likely to follow nutrition recommendation | 136 | −0.1 | −0.1 (0.0 to −0.1) | |
| Likely to extremely likely to follow nutrition recommendation | 154 | −0.1 | −0.1 (−0.1 to −0.2) | |
| Physical activity outcome expectation | Physical activity change | 0.08 | ||
| No physical activity discussion | 114 | 0.4 | 1.0 (0.3 to 1.7) | |
| Somewhat to not at all likely to follow physical activity recommendation | 164 | 0.2 | 0.0 (−0.5 to 0.5) | |
| Likely to extremely likely to follow physical activity recommendation | 178 | 0.4 | 0.3 (−0.2 to 0.8) | |
Note: Forty primary care physicians and 461 of their overweight or obese patient visits were audio recorded between December 2006 and June 2008 in Durham and Oxford, NC.
Five missing whether weight or physical activity discussed and four missing whether nutrition discussed.
Estimates from linear mixed model adjusted for clustering with outcomes of weight change for weight outcome expectations, fat change for nutrition outcome expectations and physical activity change for physical activity outcome expectations, baseline assessment of outcome, patient, physician and visit level covariates, 72 observation deleted due to missing outcome or covariates for weight and physical activity, 71 observations deleted for nutrition.
P-value from type 3 test from the three level main predictor categorical variable.
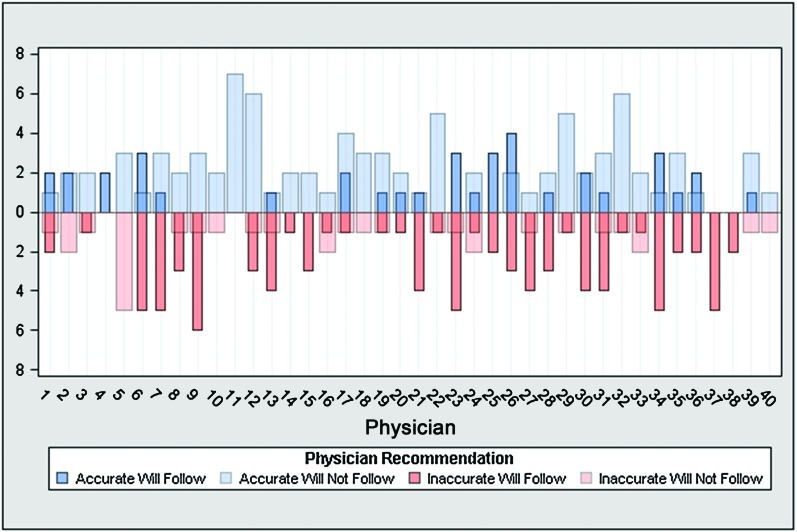
Accuracy of outcome expectations
The mean rate of accurate outcome expectations for physicians was 52% (SD = 23%) for weight, 52% (SD = 19%) for nutrition and 47% (SD = 28%) for physical activity. Physicians were most accurate that patients would ‘not’ follow recommendations. The mean rate (SD) of physician accuracy that patients followed recommendations for weight loss, improving nutrition or increasing physical activity was 16% (SD = 21%), 19% (SD = 17%) and 4% (SD = 7%), respectively. The distribution of the four combinations of accurate/inaccurate predictions by physician for weight is shown in Figure 2.
Figure 2.
Distribution of the number of accurate or inaccurate outcome expectations by physician; accurate counts are denoted in the up direction (blue) and inaccurate counts are denoted in the down direction (red). Physicians can be accurate or inaccurate about a patient following or not following recommendation; blue indicates accurate predictions for following recommendations (darker blue) or not following predictions (light blue); red indicates inaccurate predictions for following recommendations (darker red) or not follow recommendations (light red). A colour version of this image is available in Family Practice online.
Outcome expectations and change in motivation and confidence
There was little change between baseline motivation and confidence and post-visit motivation and confidence in any of the three categories (nutrition, exercise and weight loss). For motivation, 10%, 13% and 7% of patients moved from ‘not motivated’ to ‘motivated’ between baseline and post-visit reports in the respective groups. Similarly, 14%, 13% and 13% of patients moved from ‘not confident’ to ‘confident’. Patients' motivation and confidence were unrelated to physician outcome expectations that patients will follow weight, nutrition and physical activity recommendations, with one exception. A higher percentage of patients were confident that they could lose weight after the visit when their physician believed that they would follow weight loss recommendations than when physicians did not think they would follow recommendations (43% versus 31% high post-visit confidence, respectively; P = 0.06). We found no other meaningful associations between high patient post-visit motivation and confidence and physician outcome expectations that patients will follow weight, nutrition and physical activity recommendations (results not shown).
Discussion
There are several key findings. Firstly, physicians were somewhat optimistic that their patients would lose weight, improve nutrition and increase physical activity. Secondly, these outcome expectations were not related to clinically significant changes in patient weight, nutrition or physical activity. Finally, patient confidence to lose weight may have an association with physician outcome expectations about following weight loss recommendations.
Slightly more than half of physicians believed their patients would follow their recommendations. This result is surprising and inconsistent with both previous reports8,9 and with these same physicians' own baseline reports of general outcome expectations. Physicians may have a general sense that weight loss, nutrition or physical activity counselling does not help;7,9,23 however, after they have established a therapeutic alliance with a particular patient, they may feel more efficacious and optimistic that the patient will change.24 This optimism, however, might indicate that physicians are overestimating the effect of their counselling.
Indeed, physicians' outcome expectations were not consistent with actual patient changes. Given patients did not improve their behaviours much, it is not surprising that physicians were often inaccurate that patient would improve. This mismatch between outcome expectations and actual change could be problematic as physicians might feel more confident and be less receptive to training to improve their counselling.
Physician optimism might have some benefits; patients might feel more confident that they can lose weight when they feel their physician believes they will change. Physician confidence in patients might transfer down to actual patient confidence. Given, how important self-efficacy is for behaviour change, physicians expressing confidence might be an important factor in helping patients change.
Limitations of this report include generalizability given that most patients were highly educated and an observational study design. The accuracy outcome was defined based on clinically significant changes in patient outcomes. As this was not an intervention trial, not many patients met these criteria for change, and the magnitude of change used for the cut-offs may be unrealistic for an observational study, despite the results of the sensitivity analyses. The nutrition and physical activity scales used were not the gold standard, in part, because we did not want patients to guess that the study was about weight and weight-related behaviours. The accuracy analysis was also limited to the subgroup of patients where the topic of weight, nutrition or physical activity was discussed as physicians only completed the outcome expectations survey for the topics that were discussed with that patient. Strengths are that this is one of the first reports to examine physicians' ability to predict which patients will change. Furthermore, because we enrolled multiple patients per physician, we were able to characterize the within-physician outcome expectations and accuracy. This analysis is based on one of the largest datasets of audio-recorded visits with overweight and obese adult patients.
While it was encouraging that physicians were optimistic that patients would follow their counselling recommendations when they were asked about specific patients, this optimism was not well matched with clinically significant improvements. Practical implications are that physician optimism can have positive and negative consequences. Optimism might make physicians feel less in need of improvement. Research indicates, however, that physician weight loss counselling can be improved greatly.2 Positive effects, however, are that physician optimism might turn into patient optimism for change. Finding a way to maintain physician optimism while still helping them recognize the need for improvement could help enhance communication and promote weight loss among patients.
Declaration
Funding: National Institute of Health (R01CA114392, R01HL092403, R01DK64986 and R01DK075439). Dr Alexander is supported by Health Services Research Career Development Award RCD 07-006 from the Department of Veterans Affairs.
Ethical approval: Duke University Medical Center Institutional Review Board.
Conflict of interest: none.
References
- 1. Centers for Disease Control and Prevention. US Obesity trends—1985-2007. http://www.cdc.gov/obesity/data/trends.HTML. [Google Scholar]
- 2.Pollak KI, Alexander SC, Coffman CJ, et al. Physician communication techniques and weight loss in adults: Project CHAT. Am J Prev Med. 2010;39:321–8. doi: 10.1016/j.amepre.2010.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Galuska DA, Will JC, Serdula MK, Ford ES. Are health care professionals advising obese patients to lose weight? JAMA. 1999;282:1576–8. doi: 10.1001/jama.282.16.1576. [DOI] [PubMed] [Google Scholar]
- 4.Rodondi N, Humair J-P, Ghali WA, et al. Counseling overweight and obese patients in primary care: a prospective cohort study. Eur J Cardiovasc Prev Rehabil. 2006;13:222–8. doi: 10.1097/01.hjr.0000209819.13196.a4. [DOI] [PubMed] [Google Scholar]
- 5.Pollak KI, Ostbye T, Alexander SC, et al. Empathy goes a long way in weight loss discussions. J Fam Pract. 2007;56:1031–6. [PubMed] [Google Scholar]
- 6.Loureiro ML, Nayga RM., Jr Obesity, weight loss, and physician's advice. Soc Sci Med. 2006;62:2458–68. doi: 10.1016/j.socscimed.2005.11.011. [DOI] [PubMed] [Google Scholar]
- 7.Dolor RJ, Ostbye T, Lyna P, et al. What are physicians' and patients' beliefs about diet, weight, exercise, and smoking cessation counseling? Prev Med. 2010;51:440–2. doi: 10.1016/j.ypmed.2010.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alexander SC, Ostbye T, Pollak KI, et al. Physicians' beliefs about discussing obesity: results from focus groups. Am J Health Promot. 2007;21:498–500. doi: 10.4278/0890-1171-21.6.498. [DOI] [PubMed] [Google Scholar]
- 9.Huang J, Yu H, Marin E, et al. Physicians' weight loss counseling in two public hospital primary care clinics. Acad Med. 2004;79:156–61. doi: 10.1097/00001888-200402000-00012. [DOI] [PubMed] [Google Scholar]
- 10.Bandura A. Social Foundations of Thought and Action: a Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall, Inc.; 1986. [Google Scholar]
- 11.Cheng TL, DeWitt TG, Savageau JA, O'Connor KG. Determinants of counseling in primary care pediatric practice: physician attitudes about time, money, and health issues. Arch Pediatr Adolesc Med. 1999;153:629–35. doi: 10.1001/archpedi.153.6.629. [DOI] [PubMed] [Google Scholar]
- 12.Mullen PD, Pollak KI, Titus JP, Sockrider MM, Moy JG. Prenatal smoking cessation counseling by Texas obstetricians. Birth. 1998;25:25–31. doi: 10.1046/j.1523-536x.1998.00025.x. [DOI] [PubMed] [Google Scholar]
- 13.van Ryn M, Burke J. The effect of patient race and socio-economic status on physicians' perceptions of patients. Soc Sci Med. 2000;50:813–28. doi: 10.1016/s0277-9536(99)00338-x. [DOI] [PubMed] [Google Scholar]
- 14.Shannon J, Kristal AR, Curry SJ, Beresford SA. Application of a behavioral approach to measuring dietary change: the fat- and fiber-related diet behavior questionnaire. Cancer Epidemiol Biomarkers Prev. 1997;6:355–61. [PubMed] [Google Scholar]
- 15.Kristal AR, Shattuck AL, Henry HJ. Patterns of dietary behavior associated with selecting diets low in fat: reliability and validity of a behavioral approach to dietary assessment. J Am Diet Assoc. 1990;90:214–20. [PubMed] [Google Scholar]
- 16.Kannel WB, Sorlie P. Some health benefits of physical activity. The Framingham Study. Arch Intern Med. 1979;139:857–61. [PubMed] [Google Scholar]
- 17.Hays RD, Woolley JM. The concept of clinically meaningful difference in health-related quality-of-life research. How meaningful is it? Pharmacoeconomics. 2000;18:419–23. doi: 10.2165/00019053-200018050-00001. [DOI] [PubMed] [Google Scholar]
- 18.Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care. 2003;41:582–92. doi: 10.1097/01.MLR.0000062554.74615.4C. [DOI] [PubMed] [Google Scholar]
- 19.Martínez ME, Giovannucci E, Spiegelman D, Willett WC, Hunter DJ, Colditz GA. Leisure-time physical activity, body size, and colon cancer in women. J Natl Cancer Inst. 1997;89:948–55. doi: 10.1093/jnci/89.13.948. [DOI] [PubMed] [Google Scholar]
- 20.Dansinger ML, Gleason JA, Griffith JL, Selker HP, Schaefer EJ. Comparison of the Atkins, Ornish, Weight Watchers, and Zone diets for weight loss and heart disease risk reduction: a randomized trial. JAMA. 2005;293:43–53. doi: 10.1001/jama.293.1.43. [DOI] [PubMed] [Google Scholar]
- 21.Verbeke G, Molenberghs G. Linear Mixed Models for Longitudinal Data. New York, NY: Springer-Verlag; 2000. [Google Scholar]
- 22.Diggle PJ, Heagerty P, Liang K-Y, Zeger SL. Analysis of Longitudinal Data. 2nd edn. Oxford, UK: Oxford University Press; 2002. [Google Scholar]
- 23.Price JH, Desmond SM, Krol RA, Snyder FF, O'Connell JK. Family practice physicians' beliefs, attitudes, and practices regarding obesity. Am J Prev Med. 1987;3:339–45. [PubMed] [Google Scholar]
- 24.Byrne MK, Deane FP, Lambert G, Coombs T. Enhancing medication adherence: clinician outcomes from the Medication Alliance training program. Aust N Z J Psychiatry. 2004;38:246–53. doi: 10.1080/j.1440-1614.2004.01344.x. [DOI] [PubMed] [Google Scholar]