Abstract
Objective
To create a risk score for death from cardiovascular disease that can be easily used.
Design
Data from eight randomised controlled trials of antihypertensive treatment.
Setting
Europe and North America.
Participants
47 088 men and women from trials that had differing age ranges and differing eligibility criteria for blood pressure.
Main outcome measure
1639 deaths from cardiovascular causes during a mean 5.2 years of follow up.
Results
Baseline factors were related to risk of death from cardiovascular disease using a multivariate Cox model, adjusting for trial and treatment group (active versus control). A risk score was developed from 11 factors: age, sex, systolic blood pressure, serum total cholesterol concentration, height, serum creatinine concentration, cigarette smoking, diabetes, left ventricular hypertrophy, history of stroke, and history of myocardial infarction. The risk score is an integer, with points added for each factor according to its association with risk. Smoking contributed more in women and in younger age groups. In women total cholesterol concentration mattered less than in men, whereas diabetes had more of an effect. Antihypertensive treatment reduced the score. The five year risk of death from cardiovascular disease for scores of 10, 20, 30, 40, 50, and 60 was 0.1%, 0.3%, 0.8%, 2.3%, 6.1%, and 15.6%, respectively. Age and sex distributions of the score from the two UK trials enabled individual risk assessment to be age and sex specific. Risk prediction models are also presented for fatal coronary heart disease, fatal stroke, and all cause mortality.
Conclusion
The risk score is an objective aid to assessing an individual's risk of cardiovascular disease, including stroke and coronary heart disease. It is useful for physicians when determining an individual's need for antihypertensive treatment and other management strategies for cardiovascular risk.
What is already known on this topic
Many other factors are known to affect the risk of cardiovascular disease in patients with raised blood pressure
A patient's overall risk should be taken into account when determining their need for antihypertensive drugs and other strategies for improving cardiovascular health
What this study adds
A new score uses 11 risk factors to quantify an adult's risk of death from cardiovascular disease, including stroke and coronary heart disease
The score is based on a large cohort of participants in controlled trials of antihypertensive drugs
An individual's risk can be readily assessed as high or low compared with others of the same age and sex
The website www.riskscore.org.uk is available for users of the risk score
Introduction
The management of patients with hypertension often focuses on drugs and other means of controlling blood pressure without adequate regard to their overall risk of morbidity and mortality from cardiovascular disease. The goal of treatment is to reduce the risk of stroke and heart disease and to prevent premature death. Hence a range of personal factors should be considered in assessing a patient's overall cardiovascular risk. A recent inquiry emphasised the benefits of using charts or scores for cardiovascular risk in getting treatment decisions made alongside realistic estimates of patient susceptibility to cardiovascular disease.1
Other scoring methods already exist for assessing risk,2–9 but ours has several particularly useful features: it focuses on patients with raised blood pressure, and it assesses an individual's overall risk for all cardiovascular diseases, including stroke, rather than just coronary heart disease. Although the guidelines from the World Health Organization and International Society of Hypertension usefully classify hypertensive patients from low risk to very high risk of cardiovascular disease,10 we present a more quantitative and discriminating risk score based on the mortality among participants in eight randomised controlled trials of antihypertensive treatment. We aimed to enable the calculation of risk of cardiovascular death within five years from a few personal factors.
Participants and methods
The individual data analysis of antihypertensive intervention trials (INDANA) database includes all the major randomised trials of antihypertensive drugs versus placebo or no intervention for which individual patient data were available in 1995.11,12 After exhaustive literature searches and personal inquiries we are confident that all such major trials are included. Here we assess data from all eight trials with results on mortality by intention to treat, totalling 47 008 participants of whom 3001 died (1639 from cardiovascular causes) during a mean 5.2 years of follow up (table 1).13–20 The trials had differing eligibility criteria, and for the multiple risk factor intervention trial we focus only on the subset of participants with raised blood pressure.
Table 1.
Eight randomised controlled trials of antihypertensive treatment
| Trial | Blood pressure inclusion criteria (mm Hg) | Age range (years) | No of participants
|
Mean follow up (years) | No of deaths*
|
||||
|---|---|---|---|---|---|---|---|---|---|
| Randomised | In analysis* | All cardiovascular | Coronary heart disease | Stroke | All causes | ||||
| Coope and Warrender13 | Systolic 170-280 or diastolic 105-120 | 60-80 | 884 | 856 | 3.5 | 84 | 52 | 18 | 127 |
| EWPHE14 | Systolic 160-239 and diastolic 90-119 | ⩾60 | 840 | 779 | 4.4 | 153 | 49 | 50 | 266 |
| HDFP15 | Diastolic ⩾90 | 30-69 | 10 940 | 10 529 | 5.0 | 396 | 257 | 73 | 706 |
| MRC116 | Systolic <200 and diastolic 90-109 | 35-64 | 17 354 | 16 851 | 5.3 | 262 | 195 | 43 | 480 |
| MRC217 | Systolic 160-209 | 65-74 | 4 396 | 4 090 | 6.1 | 313 | 179 | 71 | 571 |
| MRFIT18 | Diastolic >90 or previous treatment | 35-58 | 8 012† | 8 006 | 6.9 | 193 | 151 | 20 | 343 |
| SHEP19 | Systolic 160-209 and diastolic <90 | ⩾60 | 4 736 | 4 472 | 4.5 | 192 | 126 | 23 | 430 |
| STOP20 | Systolic 180-229 and diastolic 90-120 or systolic <230 and diastolic >105 | 70-84 | 1 627 | 1 505 | 2.0 | 46 | 22 | 16 | 78 |
| All trials | 48 789 | 47 008 | 1639 | 1031 | 314 | 3001 | |||
Only 47 088 participants used in development of final model for cardiovascular mortality are included. †Men.
Sixteen baseline factors were available in all datasets and had a priori plausibility as risk factors: age, sex, height, body mass index, current cigarette smoking, systolic and diastolic blood pressure, heart rate, concentrations of serum total cholesterol, serum creatinine and serum uric acid, previous myocardial infarction, previous stroke, diabetes, left ventricular hypertrophy detected by electrocardiography, and treatment group.
We fitted a multivariate Cox proportional hazards model, stratified by trial, for all 16 risk factors simultaneously, with cardiovascular death as outcome. We excluded body mass index, diastolic blood pressure, heart rate, and uric acid concentration, which were non-significant predictors. Systolic blood pressure was a stronger predictor than pulse pressure. For the remaining 12 factors we investigated possible statistical interactions in risk prediction. Thus we determined a final Cox model based on 1639 cardiovascular deaths in 47 088 participants with 12 risk factors and five interactions. No interactions with treatment group were strong enough to merit inclusion, and separate analyses for each trial broadly agreed with the overall model. We found no departures from linearity for quantitative risk factors.
We converted the Cox model predictor to an integer score. Briefly, the score is directly related to an individual's probability of death from cardiovascular disease within five years. This requires a reference sample from one country, and for this purpose we chose the 20 941 participants in the two UK Medical Research Council trials. We also wanted a zero score for an adult at very low risk—that is, a woman aged 35-39 with the healthiest category of each risk factor. Having grouped each factor into convenient intervals, such as every 10 mm Hg for systolic blood pressure, an individual's score increases by an integer amount for each risk factor level above the lowest risk category. Each integer amount is a rounding of the exact figure obtained from the proportional hazards model, so that the risk score is a simple addition of whole numbers. The estimated probability of death from cardiovascular disease within five years is equal to 1−0.99958exp (0.1 × risk score).
Results
The risk score
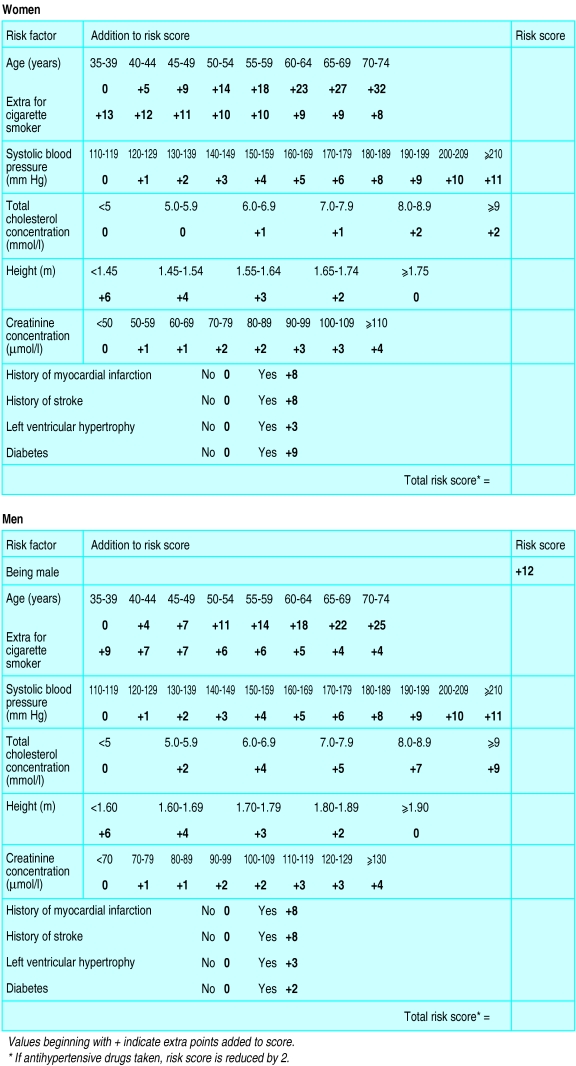
Figure 1 presents the risk score for both men and women. Age is a particularly strong risk factor—a woman aged 60–64 has 23 extra points compared with a woman aged 35-39. Sex is also important, with men having 12 extra points. The gradient for risk according to age is slightly less noticeable for men—those aged 60-64 have 18 extra points (18+12=30 points). Cigarette smoking scores more points in women and at younger ages—for example, a female smoker aged 35-39 has 13 extra points compared with just 4 extra points for a male smoker aged 70-74.
Figure 1.
Risk scores for cardiovascular disease in men and women
Systolic blood pressure has a sliding scale: 5 extra points for moderate hypertension (160-169 mm Hg) and 11 extra points for severe hypertension (>210 mm Hg), the same for both sexes and all ages. For serum total cholesterol concentration the sliding scale is steeper for men than it is for women because cholesterol is not related to stroke, and the proportion of cardiovascular deaths due to stroke is higher in women—for a cholesterol concentration of 6.0-6.9 mmol/l women should be given 1 extra point and men 4 extra points. Short stature and a raised serum creatinine concentration also contribute to the score. With a history of myocardial infarction, history of stroke, and left ventricular hypertrophy 8, 8, and 3 points should be added, respectively. Diabetes contributes more to risk in women than it does in men: 9 points should be added for women and 2 points for men.
Because this score is derived from controlled trials of hypertension, the effect of treatment can be measured: a reduction of 2 points if antihypertensive drugs are started. For any individual, points scored for each risk factor are added together to produce the total risk score.
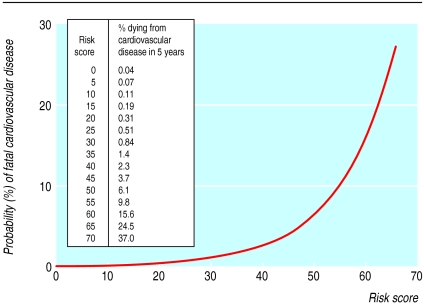
The chance of dying from cardiovascular disease
Figure 2 shows the exponential relation between the risk score and the probability of dying from cardiovascular disease in five years. Rates of cardiovascular death vary between trials and between communities in ways not fully explained by known risk factors. The curve in figure 2 relates to a British population, being based on cardiovascular death rates for participants in the two MRC trials.15,16 The risk score itself, however, is derived from data on all participants in all eight trials.
Figure 2.
Relation between risk score and probability of dying from cardiovascular disease in five years
Younger women have a low death rate from cardiovascular disease: for instance a score of 10 points—typical for a woman aged 35-39—has a five year risk of 0.11%; a score of 25, typical for men aged 35-39, 0.51%; and a score of 35, not unusual for women aged 60-64 or men aged 50-54, 1.4%. A typical score for 10 years older is 45, with a five year risk of 3.7%. A score of 55 indicates a 10% risk of cardiovascular death in five years, not uncommon for men aged 70-74, and a score of 65 indicates a 25% risk, achieved in a few elderly men only.
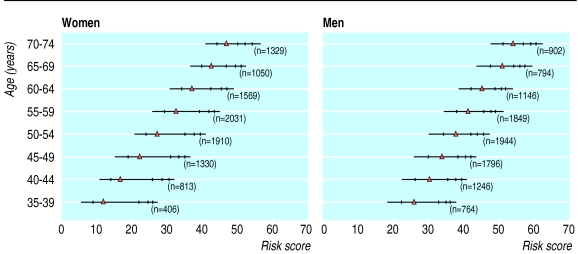
Risk score by age and sex
Figure 3 shows the noticeable influence of age and sex on the risk score for the 20 941 participants in the two MRC trials. In general, the median age specific score for a man is similar to the median score for a woman 10 years older. Age affects risk: the median age specific score for a man corresponds to the score of a man at high risk who is 10 years younger and the score of a man at very low risk who is 10 years older. A score of 45, typical for a man aged 60-64, is achieved or exceeded by only 6% of men aged 50-54 but is exceeded by virtually all men aged 70-74; 45 is also the upper 90% point for women aged 60-64 and is achieved by no woman aged 50-54.
Figure 3.
Distribution of risk scores by sex and age group. ▵ is median score. Vertical lines indicate 20th, 80th, 90th, and 95th centiles. Horizontal line covers 2nd to 98th centile. Each score distribution is skewed to right, and there are two modes in each distribution, for non-smokers and smokers
Thus when assessing individual risk, comparisons should be made with others of the same age and sex. For example, a 66 year old male smoker (22, 12, and 4 points) has a systolic blood pressure of 150 mm Hg (4 points), a total cholesterol concentration of 6.5 mmol/l (4 points), a serum creatinine concentration of 125 μmol/l (3 points), a previous myocardial infarction (8 points), and is 1.64 metres tall (4 points). His risk score is 61 points. His risk of cardiovascular death in five years is 17% (fig 1). For his age he has an unusually high cardiovascular risk (fig 3), although his systolic blood pressure is not particularly high. His risk score emphasises the importance of tackling his overall risk of cardiovascular disease in several ways—for example, lipid lowering, smoking cessation, continued monitoring, or lowering of blood pressure.
A female non-smoker aged 52 (0, 0, and 14 points) has a systolic blood pressure of 165 mm Hg (5 points), a total cholesterol concentration of 5.2 mmol/l (0 points), a creatinine concentration of 85 μmol/l (2 points), no history of disease (0 points), and is 1.63 metres tall (3 points). Her risk score is 24 points. Her risk of cardiovascular death in five years is 0.5% (fig 2), low for her age (around the 20% point in figure 3). Despite her moderately raised blood pressure the risk score identifies her overall cardiovascular risk as low. This helps to balance the benefit of continued blood pressure monitoring against that of starting antihypertensive drugs.
The risk factors
The list of risk factors chosen is not surprising, although their distributions vary between populations. Table 2 shows the distributions of risk factors for our subjects. Eligibility criteria differed between trials: one studied isolated systolic hypertension,19 whereas others primarily had an inclusion criterion for diastolic pressure. Hence the distribution of systolic blood pressure covers a wide range. The MRC trials excluded patients with previous stroke. Five trials were in elderly patients.13,14,17,19,20 The distributions of cholesterol and creatinine concentrations and height are representative of developed countries in the West. The prevalence of diabetes is low, and it is an exclusion criterion in the MRC trials.
Table 2.
Distributions of risk factors (percentages) for men and women for eight trials of antihypertensive treatment
| Women (n=20 802) | Men (n=27 987) | |
|---|---|---|
| Age (years): | ||
| <35 | 1.6 | 1.5 |
| 35-39 | 4.2 | 8.5 |
| 40-44 | 7.0 | 13.2 |
| 45-49 | 10.5 | 18.2 |
| 50-54 | 13.9 | 18.8 |
| 55-59 | 13.9 | 13.1 |
| 60-64 | 14.0 | 8.6 |
| 65-69 | 12.2 | 7.7 |
| 70-74 | 13.7 | 6.9 |
| ⩾75 | 9.1 | 3.4 |
| Systolic blood pressure (mm Hg): | ||
| <120 | 0.2 | 1.4 |
| 120-129 | 1.4 | 6.5 |
| 130-139 | 4.9 | 14.7 |
| 140-149 | 9.4 | 19.0 |
| 150-159 | 11.6 | 15.7 |
| 160-169 | 21.8 | 17.1 |
| 170-179 | 17.7 | 11.3 |
| 180-189 | 14.2 | 7.1 |
| 190-199 | 9.9 | 4.1 |
| 200-210 | 5.5 | 2.1 |
| ⩾210 | 3.4 | 1.0 |
| Cholesterol concentration (mmol/l): | ||
| <5.0 | 8.3 | 11.1 |
| 5.0-5.9 | 25.3 | 31.6 |
| 6.0-6.9 | 32.9 | 35.6 |
| 7.0-7.9 | 21.8 | 16.5 |
| 8.0-8.9 | 8.2 | 4.3 |
| ⩾9.0 | 3.5 | 0.8 |
| Height (m): | ||
| <1.50 | 6.9 | 0.3 |
| 1.50-1.59 | 40.6 | 1.9 |
| 1.60-1.69 | 45.7 | 23.0 |
| 1.70-1.79 | 6.6 | 52.8 |
| 1.80-1.89 | 0.2 | 20.8 |
| ⩾1.90 | 0 | 1.3 |
| Creatinine concentration (μmol/l): | ||
| <60 | 4.5 | 0.02 |
| 60-69 | 13.7 | 1.1 |
| 70-79 | 24.5 | 9.2 |
| 80-89 | 22.2 | 19.3 |
| 90-99 | 16.8 | 24.9 |
| 100-109 | 8.9 | 19.6 |
| 110-119 | 4.4 | 12.3 |
| 120-129 | 2.2 | 6.6 |
| ⩾130 | 2.9 | 6.7 |
| Current cigarette smoker | 22.9 | 37.9 |
| Previous myocardial infarction | 2.5 | 4.7 |
| Previous stroke | 1.2 | 1.0 |
| History of diabetes | 3.8 | 3.2 |
| Left ventricular hypertrophy | 11.2 | 13.2 |
Stroke, coronary heart disease, and all cause mortality
Separate predictions of stroke, coronary heart disease, and death from any cause are also relevant. Table 3 presents the results from the Cox model that led to the risk score for cardiovascular death, and also corresponding results for fatal coronary disease, fatal stroke, and all cause mortality.
Table 3.
Results of Cox proportional hazards models, stratified by trial, for 47 088 participants in eight trials of antihypertensive treatment
| Risk factor | Fatal cardiovascular disease (n=1639)
|
Fatal coronary heart disease (n=1031)
|
Fatal stroke (n=317)
|
All cause mortality (n=3005)
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Log hazard ratio | z score* | Log hazard ratio | z score* | Log hazard ratio | z score* | Log hazard ratio | z score* | ||||
| Sex | 1.208† | 10.39 | 1.789‡ | 11.99 | 0.063 | 0.49 | 0.645 | 11.92 | |||
| Age (per 5 years): | |||||||||||
| Women non-smokers | 0.455 | 17.48 | 0.458 | 12.12 | 0.386 | 9.81 | 0.360 | 28.13 | |||
| Women smokers | 0.381 | 12.93 | |||||||||
| Men non-smokers | 0.359 | 15.45 | 0.300 | 12.26 | |||||||
| Men smokers | 0.286 | 11.79 | |||||||||
| Systolic blood pressure (per 10 mm Hg) | 0.108 | 7.64 | 0.129 | 6.48 | 0.161 | 5.28 | 0.074 | 6.96 | |||
| Cholesterol concentration (per 1 mmol/l): | |||||||||||
| Women | 0.048 | 1.45 | 0.213 | 8.14 | |||||||
| Men | 0.180 | 6.48 | |||||||||
| Creatinine concentration (per 10 mmol/l) | 0.060 | 4.89 | 0.042 | 2.55 | 0.125 | 2.35 | 0.079 | 4.10 | |||
| Height (per 10 cm) | −0.148 | −4.17 | −0.162 | −3.62 | −0.097 | −3.70 | |||||
| Smoking status: | |||||||||||
| Women | 1.046 | 9.42 | 0.994 | 7.42 | 0.661 | 5.24 | 0.601 | 15.05 | |||
| Men | 0.606 | 8.71 | 0.470 | 6.16 | |||||||
| Diabetes: | |||||||||||
| Women | 0.911 | 6.76 | 1.039 | 5.46 | 0.419 | 1.83 | 0.397 | 5.18 | |||
| Men | 0.144 | 0.99 | 0.107 | 0.60 | |||||||
| History of stroke | 0.808 | 6.51 | 0.675 | 3.80 | 1.209 | 5.29 | 0.635 | 6.30 | |||
| History of myocardial infarction | 0.820 | 8.93 | 0.966 | 9.01 | 0.538 | 7.15 | |||||
| Left ventricular hypertrophy | 0.332 | 5.15 | 0.254 | 3.03 | 0.282 | 1.91 | 0.227 | 4.64 | |||
| Antihypertensive treatment | −0.166 | −3.34 | −0.116 | −1.86 | −0.455 | −3.96 | −0.095 | −2.61 | |||
The larger the value of z, the more highly significant the risk factor: for example, z scores of 1.96, 2.58, 3.29, and 3.49 correspond to P=0.05, P=0.01, P=0.001, and P=0.0001, respectively.
Sex difference varies with age, smoking status, cholesterol concentration, and diabetes. Log hazard ratio given here is for sex difference at age 55 for patients who are non-smokers, do not have diabetes, and have cholesterol concentration of 6 mmol/l.
Sex difference varies with age, systolic blood pressure, smoking status, and diabetes. Log hazard ratio given here is for sex difference at age 55, systolic blood pressure 160 mm Hg, being a non-smoker, and not having diabetes.
For fatal coronary disease (1031 deaths) all risk factors remain significant predictors. For fatal stroke (317 deaths) the influences of systolic blood pressure and antihypertensive treatment are more noticeable, whereas sex, cholesterol concentration, height, and a history of myocardial infarction do not predict risk. For all cause mortality all factors except cholesterol concentration are significant predictors.
Discussion
The risk score developed by us is unique in being based on a large cohort of adults with moderately raised blood pressure, both treated and not treated with antihypertensive drugs, including both European and North American populations, and covering a wide age range. Thus the score has wide applicability in general practices and hypertension clinics, providing a simple means of quantifying a patient's risk of cardiovascular disease based on what should be routinely available information. The focus on overall cardiovascular risk, both of stroke and of coronary disease, ensures that a patient's overall wellbeing, including management of other cardiovascular risk factors such as smoking and lipid lowering, gets sufficient attention, keeping control of blood pressure and antihypertensive drug treatment in proper perspective.
The score is derived from people with blood pressure sufficiently raised to be included in a trial. However, the trials' differing eligibility criteria result in a wide spread of baseline blood pressures. Thus the score may be used in the general population, not just in people meeting specific criteria for hypertension. The score takes into account systolic but not diastolic blood pressure, because diastolic blood pressure does not independently predict cardiovascular risk.21,22
Mortality from cardiovascular disease varies between countries,23which affects the generalisability of any risk score internationally. Although our data cover many developed countries, the problem remains of how to make a risk score specific to a country. Our solution has been to first obtain the most precisely estimated risk score from the whole sample of trials, but then focus on mortality in two UK trials when calculating the risk of cardiovascular disease for any individual.16,17 Because the relative importance of risk factors remains similar in most developed countries, the main complication concerns differences in mortality from cardiovascular disease between countries. For instance, the United States and United Kingdom have rather similar death rates for cardiovascular disease, making the score readily applicable to the United States. In France the rates are much lower, so if the man in the example above were French his risk of cardiovascular death within five years would be substantially less than the calculated 19%. Also, within countries there are social and geographical inequalities and secular trends in cardiovascular disease, so any assessment of risk should take account of these less quantifiable influences on health.
Assessing individual risk
Individual risk assessment should be age and sex specific (fig 3). Risk of death from cardiovascular disease varies noticeably by age and sex (for example, the man aged 65 at lowest risk is at higher risk than the woman aged 50 at highest risk), and risk management strategies need to recognise this. It would be useful to obtain age and sex specific distributions of our risk score for representative samples of individuals from other countries.
The computation of risk should be kept simple, and an integer score seemed our best approach. Sometimes not all 11 items will be known for a patient, but that is easily solved by inserting scores that are middle of the range for quantitative missing items—for example, an extra 2 points for creatinine concentration—and optimistically scoring 0 for any binary factor. However, effective health screening should avoid having data missing.
The integer score simplifies the precise Cox model for death from cardiovascular disease in table 2 although the correlation between the integer score and the Cox model linear predictor is high (r=0.98). Routine use of the risk score by busy physicians and others may be done by accessing www.riskscore.org.uk. Keying in the 11 items provides the score, the probability of death from cardiovascular disease within five years, and the individual's risk level compared with others of the same age and sex.
Components of risk score
The risk score includes 11 risk factors for coronary heart disease and stroke. Age, sex, and cigarette smoking are the strongest predictors. The sex difference narrows with age, and the impact of smoking is more noticeable in women and at younger ages. Serum total cholesterol concentration and systolic blood pressure have similar predictive strength in men, but cholesterol concentration is less important for women because their risk of coronary disease is much lower. Raised creatinine concentration24 and short stature25 are both established highly significant risk factors for coronary disease and stroke, and although not present in previous risk scores should be included here. Diabetes is a more noticeable predictor of cardiovascular disease in women than it is in men,26 and history of stroke, myocardial infarction, and left ventricular hypertrophy are obvious factors to include. Other risk factors, such as more detailed assessment of blood lipids (for example, high density lipoprotein cholesterol and triglycerides) or presence of angina or intermittent claudication, could in principle be included but were not available in all our trials, and there is a danger of making risk scores too detailed and complicated.
Of interest is the limited impact of antihypertensive treatment on overall cardiovascular risk. According to these randomised trials, antihypertensive treatment reduces the risk score by 2—that is, in a meta-analysis the relative risk reduction for death from cardiovascular disease is 15.3% (95% confidence interval 6.6% to 23.2%). This impact of treatment is more noticeable for death from stroke than it is for death from coronary disease (relative risk reduction 36.6% and 11.0%, respectively). However, some patients in untreated control groups subsequently started antihypertensive treatment, so that these estimates compare immediate treatment with a wait and see policy. Nevertheless, the risk score shows that an individual's overall risk of cardiovascular disease is multifaceted, and lowering blood pressure by drugs (a mean treatment difference in these trials of 12.8 mm Hg for systolic blood pressure and 5.8 mm Hg for diastolic blood pressure after one year) is just one aspect of patient management.
The risk score is a more quantitative complement to the guidelines from the WHO and International Society of Hypertension.10 They classify patients simply into four categories (low, medium, high, and very high risk) on the basis of blood pressure, several binary risk factors, and pre-existing disease, but use less information (age is simply above or below 55) and emphasise blood pressure more. Nevertheless the simplicity of the risk score enables a rapid preliminary assessment of risk.
Risk scores already exist from Framingham, the British regional heart study, Dundee, and the prospective cardiovascular Munster study, but each has its limitations.2,3,6–9 All were developed from just one country, and only Framingham has combined risks of stroke and coronary disease into an overall assessment of cardiovascular risk.
Basing a risk score on patients in the major randomised controlled trials of antihypertensive drugs is helpful. The cohort is large and has good follow up, so precision of risk estimates is considerably better than it is in other studies. The trials took place in several different countries, enhancing international representation. People were recruited because their blood pressure justified randomisation to active treatment or control, making the score especially relevant to the clinician-patient dialogue over whether to start antihypertensive treatment alongside other management strategies for cardiovascular disease. Trial participants are not representative of the general population, but the risk score may nevertheless be of more widespread use for screening in primary health care not necessarily motivated by raised blood pressure.
Acknowledgments
We thank John Coope, Jeffrey Cutler, Tord Ekbom, Larry Friedman, Karla Kerlikowski, Mitchell Perry, Ronald Princess, and Eleaner Schron (members of the INDANA steering committee) for helpful comments.
Footnotes
Funding: This research was supported by EC-Biomed 2 programme (contract number BMH4-CT 983291).
Competing interests: None declared.
References
- 1.Montgomery AA, Fahey T, Mackintosh C, Sharp DJ, Peters TJ. Estimation of cardiovascular risk in hypertensive patients in primary care. Br J Gen Practice. 2000;50:127–128. [PMC free article] [PubMed] [Google Scholar]
- 2.Anderson KM, Odell PM, Wilson PW, Kannel WB. Cardiovascular disease risk profiles. Am Heart J. 1991;121:293–298. doi: 10.1016/0002-8703(91)90861-b. [DOI] [PubMed] [Google Scholar]
- 3.D'Agostino RB, Russell MW, Huse DM, Ellison RC, Silbershatz H, Wilson PWF, et al. Primary and subsequent coronary risk appraisal: new results from the Framingham Study. Am Heart J. 2000;139:272–281. doi: 10.1067/mhj.2000.96469. [DOI] [PubMed] [Google Scholar]
- 4.Menotti A, Keys A, Blackburn H, Kromhout D, Karvonen M, Nissinen A. Comparison of multivariate predictive power of major risk factors for coronary heart diseases in different countries: results from eight nations of the seven countries study, 25 years of follow-up. J Cardiovascular Risk. 1995;3:69–75. [PubMed] [Google Scholar]
- 5.Pooling Project Research Group. Relationship of blood pressure, serum cholesterol, smoking habit, relative weight and ECG abnormalities to incidence of major coronary events: final report of the pooling project. J Chronic Dis. 1978;31:201–306. doi: 10.1016/0021-9681(78)90073-5. [DOI] [PubMed] [Google Scholar]
- 6.Shaper AG, Pocock SJ, Phillips AN, Walker M. Identifying men at high risk of heart attacks: strategy for use in general practice. BMJ. 1986;293:474–479. doi: 10.1136/bmj.293.6545.474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Coppola WGT, Whincup PH, Papacosta O, Walker M, Ebraham S. Scoring system to identify men at high risk of stroke: a strategy for general practice. Br J Gen Practice. 1995;45:185–189. [PMC free article] [PubMed] [Google Scholar]
- 8.Tunstall-Pedoe H. The Dundee coronary risk-disk for management of change in risk factors. BMJ. 1991;303:744–747. doi: 10.1136/bmj.303.6805.744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cullen P, von Eckardstein A, Assmann G. Diagnosis and management of new cardiovascular risk factors. Eur Heart J. 1998;19 (suppl O):S13–S19. [PubMed] [Google Scholar]
- 10.Guidelines subcommittee. 1999 World Health Organization-International Society of Hypertension guidelines for the management of hypertension. J Hypertens. 1999;17:151–183. [PubMed] [Google Scholar]
- 11.Gueyffier F, Boutitie F, Boissel JP, Coope J, Cutler J, Ekbom T, et al. INDANA: a meta-analysis on individual patient data in hypertension. Protocol and preliminary results. Thérapie. 1995;50:353–362. [PubMed] [Google Scholar]
- 12.Gueyffier F, Boutitie F, Boissel J-P, Pocock S, Coope J, Cutler J, et al. Effect of antihypertensive drug treatment on cardiovascular outcomes in women and men. Ann Intern Med. 1997;126:761–767. doi: 10.7326/0003-4819-126-10-199705150-00002. [DOI] [PubMed] [Google Scholar]
- 13.Coope J, Warrender TS. Randomised trial of treatment of hypertension in elderly patients in primary care. BMJ. 1986;293:1145–1151. doi: 10.1136/bmj.293.6555.1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Amery A, Birkenhäger W, Brixko P, Bulpitt C, Clément D, Deruyttere M, et al. Mortality and morbidity results from the European working party on high blood pressure in the elderly trial. Lancet. 1985;i:1349–1354. doi: 10.1016/s0140-6736(85)91783-0. [DOI] [PubMed] [Google Scholar]
- 15.Hypertension Detection and Follow-up Program Cooperative Group. Five-year findings of the hypertension detection and follow-up program. I. Reduction in mortality of persons with high blood pressure, including mild hypertension. JAMA. 1979;242:2562–2571. [PubMed] [Google Scholar]
- 16.Medical Research Council Working Party. MRC trial of treatment of mild hypertension: principal results. BMJ. 1985;291:97–104. doi: 10.1136/bmj.291.6488.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.MRC Working Party. Medical Research Council trial of treatment of hypertension in older adults: principal results. BMJ. 1992;304:405–412. doi: 10.1136/bmj.304.6824.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Multiple Risk Factor Intervention Trial Research Group. Multiple risk factor intervention trial: risk factor changes and mortality results. JAMA. 1982;248:1465–1477. [PubMed] [Google Scholar]
- 19.SHEP Cooperative Research Group. Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension: final results of the systolic hypertension in the elderly program (SHEP) JAMA. 1991;265:3255–3264. [PubMed] [Google Scholar]
- 20.Dalhöf B, Lindholm L, Hansson L, Shersten B, Ekbom T, Wester PO. Morbidity and mortality in the Swedish trial in old patients with hypertension (STOP-Hypertension) Lancet. 1991;338:1281–1285. doi: 10.1016/0140-6736(91)92589-t. [DOI] [PubMed] [Google Scholar]
- 21.Kannel WB. Historic perspectives on the relative contributions of diastolic and systolic blood pressure elevation to cardiovascular risk profile. Am Heart J. 1999;138:205–210. doi: 10.1016/s0002-8703(99)70311-x. [DOI] [PubMed] [Google Scholar]
- 22.Shaper AG, Phillips AN, Pocock SJ, Walker M, Macfarlane PW. Risk factors for stroke in middle aged British men. BMJ. 1991;302:1111–1115. doi: 10.1136/bmj.302.6785.1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.World Health Organization. World health statistics annual 1998. Geneva: WHO; 1998. [Google Scholar]
- 24.Wannamethee SG, Shaper AG, Perry IJ. Serum creatinine concentration and risk of cardiovascular disease. Stroke. 1997;28:557–563. doi: 10.1161/01.str.28.3.557. [DOI] [PubMed] [Google Scholar]
- 25.Wannamethee SG, Shaper AG, Whincup PH, Walker M. Adult height, stroke and coronary heart disease. Am J Epidemiol. 1998;148:1069–1076. doi: 10.1093/oxfordjournals.aje.a009584. [DOI] [PubMed] [Google Scholar]
- 26.Kannel WB, McGee DL. Diabetes and cardiovascular disease: the Framingham study. JAMA. 1979;241:2035–2038. doi: 10.1001/jama.241.19.2035. [DOI] [PubMed] [Google Scholar]