Abstract
Few spatial studies explore relationships between people and place in sub-Saharan Africa or in the context of Human Immunodeficiency Virus (HIV). This paper uses individual-level demographic and behavioral data linked to area-level, spatially-referenced socio-economic and access data to examine how the relationships between area- and individual-level risks and individual HIV status vary in rural Malawi. The Political Economy of Health framework guides interpretation. Geographically weighted regression models show significant, local-level variation indicating that area-level factors drive patterns of HIV above individual-level contributions. In distinct locations, women who live further from health clinics, major roads, and major cities are less likely to be infected. For men, HIV status is strongly associated with migration patterns in specific areas. Local-level, gender-specific approaches to HIV prevention are necessary in high risk areas.
Keywords: HIV/AIDS, Malawi, ecological drivers, spatial methods, political economy
INTRODUCTION
Where an individual lives matters for overall health and wellness (Diez Roux, 2004; Entwisle, 2007). In Malawi, a country where approximately 1 million people are infected with HIV (UNAIDS, 2007), and rural infections are rising (Bello et al., 2006), little is known about how characteristics of people and place interact to facilitate the spread of HIV. Previous studies of the drivers of HIV in rural Malawi focus on small geographic areas or on individual behavior (Barden-O’Fallon et al., 2004; Kohler et al., 2007; Smith, 2005; Watkins, 2004). Area-level factors that enable the spread of HIV, such as socio-economics and access to resources (Armour, 2006; Mtika, 2007), receive less attention.
Research is needed to examine the linkages between individuals and the area-level economic, social, and structural contexts that may shape behavior (Hobfoll, 1998). To study ecological drivers of HIV, spatial methods provide several advantages. Primarily, geographic information systems (GIS) technology makes linking large databases using geographic location possible and simplifies integration of data. Additionally, spatial regression reveals interactions through demonstrating the direction, magnitude, and distribution of associations. Lastly, mapped results may accelerate transition from research to practice.
Although use of spatial methods is gaining momentum in health research, only a few studies explore associations between health and place in developing countries (Benson et al., 2005; Heard et al., 2004; Kandala et al., 2006; Kazembe et al., 2009; Tanser, 2001), and fewer still use spatial methods to explore HIV in sub-Saharan Africa. Recent place-based research indicates growing interest in exploration of spatial relationships in sub-Saharan Africa and in the context of HIV, suggesting that associations between HIV prevalence and area-level socio-economic and access factors vary in space (Kleinschmidt et al., 2007; Lachaud, 2007; Tanser et al., 2009). Largely missing from the literature, however, are place-based studies that consider the influence of both area- and individual-level risk factors on HIV as well as reasoned theory about the mechanisms that connect health and place (Macintyre et al., 2002).
This study explores spatial associations between area-level factors, individual risk behaviors, and individual HIV status in rural Malawi using geographically weighted regression (GWR). The research uses a nationally-representative probability sample of rural Malawians and links individual-level demographic and behavioral data with area-level, spatially-referenced access and socioeconomic indicators. Associations are mapped to visually represent geographically-specific results. The Political Economy of Health (PEH) framework guides variable selection and interpretation. The role of area-level socio-economic (income inequality and absolute poverty) and access indicators (distance to roads, public healthcare facilities, and major cities) are explored, and individual-level factors including condom use, high risk sex, multiple partners, and migration are also considered. Gender is examined through stratification. For the purpose of this study, the boundaries for area-level are defined as the aggregate enumeration area, a census-defined boundary that includes approximately 500 households. Exploration of both area- and individual-level drivers of HIV in rural Malawi may enable targeting of HIV prevention and treatment efforts to specific places and populations.
BACKGROUND
In Malawi, approximately 10% of men and 13% of women are infected nationwide (National Statistical Office Malawi, 2005). Although the highest prevalence rates are in major urban areas (PEPFAR, 2007), 80% of Malawi’s population live in rural areas (UNICEF, 2008). The absolute number of rural people who are infected currently outnumber urban residents by about 3 to 1 (National Statistical Office Malawi, 2005). The epidemic has a clear gendered dimension: women under age 24 are more than 3 times more likely than their male age peers to be infected in Malawi (National Statistical Office Malawi, 2005).
Individual risk factors for HIV in Malawi are well known. Only 30% of women and 47% of men report using condoms with their last non-spousal/non-regular partner (National Statistical Office Malawi, 2005), and condoms are often reserved for sex partners perceived as higher risk of HIV infection, especially extra-marital partners (Chimbiri, 2007). Over 20% of men and women who had a sexually-transmitted infection (STI) were also infected with HIV in 2005 (National Statistical Office Malawi, 2005). Multiple, concurrent sexual partnerships are also key determinants in the spread of HIV (Morris and Kretzschmar, 1997), and these partnerships are common in Malawi (Tawfik and Watkins, 2007). Migration also aids transmission and spread of HIV (Coffee et al., 2005): HIV prevalence is 4% higher among men who migrate (National Statistical Office Malawi, 2005). Lastly, voluntary HIV testing rates are low. In 2005, only 13% of women and 15% of men had ever been tested and received results for HIV; urban residents were twice as likely to be tested as rural residents (National Statistical Office Malawi, 2005).
Framing place in the context of HIV
Socio-ecological models suggest that individuals are both affected by, and affect, their physical and socio-cultural environment (McLeroy et al., 1988; Stokols et al., 1996) and that individuals, especially women, may embody the political, economic, and social forces of the environments in which they live (Krieger, 1999). Area-level factors, however, cannot cause HIV, and a sound theoretical model is needed to illuminate the pathways by which place may influence HIV status. Specifically, the Political Economy of Health (PEH) framework suggests that societal inequalities based on class, ethnicity or gender exacerbate conditions of poor health by fostering social isolation, economic deprivation, power differentials, and disparities in service provision (Minkler et al., 1994; Whiteside and De Waal, 2004). The PEH framework rejects placing blame on individuals for their poor health (Doyal and Pennell, 1979), favoring a holistic approach that considers the macro-level disparities and inequalities (Farmer, 1999), including gender differences (Doyal, 1995), that may reduce an individual’s choices and power to effect change.
Although the PEH does not specify constructs for investigation, the literature employing the PEH notes the role of both socio-economic disparities and limited access to services on facilitating inequities that have a negative effect on health outcomes (Farmer et al., 2006; Parker et al., 2000; Wellings et al., 2006). Primarily, previous research employing the PEH identifies both absolute poverty (Minkler, 1999) and the distribution of wealth (Kawachi and Kennedy, 1997) as key influences on poor health status. In the context of HIV, communities with higher levels of absolute poverty may not provide an environment that encourages adoption of healthy behaviors (Campbell and Jovchelovitch, 2000). Area-level income inequality is associated with increased individual-level HIV risk factors including presence of an STI (Holtgrave and Crosby, 2003) and concurrent sexual partnerships (Adimora and Schoenbach, 2002).
Second, the literature evoking the PEH posits that inequalities in access to roads and cities often reflect class differences (Doyal and Pennell, 1979): closer proximity provides an increase in livelihood opportunities and availability of services that contribute to differences in health outcomes. Road access and urban areas are associated with an increased risk of HIV transmission in part because opportunities for paid sex (Girdler-Brown, 1998) and multiple partnerships (Chirwa, 1997) increase in urban transit zones. Furthermore, the PEH calls attention to the effect of inequalities in healthcare access on health outcomes (Doyal and Pennell, 1979). In much of Africa, heath services are poorly distributed (Ruger and Kim, 2006); rural residents and women generally fare worse (UNAIDS, 2008).
Lastly, the PEH emphasizes that gendered power differentials have far-reaching, negative effects on the health of women (Doyal, 1995). Biological risk factors (Quinn and Overbaugh, 2005), combined with gender inequity (Luke, 2005), contribute to higher rates of HIV among women across much of sub-Saharan Africa (Kim and Watts, 2005). Poverty compounds gendered effects. In sub-Saharan Africa, some women depend on sexual relationships for financial support (Kelly et al., 2003; Luke, 2003; Masanjala, 2007), yet their ability to suggest or use condoms to protect themselves from HIV is often limited (Dunkle et al., 2004; Luke and Kurz, 2002). This creates an unfortunate irony that women’s desire for financial security may increase their risk of HIV (Craddock, 2000).
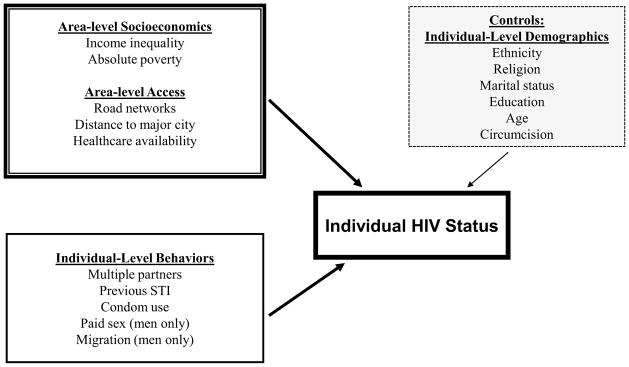
Therefore, guided by the PEH framework and the literature, this spatial study explores the empirical associations between individual HIV status and area-level socio-economic, accessibility, and gender-based inequities among men and women in rural Malawi. Based on our conceptual model, Figure 1, we hypothesize that:
Figure 1.
Area- and Individual-Level Influences on HIV Status in Malawi
Persons in areas of greater relative or absolute poverty and those with greater access to roads and urban areas will be more likely to be HIV infected. Those who live closer to Ministry of Health (MoH) clinics will be less likely to be HIV infected.
Relationships between both area- and individual-level factors will vary non-randomly in strength and magnitude over space.
The strength of associations will be greater for women than for men.
STUDY DESIGN AND METHODS
Individual-Level Data
Individual-level data come from the Malawi Demographic and Health Survey, 2004 (MDHS) (Table 1), a nationally-representative probability survey of demographics and health for women, ages 15–49, and men, ages 15–54. The standard DHS survey methodology is available from ORC Macro (ORC Macro, 1996). The MDHS uses the master sample frame from the Malawi 1998 census; enumeration areas serve as primary sampling units for the two-stage clustered sampling design (National Statistical Office Malawi, 2005). To target approximately 15,000 households, 522 clusters (64 urban and 458 rural) were randomly selected, and households were systematically sampled (National Statistical Office Malawi, 2005). All women aged 15–49 years who usually lived in the household were interviewed; every third household for the women’s interview was selected for the male questionnaire. The overall 2004 MDHS response rate was 98%.
Table 1.
Descriptive proportions of key variables among men and women
| % Women, n=2091 | % Men, n=1827 | |
|---|---|---|
| Age** | ||
| 15–19 | 12 | 12 |
| 20–24 | 26 | 21 |
| 25–29 | 19 | 20 |
| 30–34 | 16 | 16 |
| 35–39 | 11 | 11 |
| 40–44 | 10 | 10 |
| 45–49 | 7 | 6 |
| 50–54 | n/a | 3 |
| Religion | ||
| Christian | 37 | 38 |
| Muslim** | 12 | 10 |
| Catholic | 24 | 22 |
| Region** | ||
| North | 13 | 13 |
| Central | 39 | 43 |
| South | 48 | 45 |
| Ethnicity | ||
| Chewa | 34 | 35 |
| Yao | 13 | 12 |
| Lomwe | 18 | 18 |
| Education*** | ||
| None | 27 | 14 |
| Primary 0–4 | 64 | 65 |
| Grade 5 or higher | 9 | 21 |
| Marital status*** | ||
| Never married | 5 | 22 |
| Married/Union | 77 | 74 |
| Previously married | 18 | 4 |
| Wealth quintile (SES)*** | ||
| Lowest | 19 | 14 |
| Second | 24 | 23 |
| Middle | 25 | 27 |
| Fourth | 23 | 25 |
| Highest | 10 | 11 |
| Polygyny*** | 17 | 8 |
| Circumcised | n/a | 22 |
| Multiple partners in last year*** | 7 | 24 |
| Previous STI in last 12 months*** | 10 | 6 |
| Recent condom use*** | 4 | 14 |
| Ever had paid sex | n/a | 22 |
| Migrate | n/a | 12 |
| Risk score*** | ||
| 0 | 83 | 57 |
| 1 | 14 | 27 |
| 2 | 2 | 12 |
| 3 | 1 | 4 |
| HIV+ status*** | 13.8 | 9.6 |
Chi square results of difference in proportions,
p<.1,
p<.05,
p<.01
As part of the 2004 MDHS, all households selected for the male questionnaire were also selected for HIV testing. Participation in the HIV testing module was voluntary; testing and results were obtained using a standard protocol (ORC Macro, 2005). Of those selected, 2,485 rural women (response rate 71%) and 2,056 rural men (response rate 65%) accepted testing (National Statistical Office Malawi, 2005). For this study, the MDHS HIV sample is restricted to rural residents at risk of HIV through sexual transmission: 2,091 women and 1, 827 men.
The MDHS also collected Global Positioning System (GPS) data. For confidentiality, all clusters were randomly offset by up to 5km (MEASURE DHS, 2008). GPS coordinates are available for 456 rural clusters. Cluster points were projected in ArcGIS using UTM grid zone 36 south, referencing the WGS84 datum.
Area-Level Data
Area-level socio-economic data come from the Poverty Mapping Project at Columbia University, 2005 (Table 1) (Columbia University, 2008). Spatial units for the poverty mapping exercise are two to three combined rural aggregated enumeration areas (EA) from the 1998 Malawi census; units contain a minimum of 500 households. The complete dataset includes 20 measures of poverty and welfare linked to GIS shapefiles for 3004 rural units in Malawi (Benson, 2002). Towns and cities in rural areas are included. Details on methodology are available from Elbers, Lanjouw, and Lanjouw (Elbers et al., 2003) and the International Food Policy Research Institute (Benson et al., 2005).
Socio-economic status is measured by area-level Gini index and poverty headcount, two related, but distinct measures of poverty. The Gini index is a measurement of income inequality that shows the influence of economic disparities on health (Lindstrom and Lindstrom, 2006). High Gini and middle Gini variables were created by sorting all EAs by Gini coefficient, from low (greater equality) to high (greater inequality). Equal quartiles were created, and each quartile was assigned a rank from 1–4. In the analysis, group “1”, lowest Gini, serves as the reference for middle Gini (groups 2–3) and group “4”, high Gini. The poverty headcount is the percent of the population below the poverty line, a measure of economic deprivation (Krieger, 2003).
The three variables used to measure area-level access were derived from existing GIS maps of Malawi by calculating the Euclidean distance between each MDHS cluster point and the factor of interest. The distance to major roads and urban areas variables were created from digital files made for the 1998 census and available from the National Statistics Office. The locations of public Ministry of Health (MoH) facilities come from a Japanese International Cooperation Agency study from 1997–2002, available from the World Health Organization.
Combining Individual- and Area-level Variables
MDHS cluster information was spatially joined to the poverty and access geographic datasets using GIS software, ArcGIS (ESRI, 2008). Each DHS cluster was assigned the poverty and access information in the aggregate EA in which it was located. The complete area-level information was imported into STATA 9.2 (STATA, 2007) and merged with individual level data (including HIV), assigning the same area-level variables to every individual within each cluster, leaving individual-level information unique. Then, cluster coordinates for each individual were randomly scattered approximately 50 meters to provide a unique location.
DATA ANALYSIS
Multivariate, logistic GWR models are employed to test all individual- and area-level factors (Fotheringham et al., 2002) using GWR3 software (Fotheringham, 2005). Logistic models are fitted using iteratively reweighted least squares. GWR3 produces two types of results. First, similar to traditional population-averaged logistic regression models, GWR3 calculates an overall model of global associations with parameter estimates, standard errors, odds ratios and t-values. Second, GWR calculates local parameter estimates at each observation point, determining associations between predictors and HIV status for 2,091 women and 1,827 men.
To estimate local models, the influence of observations within a specific geographic range are determined using a distance decay weighting system that assigns more weight to observations closer to the local regression point than to those farther away. Selection of the optimal bandwidth is automated using a cross validation (CV) approach for separate models for men and women. This convergence process determines the bandwidth for all regression points, reducing the CV score until stable global and local parameters are found. Monte Carlo simulation tests compare the variance of the observed model parameters against 100 random calibrations of the same model, providing t-statistics of significance for local parameters (Fotheringham et al., 2002). To display the local model results and facilitate interpretation, t-statistics from individual regression points are used to predict parameter values over continuous space through interpolation using the ArcGIS Spatial Analyst spline tool.
RESULTS AND DISCUSSION
Descriptive statistics
Individual-level characteristics are detailed in Table 1. While 7% of women had more than one partner in the last year, 24% of men had multiple sexual partners in the same timeframe (p<.01). Among those who have sex, 4% of women and 14% of men used a condom with a recent sex partners (p<.01). Also, 10% of women and 6% of men (p<.01) had a sexually transmitted infection or its symptoms in the previous 12 months. Among men, 22% had ever paid for sex. Among those tested, 13.8% of women and 9.6% of men were infected with HIV.
As expected, men and women live the same average distance from a major city (73km), major road (11km), and MoH clinic (5km). The average poverty percent is 65%. Area-level Gini mean is .35 (range .12 to .67); as defined, approximately 50% of women and men live in areas of middle income inequality.
Global associations between individual- and area-level risk factors and HIV
Global models (Table 2) are spatially stationary and represent population-averaged results. Among women, those with STIs are more likely to be infected with HIV (OR 1.84, p<.01), and use of condoms with a recent sex partner increases the odds of HIV infection by 2.01 (p<.01). Surprisingly, multiple partners are not associated with HIV status in the global model. Among area-level factors, and in contrast to hypotheses, the odds of infection decrease with increasing distance to an MoH clinic (OR 0.94, p<.01). There are no other significant associations between area-level factors and HIV status at the global level.
Table 2.
Global model parameters for women and men
| Women | Men | |||||
|---|---|---|---|---|---|---|
| Parameter | Estimate | t-value | Odds Ratio | Estimate | t-value | Odds Ratio |
| Intercept | −4.08 (0.68) | −5.99*** | 0.02 | −4.30 (0.63) | −6.79*** | 0.014 |
| Individual-level demographic | ||||||
| Age | 0.02 (0.001) | 2.63*** | 1.02 | 0.03 (0.01) | 2.77*** | 1.03 |
| Education | −0.02 (0.13) | −0.19 | 0.98 | 0.05 (0.15) | 0.30 | 1.05 |
| Current marriage | 1.20 (0.46) | 2.59*** | 3.33 | 2.12 (0.47) | 4.51*** | 8.31 |
| Previous Marriage | 2.05 (0.46) | 4.44*** | 7.73 | 1.57 (0.59) | 2.66*** | 4.78 |
| Polygyny | 0.22 (0.19) | 1.17 | 1.24 | −0.09 (0.34) | −0.25 | 0.91 |
| SES | 0.25 (0.06) | 4.48*** | 1.28 | 0.25 (0.08) | 3.27*** | 1.28 |
| Chewa | −0.65 (0.20) | −3.26*** | 0.52 | −0.73 (0.25) | −2.94*** | 0.48 |
| Lomwe | 0.27 (0.19) | 1.41 | 1.31 | 0.25 (0.23) | 1.06 | 1.28 |
| Yao | 0.25 (0.27) | 0.92 | 1.28 | −0.19 (0.37) | −0.50 | 0.82 |
| Christian | 0.03 (0.15) | 0.17 | 1.02 | 0.04 (0.18) | 0.18 | 1.03 |
| Muslim | 0.08 (0.27) | 0.30 | 1.08 | 0.11 (0.40) | 0.28 | 1.12 |
| Circumcised | 0.01 (0.24) | 0.05 | 1.01 | |||
| Individual-level risk factors | ||||||
| Multiple partners | 0.40 (0.28) | 1.44 | 1.49 | 0.05 (0.28) | 0.16 | 1.05 |
| STI | 0.61 (0.20) | 3.02*** | 1.84 | 0.71 (0.31) | 2.33*** | 2.04 |
| Condom use | 0.70 (0.31) | 2.27*** | 2.01 | 0.44 (0.27) | 1.59 | 1.54 |
| Paidsex | 0.06 (0.20) | 0.29 | 1.06 | |||
| Migrate | 0.42 (0.25) | 1.72 | 1.52 | |||
| Area-level factors | ||||||
| Gini high | 0.19 (0.19) | 1.00 | 1.21 | −0.24 (0.245) | −0.98 | 0.78 |
| Gini middle | −0.01 (0.17) | −0.056 | 0.99 | 0.04 (0.205) | 0.17 | 1.03 |
| Km to MoH clinic | −0.06 (0.03) | −2.34*** | 0.94 | −0.07 (0.03) | −2.12** | 0.93 |
| Km to Major road | −0.01 (0.01) | −1.90 | 0.99 | −0.01 (0.01) | −1.49 | 0.98 |
| Km to Major city | 0.00 (0.00) | 0.36 | 1.00 | 0.00 (0.00) | 0.23 | 1.00 |
| Poverty % | 0.00 (0.00) | 0.15 | 1.00 | 0.00 (0.00) | 0.56 | 1.00 |
| Log-likelihood: | −797.35 | −512.79 | ||||
| Akaike Information Criterion: | 1640.70 | 1079.57 | ||||
| Corrected AIC (AICc) | 1641.23 | 1080.41 | ||||
Standard errors in parentheses.
p<.1,
p<.05,
p<..01
For men, among individual risk factors, only previous STI is significantly associated with HIV (OR 2.04, p<.01). Among area-level factors, similar to women, men who live further from MoH clinics are less likely to be infected (OR 0.93, p<.05). No other area-level factors are significantly associated with HIV status for men.
From global to local models: mapping spatial variation of relationships
Local spatial regression models provide a specificity of area- and individual-level associations with HIV status based on geographic location. Local regression models may be interpreted as average effects of the independent variable of interest on HIV status among men or women in a specific location, controlling for other factors.
All variables from the global multivariate model are tested in local multivariate models stratified by gender. Decreased Akaike Information Criterion (AIC) (corrected) from global to local models suggests the local model fits the data better; a decrease of more than 3 points is significant (Fotheringham et al., 2002). Among women, the 15 point drop suggests that local models are a better fit and demonstrates that global models may mask considerable spatial variation. The 5 point drop in the AIC from the global to the local model for men suggests only a small increase in fit, signifying less spatial variation.
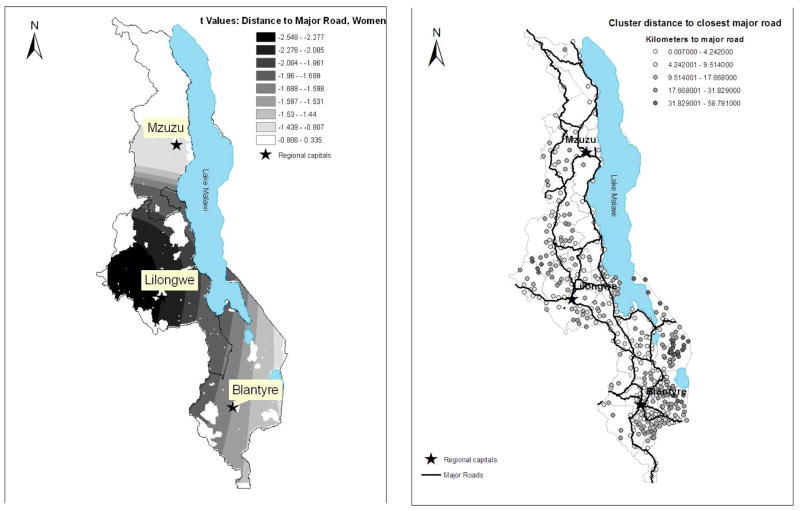
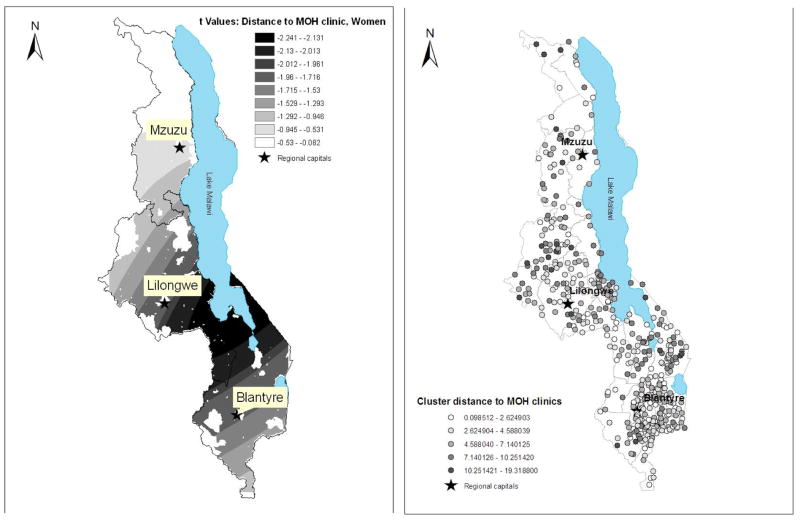
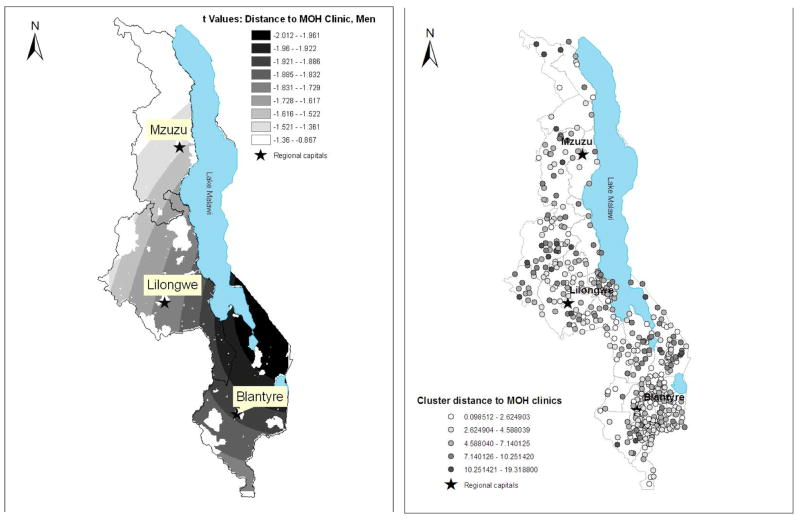
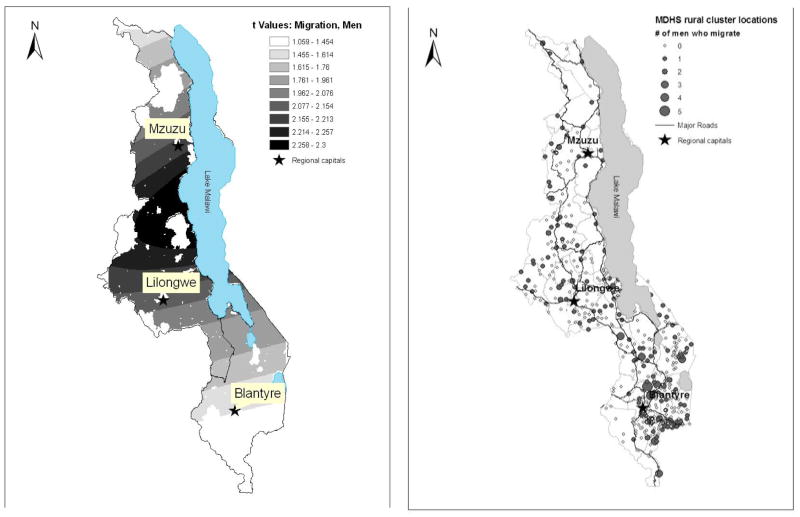
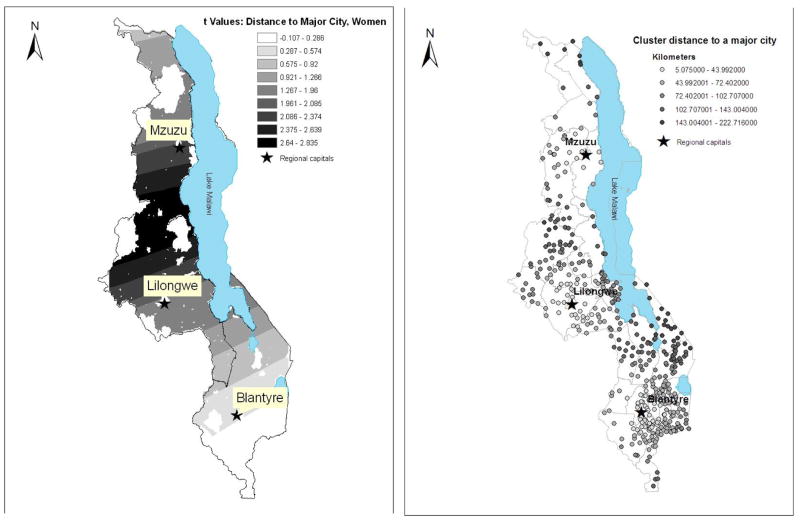
Local regression model results are presented in Tables 3 and 4. Student t-values of ±1.96 indicate significance at the .05 level. Factors that are significant for more than 10% of the study population are illustrated in Figures 2–4 for women and Figures 5–6 for men. In each map pairing, local t-statistics are mapped on the left side. Darker shades indicate locations where the variable of interest is significantly associated with odds of HIV infection. Paired maps on the right show the distribution of the variable of interest within the study population.
Table 3.
Comparison of Local Parameter summaries to global parameter for women
| Label | From Local Parameter Model | Global model parameter | |||||
|---|---|---|---|---|---|---|---|
| Min. | Lwr Quartile | Median | Upr Quartile | Max. | % with sig. local t value | ||
| Intercept | −7.45 | −5.33 | −4.31 | −3.96 | −3.59 | 100 | −4.08 |
| Demographic factors | |||||||
| Age | 0.02 | 0.02 | 0.02 | 0.02 | 0.04 | 83 | 0.02 |
| Education | −0.36 | −0.03 | 0.01 | 0.02 | 0.03 | 0 | −0.02 |
| Chewa | −0.80 | −0.73 | −0.58 | −0.41 | 0.15 | 65 | −0.65 |
| Lomwe | −0.95 | 0.07 | 0.11 | 0.34 | 0.53 | 0 | 0.27 |
| Yao | 0.03 | 0.06 | 0.11 | 0.35 | 0.84 | 0 | 0.25 |
| Christian | −0.05 | −0.00 | 0.02 | 0.03 | 0.85 | 0 | 0.03 |
| Muslim | −0.32 | −0.16 | 0.02 | 0.09 | 0.17 | 0 | 0.08 |
| Previous marriage | 1.26 | 2.17 | 2.36 | 2.42 | 2.48 | 91 | 2.05 |
| Current marriage | −0.17 | 1.29 | 1.51 | 1.62 | 1.67 | 80 | 1.20 |
| Polygyny | −0.62 | 0.16 | 0.31 | 0.42 | 0.51 | 30 | 0.22 |
| SES | 0.21 | 0.24 | 0.26 | 0.27 | 0.70 | 100 | 0.25 |
| Individual-level risk factors | |||||||
| Multiple partners | 0.25 | 0.31 | 0.34 | 0.39 | 1.55 | 0 | 0.40 |
| STI | 0.50 | 0.55 | 0.57 | 0.65 | 1.14 | 93 | 0.61 |
| Condom use | 0.47 | 0.54 | 0.60 | 0.71 | 0.85 | 6 | 0.67 |
| Area-level factors | |||||||
| Gini high | 0.05 | 0.21 | 0.23 | 0.24 | 0.26 | 0 | 0.19 |
| Gini medium | −0.52 | 0.04 | 0.04 | 0.05 | 0.10 | 0 | −0.01 |
| Km to MOH | −0.06 | −0.06 | −0.05 | −0.05 | −0.01 | 29 | −0.06 |
| Km major road | −0.03 | −0.02 | −0.01 | −0.01 | 0.01 | 25 | −0.01 |
| Km to major city | 0.00 | 0.00 | 0.00 | 0.01 | 0.01 | 27 | 0.00 |
| Poverty % | −0.01 | −0.00 | 0.00 | 0.01 | 0.02 | 2 | 0.00 |
| Local Logistic Model Diagnostics | |||||||
| Log Likelihood: | −767.07 | ||||||
| Akaike Information Criterion | 1623.78 | ||||||
| Corrected AIC | 1625.79 | ||||||
Table 4.
Comparison of Local Parameter values to global model for men
| Label | From Local Parameter Model | Global model parameter | |||||
|---|---|---|---|---|---|---|---|
| Min. | Lwr Quartile | Median | Upr Quartile | Max. | % with sig. local t value | ||
| Intercept | −6.46 | −4.78 | −4.24 | −3.95 | −3.79 | 100 | −5.44 |
| Demographic factors | |||||||
| Age | 0.04 | 0.04 | 0.04 | 0.05 | 0.06 | 100 | 0.03 |
| Education | −0.23 | −0.11 | 0.02 | 0.19 | 0.69 | 5 | 0.05 |
| Chewa | −0.82 | −0.81 | −0.79 | −0.69 | −0.25 | 90 | −0.73 |
| Lomwe | 0.06 | 0.11 | 0.21 | 0.34 | 0.64 | 0 | 0.23 |
| Yao | −0.59 | −0.28 | −0.26 | −0.25 | −0.20 | 0 | −0.19 |
| Christ | −0.12 | −0.04 | 0.06 | 0.19 | 0.31 | 0 | 0.04 |
| Muslim | −0.33 | −0.19 | −0.02 | 0.23 | 1.43 | 0 | 0.11 |
| Married | 2.07 | 2.11 | 2.15 | 2.19 | 2.52 | 100 | 2.12 |
| Previously married | 1.17 | 1.21 | 1.26 | 1.32 | 2.94 | 46 | 1.57 |
| Polygyny | −0.47 | 0.16 | 0.34 | 0.43 | 0.47 | 0 | −.09 |
| SES | 0.07 | 0.19 | 0.23 | 0.27 | 0.31 | 87 | 0.25 |
| Circum | −0.56 | −0.04 | 0.04 | 0.07 | 0.09 | 0 | 0.01 |
| Individual-level risk factors | |||||||
| Multiple partners | −0.56 | −0.55 | −0.53 | −0.51 | −0.44 | 0 | 0.05 |
| STI | 0.48 | 0.67 | 0.72 | 0.78 | 0.86 | 75 | 0.71 |
| Condom use | 0.37 | 0.44 | 0.49 | 0.54 | 0.85 | 0 | 0.44 |
| Paidsex | −0.21 | 0.12 | 0.17 | 0.19 | 0.22 | 0 | 0.06 |
| Migrate | 0.35 | 0.43 | 0.51 | 0.59 | 0.68 | 47 | 0.42 |
| Area-level factors | |||||||
| Gini high | −0.46 | −0.39 | −0.32 | −0.25 | −0.18 | 0 | −0.24 |
| Gini mid | −0.66 | −0.08 | 0.04 | 0.11 | 0.14 | 0 | 0.04 |
| KM to MOH | −0.07 | −0.07 | −0.06 | −0.06 | −0.05 | 10 | −0.07 |
| Km to major road | −0.02 | −0.02 | −0.02 | −0.02 | −0.01 | 0 | −0.01 |
| Km to major city | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0 | 0.00 |
| Poverty % | −0.00 | 0.00 | 0.00 | 0.01 | 0.02 | 0 | 0.00 |
| Local Logistic Model Diagnostics | |||||||
| Log Likelihood | −497.81 | ||||||
| Akaike Information Criterion | 1073.53 | ||||||
| Corrected AIC | 1075.27 | ||||||
Figure 2.
Distance to major road, women
Figure 4.
Distance to MOH, women
Figure 5.
Distance to MOH, men
Figure 6.
Migration, men
Local spatial variation among women
Although individual risk factors are significant (Table 3), the significance of three area-level access factors above the contribution of individual-level influences illustrates the importance of place-based effects.
First, distance to a major road is negatively and significantly associated with HIV status for 25% of women located in the Central Region near transportation arteries connecting Lilongwe and areas along the Mozambique border (Figure 2). Women who live closer to a major road in this area have increased odds of HIV infection. This finding supports a recent study in South Africa concluding that women living in homesteads closer to a road were more likely to be infected than women who lived further from main transportation arteries (Tanser et al., 2000).
Second, distance to a major city is also significant and negative for 27% of the sample clustered in the middle of the country between Lilongwe and Mzuzu (Figure 3). Women in this area who live closer to a major city are more likely to be infected. Both these findings support the link between increased access and increased risk of HIV for women in specific locations. More access to roads may increase risk behaviors through increased access to markets and social networks, resulting in additional sex partners (Tawfik and Watkins, 2007). In contrast, in more isolated locations, including those in the Central Region, distance or cost of travel may be prohibitive, potentially reducing risk behaviors associated with urban areas.
Figure 3.
Distance to major city, women
Third, similar to the global model, distance to an MoH clinic is negatively associated with HIV status: women who live closer to an MoH clinic are more likely to be infected than women who live further from an MoH clinic (Figure 4). This relationship is significant for 29% of women clustered in the Central and Southern Regions. The direction of this association is unexpected, conflicting with previous research showing proximity to health centers as protective against HIV for women (Gabrysch et al., 2008). It is unlikely that access to these services increases a woman’s likelihood of infection. Rather, because MoH health facilities are typically located in small population and transit areas (Ministry of Health, 2007), it is probable that clinics serve as a proxy for small market centers where women may engage in higher risk behavior such as extramarital partnerships (Swidler & Watkins, 2007), increasing their risk of infection.
Although not shown, individual-level risk factors also exemplify significant spatial variation. Previous sexually transmitted infection is significantly and positively associated with HIV status for 93% of women covering the entire Central and Southern Regions of the country. Condom use is significant in fewer than 10% of local models. Multiple partnerships is not significant in any location.
Overall, the significance of the area-level variables in local models, over and above the contribution of known individual-level risk behaviors, suggests that global associations dilute important drivers of HIV in specific geographic areas. In particular, and as supported by the PEH, differences in access lead to variations in HIV transmission patterns: women with more access to roads, cities, and clinics are more likely to be infected likely due to increased mobility (Porter, 2002) and engagement in subsequent risk behaviors (Mtika, 2007). As a corollary, in this situation, exclusion and isolation appears protective. Contrary to the conceptual model, income inequality and absolute poverty are not associated with HIV status in global or local models. This lack of association may be due to the pervasive nature of poverty in rural Malawi, masking relationships that might be evident in more economically diverse areas.
Spatial variation among men
As expected from the global model, among men there is little spatial variation and few significant factors associated with HIV at the local level (Table 4). Three risk factors show significant spatial variation at the local level, providing only a marginal improvement over the global model.
Among area-level factors, only distance to an MoH clinic is significantly associated with HIV status. For 10% of men clustered near the southern shores of Lake Malawi along the border with Mozambique (Figure 5), those who live further from an MoH clinic are significantly less likely to be infected. Similar to the women, this relationship contradicts previous research noting the association between active health workers and decreased HIV-related risk behaviors among men in Zambia (Benefo, 2008). As suggested previously, however, distance to an MoH clinic is likely a proxy for distance to a smaller commercial center. In Malawi, transit zones are associated with paid sex and multiple partnerships among men (Chirwa, 1997), factors that increase risk of HIV. Therefore, it is possible that small commercial hubs in these lakefront districts may be dissimilar to other locations in Malawi increasing the likelihood of infection in these specific locations.
Among individual risk factors, migration is significant and positive for 47% of men in local models (Figure 6), demonstrating the value of local models for revealing relationships diluted at the global level. In areas of significance, mostly between the districts of Mangochi and central Mazimba (including areas around Lilongwe and Mzuzu), men may have distinct internal or external migration patterns. These locations of higher risk may facilitate behaviors, including multiple partnerships, that increase the likelihood of infection.
Overall, and as forecast by the PEH, the dearth of significant associations may reflect the heightened status of men in comparison to women (Doyal, 1995). In Malawi, men typically have more access to income and hold more social power than women (Schatz, 2005). Social norms of masculinity and marriage often include controlling women (Chirwa, 1997), providing men with decision-making power over partner selection and use of condoms (Kaler, 2003). Improvements in rural infrastructure may also enable men’s mobility, buffering the influences of area-level socioeconomic and access factors.
CONCLUSION
This study demonstrates that place matters in the context of HIV in rural Malawi, and that area-level access factors play a significant role in increasing HIV risk above and beyond individual-level contributions in specific locations. Among women, access to major roads, major cities, and health clinics in distinct areas increases the likelihood of infection, providing a cautionary note for future development. Among men, HIV status is strongly associated with migration patterns in specific areas; the lack of significant area-level drivers may result from the buffering effect of men’s higher societal status.
This spatial analysis leads to two important conclusions. First, ecological factors such as economic underdevelopment, access, and power differentials appear to create social and economic risk environments in particular areas. Drawing on the PEH and the conceptual model for interpretation (Figure 1), area-level inequalities in these specific locations likely limit individual choice, constrain behavior, and restrict ability to make positive health decisions (Doyal, 1995; Doyal and Pennell, 1979; Minkler, 1999), thus increasing vulnerability to HIV infection (Farmer et al., 2006; Parker et al., 2000). Second, gender plays a role in the spatial determinants of HIV. The PEH posits that socio-economic environments may reinforce gender inequality, exacerbating the influence of area-level factors on HIV status (Doyal, 1995). As men generally control the specifics of sex (Sayles et al., 2006), women may be left with limited power to protect themselves against HIV in rural Malawi (Kathewera-Banda, 2005). In Malawi, the interactive of effects of area-level factors and gender on HIV status may be more pronounced in specific geographic locations.
Using spatial methods to explore place-based effects on HIV in Malawi presents several challenges. First, people are likely to self select into neighborhoods, making area-level effects less than randomly distributed among the populations (Oakes, 2004). Also, geographic information from developing countries is sparse, and combining multiple geographic layers from various sources with different scales may add small errors in location information, potentially allocating individuals to incorrect geographic areas. Although government health facilities provide the majority of care, excluding other clinic options has unknown effects on measuring access to health services. The magnitude and direction of biases cannot be determined with the available data.
Overall, the results contribute to the growing body of evidence connecting health and place by expanding application of spatial methods to exploration of both individual- and area-level risk factors for HIV. To slow the spread of HIV in rural Malawi, successful interventions need to account for differences between both individuals and the areas in which they live, and policies must be locally adapted to address these variations. Although this study reveals where area- and individual-level factors drive HIV in rural Malawi, why and how HIV is influenced by these factors remain unanswered. Additional studies at finer spatial scales, and complementary qualitative research focused on identification of the specific characteristics of women and men in the higher risk areas identified in this study, would help elucidate these relationships and facilitate the development of tailored policy and intervention.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Adimora AA, Schoenbach VJ. Contextual factors and the black-white disparity in heterosexual HIV transmission. Epidemiology. 2002;13:707–712. doi: 10.1097/00001648-200211000-00016. [DOI] [PubMed] [Google Scholar]
- Armour L. Trying to survive in times of poverty and AIDS: women and multiple-partner sex in Malawi. Aids Care-Psychological and Socio-Medical Aspects of AIDS/HIV. 2006;18:404–404. [Google Scholar]
- Barden-O’Fallon JL, deGraft-Johnson J, Bisika T, Sulzbach S, Benson A, Tsui AO. Factors associated with hiv/aids knowledge and risk perception in rural Malawi. Aids and Behavior. 2004;8:131–140. doi: 10.1023/B:AIBE.0000030244.92791.63. [DOI] [PubMed] [Google Scholar]
- Bello GA, Chipeta J, Aberle-Grasse J. Assessment of trends in biological and behavioural surveillance data: is there any evidence of declining HIV prevalence or incidence in Malawi? British Medical Journal. 2006;82:i9. doi: 10.1136/sti.2005.016030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benefo KD. Determinants of Zambian Men’s Extra-Marital Sex: A Multi-level Analysis. Archives of Sexual Behavior. 2008;37:517–529. doi: 10.1007/s10508-007-9243-7. [DOI] [PubMed] [Google Scholar]
- Benson T. Correlates of poverty measures in Malawi—An application of poverty mapping at the sub-district scale. Conference on Understanding Poverty and Growth in Sub-Saharan Africa, Centre for the Study of African Economies; St. Catherine’s College, Oxford, UK. 2002. pp. 18–19. [Google Scholar]
- Benson T, Chamberlin J, Rhinehart I. An investigation of the spatial determinants of the local prevalence of poverty in rural Malawi. Food Policy. 2005;30:532–550. [Google Scholar]
- Campbell C, Jovchelovitch S. Health, community and development: towards a social psychology of participation. Journal of Community & Applied Social Psychology. 2000;10:255–270. [Google Scholar]
- Chimbiri AM. The condom is an ‘intruder’ in marriage: Evidence from rural Malawi. Social Science & Medicine. 2007;64:1102–1115. doi: 10.1016/j.socscimed.2006.10.012. [DOI] [PubMed] [Google Scholar]
- Chirwa WC. Migrant labour, sexual networking and multi-partnered sex in Malawi. Health Transition Review. 1997;7:5–15. [Google Scholar]
- Coffee MP, Garnett GP, Mlilo M, Voeten H, Chandiwana S, Gregson S. Patterns of movement and risk of HIV infection in rural Zimbabwe. Journal of Infectious Diseases. 2005;191:S159–S167. doi: 10.1086/425270. [DOI] [PubMed] [Google Scholar]
- Columbia University. Poverty Mapping Project: The Center for International Earth Science Information Network. 2008. [Google Scholar]
- Craddock S. Disease, social identity, and risk: rethinking the geography of AIDS. Transactions of the Institute of British Geographers. 2000;25:153–168. [Google Scholar]
- Diez Roux AV. Estimating neighborhood health effects: the challenges of causal inference in a complex world. Social Science & Medicine. 2004;58:1953–1960. doi: 10.1016/S0277-9536(03)00414-3. [DOI] [PubMed] [Google Scholar]
- Doyal L. What Makes Women Sick: Gender and the Political Economy of Health. Rutgers University Press; 1995. [Google Scholar]
- Doyal L, Pennell I. The Political Economy of Health. Pluto Press; 1979. [Google Scholar]
- Dunkle KL, Jewkes RK, Brown HC, Gray GE, McIntryre JA, Harlow SD. Transactional sex among women in Soweto, South Africa: prevalence, risk factors and association with HIV infection. Social Science & Medicine. 2004;59:1581–1592. doi: 10.1016/j.socscimed.2004.02.003. [DOI] [PubMed] [Google Scholar]
- Elbers C, Lanjouw JO, Lanjouw P. Micro-Level Estimation of Poverty and Inequality. Econometrica. 2003;71:355–364. [Google Scholar]
- Entwisle B. Putting people into place. Demography. 2007;44:687–703. doi: 10.1353/dem.2007.0045. [DOI] [PubMed] [Google Scholar]
- ESRI. ArcGIS. 9.2. ESRI; 2008. [Google Scholar]
- Farmer P. Infections and Inequalities: The Modern Plagues. University of California Press; 1999. [Google Scholar]
- Farmer P, Nizeye B, Stulac S, Keshavjee S. Structural violence and clinical medicine. PLoS Med. 2006;3:e449. doi: 10.1371/journal.pmed.0030449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fotheringham AS. GWR. 3.0 2005. [Google Scholar]
- Fotheringham AS, Brunsdon C, Charlton M. Geographically Weighted Regression: The Analysis of Spatially Varying Relationships. Wiley; 2002. [Google Scholar]
- Gabrysch S, Edwards T, Glynn JR. The role of context: neighbourhood characteristics strongly influence HIV risk in young women in Ndola, Zambia. Trop Med Int Health. 2008;13:162–170. doi: 10.1111/j.1365-3156.2007.01986.x. [DOI] [PubMed] [Google Scholar]
- Girdler-Brown B. Eastern and Southern Africa. International Migration. 1998;36:513–551. doi: 10.1111/1468-2435.00058. [DOI] [PubMed] [Google Scholar]
- Heard NJ, Larsen U, Hozumi D. Investigating access to reproductive health services using GIS: Proximity to services and the use of modern contraceptives in Malawi. African Journal of Reproductive Health. 2004:164–179. [PubMed] [Google Scholar]
- Hobfoll SE. Ecology, community, and AIDS prevention. Am J Community Psychol. 1998;26:133–144. doi: 10.1023/a:1021838325362. [DOI] [PubMed] [Google Scholar]
- Holtgrave DR, Crosby RA. Social capital, poverty, and income inequality as predictors of gonorrhoea, syphilis, chlamydia and AIDS case rates in the United States. Med Soc Vener Dis. 2003:62–64. doi: 10.1136/sti.79.1.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaler A. “My girlfriends could fill a yanu-yanu bus”: Rural Malawian men’s claims about their own serostatus. Demographic Research. 2003:349–372. [Google Scholar]
- Kandala NB, Magadi MA, Madise NJ. An investigation of district spatial variations of childhood diarrhoea and fever morbidity in Malawi. Social Science & Medicine. 2006;62:1138–1152. doi: 10.1016/j.socscimed.2005.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kathewera-Banda MGCF, Hendriks S, Kachika T, Mitole Z, White S. Sexual violence and women’s vulnerability to HIV transmission in Malawi: a rights issue. International Social Science Journal. 2005;57:649–660. [Google Scholar]
- Kawachi I, Kennedy BP. Socioeconomic determinants of health: Health and social cohesion: why care about income inequality? British Medical Journal. 1997;314:1037. doi: 10.1136/bmj.314.7086.1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazembe LN, Muula AS, Simoonga C. Joint spatial modeling of common morbidities of childhood fever and diarrhoea in Malawi. Health and Place. 2009;15:165–172. doi: 10.1016/j.healthplace.2008.03.009. [DOI] [PubMed] [Google Scholar]
- Kelly RJ, Gray RH, Sewankambo NK, Serwadda T, Wabwire-Mangen F, Lutalo T, Wawer MJ. Age differences in sexual partners and risk of HIV-1 infection in rural Uganda. Jaids-Journal of Acquired Immune Deficiency Syndromes. 2003;32:446–451. doi: 10.1097/00126334-200304010-00016. [DOI] [PubMed] [Google Scholar]
- Kim JC, Watts CH. Gaining a foothold: tackling poverty, gender inequality, and HIV in Africa. British Medical Journal. 2005;331:0. doi: 10.1136/bmj.331.7519.769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleinschmidt I, Pettifor A, Morris N, MacPhail C, Rees H. Geographic distribution of human immunodeficiency virus in South Africa. Am J Trop Med Hyg. 2007;77:1163–1169. [PMC free article] [PubMed] [Google Scholar]
- Kohler HP, Behrman JR, Watkins SC. Social networks and HIV/AIDS risk perceptions. Demography. 2007;44:1–33. doi: 10.1353/dem.2007.0006. [DOI] [PubMed] [Google Scholar]
- Krieger N. Embodying Inequality: A review of concepts, measures, and methods for studying health consequences of discrimination. International Journal of Health Services. 1999;29:295–352. doi: 10.2190/M11W-VWXE-KQM9-G97Q. [DOI] [PubMed] [Google Scholar]
- Krieger N. Monitoring socioeconomic inequalities in sexually transmitted infections, tuberculosis, and violence: Geocoding and choice of area-based socioeconomic measures - The public health disparities geocoding project (US) Public Health Reports. 2003;118:240–260. doi: 10.1093/phr/118.3.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lachaud JP. HIV prevalence and poverty in Africa: Micro-and macro-econometric evidences applied to Burkina Faso. Journal of Health Economics. 2007;26:483–504. doi: 10.1016/j.jhealeco.2006.10.007. [DOI] [PubMed] [Google Scholar]
- Lindstrom C, Lindstrom M. “Social capital,” GNP per capita, relative income, and health: An ecological study of 23 countries. International Journal of Health Services. 2006;36:679–696. doi: 10.2190/C2PP-WF4R-X081-W2QN. [DOI] [PubMed] [Google Scholar]
- Luke N. Age and economic asymmetries in the sexual relationships of adolescent girls in sub-Saharan Africa. Studies in Family Planning. 2003;34:67–86. doi: 10.1111/j.1728-4465.2003.00067.x. [DOI] [PubMed] [Google Scholar]
- Luke N. Confronting the ‘sugar daddy’ stereotype: age and economic asymmetries and risky sexual behavior in urban Kenya. Int Fam Plan Perspect. 2005;31:6–14. doi: 10.1363/3100605. [DOI] [PubMed] [Google Scholar]
- Luke N, Kurz KM. Cross-generational and transactional sexual relations in sub-Saharan Africa: Prevalence of behavior and implications for negotiating safer sexual practices. Population Services International; Washington, D.C: 2002. [Google Scholar]
- Macintyre S, Ellaway A, Cummins S. Place effects on health: how can we conceptualise, operationalise and measure them? Social Science & Medicine. 2002;55:125–139. doi: 10.1016/s0277-9536(01)00214-3. [DOI] [PubMed] [Google Scholar]
- Masanjala W. The poverty-HIV/AIDS nexus in Africa: A livelihood approach. Social Science & Medicine. 2007;64:1032–1041. doi: 10.1016/j.socscimed.2006.10.009. [DOI] [PubMed] [Google Scholar]
- McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Education & Behavior. 1988;15:351. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- MEASURE DHS. Geographic Information Methodology -Collecting Geographic Data. 2008. [Google Scholar]
- Ministry of Health; Department of Health Planning & Policy Development. Malawi National Health Accounts (NHA) 2002–2004 with Subaccounts for HIV and AIDS, Reproductive and Child Health. Lilongwe, Malawi: 2007. [Google Scholar]
- Minkler M. Personal responsibility for health? A review of the arguments and the evidence at century’s end. Health Education & Behavior. 1999;26:121. doi: 10.1177/109019819902600110. [DOI] [PubMed] [Google Scholar]
- Minkler M, Wallace SP, McDonald M. The political economy of health: a useful theoretical tool for health education practice. International Quarterly of Community Health Education. 1994;15:111–125. doi: 10.2190/T1Y0-8ARU-RL96-LPDU. [DOI] [PubMed] [Google Scholar]
- Morris M, Kretzschmar M. Concurrent partnerships and the spread of HIV. AIDS. 1997;11:641–648. doi: 10.1097/00002030-199705000-00012. [DOI] [PubMed] [Google Scholar]
- Mtika MM. Political economy, labor migration, and the AIDS epidemic in rural Malawi. Social Science & Medicine. 2007;64:2454–2463. doi: 10.1016/j.socscimed.2007.04.006. [DOI] [PubMed] [Google Scholar]
- National Statistical Office Malawi. Malawi Demographic and Health Survey 2004. NSO and ORC Macro; Calverton, MD: 2005. [Google Scholar]
- Oakes JM. The (mis) estimation of neighborhood effects: causal inference for a practicable social epidemiology. Social Science & Medicine. 2004;58:1929–1952. doi: 10.1016/j.socscimed.2003.08.004. [DOI] [PubMed] [Google Scholar]
- ORC Macro. Sampling Manual, DHS-III Basic Documentation. Calverton, Maryland: 1996. [Google Scholar]
- ORC Macro. HIV testing laboratory manual: Demographic and Health Surveys. Calverton MD: ORC Macro; 2005. [Google Scholar]
- Parker RG, Easton D, Klein CH. Structural barriers and facilitators in HIV prevention: a review of international research. AIDS. 2000;14:S22–S32. doi: 10.1097/00002030-200006001-00004. [DOI] [PubMed] [Google Scholar]
- PEPFAR. Country Profile. Malawi: 2007. [Google Scholar]
- Porter G. Living in a walking world: Rural mobility and social equity issues in sub-Saharan Africa. World Development. 2002;30:285–300. [Google Scholar]
- Quinn TC, Overbaugh J. HIV/AIDS in women: an expanding epidemic. Science. 2005;308:1582–1583. doi: 10.1126/science.1112489. [DOI] [PubMed] [Google Scholar]
- Ruger JP, Kim HJ. Global health inequalities: an international comparison. Journal of Epidemiology and Community Health. 2006;60:928–936. doi: 10.1136/jech.2005.041954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sayles JN, Pettifor A, Wong MD, MacPhail C, Lee SJ, Hendriksen E, Rees HV, Coates T. Factors associated with self-efficacy for condom use and sexual negotiation among South African youth. J Acquir Immune Defic Syndr. 2006;43:226–233. doi: 10.1097/01.qai.0000230527.17459.5c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schatz E. ‘Take your mat and go’! Rural Malawian women’s strategies in the HIV/AIDS era. Culture Health & Sexuality. 2005;7:479–492. doi: 10.1080/13691050500151255. [DOI] [PubMed] [Google Scholar]
- Smith KP. Perceptions of risk and strategies for prevention: responses to HIV/AIDS in rural Malawi. Social Science & Medicine. 2005;60:649–660. doi: 10.1016/j.socscimed.2004.06.009. [DOI] [PubMed] [Google Scholar]
- STATA. 2007;9.2 [Google Scholar]
- Stokols D, Allen J, Bellingham RL. The social ecology of health promotion: implications for research and practice. Am J Health Promot. 1996;10:247–251. doi: 10.4278/0890-1171-10.4.247. [DOI] [PubMed] [Google Scholar]
- Tanser F. New approaches to spatially analyse primary health care usage patterns in rural South Africa. Tropical Medicine & International Health. 2001;6:826–838. doi: 10.1046/j.1365-3156.2001.00794.x. [DOI] [PubMed] [Google Scholar]
- Tanser F, Barnighausen T, Cooke GS, Newell ML. Localized spatial clustering of HIV infections in a widely disseminated rural South African epidemic. International Journal of Epidemiology. 2009 doi: 10.1093/ije/dyp148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanser F, Lesueur D, Solarsh G, Wilkinson D. HIV heterogeneity and proximity of homestead to roads in rural South Africa: an exploration using a geographical information system. Trop Med Int Health. 2000;5:40–46. doi: 10.1046/j.1365-3156.2000.00513.x. [DOI] [PubMed] [Google Scholar]
- Tawfik L, Watkins SC. Sex in Geneva, sex in Lilongwe, and sex in Balaka. Social Science & Medicine. 2007;64:1090–1101. doi: 10.1016/j.socscimed.2006.10.002. [DOI] [PubMed] [Google Scholar]
- UNAIDS. Malawi 2008 country progress report, viewed on February 10, 2009. 2007 < http://www.unaids.org/en/CountryResponses/Countries/malawi.asp>.
- UNAIDS. Rural HIV/AIDS, viewed on April 23, 2009. 2008 < http://www.unaids.org/en/CountryResponses/Countries/malawi.asp>.
- UNICEF. Country Page: Malawi, viewed on January 3, 2010. 2008 < http://www.unicef.org/infobycountry/malawi_statistics.html>.
- Watkins SC. Navigating the AIDS epidemic in rural Malawi. Population and Development Review. 2004;30:673. [Google Scholar]
- Wellings K, Collumbien M, Slaymaker E, Singh S, Hodges Z, Patel D, Bajos N. Sexual behaviour in context: a global perspective. Lancet. 2006;368:1706–1728. doi: 10.1016/S0140-6736(06)69479-8. [DOI] [PubMed] [Google Scholar]
- Whiteside A, De Waal A. ‘That’s resources you see!’: Political economy, ethics and the HIV/AIDS epidemic. New Political Economy. 2004;9:581–594. [Google Scholar]