Abstract
Study design: Two cases of intraoperative, iatrogenic cervical spine fractures in patients with ankylosing spondylitis are reported. Objective: To describe the uncommon complication of iatrogenic cervical spine fractures occurring during spine surgery in patients with ankylosing spondylitis. Summary of background data: To our knowledge, this is the first report on this rare complication. Methods: A 39-year-old patient (1) with ankylosing spondylitis was operated on for cervical stenosis due to C1/2 anterolisthesis. Fifteen hours postoperatively, he developed acute quadriplegia. MRI revealed a fracture/dislocation of C6 on C7 and compression of the spinal cord at this level. Revision was performed with decompression and instrumentation from the occiput to T3. A 55-year-old patient (2) with ankylosing spondylitis and thoracic hyperkyphosis underwent a correction procedure consisting of costotransversectomy, anterior cage implantation at T8/9, and posterior instrumentation from T4 to L1. Halo traction was temporarily applied for correction. At the end of the operation, with the patient still under anesthesia, increased mobility of the cervical spine was noticed. Emergent MRI revealed a fracture of the anterior structures of C6/7. Posterior instrumentation from C5 to T1 was then performed. Results: Quadriplegia persisted in patient 1 until his death secondary to further complications. Patient 2 was mobilized without any neurologic deficits. The fracture healed in good alignment. Conclusions: Iatrogenic fractures of the cervical spine during surgery in ankylosing spondylitis patients are a rare but potentially severe complication. Early diagnosis and therapy are necessary before dislocation, cord compression, and subsequent neurologic impairment occur.
Keywords: Ankylosing spondylitis, Iatrogenic fracture, Cervical spine fracture
Introduction
Ankylosing spondylitis is a chronic inflammatory disease leading to progressive synostosis of the spine. The process of ankylosis usually presents in the lumbar spine before progressing cephalad to the thoracic and finally, the cervical spine. Eventually, this process results in a rigid, ankylosed spine. The ankylosed spine has an increased tendency to fracture, due to rigidity, long lever arms, and decreased bone mineral content.
Several surgical procedures utilized in the treatment of ankylosing spondylitis require reduction manoeuvres. These manoeuvres may increase the risk of fracture and potentially catastrophic sequelae.
In this report, we present two cases of iatrogenic cervical spine fractures in ankylosing spondylitis patients following reduction manoeuvres during spinal surgery.
Case 1
A 39-year-old patient with longstanding ankylosing spondylitis was transferred to our emergency room by helicopter from an outside clinic. He was initially admitted for evaluation of increasing paresis of both arms and glove-like hypoesthesia of both hands. During his stay in the outside clinic, he had developed acute urinary bladder and anal sphincter dysfunction and paresis of both lower limbs (Fig. 1a–d).
Fig. 1.
a Case 1: A 39-year-old patient with ankylosing spondylitis and rotatory subluxation of C1–C2. Note high-grade stenosis at C1/2 and no stenosis in the lower cervical spine. CT scans at the level of C1/2 in the same patient preoperatively (b), and postoperatively after reduction and instrumentation (c). d MRI scans 15 h postoperatively: complete decompression at the craniocervical junction, but new dislocation and stenosis at C6
On examination in our clinic, he was noted to have a fixed tilt of the cervical spine with fixed rotation to the left; his chin rested on his chest. Active rotation was impossible. He complained of pain in his neck and arms in addition to the aforementioned neurological deficits. Speech, verbal articulation, and pharyngeal function were normal. Bilateral strength testing revealed: deltoids grade 2-3/5, biceps 3-4/5, triceps 2-3/5, wrist extension and flexion 2/5, iliopsoas muscle 2-3/5, knee extension 4/5, ankle extension, and flexion 3/5. Sensibility was lost caudal to C3. Deep tendon reflexes were increased on the left. Babinski sign was present on the left side.
Emergent CT-scan revealed anterior subluxation of C1 on C2 with rotation to the left; destruction of the lateral masses of C1 and C2; severe stenosis and cord compression at C1–C2; and atlanto-occipital ankylosis.
A CT-angiogram showed hypoplasia of the left vertebral artery and elongation of the right vertebral artery due to the vertebral luxation.
MRI had to be done with the patient in the right decubitus position due to the fixed tilt of his cervical spine. The MRI showed medullary edema at the level of C1.
The patient underwent posterior decompression at C1, reduction of C1 on C2, and instrumentation from the occiput to C5 bilateral. Pedicle screws were inserted in C2, C3, C4, and C5. An occipital plate was utilized. Decompression was completed via resection of the posterior arch of C1. Crutchfield tongs was applied to the skull. With traction and rotation of the tongs, a complete reduction of the rotatory subluxation at C1–C2 was achieved, with direct visualization of the spinal cord. Reduction was maintained with contoured rods from the occiput to C5.
Postoperatively, the patient demonstrated slightly improved neurologic deficits. Fifteen hours after the operation, however, the patient developed increasing quadriplegia afflicting especially both lower extremities. An emergent MRI revealed a hyperextension-type injury with fracture through C6/7. This injury resulted in a high-grade stenosis of the spinal canal by the C6 lamina with compression of the spinal cord and medullary edema from C4 to T1. Occlusion of the right vertebral artery at C1 resulted in an infarction of the cerebellum on the right side.
Immediate revision was performed with posterior decompression, reduction, and instrumentation from the occiput to T3. Following the surgery, the patient’s neurologic deficits were improved in both upper extremities. His strength was grade 4/5 throughout and he regained sensibility to C5. Hyper-reflexia of both arms and paraplegia of both legs persisted.
The following day, the patient experienced a sudden respiratory difficulty and extreme bradycardia, and CPR was necessary. MRI showed partial occlusion of the left vertebral artery with a circumscribed thrombus in the basilar artery and cerebellar infarction. Five days later, the patient developed cerebral hypoxia, compression of brainstem and tonsillar hernation. EEG 11 days after the revision documented cerebral death.
Case 2
A 55-year-old patient with ankylosing spondylitis presented to our clinic with pronounced thoracic hyperkyphosis. The patient found his posture detrimental to performing his activities of daily living. The patient was severely psychologically upset by his functional loss and cosmetic appearance. He reported a recent and significant increase in back pain (Fig. 2a–d).
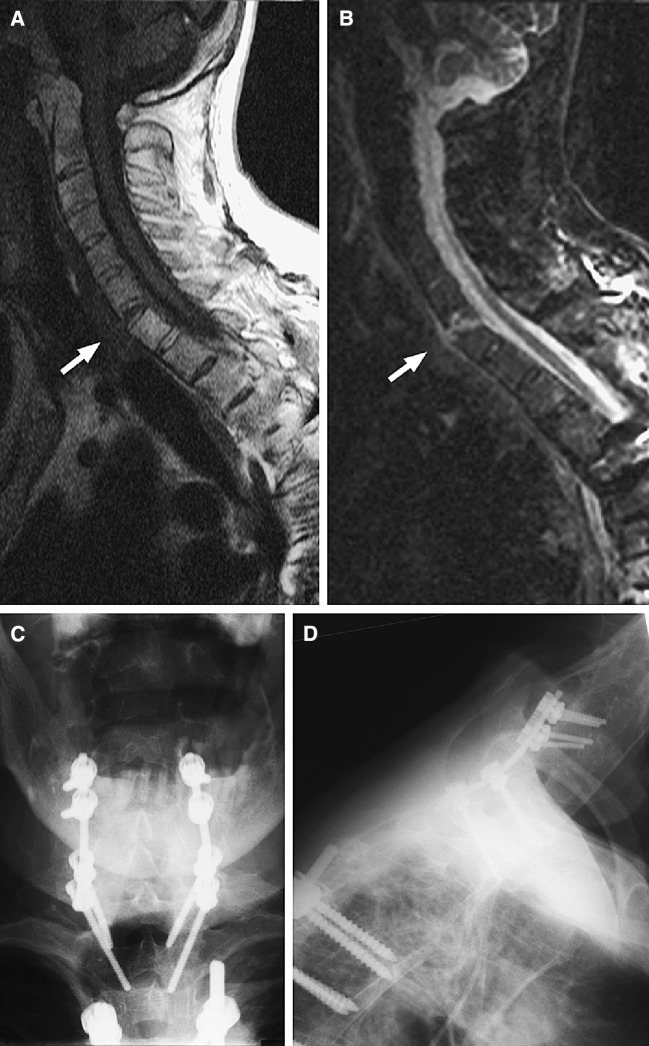
Fig. 2.
a and b Case 2: The postoperative MRI scans show a hyperextension injury C6/7 with disruption of the intervertebral disc, no major dislocation, and no stenosis of the spinal canal. c and d Same patient after posterior instrumentation C4 to T1
Upon evaluation, the patient was noted to have a stuttering gait, severe thoracic hyperkyphosis, and compensatory hyperlordosis of the cervical spine. He complained of pain in the area of T8/9 posteriorly. His spine was obviously ankylosed and stiff. He was only able to achieve an erect stance and horizontal gaze with his knees flexed. Neurologic examination revealed intact sensation, normal muscle strength, and normal reflexes.
Radiographs demonstrated ankylosis of the entire spine and sacroiliac joints with osteopenia. There was an Andersson lesion at T8/T9 with segmental kyphosis and sclerosis of the adjacent endplates [1]. The thoracic kyphosis between T2 and T12 measured 108° with a kyphotic angulation of 35° between T8 and T9. The C7 plumbline with extended knees fell 65 mm anterior to the posterior-superior edge of the S1 endplate.
We performed realignment-spondylodesis through bilateral costotransversectomies, a wedge osteotomy at T8/9, anterior Harms cage interposition, and posterior instrumentation from T4 to L1. During this procedure, correction was achieved via traction and extension of the head through a halo ring.
Immediately after the operation, while still in the operating room, we noted abnormal mobility of the cervical spine. The image intensifier was brought in, but we were unable to clearly visualize the lower cervical spine due to osteopenia and shoulder overlap. Consequently, an emergent MRI was performed under the same anesthesia. A pillow was used to raise the pelvis and lower the head. This allowed positioning of the cervical spine in the MRI. These studies revealed a hyperextension injury at C6/7 with rupture of the intervertebral disc. The gap in the disc space led to a segmental lordosis of 10°. There was a small hematoma within the epidural space, and a hematoma between the spinal processes T6 and T7.
The patient was brought back to the operating room without further delay. A posterior approach was undertaken in the region of the injury. A fracture of the spinal process T6 was found, the ankylosed joints were still intact. Stabilization with posterior instrumentation from C4 to T1 was performed.
The rest of the postoperative course was uneventful. Mobilization in a TLSO was initiated on the first postoperative day. The brace was worn for 12 weeks total. During the most recent follow-up, bony consolidation had occurred at the cervical and thoracic levels. The patient was neurologically and clinically asymptomatic and his posture was significantly improved.
Discussion
Patients with ankylosing spondylitis are at a higher risk of spinal fracture than the normal population [3, 4, 7–9, 11]. Even minor trauma may result in a spinal fracture. This is due to multiple factors. First, the incidence of osteoporosis or osteopenia is increased compared to the normal population [2, 5, 6, 9, 10]. Second, the spine is unusually rigid. In contrast to a normal flexible spine, the ankylosed spine is unable to dissipate trauma energy into its surrounding soft tissues. This energy must be absorbed in the bony structures of the spine. Third, long lever arms are present which create enormous focal bending forces.
Fracture in ankylosing spondylitis by minor trauma does not necessarily mean a complete fracture of the anterior and posterior structures of the spine with dislocation. In the second case presented here, there was a fracture in the anterior part of the spine, the region of the synostosed vertebral bodies. This fracture could not be visualized by plain radiographs due to osteopenia and shoulder overlap. The synostosed joints were still intact in the MRI scans as well as intraoperatively during revision surgery. Clinically, a slight elasticity was noticed. This incomplete fracture of the anterior structures of the spine still creates significant instability. Without adequate trauma the posterior structures may fracture as well and dislocation with neurologic compromise may ensue. We assume that the patient in the first case experienced a similar partial, but unrecognized, fracture. The weight of the patient’s head while supine was enough to cause a dislocation and spinal cord injury.
A similar case was described by Rinsky et al. [12]. A patient with ankylosing spondylitis had neck pain after a fall at home. Initially, there was no obvious dislocation or neurologic deficit. A second, minor trauma (chiropractic manipulation) was then sufficient to cause dislocation and tetraplegia.
These incomplete, undisplaced fractures in ankylosing spondylitis are a challenging diagnostic problem. Given the slightest suspicion of fracture, a thorough workup is obligatory. Plain radiographs usually do not easily demonstrate minute changes in the bony outline. In addition, assessment is made more difficult due to the overlying structures of the cervicothoracic junction overshadowing an already osteopenic spine.
The most efficient diagnostic tool is the MRI with sequences sensitive for bone marrow edema followed by CT. However, this is usually not available in the operating room and in case of severe thoracolumbar kyphosis, it may be difficult to place the patient in the MRI. In these cases, it may help to raise the pelvis or to place the patient on his side.
The increased propensity for fracture in ankylosing spondylitis must be considered during surgery on these patients. It would seem that patients with a high degree of osteoporosis or osteopenia are at high risk, however, these fractures may also occur in those with inconspicuous bone density. The cervicothoracic region of the spine seems to be most vulnerable. We therefore recommend that all patients with ankylosing spondylitis should be positioned in the operating room very carefully. Under no circumstances should the patient’s head be subjected to flexion or extension forces and consequently it should be supported at all times. All manipulations and reductions must be performed with utmost care. Reduction via long lever arms, especially via manipulation of the head, should be the exception. Should it be necessary, we strongly recommend a radiographic control of the cervical spine and the cervicothoracic junction after the reduction manoeuvre. Should there be any doubt, MRI is imperative.
Conclusions
Ankylosing spondylitis patients are at higher risk of spinal fractures due to long lever arms and poor bone quality. Surgeons have to consider this when positioning patients and especially during intraoperative reduction manoeuvres. Traction or corrective manoeuvres should be performed with utmost care. In cases of suspected fracture, an MRI scan is obligatory.
References
- 1.Andersson O. Röntgenbilder vid spondylarthritis ankylopoetica. Nord Med Tidskr. 1937;14:200. [Google Scholar]
- 2.Capaci K, Hepguler S, Argin M, Tas I. Bone mineral density in mild and advanced ankylosing spondylitis. Yonsei Med J. 2003;44(3):379–384. doi: 10.3349/ymj.2003.44.3.379. [DOI] [PubMed] [Google Scholar]
- 3.Cooper C, Carbone L, Michet CJ, Atkinson EJ, O‘Fallon WM, Melton LJ 3rd. Fracture risk in patients with ankylosing spondylitis: a population based study. J Rheumatol. 1994;21(10):1877–1882. [PubMed] [Google Scholar]
- 4.Donnelly S, Doyle DV, Denton A, Rolfe I, McCloskey EV, Spector TD. Bone mineral density and vertebral compression fracture rates in ankylosing spondylitis. Ann Rheum Dis. 1994;53(2):117–121. doi: 10.1136/ard.53.2.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dos Santos FP, Constantin A, Laroche M, Destombes F, Bernard J, Mazieres B, Cantagrel A. Whole body and regional bone mineral density in ankylosing spondylitis. J Rheumatol. 2001;28(3):547–549. [PubMed] [Google Scholar]
- 6.El Maghraoui A, Borderie D, Cherruau B, Edouard R, Dougados M, Roux C. Osteoporosis, body composition, and bone turnover in ankylosing spondylitis. J Rheumatol. 1999;26(10):2205–2209. [PubMed] [Google Scholar]
- 7.Finkelstein JA, Chapman JR, Mirza S. Occult vertebral fractures in ankylosing spondylitis. Spinal Cord. 1999;37(6):444–447. doi: 10.1038/sj.sc.3100837. [DOI] [PubMed] [Google Scholar]
- 8.Hitchon PW, From AM, Brenton MD, Glaser JA, Torner JC. Fractures of the thoracolumbar spine complicating ankylosing spondylitis. J Neurosurg. 2002;97(Suppl. 2):218–222. doi: 10.3171/spi.2002.97.2.0218. [DOI] [PubMed] [Google Scholar]
- 9.Mitra D, Elvins DM, Speden DJ, Collins AJ. The prevalence of vertebral fractures in mild ankylosing spondylitis and their relationship to bone mineral density. Rheumatology (Oxford) 2000;39(1):85–89. doi: 10.1093/rheumatology/39.1.85. [DOI] [PubMed] [Google Scholar]
- 10.Mullaji AB, Upadhyay SS, Ho EK. Bone mineral density in ankylosing spondylitis. DEXA comparison of control subjects with mild and advanced cases. J Bone Joint Surg Br. 1994;76(4):660–665. [PubMed] [Google Scholar]
- 11.Olerud C, Frost A, Bring J. Spinal fractures in patients with ankylosing spondylitis. Eur Spine J. 1996;5(1):51–55. doi: 10.1007/BF00307827. [DOI] [PubMed] [Google Scholar]
- 12.Rinsky LA, Reynolds GG, Jameson RM, Hamilton RD. A cervical spinal cord injury following chiropractic manipulation. Paraplegia. 1976;13(4):223–227. doi: 10.1038/sc.1976.35. [DOI] [PubMed] [Google Scholar]