Abstract
The authors conducted a study to determine at what stage after surgery the subsidence occurred, and to assess the relationships of radiographic fusion and the recurrence of symptoms with the development of subsidence. Ninety patients underwent a single-level anterior lumbar interbody fusion (ALIF) using paired stand-alone rectangular cages between November 2000 and June 2002. All patients had regular clinical or imaging follow-up for a minimum of 19 months (range 19–38 months, mean = 27 months). The ratio of male to female patients was 1:3.1. The patients’ ages at the time of ALIF ranged from 25 to 72 years, with a mean of 53 years. The preoperative and postoperative intervertebral disc heights were serially measured by plain radiographs. The location of cage subsidence into the vertebral body and times until the presence of subsidence were also assessed. The mean preoperative intervertebral disc height was 11.6±3.1 mm, which spread immediately after surgery to 16.9±2.0 mm. This increase was statistically significant (P=0.001). At the last follow-up visit, the mean intervertebral disc height had been reduced to 13.2±2.4 mm. Sixty-nine of 90 patients (76.7%) developed cage subsidence into the surrounding vertebral body. Subsidence was more often noted in the superior endplate above the cage with regard to the location of cage subsidence [superior endplate: 27 patients (39.1%), inferior endplate: 12 patients (17.3%), both: 30 patients (43.6%)]. The onset of subsidence varied from 0.25 to 8 months after surgery (median, 2.75 months). The 8-, 12-, and 16-week actuarial rates for developing cage subsidence were 38.9, 63.4, and 70.7%, respectively, when using the Kaplan–Meier method. There was no statistical correlation between the recurrence of symptoms (P=0.3952) and radiographic fusion (P=0.9518) with the log-rank test in development of subsidence. This study demonstrates that cage subsidence is an expected occurrence after ALIF using stand-alone rectangular cages. The 3- and 4-month actuarial rates for developing cage subsidence were 63.4 and 70.7%, respectively, and cage subsidence had no correlation with recurrence of symptoms and radiographic fusion in our study.
Keywords: Anterior lumbar interbody fusion (ALIF), Cage, Subsidence
Introduction
The anterior lumbar interbody fusion (ALIF) has evolved into an effective treatment option in patients with lumbar degenerative disorders since the introduction of various cages for ALIF. This procedure accomplishes multiple goals simultaneously [3, 6]. First, it avoids violation of the spinal canal and reduces the formation of epidural scar tissue. Second, it destabilizes the spine minimally compared with a similarly aggressive posterior approach, offering some degree of immediate stabilization of the motion segment and preserving spinal stability. Finally, ALIF allows a more efficient restoration of disc interspace height, decompresses the intervertebral foramen, and permits treatment of foraminal stenosis by distracting the affected degenerated segment and placing the interbody fusion devices. Recent advances in minimal invasive techniques have generated a great deal of interest in the ALIF procedure and have had spine surgeons consider it as being less invasive than the posterior fusion techniques [1, 6].
Subsidence is a term used to describe a decrease in the vertical height of the disc space prior to complete incorporation of the fusion mass. Some authors reported on the comparison of disc space heights after ALIF [5, 7, 10, 14, 15]. It was found that some reduction of disc space height, after initial distraction, occurred in many patients following ALIF using autologous iliac crest bone grafting. However, there are few published articles describing the fate of cages after ALIF using paired stand-alone rectangular cages. The authors embarked on a study to determine at what stage after surgery the subsidence occurred, to assess the relationships of radiographic fusion and the recurrence of symptoms with the development of subsidence.
Material and methods
Patient population
Ninety patients underwent a single-level ALIF using paired stand-alone rectangular cages in our hospital between November 2000 and June 2002. The ratio of male to female patients was 1:3.1. The patients’ ages at the time of ALIF ranged from 25 to 72 years with a mean age of 53 years. All patients had regular clinical or imaging follow-up for a minimum of 19 months (range: 19–38 months, mean = 27 months).
The preoperative diagnoses were degenerative disc disease with severe disc space narrowing in 73 patients, grade I degenerative spondylolisthesis in 14 patients, and recurrent disc herniation in three patients. The fused levels at which the cages were inserted were as follows: L4–5 (49 patient), L5–S1 (33 patients), and L3–4 (eight patients). The summary of patients’ demographic characteristics, preoperative diagnosis, and level of segments fused for the entire series is presented in Table 1.
Table 1.
Demographic characteristics, preoperative diagnosis, and level of segments fused
| Parameter | |
|---|---|
| Mean age at the time of ALIF | 53 years (25–72) |
| Gender ratio | 1:3.1 |
| Mean follow up duration | 27 months (19–38) |
| Diagnosis | |
| Degenerative disc disease with disc space narrowing | 73 |
| Degenerative spondylolisthesis(grade I) | 14 |
| Recurrent disc herniation | 3 |
| Involved level | |
| L4–L5 | 49 |
| L5–S1 | 33 |
| L3–L4 | 8 |
Surgical technique
We modified the mini-open laparotomy, which was originally reported by Onimus [11], with the use of a left-sided retroperitoneal approach, and employed it as a standard approach to the anterior lumbar spine. All the surgical procedures were performed by the same surgeon (K.H.S.), who had extensive experience with the technique used.
With the patient supine, a standard midline vertical 4-cm sized incision was made 1 cm below the umbilicus for L4/5, at the umbilicus for the L3/4, and halfway between the umbilicus and the symphysis pubis for the L5/S1 approach. In women, a cosmetic horizontal suprapubic incision was available for the L5/S1 approach.
As much of the nucleus as possible was removed so that the posterior annulus was exposed at the involved level. Intervertebral distraction using an interspace distracter plug facilitated resection of disc material and allowed cage insertion. Care should be taken to resect only the cartilaginous endplate with the careful preservation of the bony endplates to ensure a mechanically stable recipient site. The chamber of cages was packed with allograft bone chips (Regeneration Technology, Alachua, Fla., USA). Three kinds of cages were used in our series [Lumbar I/F cage (DePuy Acromed, Raynham, Mass., USA), Fidji cage (Spine Next, Bordeaux, France), Titanium OIC cage (Stryker Spine, Cestas, France)]. After surgery, patients were usually allowed out of bed by day 3 and instructed to wear a custom-made rigid lumbar orthosis during the day for 2 months.
Radiographic analysis
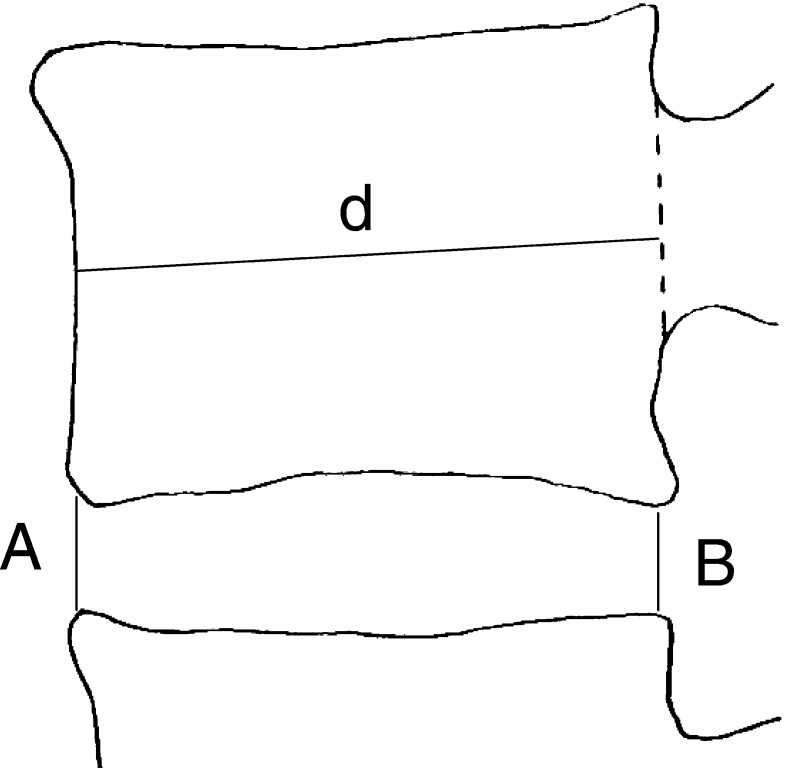
Radiologic evaluation was performed using standing AP, lateral plain radiograph, and dynamic flexion-extension films in lateral decubitus to determine the fusion. Data obtained in all patients were entered into a database on admission and this was updated whenever the patients returned for follow-up. Radiographic results and clinical details were retrospectively reviewed. The intervertebral disc height was measured using the method employed in the study by Cheung et al. [5] (Fig. 1). The intervertebral disc height was expressed as an average (disc height index) of the sum of the measurements at the anterior and posterior regions of the disc. The disc space height was normalized with the anteroposterior diameter of the upper vertebral body to correct for the magnification differences of the radiographs. The radiologic assessment was graded as I, II, III or IV according to the fusion criteria proposed by Bridwell et al. [4]: grade I, fused with remodeling and trabeculae; grade II, graft intact, not fully remodeled and incorporated though but with no lucencies above or below; grade III, graft intact but a definite lucency at the top or bottom of the graft; grade IV, definitely not fused with resorption of bone graft and with collapse. Grades I and II were considered as solid fusion. The same independent investigator (Y.W.C.) analyzed the radiographic results, including measurement of disc height index and fusion grading.
Fig. 1.
The intervertebral disc height was expressed as an average (disc height index—A+B/2) of sum of measurements at anterior and posterior regions of the disc and the disc space height was normalized with the anteroposterior diameter (d) of the upper vertebral body to correct for the magnification differences of the radiographs
Statistical analysis
All the data were analyzed using a paired sample t-test. Investigator’s measurement error was calculated to be less than 2 mm (P<0.05). Interval from date of surgery to date of presence of cage subsidence was assessed and actuarial rate for developing cage subsidence was calculated by the Kaplan–Meier method. Comparisons of Kaplan–Meier curves between two groups (fusion group and non-fusion group, recurrence of symptoms group and non-recurrence of symptoms group) were performed using the log-rank test. All the statistical analyses were performed using SPSS software (SPSS, Version 10, SPSS, Chicago, Ill., USA).
Results
Radiologic measurements (disc height index loss)
The mean preoperative intervertebral disc height was 11.6±3.1 mm, which spread immediately after surgery to 16.9±2.0 mm. This increase was statistically significant (P=0.001). At the last follow-up visit, the mean intervertebral disc height had been reduced to 13.2±2.4 mm. Despite the reduction of intervertebral disc height after initial distraction, intervertebral disc space at the last follow-up was significantly higher than the preoperative one and there was statistical difference between preoperative intervertebral disc height and that at the last follow-up visit (P<0.05). Cage subsidence was defined as a measured decrease of disc space height by more than 2 mm on follow-up radiographs because investigator’s measurement error was calculated to be less than 2 mm. On this basis, 69 of 90 patients (76.7%) developed cage subsidence into the surrounding vertebral body.
Location of cage subsidence
Subsidence was more often noted in the superior endplate above the cage with regard to the location of cage subsidence [superior endplate: 27 patients (39.1%), inferior endplate: 12 patients (17.3%), both: 30 patients (43.6%)] (Fig. 2, 3).(Fig. 3)
Fig. 2.
A series of plain radiographs (59-year-old female) obtained (a) preoperatively, postsurgery (b) 1 month, and (c) 26 months, demonstrating a well-maintained disc space without any subsidence
Fig. 3a–d.
A 47-year-old Korean female underwent a L4-5 ALIF. A plain radiograph (b) obtained 2 weeks after operation demonstrated that cage started to subside to the superior endplate, although disc space was markedly distracted compared with the preoperative lateral radiograph (a). Subsidence was noted mainly in the superior endplate above the cage on the lateral X-ray at 5-week (c) and 9-week (d) follow-up visit
Actuarial rate for developing cage subsidence
The onset of subsidence varied from 0.25 to 8 months after surgery; the median time for cage subsidence was 2.75 months. The 8-, 12-, and 16-week actuarial rates for developing cage subsidence were 38.9, 63.4, and 70.7%, respectively, when using the Kaplan–Meier method (Fig. 4).
Fig. 4.
Graph showing a Kaplan–Meier survival curve for all 90 patients. The y-axis of this graph actually represents subsidence-free survival. The onset of subsidence varied from 0.25 to 8 months after surgery (median, 2.75 months). The 3- and 4-month actuarial rates for developing cage subsidence were 63.4 and 70.7%, respectively
On the basis of the criteria for determining fusion, the investigator assigned 59 grade I fusions (65.6%), 19 grade II fusions (21.1%), three grade III fusions (3.3%), and nine grade IV fusions (10.0%). Therefore, fusion was found to be solid in 78 of 90 patients (86.7%). During the follow-up period, recurrence of symptoms developed in 19 of 90 patients (21.1%). There was no statistical correlation between recurrence of symptoms (P=0.3952) and radiographic fusion (P=0.9518) with the log-rank test in development of subsidence (Fig. 5).
Fig. 5.
Graph demonstrating Kaplan–Meier survival curves by (a) status of fusion and (b) recurrence of symptoms. There was no statistical correlation between recurrence of symptoms (P=0.3952) and radiographic fusion (P=0.9518) with the log-rank test in development of subsidence
Discussion
Over the last decade, there have been growing interests in the use of cages for ALIF. In degenerative disc disease, the major source of the pain is thought to result from the degenerative disc itself and/or the facet joints and ALIF is one of the alternatives for the treatment of degenerative disc disease of the lumbar spine [2, 9]. Many spine centers have increasingly performed ALIF using cages due to the claimed advantages, such as avoidance of donor site morbidity, no difficulty of cutting precise bony channels, and no risk of postoperative bone graft collapse [3, 17]. However, there have been few attempts to understand the fate of cages after ALIF using paired stand-alone rectangular cages.
In a previous study, some authors reported that disc height loss after ALIF with bone graft occurred. Dennis et al. [7] investigated the disc height after ALIF using autogenous, cadaver, or mixed iliac crest grafts and found that 100% of the levels underwent a loss of disc height and 46% narrower than their preoperative heights. More recently, Cheung et al. [5] assessed 67 patients who underwent ALIF at L4–L5 with autologous iliac crest graft. They found that the mean disc space height at the last follow-up (12.6±2.3 mm) was about the same as the mean preoperative disc space height (12.1±2.9 mm), and that there was no significant difference between preoperative disc space height and that at the last follow-up assessment. In the current study, despite the reduction of disc space height after initial distraction, intervertebral disc space at the last follow-up (13.2±2.4 mm) was significantly higher than the preoperative one (11.6±3.1 mm) and there was a statistical difference between preoperative disc space height and that at the last follow-up visit (P<0.05). In this context the data obtained in our series showed that cage seemed to be superior to bone graft in terms of maintaining intervertebral disc height.
The density and thickness of the vertebral endplate have been shown to increase toward the vertebral periphery [13]. Grant et al. [8] conducted a biomechanical investigation in a human cadaveric model to determine whether there are regional differences in endplate strength, and whether any differences identified are affected by endplate (superior versus inferior). They found that the lumbar endplate structural property maps shared several common features: the posterior is stronger than the anterior; the periphery is stronger than the center, the strongest points are the posterolateral area, just in front of the pedicles, and the superior and inferior lumbar endplates differ in that the inferior endplate is about 40% stronger than the superior endplate. In our series, subsidence was more often noted in the superior endplate (superior endplate: 39.1% vs inferior endplate: 17.3%). This result is consistent with the biomechanical study of Grant et al. [8] in that the superior endplate is much weaker than the inferior endplate.
As to what stage after surgery cage subsidence occurred, our study found that the median time for cage subsidence was 2.75 months, and that the onset of subsidence varied from 0.25 to 8 months after surgery. The 3- and 4-month actuarial rates for developing cage subsidence were 63.4 and 70.7%, respectively, in our study. Kumar et al. [10] reported that subsidence was found to occur mainly within the first 15 days after ALIF using femoral strut allograft. Cheung et al. [5] found that the disc height reduction occurred mainly within the first 3 months after ALIF with autologous iliac crest graft. These findings in the literature differ quite a bit in their results from that achieved in our study in that cage subsidence occurred some time later than bone graft.
The etiology that influences the tendency to subsidence of intervertebral cages is not fully understood. Clearly, the adequate preparation of the endplates is a key issue to prevent subsidence. Oxland et al. [12] recently conducted a biomechanical study to determine the effect of endplate removal on the structural properties. They found that removal of the vertebral endplate significantly reduced the local strength and stiffness magnitudes in the lower lumbar vertebral bodies (L3–L5), leading to an increased risk of implant subsidence. Therefore, we believe care should be taken to remove only the cartilaginous endplates by a meticulous technique to carefully preserve the bony endplate, to ensure a mechanically stable recipient site, and to reduce the potential for cage subsidence during the preparation. Another significant issue is the shape of the cage. Steffen et al. [16] reported on the effect of implant design on the compressive strength of interbody constructs in a human cadaveric study. They tested two different cage designs. The first had a solid endplate face providing 100% surface contact and the second had a large central opening with a peripheral rim. They noted that a cage with only peripheral support resting on the apophyseal ring offered axial mechanical strength similar to that of a cage with a solid face providing entire surface contact, and that might be beneficial in terms of fusion outcome. The advantage of this cage concept is that graft material placed inside the cage can be in close contact on a larger and noninterrupted surface with the host bone. Therefore, we think such a cage with a large central opening and a peripheral rim resting peripherally on the endplate may better resist subsiding into the vertebral body than rectangular cages.
With regard to the relationship of radiographic fusion and recurrence of symptoms with the development of subsidence, we noted that subsidence had no correlation with recurrence of symptoms and radiographic fusion. We think subsidence is the incorporation process of the cage to both endplates. The endplate tends to be curved and often concave; thus, in many cases only the periphery of the cage is initially in contact with the endplates. When loaded, it punches through the endplate and subsides to some degree before it achieves better contact with the bone, leading to the reduction of disc space height.
Finally, we can face the question: does cage subsidence really matter clinically? As shown in our study, the operated disc spaces demonstrated a reduction after initial distraction. This finding is in direct contradiction with the purpose of intervertebral cages, which are designed to keep the height of the disc space constant following surgery. However, we believe that cages went into bones. The loss of disc space height did not preclude an excellent or good clinical outcome.
We acknowledge that our study design has a limit in that retrospective, non-randomized series can introduce selection bias in terms of the patients who are available for study with adequate follow-up. Therefore, the authors think further prospective, randomized controlled trials need to be performed to determine more adequately the unequivocal factors responsible for the development of cage subsidence.
Conclusions
We conducted a retrospective analysis to determine at what stage after surgery the subsidence occurred, to assess the relationships of radiographic fusion and recurrence of symptoms with the development of subsidence. From the current study, it can be concluded that cage subsidence is an expected occurrence after ALIF using paired stand-alone rectangular cages. The 3- and 4-month actuarial rates for developing cage subsidence were 63.4 and 70.7%, respectively, and cage subsidence had no correlation with recurrence of symptoms and radiographic fusion in our study.
References
- 1.Bak KH, Kim YS, Kim JM, Kim CH, Koh Y, Oh SH, Oh SJ, Kim KM, Kim NK. Minimally invasive anterior lumbar interbody fusion (in Korean) J Korean Neurosurg Soc. 1998;27:792–799. [Google Scholar]
- 2.Blumenthal SL, Baker J, Dossett A, Selby DK. The role of anterior lumbar fusion for internal disc disruption. Spine. 1988;13:566–569. doi: 10.1097/00007632-198805000-00023. [DOI] [PubMed] [Google Scholar]
- 3.Brantigan JW, Steffee AD. A carbon-fiber implant to aid interbody lumbar fusion: two-year clinical results in the first 26 patients. Spine. 1993;182:106–2117. doi: 10.1097/00007632-199310001-00030. [DOI] [PubMed] [Google Scholar]
- 4.Bridwell KH, Lenke LG, McEnery KW, Baldus C, Blanke K. Anterior fresh frozen structural allografts in the thoracic and lumbar spine. Spine. 1995;20:1410–1418. [PubMed] [Google Scholar]
- 5.Cheung KM, Zhang YG, Lu DS, Luk KD, Leong JC. Reduction of disc space distraction after anterior lumbar interbody fusion with autologous iliac crest graft. Spine. 2003;28:1385–1389. doi: 10.1097/01.BRS.0000067093.47584.CA. [DOI] [PubMed] [Google Scholar]
- 6.Choi JY, Jeong HT, Hyun YI, Sung YS, Lee YS, Sung KH. A retrospective study of the fusion rate and clinical outcome after mini-open ALIF using paired stand-alone rectangular cages (in English) J Korean Neurosurg Soc. 2004;36:28–33. [Google Scholar]
- 7.Dennis S, Watkins R, Landaker S, Dillin W, Springer D. Comparison of disc space heights after anterior lumbar interbody fusion. Spine. 1989;14:876–878. doi: 10.1097/00007632-198908000-00019. [DOI] [PubMed] [Google Scholar]
- 8.Grant JP, Oxland TR, Dvorak MF. Mapping the structural properties of the lumbosacral vertebral endplates. Spine. 2001;26:889–896. doi: 10.1097/00007632-200104150-00012. [DOI] [PubMed] [Google Scholar]
- 9.Inoue S, Watanabe T, Hirose A, Tanaka T, Matsui N, Saegusa O, Sho E. Anterior discectomy and interbody fusion for lumbar disc herniation: a review of 350 cases. Clin Orthop. 1984;183:22–31. [PubMed] [Google Scholar]
- 10.Kumar A, Kozak JA, Doherty BJ, Dickson JH. Interspace distraction and graft subsidence after anterior lumbar fusion with femoral strut allograft. Spine. 1993;18:2393–2400. doi: 10.1097/00007632-199312000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Onimus M, Papin P, Gangloff S. Extraperitoneal approach to the lumbar spine with video assistance. Spine. 1996;21:2491–2494. doi: 10.1097/00007632-199611010-00016. [DOI] [PubMed] [Google Scholar]
- 12.Oxland TR, Grant JP, Dvorak MF, Fisher CG. Effects of endplate removal on the structural properties of the lower lumbar vertebral bodies. Spine. 2003;28:771–777. [PubMed] [Google Scholar]
- 13.Roberts S, McCall IW, Menage J, Haddaway MJ, Eisenstein SM. Does the thickness of the vertebral subchondral bone reflect the composition of the intervertebral disc. Eur Spine J. 1997;6:385–389. doi: 10.1007/BF01834064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sandhu HS, Turner S, Kabo JM, Kanim LEA, Liu D, Nourparvar A, Delamarter RB, Dawson EG. Distractive properties of a threaded interbody fusion device: an in vivo model. Spine. 1996;21:1201–1210. doi: 10.1097/00007632-199605150-00013. [DOI] [PubMed] [Google Scholar]
- 15.Soini J. Lumbar disc space heights after external fixation and anterior interbody fusion: a prospective 2-year follow-up of clinical and radiographic results. J Spinal Disord. 1994;7:487–494. [PubMed] [Google Scholar]
- 16.Steffen T, Tsantrizos A, Aebi M. Effect of implant design and endplate preparation on the compressive strength of interbody fusion constructs. Spine. 2000;25:1077–1084. doi: 10.1097/00007632-200005010-00007. [DOI] [PubMed] [Google Scholar]
- 17.Weiner BK, Fraser RD. Spine update lumbar interbody cages. Spine. 1998;23:634–640. doi: 10.1097/00007632-199803010-00020. [DOI] [PubMed] [Google Scholar]