Abstract
Endoscopic minimally invasive techniques have become an established method of fracture stabilisation in the spine. In view of this fact, anterior stabilisation strategies must be reconsidered, as monosegmental A 3.1 compression fractures are increasingly being stabilised endoscopically from the anterior aspect using minimally invasive techniques. This study investigated the biomechanical necessity of anterior two-point or four-point stabilisation in the instrumentation of mono- and bisegmental fractures. In three biomechanical in vitro studies, burst fracture stabilisation was simulated, and anterior short fixation devices were tested under load with pure moments up to 3.75 Nm to evaluate the biomechanical stabilising characteristics of different kinds of instrumentations in flexion/extension, lateral bending, and axial rotation. Only anterior four-point stabilisation resulted in sufficient primary stability both in mono- and bisegmental instrumentation and therefore represents the standard procedure in open as well as in minimally invasive spinal surgery.
Keywords: Biomechanics, Thoracolumbar burst fractures, Spinal stabilisation, Minimally invasive spinal surgery
Introduction
Minimally invasive techniques have become established clinically in spinal traumatology thanks to sophisticated new instruments that can be used both open and endoscopically because of modified, specially adapted implantation methods [3–5, 7, 10, 17, 20–25].
Based on these new minimally invasive techniques, a trend is developing to stabilise monosegmental A 3.1/3.2 fractures anteriorly only [2]. Bisegmental stabilisation within the thorax often necessitates splitting the diaphragm to get to the caudally adjacent vertebrae [3–5, 10, 23]. However, it is very difficult intraoperatively to get to the L2 level from a thoracic approach and also to place the instrumentation. In addition, so far there have been no biomechanical investigations on what kind of mono- or bisegmental stabilisation is required and whether two-point stabilisation with a stable angle (one screw of stable angulation in each adjacent vertebral body with an overbridging implant) or four-point stabilisation (two screws of stable angulation in each adjacent vertebral body with an overbridging implant) is necessary in order to achieve adequate primary stability while at the same time avoiding overtreatment. This is particularly of interest for endoscopic procedures in which minimized implants are desirable that will still ensure sufficient primary stability, especially when the treatment is only anterior. Considering minimally invasive stabilisation techniques, a large quantity of implant parts and large implant components are a hindrance. It is also not easy to insert two screws that must be placed parallel within a vertebral body from the left side endoscopically because of the “flight angle.” An additional port is often necessary in this regard for implanting the anteriorly situated screw, so biomechanically sufficient two-point stabilisation is actually desirable. The aim of this study was to clarify biomechanically whether only anterior four-point stabilisation results in sufficient anterior primary stability both in mono- and bisegmental instrumentation.
Materials and methods
Because the framework conditions for spinal implant testing are complex to simulate and because the in vivo loads on the spine are still insufficiently known, the in vitro situation according to current knowledge has to be simulated as precisely and comparably as possible [29]. The Association for Spinal Surgery has therefore drawn up recommendations for standardised implant testing [30]. All of the following biomechanical investigations were carried out in our spine tester, which meets these requirements [28].
The biomechanical in vitro investigations were each conducted on six T10–L2 human spinal specimens. The average specimen age was determined in each case. Before testing, the specimens were packed three times in freezer film and deep frozen at −28°C. The bone density was measured using quantitative computed tomography (CT; XCT-9600A pQCT, Stratec, Birkenfeld, Germany) in a horizontal line in each vertebral body. The CT was calibrated beforehand using a hydroxyapatite phantom. Before testing, the specimens were thawed to room temperature. The soft tissues and muscles were removed, carefully preserving all discoligamentous structures. During the entire test preparations and testing, the specimens were kept moist with 0.9% NaCl solution. The test conditions at a normal room temperature of 20°C and an average humidity of 60% were recorded continuously during the tests with a hygrometer in order to monitor and minimize the effects of soft-tissue degeneration on the specimens. For fixing in the spine tester, T10 and L2 were cast in Technovit blocks (Technovit 3040, Heraeus Kulzer, Wehrheim/Ts, Germany) [28]. To achieve a better purchase of the vertebrae in this material, short screws were inserted into the caudal and cranial bone structures that were to be cast. The lower resin block was then fixed firmly in the spinal loading simulator and the upper one in a cardan joint (Fig. 1). Stepper motors were integrated into this cardan joint, which transmits pure moments of ±3.75 Nm for flexion/extension, left and right lateral bending, and axial left and right rotation to the specimens. The remaining other five degrees of freedom were unrestricted in order to allow free mobility of the specimens. The specimens were first tested in the intact state. After that, the desired defect in the region of the 12th thoracic vertebra was produced and stabilised appropriately. The following comparisons were made in the three series of tests (Fig. 2):
Fig. 1.
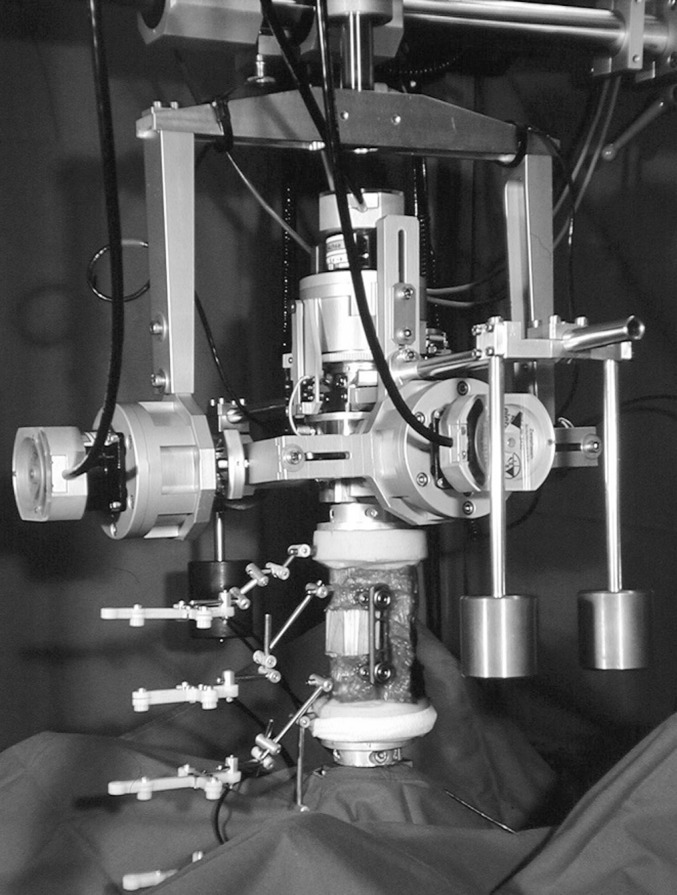
Spine tester
Fig. 2.
Test sequence
Two different anterior defects were investigated—on the one hand, monosegmental stabilisation to simulate the treatment of an A 3.1 fracture, and on the other hand, bisegmental stabilisation as a biomechanical in vitro simulation of the treatment of an A 3.3 fracture. In the first case, only the T11/T12 intervertebral disc was removed; a bone graft site was created in the adjacent bone structures of T11 and T12, and a wood block of appropriate size simulating the tricortical bone graft was implanted using press-fit technique. The anterior longitudinal ligament was preserved. The corresponding stabilisation took place on the left. Bisegmental stabilisation was carried out by removing discs T11/T12 and T12/L1 and removing the bony anterior parts of the vertebral body of T12 and the anterior longitudinal ligament. The resulting defect was replaced with a wood block simulating the tricortical bone graft using press-fit technique and was also stabilised by bridging on the left side.
The first test series was carried out on six human thoracic spinal segments. The specimen age was 83±7 years, and the bone density was 152±30 mg/cm3. The corresponding stabilisation was performed using the HMA system with plates (Hollow Modular Anchorage System, Aesculap, Tuttlingen, Germany). The screw length was 35 mm, and the screw diameter was 10 mm. The plate length varied between 80 and 100 mm. The monosegmental defect was tested first, and then the bisegmental defect. The cranially anchored HMA screw could be left while the plate length was adjusted by loosening the plate-screw connecting element accordingly, and the hold of this screw could then be checked by retightening it.
In the second series of tests, anterior two-point stabilisation with stable angulation was compared with four-point stabilisation. The specimen age of the six human vertebral segments used was 68±4 years, and the bone density was 219±12 mg/cm3. The standardised bisegmental defect described above was stabilised either with the anterior component of the US system (Universal Stabilization System, Stratec, Oberdorf, Switzerland) as two-point stabilisation, or with the Ventrofix (Stratec, Oberdorf, Switzerland) as four-point stabilisation. The specimens stabilised with the Ventrofix were tested after the testing of the two-point stabilisation. The posterior screw is identical and compatible with both systems and could therefore be used again for implantation of the Ventrofix. The screw length of the posterior screws was 40 mm each. The anterior screw of the Ventrofix had a length of 35 mm, with an identical diameter of 7 mm. The rod length was 90 mm.
In the third series of tests, monosegmental reconstruction was compared with bisegmental reconstruction with angle-stable four-point stabilisation alone. The specimen age was 77±18 years, and the bone density was 145±40 mg/cm3. The MACS TL Twin Screw System (Aesculap, Tuttlingen, Germany), which has been fully adapted to the endoscopic technique, was used for instrumentation. The employed screw length of the posterior polyaxial MACS TL screw was 40 mm, and that of the anterior one was 35 mm. The plate length varied between 80 and 100 mm.
The instrumentation of the implants was carried out according to the manufacturers’ instructions. The implant position was checked and documented with anteroposterior and lateral radiographs. The entire test sequence was conducted in accordance with the recommendations on standardised implant testing of the Association for Spinal Surgery [30]. Three test cycles each with pure moments of ±3.75 Nm in flexion/extension, left/right lateral bending, and left/right rotation with a constant rate of 1.9°/s without axial preload were applied. The resulting three-dimensional movements between all segments and the stabilised region were measured with an ultrasonic movement analysis system (measurement accuracy 0.1°) (Cmstrao 1.0, Zebris, Isny, Germany). The total range of motion (ROM) with maximum applied load and the neutral zone (NZ) as a measure of flexibility without load were analysed [14, 15]. The third cycle was used for analysis in order to eliminate the viscoelastic effects of the first two cycles. The Friedman test and the Wilcoxon signed rank test were used for statistical analysis, where the P-values obtained in this study should indicate tendencies and emphasise the descriptive statistics and not reflect statistically significant differences, as many parameters were measured under different conditions. As is the practice in other similar studies, correction of the P-values with a Bonferroni–Holm test was omitted, which would have led to multiple comparisons to P-values >0.05 and so to a considerable loss of information [18–21].
Results
Mono- versus bisegmental stabilisation
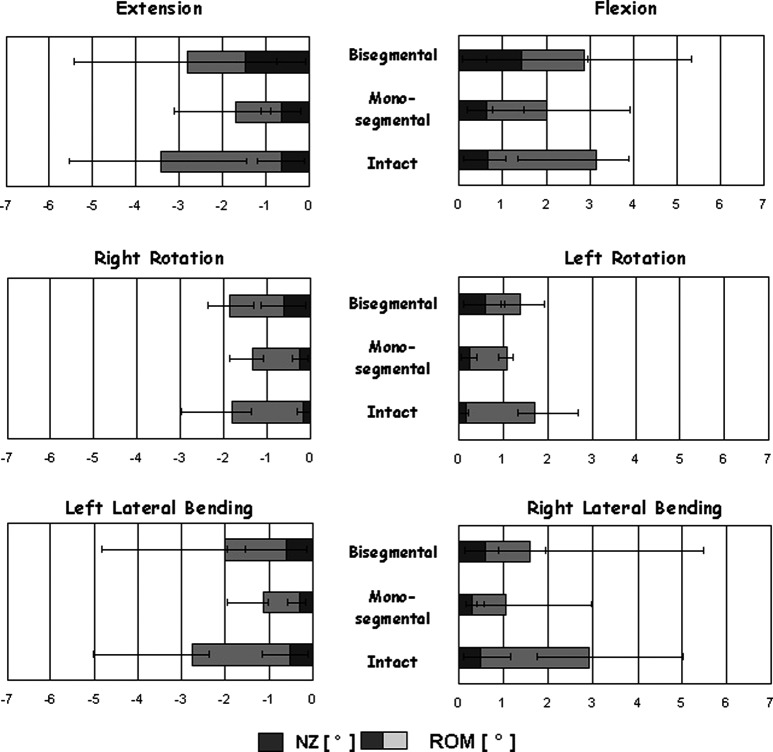
With monosegmental stabilisation using the HMA System, the total ROM in flexion/extension was reduced from ROMflexion intact 3.2° to 2.0° (NZflexion from 0.7° to 0.7°) and from ROMextension intact 3.4° to 1.7° (NZextensionfrom 0.7° to 0.7°). With bisegmental instrumentation, the ROMflexion was 2.9° (NZflexion 1.5°), and the ROMextension was 2.8° (NZextension 1.5°) (Fig. 3).
Fig. 3.
Median and ROM (degree) and NZ (degree) of the mono- or bisegmental T11–T12/L1 segment stabilised with the HMA System (two-point stabilisation) in flexion/extension, rotation, and lateral bending
With monosegmental stabilisation using the HMA system, the total ROM in axial rotation was reduced from ROMleft rotation intact 1.7° to 1.1° (NZleft rotation from 0.2° to 0.2°) and from ROMright rotation intact 1.8° to 1.3° (NZright rotation from 0.2° to 0.2°). With bisegmental instrumentation, the ROMleft rotation was 1.4° (NZleft rotation 0.6°), and the ROMright rotation was 1.9° (NZright rotation 0.6°) (Fig. 3).
With monosegmental stabilisation using the HMA System, the total ROM in lateral bending was reduced from ROMright lateral bending intact 2.9° to 1.1° (NZright lateral bending from 0.5° to 0.3°) and from ROMleft lateral bending intact 2.8° to 1.1° (NZleft lateral bending from 0.5 ° to 0.3°). With bisegmental instrumentation, the ROMright lateral bending was 1.6° (NZright lateral bending 0.6°) and the ROMleft lateral bending was 2.0° (NZleft lateral bending 0.6°) (Fig. 3). The P-values obtained with the Friedman and Wilcoxon tests are listed in Table 1.
Table 1.
Resulting P-values
| Two-point stabilisation (P-values) | Flexion ROM+ | Extension ROM− | Lateral ROM+ | Bending ROM− | Axial ROM+ | Rotation ROM− |
|---|---|---|---|---|---|---|
| Friedman test | 0.25 | 0.07 | 0.01 | 0.01 | 0.04 | 0.04 |
| Wilcoxon test Mono- versus bisegmental |
0.14 | 0.08 | 0.03 | 0.05 | 0.27 | 0.07 |
Two-point versus four-point stabilisation
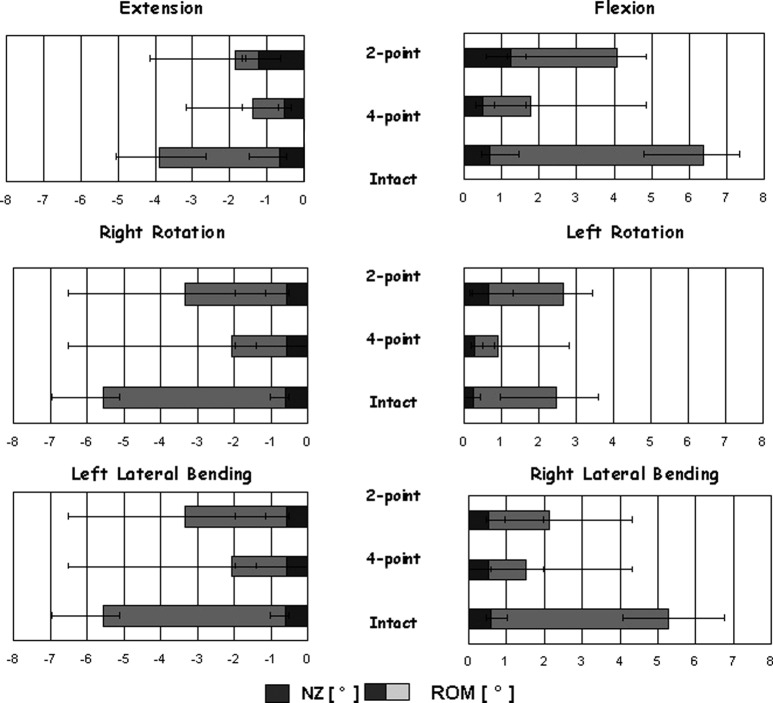
With four-point stabilisation, the total ROM in flexion/extension was reduced from ROMflexion intact 6.4° to 1.8° (NZflexion from 0.7° to 0.5°) and from ROMextension intact 3.9° to 1.4° (NZextension from 0.7° to 0.5°). With two-point instrumentation, the ROMflexion was 4.1° (NZflexion 1.2°), and the ROMextension was 1.9° (NZextension 1.2°) (Fig. 4).
Fig. 4.
Median and ROM (degree) and NZ (degree) of the bisegmental T11–T12/L1 segment stabilised with the US system (two-point stabilisation) or Ventrofix (four-point stabilisation) in flexion/extension, rotation, and lateral bending
With stabilisation using four-point stabilisation, the total ROM in axial rotation was reduced from ROMleft rotation intact 2.5° to 0.9° (NZleft rotation from 0.3° to 0.3°) and from ROMright rotation intact 3.1° to 1.3° (NZright rotation from 0.3° to 0.3°). With two-point instrumentation, the ROMleft rotation was 2.7° (NZleft rotation 0.7°), and the ROMright rotation was 2.7° (NZright rotation 0.7°) (Fig. 4).
With stabilisation using four-point stabilisation, the total ROM in lateral bending was reduced from ROMright lateral bending intact 5.3° to 1.5° (NZright lateral bending from 0.6° to 0.5°) and from ROMleft lateral bending intact 5.5° to 2.1° (NZleft lateral bending from 0.6 ° to 0.5°). With two-point instrumentation, the ROMright lateral bending was 2.1° (NZright lateral bending 0.6°), and the ROMleft lateral bending was 3.3° (NZleft lateral bending 0.6°) (Fig. 4). The P-values obtained with the Friedman and Wilcoxon tests are listed in Table 2.
Table 2.
Resulting P-values
| P-values | Flexion ROM+ | Extension ROM− | Lateral ROM+ | Bending ROM− | Axial ROM+ | Rotation ROM− |
|---|---|---|---|---|---|---|
| Friedman test | 0.25 | 0.05 | 0.10 | 0.50 | 0.01 | 0.01 |
| Wilcoxon test Two-point versus four-point |
0.14 | 0.06 | 0.03 | 0.05 | 0.46 | 0.06 |
Mono- versus bisegmental stabilisation with four-point stabilisation
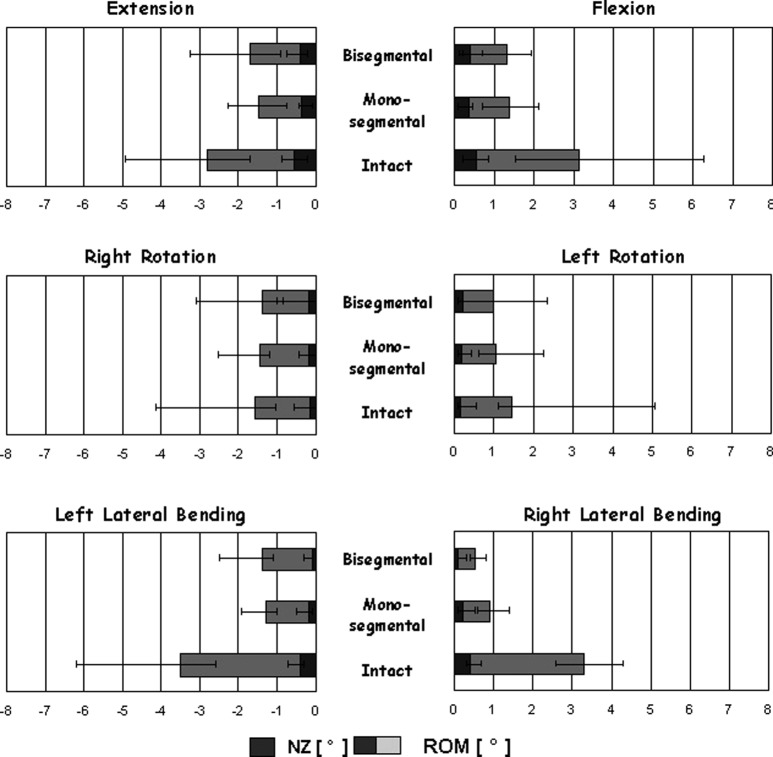
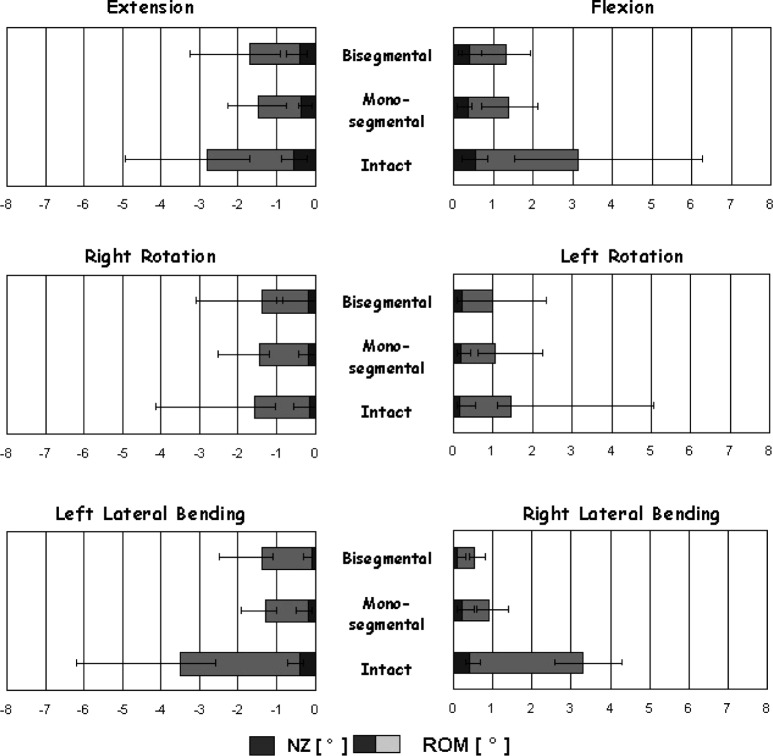
With monosegmental stabilisation using the MACS TL Twin Screw System, the total ROM in flexion/extension was reduced from ROMflexion intact 3.1° to 1.4° (NZflexion from 0.6° to 0.4°) and from ROMextension intact 2.8° to 1.5° (NZextension from 0.6 ° to 0.4°). With bisegmental instrumentation, the ROMflexion was 1.3° (NZflexion 0.4°), and the ROMextension was 1.7° (NZextension 0.4°) (Fig. 5).
Fig. 5.
Median and ROM (degree) and NZ (degree) of the mono- or bisegmental T11–T12/L1 segment stabilised with the MACS TL System (four-point stabilisation) in flexion/extension, rotation, and lateral bending
With monosegmental stabilisation using the MACS TL Twin Screw System, the total ROM in axial rotation was reduced from ROMleft rotation intact 1.4° to 1.0° (NZleft rotation from 0.2° to 0.2°) and from ROMright rotation intact 1.6° to 1.5° (NZright rotationfrom 0.2° to 0.2°). With bisegmental instrumentation, the ROMleft rotation was 1.0° (NZleft rotation 0.4°), and the ROMright rotation was 1.4° (NZright rotation 0.2°) (Fig. 5).
With monosegmental stabilisation using the MACS TL Twin Screw System, the total ROM in bending was reduced from ROMright lateral bending intact 3.3° to 0.9° (NZright lateral bending from 0.4° to 0.2°) and from ROMleft lateral bending intact 3.5° to 1.3° (NZleft lateral bending from 0.4 ° to 0.2°). With bisegmental instrumentation, the ROMright lateral bending was 0.5° (NZright lateral bending 0.1°), and the ROMleft lateral bending was 1.4° (NZleft lateral bending 0.1°) (Fig. 5). The P-values obtained with the Friedman and Wilcoxon tests are listed in Table 3.
Table 3.
Resulting P-values
| Four-point stabilisation (P-values) | Flexion ROM+ | Extension ROM− | Lateral ROM+ | Bending ROM− | Axial ROM+ | Rotation ROM− |
|---|---|---|---|---|---|---|
| Friedman test | 0.04 | 0.02 | 0.31 | 0.02 | 0.20 | 0.61 |
| Wilcoxon test Mono- versus bisegmental |
0.60 | 0.17 | 0.07 | 0.6 | 0.07 | 0.34 |
Discussion
Sufficient mechanical stability of an anterior spinal instrumentation is of crucial importance, especially in minimally invasive spine surgery without additional dorsal fixation. In this study, it could be shown that for an exclusively anterior instrumentation, four-point stabilisation is required to achieve primary stability both in mono- and bisegmental instrumentation.
Compared with monosegmental stabilisation, with two-point stabilisation such as the HMA stabilisation, the primary stability diminishes in the case of bisegmental stabilisation by 53% in flexion/extension, 64% in lateral bending, and 37% in axial rotation. On the other hand, if bisegmental stabilisation is carried out with four-point stabilisation (Ventrofix), stability increases compared with the two-point bracing (US System ventral) by 47% in flexion/extension, 35% in lateral bending, and 59% in axial rotation. By using the newly developed four-point stabilisation MACS TL Twin Screw instrumentation, in contrast, a difference of up to 5% at most between mono- or bisegmental stabilisation is found with anterior stabilisation. This investigation demonstrates the necessity of anterior four-point stabilisation for both types of defects. Four-point stabilisation of this class should accordingly be regarded as standard anteriorly. This also applies to combined instrumentation, as the posterior implant is often removed early. So far there have been no comparable investigations with a similar objective. However, the values obtained for ROM and the NZ are similar to those of other studies [1, 6, 8, 9, 12–15, 27, 31].
Despite the improved screw holding strength, as shown in pull-out tests [26], adequate primary stability could not be achieved bisegmentally with the HMA system, probably because of possible translation movements over the axes. The obviously increased laxity of the specimen treated in this way is reflected in the dramatic increase in the NZ, especially in flexion/extension. Eliminating the translation movements by the additional anterior screw with four-point stabilisation when using the Ventrofix leads to the described decreases in total ROM in all directions when there is a bisegmental defect, and thus to an increase in primary stability.
All studies were conducted in accordance with the recommendations on standardising implant testing on the spine [30]. The use of pure moments in this study corresponds to the currently accepted loading mode for implant testing [14–16, 28, 30]. However, with this type of in vitro test, a few limitations must be pointed out.
Because different test conditions were selected in various earlier studies and because the choice of specimen differs (species, age, bone density), comparisons are difficult [11]. However, the values for ROM and the NZ can be compared with the studies listed [1, 6, 8, 9, 12–15, 27, 31]. Muscle strength, body weight, and so forth were neglected, and in addition, the tests were conducted with specimens from an advanced age group with poor bone density. Because only parameters of primary stability can be recorded with the listed test conditions, the test results only cautiously provide a basis for estimating long-term results for clinical use.
In light of current technical innovations favouring minimally invasive endoscopic spine surgery, the ventral anterior procedure should be carefully indicated. It is important to realise that only anterior four-point stabilisation enables primary stability to be obtained both in mono- and bisegmental instrumentation. We recommend therefore that four-point stabilisation be considered a standard in minimally invasive procedures.
Footnotes
An erratum to this article can be found at http://dx.doi.org/10.1007/s00586-005-1039-7
References
- 1.An HS, Lim TH, You JW, Hong JH, Eck J, McGrady LM. Biomechanical evaluation of anterior thoracolumbar spinal instrumentation. Spine. 1995;20:1979–1983. doi: 10.1097/00007632-199509150-00003. [DOI] [PubMed] [Google Scholar]
- 2.Been Eur Spine J. 2003;13:101. doi: 10.1007/s00586-003-0576-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beisse R, Potulski M, Temme C, Buhren V. Endoscopically controlled division of the diaphragm. A minimally invasive approach to ventral management of thoracolumbar fractures of the spine. Unfallchirurg. 1998;101(8):619–627. doi: 10.1007/s001130050315. [DOI] [PubMed] [Google Scholar]
- 4.Buhren V. Thoracoscopic management of fractures of the thoracic and lumbar spine. Langenbecks Arch Chir Suppl Kongressbd. 1998;115:108–112. [PubMed] [Google Scholar]
- 5.Buhren V, Beisse R, Potulski M. Minimally invasive ventral spondylodesis in injuries to the thoracic and lumbar spine. Chirurgie. 1997;68(11):1076–1084. doi: 10.1007/s001040050326. [DOI] [PubMed] [Google Scholar]
- 6.Gurr KR, Mc Afee PC, Shih CM. Biomechanical analysis of anterior and posterior instrumentation systems after corpectomy: a calf spine model. J Bone Joint Surg Am. 1988;70:1182–1191. [PubMed] [Google Scholar]
- 7.Hartwig E, Bischoff M, Kinzl L, Kramer M, Hawner A, Schultheiss M. Kostenträgerrechnung thorakoskopischerOperationsverfahren in der Versorgung von Wirbelfrakturen der Brust und Lendenwirbelsäule unter Berücksichtigung des pauschalisierten Vergütungssystem. Gesundh ökon Qual manag. 2003;8:231–237. doi: 10.1055/s-2003-41749. [DOI] [Google Scholar]
- 8.Hitchon P, Goal VK, Rogge T, Grosland N, Torner J. Biomechanical studies on two anterior thoracolumbar implants in cadaveric spines. Spine. 1999;24(3):213–218. doi: 10.1097/00007632-199902010-00004. [DOI] [PubMed] [Google Scholar]
- 9.Hitchon PW, Goel VK, Rogge TN, Torner JC, Dooris AP, Drake JS, et al. In vitro biomechanical analysis of three anterior thoracolumbar implants. J Neurosurg. 2000;93(Suppl 2):252–258. doi: 10.3171/spi.2000.93.2.0252. [DOI] [PubMed] [Google Scholar]
- 10.Kim DH, Jaikumar S, Kam AC. Minimally invasive spine instrumentation. Neurosurgery. 2002;51(Suppl 5):15–25. [PubMed] [Google Scholar]
- 11.Kotani YCB, Parker L, Kanayama M, Mc Afee P. Static and fatique biomechanical properties of anterior thoracolumbar instrumentation systems using a synthetic model. Spine. 1999;14:1406–1413. doi: 10.1097/00007632-199907150-00004. [DOI] [PubMed] [Google Scholar]
- 12.Lim TH, An HS, Hong JH, Ahn JY, You JW, Eck J, et al. Biomechanical evaluation of anterior and posterior fixations in an unstable calf spine model. Spine. 1997;22(3):261–266. doi: 10.1097/00007632-199702010-00005. [DOI] [PubMed] [Google Scholar]
- 13.Panjabi MM. Biomechanical evaluation of spinal fixation devices: I. A conceptual framework. Spine. 1988;13(10):1129–1134. doi: 10.1097/00007632-198810000-00013. [DOI] [PubMed] [Google Scholar]
- 14.Panjabi J Spinal Disord. 1992;5:383. doi: 10.1097/00002517-199212000-00001. [DOI] [PubMed] [Google Scholar]
- 15.Panjabi MM. The stabilizing system of the spine. Part II. Neutral zone and instability hypothesis. J Spinal Disord. 1992;5(4):390–397. doi: 10.1097/00002517-199212000-00002. [DOI] [PubMed] [Google Scholar]
- 16.Panjabi MM, Kato Y, Hoffman H, Cholewicki J, Krag MH. A study of stiffness protocol as exemplified by testing of a burst fracture model in sagittal plane. Spine. 2000;25(21):2748–2754. doi: 10.1097/00007632-200011010-00006. [DOI] [PubMed] [Google Scholar]
- 17.Regan JJ, Ben-Yishay A, Mack MJ. Video-assisted thoracoscopic excision of herniated thoracic disc: description of technique and preliminary experience in the first 29 cases. J Spinal Disord. 1998;11(3):183–191. [PubMed] [Google Scholar]
- 18.Richter M, Wilke HJ, Kluger P, Claes L, Puhl W. Biomechanical evaluation of a newly developed monocortical expansion screw for use in anterior internal fixation of the cervical spine. In vitro comparison with two established internal fixation systems. Spine. 1999;24(3):207–212. doi: 10.1097/00007632-199902010-00002. [DOI] [PubMed] [Google Scholar]
- 19.Schmidt R, Wilke HJ, Claes L, Puhl W, Richter M. Pedicle screw enhance primary stability in multilevelcervical corpectomies: biomechanical in vitro comparison of different implants including constrained and nonconstrained posterior instrumentations. Spine. 2003;28(16):1821–1828. doi: 10.1097/01.BRS.0000083287.23521.48. [DOI] [PubMed] [Google Scholar]
- 20.Schultheiss M, Claes L, Wilke H-J, Kinzl L, Hartwig E. Enhanced primary stability through additional cementable cannulated rescue screw for anterior thoracolumbar plate application. J Neurosurg. 2003;98:50–55. doi: 10.3171/spi.2003.98.1.0050. [DOI] [PubMed] [Google Scholar]
- 21.Schultheiss Thoracolumbar fracture. 2003;stabilization:comparative. [Google Scholar]
- 22.Schultheiss Eur Spine J. 2004;13:598. doi: 10.1007/s00586-004-0674-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schultheiss M, Kinzl L, Claes L, Wilke HJ, Hartwig E. Minimally invasive ventral spondylodesis for thoracolumbar fracture treatment: surgical technique and first clinical outcome. Eur Spine J. 2003;12(6):618–624. doi: 10.1007/s00586-003-0564-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schultheiss M, Wilke HJ, Claes L, Kinzl L, Hartwig E. MACS-TL polyaxial screw XL. A new concept for increasing stability of ventral spondylodesis in the presence of dorsal injuries. Orthopade. 2002;31(4):397–401. doi: 10.1007/s00132-001-0282-9. [DOI] [PubMed] [Google Scholar]
- 25.Schultheiss M, Wilke HJ, Claes L, Kinzl L, Hartwig E. MAC-TL twin screw. A new thoracoscopic implantable stabilization system for treatment of vertebral fractures–implant design, implantation technique and in vitro testing. Orthopade. 2002;31(4):362–367. doi: 10.1007/s00132-001-0276-7. [DOI] [PubMed] [Google Scholar]
- 26.Schultheiss M, Wilke H-J, Wenger K, Kinzl L, Claes L. Biomechanical in vitro comparison of anterior vertebral body screw fixation strength. J Bone Joint Surg Br. 1999;81B(Suppl 1):48. [Google Scholar]
- 27.Shono Y, McAfee PC, Cunningham BW. Experimental study of thoracolumbar burst fractures. A radiographic and biomechanical analysis of anterior and posterior instrumentation systems. Spine. 1994;19(15):1711–1722. doi: 10.1097/00007632-199408000-00010. [DOI] [PubMed] [Google Scholar]
- 28.Wilke HJ, Claes L, Schmitt H, Wolf S. A universal spine tester for in vitro experiments with muscle force simulation. Eur Spine J. 1994;3(2):91–97. doi: 10.1007/BF02221446. [DOI] [PubMed] [Google Scholar]
- 29.Wilke HJ, Rohlmann A, Neller S, Schultheiss M, Bergmann G, Graichen F, et al. Is it possible to simulate physiologic loading conditions by applying pure moments? A comparison of in vivo and in vitro load components in an internal fixator. Spine. 2001;26(6):636–642. doi: 10.1097/00007632-200103150-00014. [DOI] [PubMed] [Google Scholar]
- 30.Wilke HJ, Wenger K, Claes L. Testing criteria for spinal implants: recommendations for the standardization of in vitro stability testing of spinal implants. Eur Spine J. 1998;7(2):148–154. doi: 10.1007/s005860050045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zdeblick TA, Warden KE, Zou D, McAfee PC, Abitbol JJ. Anterior spinal fixators. A biomechanical in vitro study. Spine. 1993;18(4):513–517. [PubMed] [Google Scholar]