Abstract
The objective of this study was to determine atlanto-axial bone morphometric measurements related to screw transarticular fixation technique. One hundred helical computerized tomography (helical CT) scans with volumetric acquisition, including the first and the second cervical vertebrae, were studied. The screw insertion axis according to the Magerl technique for C1–C2 transarticular fixation was the referential to select the correct oblique axial and oblique parasagittal planes obtained with multiplanar reconstruction (MPR) on helical CT. The selected measured parameters on each side of the vertebrae were C2 interarticular isthmus height and width, optimal screw length, optimal screw trajectory sagittal and axial angles, and the distance between the ideal screw trajectory and the vertebral artery groove. C2 interarticular isthmus height measured 7.75±1.27 mm, C2 interarticular isthmus width 7.94±1.72 mm, optimal screw length 39.03±2.81 mm, optimal screw trajectory sagittal angle 57.54±5.28°, optimal screw trajectory medial angle 7.90±4.05°. Isthmus narrowing under 5 mm (height and/or width) was seen in 5% of cases. In 30% of cases reconstructed parasagittal images showed the vertebral artery groove. In those cases, the distance between the vertebral artery groove and the ideal screw path was measured. This distance measured under 2.5 mm in 7% of C2 articular masses. A classification of C2 articular mass morfology was proposed. The C2 articular masses without anatomic variations predisposing to vertebral artery injury were considered type I. The C2 articular masses potentially associated with vascular injury (12%) were classified as type II. Potential risk was identified at the C2 isthmus only (3%), at the anterior portion of C2 articular mass only (7%) or at both regions (2%). According to selected criteria 18% of patients would have at least one side C2 articular mass with potential risk for the vertebral artery. In 6% of patients the potential risk was identified bilaterally. There is a great variation in the maximum and minimum values of the anatomic measurements. Therefore preoperative CT scans are very important to identify type II cases, such that the surgeon may preoperatively define the bony anatomy trough which the screws will pass.
Keywords: Atlanto-axial joint, Arthrodesis, Helical computed tomography, Uupper cervical spine
Introduction
Transarticular screw fixation has been used used for posterior C1–C2 arthrodesis [2, 3, 5, 6, 11, 14, 16, 19, 23]. There are numerous indications for this procedure in both traumatic and non-traumatic lesions. Fundamentally, these indications are related to chronic and acute atlanto-axial instability. Transarticular screw arthrodesis provides immediate rigid atlanto-axial fixation and it has biomechanical advantages when compared to other techniques [7, 9, 17, 22]. Transarticular C1–C2 screw fixation could be performed even with fracture, destruction or absence of the posterior arch of the atlas. It also permits concurrent laminectomy to be performed if necessary. However, the anatomy of this region makes proper screw insertion challenging, and there is a danger of injury to the vertebral artery or to other neurovascular structures. This risk is partially related to anatomical variations.
Madawi et al. [13] identified three risk factors for vertebral artery injury associated with atlanto-axial transarticular screws: incomplete reduction prior to screw placement, previous transoral surgery with removal of the anterior tubercle or the arch of the atlas, thus eliminating an important fluoroscopic landmark, and failure to appreciate individual anatomical variations of the vertebral artery in C2 isthmus or lateral mass. In addition conditions leading to atlantoaxial instability, like fractures or rheumatoid arthritis, can alter the morphology of this area making proper screw placement potentially more difficult or impossible.
The use of preoperative diagnostic imaging prior to transarticular screw arthrodesis has also being pointed out in the literature [3, 10, 12, 15, 18]. In this study, the bone morphology of the atlantoaxial region was examined to define the relation of bony elements to the vertebral artery and the spinal canal. A preoperative helical computed tomography protocol is proposed, with multiplanar reconstructions on oblique axial and parasagittal planes.
Materials and methods
Computed tomography helical scans of 100 patients were used in this study. Patients underwent CT examination for investigation of carotid artery disease. Sixty-one patients were male and 39 were female. The mean age was 66.4 years (age range 14–86 years).
The helical CT examinations were performed using a PQ 5000 helical scanner (Picker International, Cleveland, Ohio, USA). Images were acquired in the axial plane with 3 mm sections, 1.5 mm reconstruction interval and a 2.0 pitch factor. All acquisitions were volumetric and included the complete atlanto-axial segment. Helical CT examinations were performed after 120–150 ml intravenous contrast injection with a power injector at 3–4 ml/s, with scan delay from 25 to 30 s.
The CT files were reloaded from magnetic tapes to a Voxel Q Picker computer workstation. The multiplanar reconstructions were performed and the ideal screw path for transarticular C1–C2 fixation was the referential to obtain the correct oblique parasagittal and axial planes. The oblique axial plane was chosen from C2 inferior articular facet to the midpoint of the anterior cortical bone of C1 lateral mass, trough the midpoint of C2 isthmus (Fig. 1). The oblique parasagittal plane was chosen from C2 inferior articular facet passing trough the midpoint of C2 isthmus and reaching the middle portion of the anterior cortex of C1 lateral mass (Fig. 2). Measurements were performed with a digital caliper in the multiplanar reconstruction images.
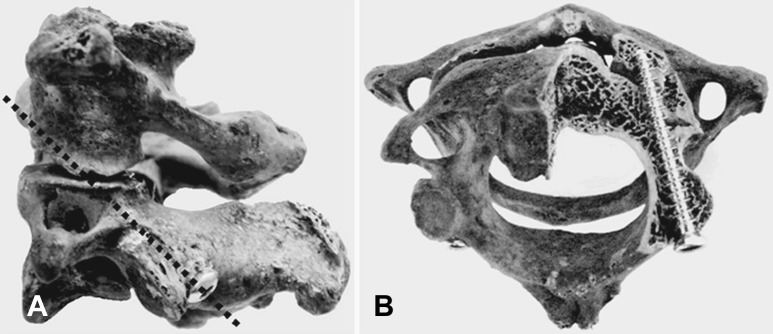
Fig. 1.
Axial oblique plane related to C1–C2 transarticular screw ideal trajectory. A Lateral view of atlanto-axial cadaveric vertebrae with dotted straight line representing the oblique axial plane B Specimen showing axial oblique plane analogous to the obtained plane at CT multiplanar reconstruction. There is superposition of a 3.5 mm screw for better illustration
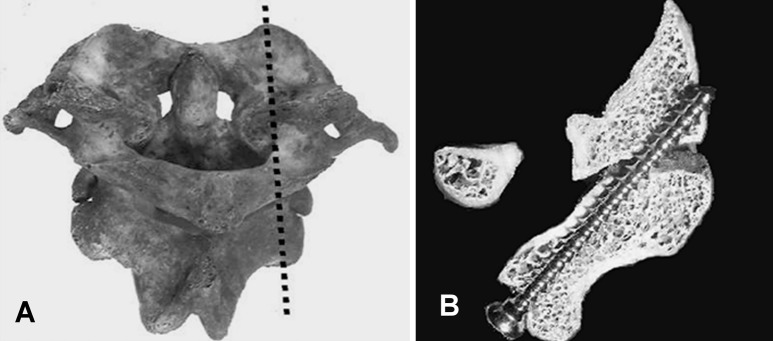
Fig. 2.
Parasagittal oblique plane related to C1–C2 transarticular screw ideal trajectory. A Posterior view of atlanto-axial vertebrae, where dotted line represents the parasagittal oblique plane. B Specimen showing oblique parasagittal plane analogous to CT multiplanar reconstruction. There is superposition of a 3.5 mm screw for better illustration
The selected parameters for measurement were C2 interarticular isthmus height and width, optimal screw length, and optimal screw trajectory sagittal and axial angles. In some cases reconstructed parasagittal images showed the vertebral artery groove. In these cases, the distance between the arterial groove and the ideal screw path was measured. For all purposes in this paper, the C2 isthmus was defined as suggested by Benzel [1].
The interarticular isthmus width and the screw optimal trajectory medial angle were measured on the oblique axial plane (Fig. 3). On the parasagittal plane the measured parameters were interarticular isthmus height, the optimal screw trajectory sagittal angle and optimal screw length (Fig. 4). In cases that the vertebral artery groove appeared on oblique parasagittal images the smaller distance from the groove to the optimal screw path was also measured.
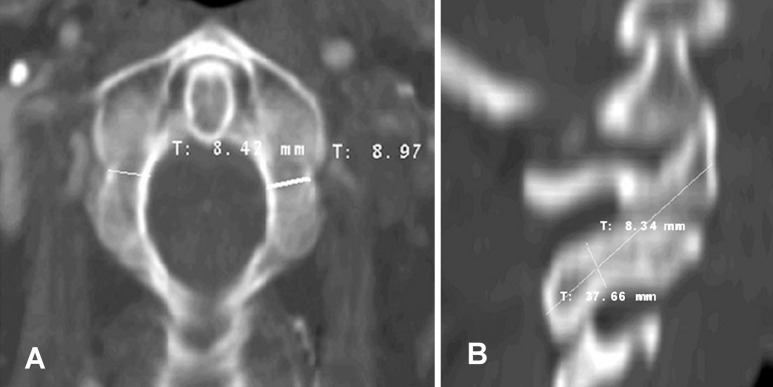
Fig. 3.
A Oblique axial plane in CT multiplanar reconstruction showing right and left isthmus width. B Parasagittal oblique plane with optimal screw length and isthmus height
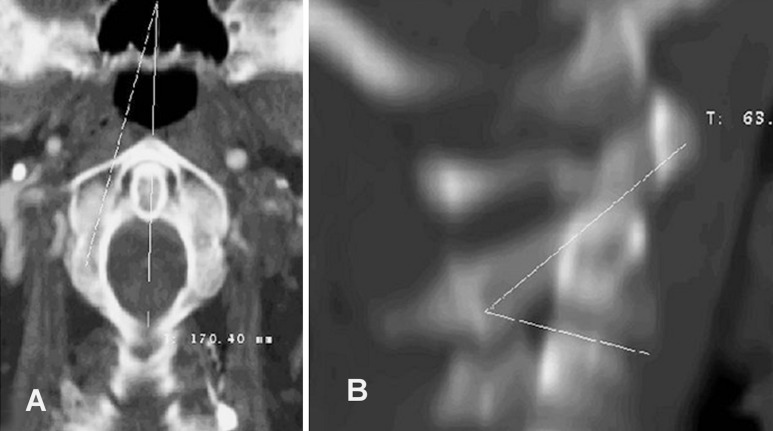
Fig. 4.
Oblique planes and angle measurements. A Axial oblique plane. B Parasagittal oblique plane
Interarticular isthmus height and width were measured perpendicular to the cortical bone and including cortical and cancellous bone, therefore corresponding to the isthmus external diameters. Isthmus height and width were measured at the thinnest points in the respective oblique reconstructed images.
The measured medial angle was made by a line parallel to the longitudinal axis of the isthmus and a line connecting the midpoint of the odontoid process to the junction C2 posterior arch at the midline. Positive medial angles values were attributed when the optimal screw path direction was antero-medial and negative medial angles were attributed when this direction was antero-lateral.
Optimal screw trajectory sagittal angle was obtained from a line parallel to the longitudinal isthmus axis and a line parallel to the vertebral body inferior endplate. Images utilized for measuring this angle were reconstructed with 12 mm thickness, allowing simultaneous identification of the inferior endplate and isthmus.
Statistical methods
Quantitative variables were compared using Student’s t-test after verification that the distribution of the variables was normal. The comparison of patient age to the measured parameters was made by Pearson correlation coefficient (r).
The reproducibility of the measuring method was assessed with repeated observations in a subgroup of 15 patients 2 months after the initial analysis. An intraclass correlation coefficient was calculated for each linear and angular parameter.
Results
Based on 100 atlanto-axial segments measured, the mean, range and standard deviation (SD) were calculated for each parameter. Calculations were also made separately for male and female and for right and left sides. There was a large variation in the measured parameters (Tables 1, 2).
Table 1.
Linear parameters related to transarticular atlanto-axial fixation measured on CT multiplanar reconstruction images (in mm). RIW right isthmus width, RIH right isthmus height, ROSL right optimal screw length, LIW left isthmus width, LIH left isthmus height, LOSL left optimal screw length, n number of patients
| Parameters | n | Mean | SD | Minimum | Maximum |
|---|---|---|---|---|---|
| RIW | 100 | 7.75 | 1.23 | 4.70 | 10.61 |
| RIH | 100 | 8.23 | 1.72 | 3.32 | 11.96 |
| ROSL | 100 | 38.74 | 3.04 | 26.90 | 46.94 |
| LIW | 100 | 7.77 | 1.33 | 3.62 | 10.15 |
| LIH | 100 | 7.73 | 1.75 | 1.89 | 9.44 |
| LOSL | 100 | 39.51 | 2.52 | 34.33 | 47.43 |
Table 2.
Angular parameters related to transarticular atlanto-axial fixation measured on CT multiplanar reconstruction images (in degrees). RMA right medial angle, RSA right sagittal angle, LMA left medial angle, LSA left sagittal angle, n number of patients
| Parameters | n | Mean | SD | Minimum | Maximum |
|---|---|---|---|---|---|
| RMA | 100 | 7.53 | 3.88 | −2.87 | 18.69 |
| RSA | 100 | 58.12 | 5.22 | 44.95 | 71.26 |
| cgrid LMA | 100 | 8.20 | 4.15 | −2.61 | 18.08 |
| LSA | 100 | 57.05 | 5.41 | 44.09 | 68.13 |
Differences related to sex were found to be significant for linear parameters that were larger on the male vertebrae (Table 3). No significant differences between male and female were found for the angular parameters (Table 3).
Table 3.
Comparison for measured values between male and female. RIW right isthmus width, RIH right isthmus height, ROSL right optimal screw length, RMA right medial angle, RSA right sagittal angle, LIW left isthmus width, LIH left isthmus height, LOSL left optimal screw length, LMA left medial angle, LSA left sagittal angle
| Male | Female | p | |||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| RIW | 8.03 | 1.10 | 7.31 | 1.31 | 0.004 |
| RIH | 8.59 | 1.66 | 7.66 | 1.70 | 0.007 |
| ROSL | 38.86 | 2.63 | 36.99 | 2.82 | <0.001 |
| RMA | 7.57 | 3.64 | 7.48 | 4.29 | 0.91 |
| RSA | 58.64 | 5.14 | 57.30 | 5.30 | 0.21 |
| LIW | 8.20 | 1.03 | 7.11 | 1.47 | <0.001 |
| LIH | 8.19 | 1.71 | 7.02 | 1.58 | <0.001 |
| LOSL | 40.42 | 2.23 | 38.08 | 2.29 | <0.001 |
| LMA | 7.69 | 4.21 | 9.00 | 3.98 | 0.12 |
| LSA | 57.71 | 5.48 | 56.02 | 5.22 | 0.13 |
The mean isthmus width was 7.75±1.27 mm, the mean right isthmus width was 7.75±1.23 mm, the mean left isthmus width was 7.77±1.33 mm. The mean isthmus height was 7.94±1.72 mm, the mean right isthmus height was 8.23±1.72 mm, the mean left isthmus height was 7.73±1.75 mm. The mean optimal screw length was 39.03±2.81 mm, the mean right optimal screw length was 38.74±3.04 mm, the mean left optimal screw length was 39.51±2.52 mm.
The mean medial angle was 7.90±4.05°, the mean right medial angle was 7.53±3.88° and the mean left medial angle was 8.20±4.15°. The mean sagittal angle was 57.54±5.28°, the mean right sagittal angle was 58.12±5.22° and the mean left sagittal angle was 57.05±5.41°.
In the most part of the analyzed vertebrae (70%) there was no visualization of the vertebral artery groove in the selected oblique parasagittal images. In 23% of the cases the vertebral artery groove was identified in only one side of the vertebra. In the remaining 7%, it was visualized in both sides. In the group where the groove was present on the selected images 12 patients were female and 18 were male.
Visualizing the vertebral artery groove in the selected oblique parasagittal image does not necessarily implicate potential risk to the artery when transarticular fixation is performed. It was considered that a distance less than 2.5 mm between the groove and the screw path would make transarticular fixation technically difficult and with great risk of vertebral artery injury.
Reproducibility of measurements was considered excellent for six parameters, with correlation coefficient >0.75, and reasonable to good, between 0.75 and 0.5, for other four parameters (left side isthmus height: 0.566; right side optimal screw length: 0.739; right side screw trajectory medial angle: 0.706 and left side screw trajectory medial angle: 0.723) . In no case was the correlation considered poor (correlation coefficient <0.4).
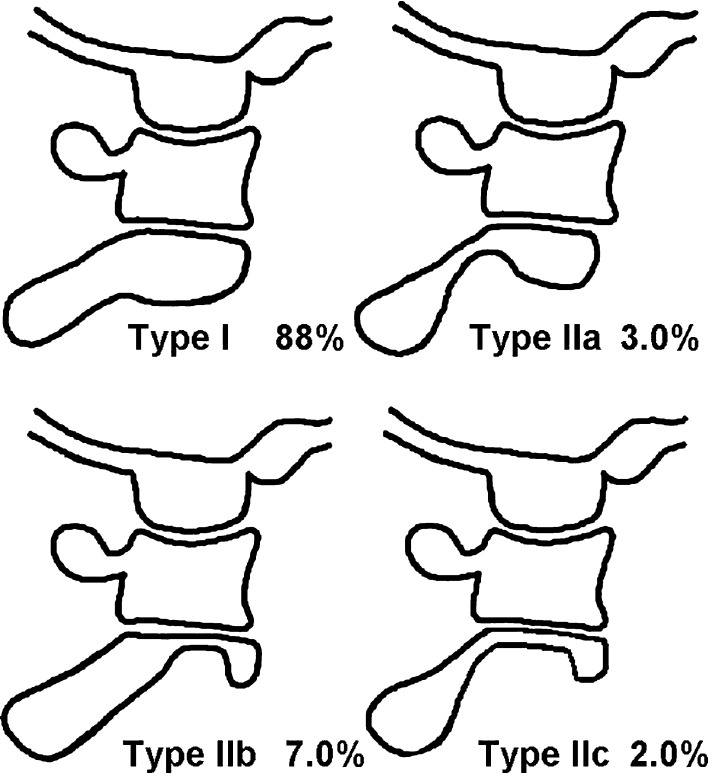
According to the observations and obtained results, a classification of the axis morphology was proposed. The morphology of the articular mass in the oblique axial and parasagittal reconstructed images were the referentials for the classification (Figs 5, 6). Each side of the vertebrae was considered separately for measurement and classification purposes. The type I articular masses showed no anatomical variations that could be related to potential risk to the vertebral artery in the transarticular arthrodesis technique (Fig. 6). Cases showing anatomical variations associated to potential risk for the vertebral artery integrity in transarticular arthrodesis were classified as type II (Fig. 6). Type II articular masses could be subdvided in types IIa, IIb and IIc, depending on which area was abnormal (Figs 5, 6). In type IIa were classified the cases with isthmus narrowing, considering isthmus height or width measuring less than 5 mm as the criteria. Type IIb articular masses showed a prominent vertebral artery groove in its anterior portion. The distance between the groove and the optimal screw path was less than 2.5 mm in type IIb articular masses. Type IIc cases showed criteria both for type IIa and IIb, with narrowing of isthmus and of the anterior portion of the articular mass. The analyzed sample was composed of 88% of type I articular masses, 3% of type IIa, 7% of type IIb and 2% of type IIc.
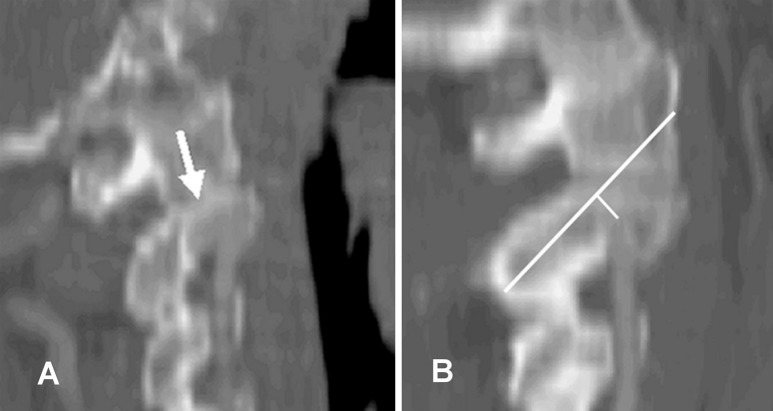
Fig. 5.
A Parasagittal oblique reconstruction at the ideal screw path for C1–C2 transarticular fixation showing the vertebral artery (arrow). B Another case showing optimal screw length measurement and measurement of the distance between the arterial groove and the screw trajectory
Fig. 6.
Classification of C2 articular masses morphology as demonstrated on CT parasagittal oblique multiplanar reconstructions
Type IIa articular masses were seen in 2% of all right side articular masses and in 4% of all left side articular masses studied. Type IIb were seen in 9% of all right side articular masses and in 5% of all left side articular masses studied. Type IIc were seen in 2% of both right and left side articular masses studied.
Forty percent of type IIb were bilateral (four patients) and 60% were unilateral (six patients). On two occasions, the same patient had the right side articular mass classified as type IIb and the left side as type IIa. Bilateral type IIa or type IIc cases were not identified.
The number of type IIb and type IIc cases was equal for both sexes. Type IIa classification was twice as common for female sex.
Anatomical variations resulting in increased risk to vertebral artery in the transarticular fixation technique were present in 12% of articular masses and in 18% of patients. In 6% of patients there was simultaneous risk for the right and left vertebral arteries according to the selected criteria. In 12% of patients risk was identified unilateraly, according to selected criteria.
Discussion
This study was undertaken to elucidate anatomical features of the vertebrae C1 and C2 that are important in the transarticular screw fixation. The study also aimed to identify the percentage of patients who may be at risk for vertebral artery injury when this technique is applied.
Madawi et al. [12] studied the groove for the vertebral artery in 50 dry specimens of the second cervical vertebra. In 11 specimens, one of the grooves was deep enough to reduce the internal height of the lateral mass to ≤2.1 mm. The internal height of the lateral mass was measured just above the arterial groove. Madawi et al. [12] considered that the placement of a transarticular screw would put the vertebral artery at extreme risk in vertebrae that present narrowing of the lateral mass at the same point that they measured the internal height. In their sample, 22% of patients would be at risk for vertebral artery injury during C1–C2 transarticular fixation.
Multiple clinical studies showed a much smaller frequency of this complication. Vertebral artery injury reports associated with C1–C2 transarticular fixation is very variable. There is a case report of vertebral artery injury resulting in arteriovenous fistula as a complication of C1–C2 transarticular screw fixation [2]. In general, the reported frequency of vertebral artery injury varies from 0 to 2.4% [3, 6, 8, 11, 16, 19, 23]. There is only one report with 8.2% (five cases) of vertebral artery injury, but in all this five cases there was no good reduction of C1–C2 subluxation before the screw insertion [13]. Probably poor reduction was the related factor to put in risk the vertebral artery.
The reported vertebral artery injury frequency in clinical studies contrasts with the risk estimated by Madawi et al. [12]. There are two important factors that could explain this apparent disagreement. The first is that many of the published series showing low incidence of vertebral artery injury included preoperative diagnostic imaging assessment of the patients. So in these series anomalous vertebral artery trajectories probably were known before surgery and precaution could be the point to explain the low incidence of arterial injuries. The second factor is that in the transarticular screw fixation technique as described by Magerl [5, 11, 14], the screw is inserted in the atlanto-axial complex in such a way that it tends to avoid the most inferior and lateral portions of C2 lateral mass. The screw usually passes more medially. Probably even in some cases with C2 articular mass internal height narrowing, as measured by Madawi et al. [12], the verterbal artery groove does not approximate the optimal screw path.
To evaluate the true interference from the vertebral artery groove and from other possible anatomical variations in the transarticular fixation technique the present study appraised the bony elements directly in the screw path. In the present study, 7% of articular masses showed a dangerous distance (distance measuring less than 2.5 mm, according to the selected criteria) from the vertebral artery groove to the screw ideal trajectory. They correspond to type IIb cases.
The value of 2.5 mm chosen to represent the security limit for the distance between the screw pathway and the vertebral artery groove is obviously arbitrary. It was though chosen as 2.5 mm to be equivalent to the security limit adopted in previous literature [15]. Mandel et al. [15] considered that isthmus height and width measurements as thick as 5 mm were safe for this type of instrumentation. If one realizes that the screw pathway is adimensional, the safe distance adopted by Mandel et al. [15] from the screw trajectory to each of the isthmus external surfaces would be the same, 2.5 mm.
Mandel et al. [15] previously studied C2 isthmus dimensions interested in the placement of transarticular screws. The present study also measured the isthmus height and width, and in despite of different population and methodology the mean results were similar. Mandel et al. [15] did not study the axis articular mass directly. They found 11.7% of narrowed isthmus, with at least one diameter measuring less than 5 mm. In the present study only 5% of C2 isthmus were found to measure less than 5 mm, corresponding to the cases classified as type IIa and type IIc.
The optimal screw length for transarticular arthrodesis has been described in the literature, although in smaller samples [4, 9]. The present results are very close to the previously reported results. Xu et al. [20, 21] assessed the value of using lateral radiographs in evaluating the optimal screw length in transarticular C1–C2 fixation. Their results showed that intraoperative lateral fluoroscopy may not be reliable in determining optimal screw length, although it is valuable in directing accurate screw angle in the sagittal plane. The optimal screw length is an important question since the area where the hypoglossal nerve lies is approximately 2–3 mm lateral to the middle of the anterior aspect of the C1 lateral mass [4]. Hypoglossal nerve injury is a complication associated with transarticular C1–C2 screw placement and can be caused by a misdirected or too long screw [6].
To our knowledge there has been no previous study measuring directly the optimal screw insertion angles for this type of arthrodesis. Madawi et al. [13] described the medial angle of C2 facet pedicle complex. Xu et al. [20] assessed medial and sagittal C2 pedicle angles, that are in reality isthmus angles. Those angles are obviously different from the screw trajectory angles. The screw trajectory does not follow the isthmus long axis, since it aims at the C1 lateral mass and not the C2 vertebral body.
There are some aspects to be considered about the present study methodology. First, normalization of the measurements was not available to account for patient constitutional characteristics like height and weight. Also, patients age and gender are biased by the nature of the investigation, since initially the patients were scanned for carotid arterial diseases. Osteoarthosis changes of C1–C2 anatomy are more likely to occur in patients in the studied group, and this probably has some influence in the performed measurements. Although intraobserver agreement was very good, interobserver assessment of measurements are not available.
Atlanto-dental interval plays an important role in the screw trajectory [13]. Atlanto-dental interval was not directly measured in our study. In the other hand no cases with atlanto-axial luxation or subluxation were present, such that this should not be a major concern when interpreting our results
The images in this study are acceptable but better resolution reconstructions can be achieved for clinical purposes. Since CT examinations were performed for carotid arterial studies the imaging protocol was not optimized for pre-operative evaluation of C1–C2 region. For specific preoperative study of atlanto-axial posterior fixation it would be better to use thinner sections.
To have consistency in our measurements it was necessary to define the “ideal” or “optimal” screw trajectory in some way. It is very likely that when planning a C1–C2 fixation surgery the ideal screw trajectory for some cases would be somewhat different from the one proposed in this paper. In daily practice it is not advantageous to be rigorously tied to fixed rules, at least in this case, since individual anatomic variations could be present.
The present study with results totalized 12% of C2 articular masses at potential risk to the vertebral artery if transarticular screw fixation is considered. The C2 articular mass may show narrowing at the isthmus, at its anterior portion or both.
A classification depicting this consideration is proposed to facilitate the identification of cases without risk (type I) and cases were C1–C2 screw fixation would likely be a risky procedure (type II). This could facilitate evaluation by and communication with radiologists, who are usually not aware of details of screw trajectory. Many times, the spine surgeon is not present when mutiplanar reconstructions are performed and documented at the CT workstation.
A preoperative imaging protocol with helical CT multiplanar reconstructions is also proposed, with emphasis in the oblique axial and parasagittal planes that are selected to demonstrate the screw pathway.
Conclusion
Morphometric measurements related to screw transarticular arthrodesis technique were described. There is a great variation in the maximum and minimum values of the anatomic measurements. Care must be taken in utilizing the statistical results in surgical practice. This study confirms that anatomical variations can be associated to technical difficulty for placement of transarticular C1–C2 screws. Therefore, helical CT multiplanar (MPR) reconstructions are very important for a pre operative assessment. CT measurements showed good reproducibility. We emphasize that the use of oblique axial and oblique parasagittal reconstructions in the screw trajectory is an easy and safe way to achieve optimal preoperative evaluation.
References
- 1.Benzel EC. Anatomic consideration of C2 pedicle screw placement: letter to the editor. Spine. 1996;21:2301–2302. doi: 10.1097/00007632-199610010-00028. [DOI] [PubMed] [Google Scholar]
- 2.Coric D, Branch CL, Wilson JA, Robinson JC. Arteriovenous fistula as a complication of C1-C2 transarticular screw fixation: case report and review of the literature. J Neurosurg. 1996;85:340–343. doi: 10.3171/jns.1996.85.2.0340. [DOI] [PubMed] [Google Scholar]
- 3.Dickman CA, Sonntag VKH. Posterior C1-C2 transarticular screw fixation for atlantoaxial arthrodesis. Neurosurgery. 1998;43:275–281. doi: 10.1097/00006123-199808000-00056. [DOI] [PubMed] [Google Scholar]
- 4.Ebraheim NA, Misson JR, Xu R, Yeasting RA. The optimal trans-articular C1-C2 screw length and the location of the hypoglossal nerve. Surg Neurol. 2000;53:208–210. doi: 10.1016/s0090-3019(00)00160-9. [DOI] [PubMed] [Google Scholar]
- 5.Grob D, Magerl F. Surgical stabilization of C1 and C2 fractures. Orthopade. 1987;16:46–54. [PubMed] [Google Scholar]
- 6.Grob D, Jeanneret B, Aebi M, Markwalder T. Atlanto-axial fusion with transarticular screw fixation. J Bone Joint Surg [Br] 1991;73:972–976. doi: 10.1302/0301-620X.73B6.1955447. [DOI] [PubMed] [Google Scholar]
- 7.Grob D, Crisco JJ, Panjabi MM, Wang P, Dvorak J. Biomechanical evaluation of four different posterior atlantoaxial fixation techniques. Spine. 1991;17:480–490. doi: 10.1097/00007632-199205000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Haid RW. C1-C2 transarticular screw fixation: technical aspects. Neurosurgery. 2001;49:71–74. doi: 10.1097/00006123-200107000-00011. [DOI] [PubMed] [Google Scholar]
- 9.Hanson PB, Montesano PX, Sharley NA, Rauschning W. Anatomic and biomechanical assesment of transarticular screw fixation for atlantoaxial instability. Spine. 1991;16:1141–1145. doi: 10.1097/00007632-199110000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Howington JU, Kruse JJ, Awasthi D. Surgical anatomy of the C2 pedicle. J Neurosurg. 2001;95:88–92. doi: 10.3171/spi.2001.95.1.0088. [DOI] [PubMed] [Google Scholar]
- 11.Jeanneret B, Magerl F. Primary posterior fusion C1/C2 in odontoid fractures: indications, techniques, and results of transarticular screw fixation. J Spinal Disord. 1992;5:464–475. doi: 10.1097/00002517-199212000-00012. [DOI] [PubMed] [Google Scholar]
- 12.Madawi AA, Solanki G, Casey ATH, Crokard HA. Variation of the groove in the axis vertebra for the vertebral artery—implications for instrumentation. J Bone Joint Surg. 1997;79:820–823. doi: 10.1302/0301-620X.79B5.7566. [DOI] [PubMed] [Google Scholar]
- 13.Madawi AA, Casey ATH, Solanki GA, Tuite G, Veres R, Crokard HA. Radiological and anatomical evaluation of the atlantoaxial transarticular screw fixation technique. J Neurosurg. 1997;86:961–968. doi: 10.3171/jns.1997.86.6.0961. [DOI] [PubMed] [Google Scholar]
- 14.Magerl F, Seeman PS (1987) Stable posterior fusion of the atlas and axis by trans-articular screw fixation. In: Kehr P, Weidner A (eds) Cervical spine. Springer, Berlin Heidelberg New York, pp 322–327
- 15.Mandel IM, Kambach BJ, Petersilge CA, Johnstone B, Yoo JU. Morphologic considerations of C2 isthmus dimensions for the placement of transarticular screws. Spine. 2000;25:1542–1547. doi: 10.1097/00007632-200006150-00014. [DOI] [PubMed] [Google Scholar]
- 16.Marcotte P, Dickman CA, Sonntag VKH, Karahalios DG, Drabier J. Posterior atlantoaxial facet screw fixation. J Neurosurg. 1993;79:234–237. doi: 10.3171/jns.1993.79.2.0234. [DOI] [PubMed] [Google Scholar]
- 17.Naderi S, Crawford NR, Song GS, Sonntag VKH, Dickman CA. Biomechanical comparison of C1-C2 posterior fixations: cable, graft, and screw combinations. Spine. 1998;23:1946–1956. doi: 10.1097/00007632-199809150-00005. [DOI] [PubMed] [Google Scholar]
- 18.Solanski GA, Crockard HA. Preoperative determination of the safe superior transarticular screw trajectory trough the lateral mass. Spine. 1999;24:1477–1482. doi: 10.1097/00007632-199907150-00014. [DOI] [PubMed] [Google Scholar]
- 19.Stillerman CB, Wilson JA. Atlanto-axial stabilization with posterior transarticular screw fixation:technical description and report of 22 cases. Neurosurgery. 1993;32:948–955. doi: 10.1227/00006123-199306000-00011. [DOI] [PubMed] [Google Scholar]
- 20.Xu R, Nadaud MC, Ebraheim NA, Yeasting RA. Morphology of the second cervical vertebra and the posterior projection of the C2 pedicle axis. Spine. 1995;20:259–263. doi: 10.1097/00007632-199502000-00001. [DOI] [PubMed] [Google Scholar]
- 21.Xu R, Ebraheim NA, Misson JR, Yeasting RA. The reliability of the lateral radiograph in determination of the optimal transarticular C1-C2 screw length. Spine. 1998;23:2190–2194. doi: 10.1097/00007632-199810150-00009. [DOI] [PubMed] [Google Scholar]
- 22.Wilke HJ, Fischer K, Kluger A, et al. In vitro investigations of internal fixation systems of the upper cervical spine: stability of posterior atlanto-axial fixation techniques. Eur Spine J. 1992;1:191–199. doi: 10.1007/BF00301312. [DOI] [PubMed] [Google Scholar]
- 23.Wright NM, Lauryssen C. Vertebral artery injury in C1-C2 transarticular screw fixation: results of a survey of the AANS/CNS section on disorders of the spine and peripheral nerves. J Neurosurg. 1998;88:634–640. doi: 10.3171/jns.1998.88.4.0634. [DOI] [PubMed] [Google Scholar]