Abstract
Purpose: To examine the frequency distribution of the Ser680Asn polymorphism of the follicle-stimulating hormone receptor (FSHR) gene in ovarian dysfunction (OD) infertile women, “poor responders” (PR) and “good responders” (GR).
Methods: The hormonal profiles and treatment of all patients were analyzed and FSHR polymorphism was examined by PCR and RFLP. Women from all groups were classified as Asn/Asn, Asn/Ser, and Ser/Ser genotypes.
Results: The frequency distribution of Ser/Ser, Asn/Ser and Asn/Asn variants in OD patients was 45.5, 22.7, and 31.8%, respectively. Day 3 FSH levels in OD and GR patients were higher in Ser/Ser and Asn/Asn subgroups. Asn/Ser carriers from OD and GR groups provided more follicles and oocytes compared to other allelic variants.
Conclusions: GR patients carry more often the Asn/Ser genotype. The latter is correlated with more follicles and oocytes in both OD and GR patients. The Ser/Ser variant might be related to higher serum FSH levels, while the Asn/Ser with lower.
KEY WORDS : FSH receptor, gene polymorphisms, ovarian response, ovarian stimulation.
INTRODUCTION
Follicle stimulation hormone (FSH) and luteinizing hormone (LH) are two pituitary glycoproteins which are essential for normal gonadal function. They coordinate and regulate gonadal growth, differentiation, endocrine function and gametogenesis in both sexes (1,2). The effects of FSH and LH are mediated through binding to specific cell surface receptors, FSHR and LHR, respectively. We have previously demonstrated the presence of FSHR and LHR messenger RNA (mRNA) in both mouse and human denuded oocytes and preimplantation embryos from zygotes to blastocysts, thus indicating a possible role for gonadotrophins in the resumption of meiosis and early embryonic development (3,4).
FSHR and LHR belong to the large family of G-protein-coupled receptors, which span the plasma membrane seven times and transduce the biological action of FSH and LH, using cyclic AMP (cAMP) as the main intracellular second messenger (5,6). The FSHR gene contains a single large exon, which encodes the transmembrane and intracellular domains, and nine smaller exons which encode the extracellular domain. The complementary DNA encoding the FSHR has been cloned in several species, including human species (7–9). An inactivating mutation in the FSHR gene has been described in Finnish families with autosomal recessive premature ovarian failure (POF), while studies in a Brazilian and a Japanese population with POF failed to identify similar genomic alterations (10–13).
In assisted reproduction programs, the response of “good responders” or “poor responders” to exogenous FSH is individualized and the ovarian response to intense gonadotrophin stimulation is difficult to predict. Ovarian response to FSH stimulation has been shown to depend on the FSH genotype. Mayorga et al. investigated the role of two distinct FSHR variants, Thr307/Asn680 and Ala307/Ser680, in the ovarian response to FSH in women undergoing controlled ovulation induction. Using a standard stimulation regimen, the authors reported a highly significant difference in the number of ampoules required for successful ovulation induction. This finding was related to the patients’ day 3 serum FSH levels (14).
Day 3 serum FSH seems, indeed, to be the best predictive marker for ovarian function, even though a significant intraindividual variation from cycle to cycle and potential differences in the bioactivity of FSH measured should be taken into consideration (15,16). Other factors proposed to affect ovarian response to FSH are the distribution of FSH isoforms and the single nucleotide polymorphisms (17,18). Various parameters which could be used to estimate a patient's ovarian reserve, are easily measurable, minimally invasive and inexpensive have been described. Scott et al. have suggested that day 3 basal FSH levels represent a parameter which might meet the above criteria (15). Other authors detected differences between inhibin levels in normal and poor responders during complex ovulation induction cycles, but still basal levels were not different (19). Furthermore, studies examining inhibin levels in women with different ages provide little support for this specific parameter. It has also been reported that luteinized granulosa cells from women with elevated day 3 FSH levels produce less steroids, are less viable in culture, have a reduced mitotic index and produce decreased quantities of insulin growth factor I and II (IGFI and IGFII). In contrast, no differences in inhibin production were detected (20). Basal FSH level screening has been extremely well studied and validated in assisted reproduction regimens and remains the screening tool of choice in many programs.
In the present study, we examined the prevalence of Ser680Asn polymorphisms of the FSHR gene. Furthermore, we investigated the associations between the receptor polymorphisms and hormonal profiles. Finally, we correlated the variants with the clinical characteristics of assisted reproductive technologies (ART) in “poor responders” (PR), “good responders” (GR) and “ovarian dysfunction” (OD) Greek patients.
MATERIALS AND METHODS
Seventy-nine subfertile women and 46 normo-ovulatory women, who presented at the IVF Unit of the “Alexandra” Maternity Hospital, were included in this study. Institutional review board approval was obtained.
Thirty-five were documented as “poor responders” in a previous attempt. In our study, patients that had either: (a) three or less follicles developed or three or less eggs retrieved after ovulation induction for IVF or ICSI or (b) serum oestradiol concentrations between 500 and 660 pg/mL at the time of human chorionic gonadotropin (hCG) administration were considered as poor responders (20,21). Since there is no consistent definition of poor responders in the literature, the above thresholds were selected because they represent the lowest 10% of ovarian responsiveness among patients who participated in this study. These definitions are similar to others previously described (20–22). Forty-six more women who had been previously treated in our IVF clinic were selected as “good responders.” Good responder patients aged between 25 and 34 years, presented with FSH and LH levels within the normal range and normal body mass index. We collected more than eight oocytes from each of these patients. The fertilization rate was 99%, the quality of embryos was excellent and oestradiol (E2) levels on the day of hCG administration ranged between 1500 and 3500 pg/mL. Fourty-four women with “ovarian dysfunction” constituted the last group of patients in this study, who had previously undergone stimulation with the short protocol. FSH level on day 3 of the menstrual cycle was above 9 IU/L (normal range 2–9). A group of imminent ovarian failure (IOF) patients characterized by regular menstrual cycles and slightly elevated follicular phase FSH, has been previously described (23). These patients are often referred to as having imminent or incipient ovarian failure (24–26). In our study we named them “ovarian dysfunction” patients. Koning et al. suggested that elevatedFSH in women with IOF might be explained by the presence of higher FSH pulses (23). These larger FSH pulses result from an increase in pituitary response to GnRH. The patients were screened only for the presence of abnormalities in the FSH polymorphism analysis. After clinical and laboratory examination these patients were enrolled either in IVF or ICSI programs. In this study, neither patients with polycystic ovary syndrome, nor patients with an abnormal LH-to-FSH ratio were included. The LH-to-FSH ratio of the enrolled patients was within the normal limits.
Basal (day 3) serum FSH, LH, and prolactin levels were measured by electrochemiluminescence immunoassay (Roche Molecular, Biochemicals, Mannheim, Germany) in the cycle just before ovulation induction. This practice is being routinely applied in our department for several years and does not include measurement of basal estradiol levels. Prolactin levels are measured for a better evaluation of the patient, since unusually high serum prolactin levels could lead to cycle cancellation and appropriate treatment prior to initiation of an IVF cycle. The E2 level on the day of hCG administration was measured using a commercially available chemiluminescent Microparticle Immunoassay (CMIA) kit (Abbott Laboratories, Abbott Park, IL, USA).
Women defined as “good responders” were superovulated with exogenous gonadotrophin administration. The stimulation protocol is described briefly as follows (27). On day 21 of the previous cycle, a baseline ultrasound scan was performed and buserelin acetate intranasal spray administration began at a dose of 100 μg five times per day. GnRH agonist administration was maintained until hCG administration began. The extent of ovarian suppression in all patients’ was evaluated by ultrasound scan and serum E2 levels (≤40 pg/mL) before starting exogenous gonadotrophin administration (about 15 days after administering the spray). Having performed a follow-up, hCG was given when at least two follicles were larger than 18 mm and serum oestrogen levels were rising.
Oocytes were retrieved 34 h after the administration of 10,000 IU hCG. Follicular aspiration and oocyte retrieval were performed by transvaginal ultrasound guided puncture. Approximately 4 h after oocyte collection, the cumulus and corona cells were removed by incubation in Ham's F-10 medium (Invitrogen Life Technologies, Paisley, UK) with 80 IU/mL hyaluronidase (type VII, 320 IU/mg; Sigma-Aldrich, Dorset, UK) for 30 s. The oocytes were then transferred to fresh medium, and adhering corona cells were further removed by mechanical pipetting. Several microscopic examinations were performed to ensure complete removal of cumulus cells before ICSI took place.
ICSI was performed only in mature oocytes which had extruded the first polar body (metaphase II). The ICSI procedure was performed following conventional techniques (28).
The “poor responder” and “ovarian dysfunction” patients who met the above criteria began a short-term protocol with buserelin (500 μg/day intranasal) on cycle day 2. Gonadotrophin administration began on day 3 at a dose of 200 IU of rFSH (16).
Plasma E2 levels were measured daily starting 7 days after commencing the regimen until the day after hCG administration. The first scan was performed on day 7 and subsequent scans were performed every day until oocyte retrieval.
The dose of rFSH was adjusted according to ovarian response 6 days after the onset of gonadotrophin administration. GnRHa administration was continued until 10,000 IU of human chorionic gonadotropin (hCG) were injected intramuscularly. At the same time the mean diameter of at least two leading follicles was above 18 mm and serum E2 level was rising.
The long stimulation protocol was chosen for the group of “good responders” because this one results in the best outcome when applied for such patients, according to literature and to our experience. For the “poor responders” and the “ovarian dysfunction” groups of patients the short protocol of stimulation was followed for similar reasons. All the protocols used in these groups of patients have been previously described in detail (29).
Embryos were scored and chosen for transfer based on rapid cleavage, absence of fragmentation, and size of blastomeres (good quality, A; poor quality, B) (28).
Genomic DNA was obtained from peripheral blood leukocytes with the QIAamp DNA Blood Kit (QIAGEN, Hilden, Germany) according to the manufacturer's instructions. Polymerase chain reaction amplification of a fragment of exon 10 of the FSHR was performed with the use of specific oligonucleotide primers, as described elsewhere (30). The region of nucleotide number 1624 to 2143 was amplified using primer 1: 5′-TTTGTGGTCATC-TGTGGCTGC-3′ and primer 2: 5′-CAAAGGCAAGGACTGAATTATCATT-3′. The PCR product was 520 bp long. The PCR reaction was performed in a final volume of 50 μL containing 1× PCR buffer, 1.5 mM MgCl2, 200 μM of each dNTP, 1 μM of each primer, two units of Taq-DNA polymerase (Invitrogen Life Technologies) and 5 μL of the DNA template. The cycling conditions were as follows: initial denaturation at 94°C for 5 min, 40 cycles consisting of denaturation at 94°C for 1 min, annealing at 60°C for 1 min, extension at 72°C for 1 min and a final elongation step at 72°C for 10 min. All reactions were overlaid with light white oil and the MJ Research PTC200 Thermal cycler (Waltham, MA) was used in all experiments. PCR products were visualized under UV light and photographed with a polaroid camera.
PCR products of exon 10 were digested with BsrI. Digestion was performed in 10 μL reactions containing 1× reaction buffer, five units of the restriction enzyme and 8 μL of purified PCR product, incubated at 37°C overnight. Restriction endonuclease digestion products were visualized in 2.5% agarose gels and photographed. The presence of the Asn680Ser genotype introduces a restriction site for BsrI as it creates the A to G transition. Therefore, three different patterns can be observed, a 520 bp band (for 680 Asn/Asn), a 520bp and a 413 bp band (for 680 Asn/Ser), and a 413 bp band (for 680 Ser/Ser). All PCR products were sequenced on both strands to confirm the results and examine the presence of polymorphisms.
For statistical interpretation of the results the Kruskal Wallis and Mann–Whitney tests were employed. The first was used for the analysis of variance between subgroups and the second for the comparison between subgroups and chi-square analysis for frequency distribution. Correlations were evaluated using Spearman's correlation coefficient. Probabilities of less than 0.05 were accepted as significant. Data are presented as mean ± standard deviation, unless otherwise stated.
RESULTS
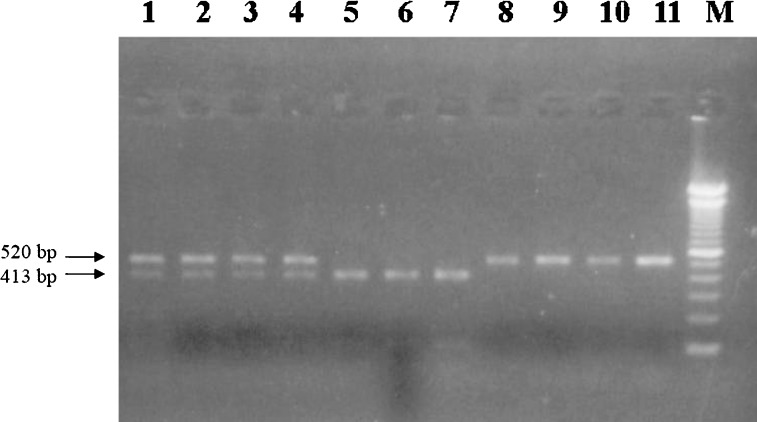
All PCR reactions yielded products of the expected size. RFLP analysis for the polymorphism at position 680 (exon 10) determined the genotype distribution for Ser/Ser, Asn/Ser, Asn/Asn polymorphism in patients with ovarian dysfunction (OD), poor responders (PR) and good responders (GR). RFLP results from randomly selected samples are presented in Fig. 1.
Fig. 1.
RFLP analysis of the Asn680Ser FSHR variant. Following BsrI digestion of the PCR products, 2.5% agarose gel electrophoresis revealed the patterns presented. lanes 1–4 present two bands, 520 and 413 bp, corresponding to the Asn/Ser variant, lanes 4–7 present a 413 bp band corresponding to the Ser/Ser variant, and lanes 8–11 present a 520 bp band corresponding to the Asn/Asn variant. M represents a 100 bp molecular size marker (Invitrogen Life Technologies).
We analyzed the hormonal and ovulation results according to the genotype variant (Ser/Ser, Asn/Ser, Asn/Asn). Significant differences are summarized on Table I. Gonadotropin dose correlated significantly with the observed levels of day 3 FSH (Spearman's correlation coefficient, p < 0.05). This correlation becomes stronger if the Spearman's coefficient is calculated for each specific genotype variant subgroup (Ser/Ser: p < 0.001; Asn/Ser: p < 0.01; Asn/Asn: p < 0.05).
Table I.
Biological and Clinical Characteristics of 125 Patients Who Underwent IVF/ICSI, Grouped According to FSHR Polymorphism
| Age (year) | FSH (mIU/mL) | LH (mIU/mL) | PRL (ng/mL) | Estrogen levels on HCG admin (pg/mL) | Total rFSH dose (IU) | Stimulation days | No. of follicles | No. of oocytes | Mature oocytes (%) | Fertilization rate (%) | Pregnancies (n) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Asn/Ser | 29 ± 3 | 7.2 ± 3.4* | 4.8 ± 2*** | 10.2 ± 1.9*** | 2725 ± 1788** | 3089 ± 1430 | 11 ± 0 | 8.4 ± 2.9*** | 7.8 ± 2.9*** | 70.2 ± 2.5 | 97.0 ± 5.1 | 3 / 49 |
| Ser/Ser | 30 ± 3 | 9.1 ± 3.5* | 7.9 ± 1.2*** | 14.7 ± 3.9*** | 1579 ± 1150** | 3518 ± 1510 | 11 ± 1 | 6.5 ± 2.1*** | 6.1 ± 2.4*** | 67.0 ± 12.1 | 97.2 ± 2.3 | 3 / 42 |
| Asn/Asn | 32 ± 3 | 8.4 ± 2.1* | 6.6 ± 3.5*** | 12.8 ± 2.8*** | 1262 ± 660** | 3132 ± 981 | 11 ± 0 | 5.6 ± 2.8*** | 5.2 ± 3.6*** | 91.3 ± 10.1 | 95.0 ± 5.5 | 2 / 34 |
Note. Kruskal Wallis test for the analysis of variance.
*p < 0.05; **p < 0.01; ***p < 0.001.
In OD and GR patients, day 3 FSH levels were statistically higher in Ser/Ser and Asn/Asn subgroups compared to Asn/Ser subgroup of patients (p < 0.05 and p < 0.001 respectively), thus indicating a relative resistance to the action of FSH in the former subgroups. As a confirmation to this, estrogen levels on the day of hCG administration were significantly higher in the Asn/Ser subgroup (p < 0.01). Moreover, the numbers of preovulatory follicles and collected oocytes were higher in the Asn/Ser subgroup (p < 0.01) (Table I). However, pregnancy rates were similar between the three subgroups (Asn/Ser: 3/49; Ser/Ser: 3/42; Asn/Asn: 2/34).
Frequencies of the allelic variants in the OD group (44 patients) were equally distributed: Ser/Ser: 20 (45.5%), Asn/Ser: 10 (22.7%) and Asn/Asn: 14 (31.8%) (chi-squarep = 0.178)(Table II). The three genotypes were equally distributed in the PR group as well (chi-square p = 0.49). However, patients in the GR group had a statistically significant tendency to carry the Asn/Ser variant(p < 0.05) (Table II).
Table II.
Frequency Distribution of Different Allelic Variants in 125 Women According to Ovarian Function
| Asn/Ser | Ser/Ser | Asn/Asn | Total | |
|---|---|---|---|---|
| Ovarian dysfunction | 10a | 20a | 14a | 44 |
| Poor responders | 15a | 10a | 10a | 35 |
| Good responders | 24* | 12* | 10* | 46 |
| Total | 49a | 42a | 34a | 125 |
Note. Data are number of subjects. Chi-square analysis of frequency distribution.
aNon significant.
*p < 0.05.
By definition, OD patients had significantly higher levels of FSH and LH, in comparison with the PR and GR groups (p < 0.001). Estrogen levels on the day of hCG administration were significantly higher in the Asn/Ser variant subgroup, of the OD and GR patients, signifying a more intense ovarian response (p < 0.001) (Table III). This finding was further supported by the significantly lower levels of recombinant gonadotrophin dose required for ovulation induction, in comparison with what happens with the Ser/Ser variant of the OD and the Asn/Asn variant of the GR group (p < 0.05 and p < 0.01, respectively) (Table III).
Table III.
Biological and Clinical Characteristics of 125 Patients Who Underwent IVF/ICSI, Grouped According to Ovarian Response
| Age (year) | FSH (mIU/ mL) | LH (mIU/ mL) | E2 (pg/mL) on HCG administration (pg/mL) | Gonadotropin dose (IU) | Follicles (#) | Oocytes (#) | Pregnancies | |
|---|---|---|---|---|---|---|---|---|
| Ovarian dysfunction (OD) | ||||||||
| Asn/Ser | 28 ± 4 | 15.8 ± 5.7 | 10.7 ± 1.1 | 2822 ± 319*** | 3528 ± 559 | 9.3 ± 1.4* | 7.8 ± 1.6* | 0 / 10 |
| Ser/Ser | 32 ± 3 | 14.3 ± 2.1 | 8.8 ± 2.3 | 740 ± 89*** | 4491 ± 25.0* | 4.3 ± 1.1* | 4.5 ± 1.1* | 1 / 20 |
| Asn/Asn | 28 ± 3 | 13.6 ± 1.2 | 10.1 ± 1.3 | 1344 ± 16*** | 3422 ± 484 | 3.5 ± 1.1* | 4.6 ± 0.4* | 0 / 14 |
| Poor responders (PR) | ||||||||
| Asn/Ser | 31 ± 3 | 5.5 ± 0.7*** | 3.8 ± 0.6*** | 595 ± 164 | 4873 ± 764 | 5 ± 0.8*** | 4 ± 0.6*** | 0 / 15 |
| Ser/Ser | 32 ± 2 | 8.0 ± 0.5*** | 7.8 ± 1.3*** | 557 ± 149 | 4720 ± 1009 | 5 ± 0.8*** | 4 ± 0.9*** | 0 / 10 |
| Asn/Asn | 34 ± 2 | 8.1 ± 0.5*** | 2.1 ± 0.5*** | 728 ± 294 | 3787 ± 968** | 3 ± 0.6*** | 2 ± 0.5*** | 1 / 10 |
| Good responders (GR) | ||||||||
| Asn/Ser | 28.3 ± 2.6 | 6.9 ± 0.8 | 4.6 ± 1.3*** | 4055 ± 1080*** | 1849 ± 218** | 11 ± 0.8*** | 10 ± 0.6*** | 3 / 24 |
| Ser/Ser | 28.8 ± 1.8 | 6.4 ± 1.4 | 7.4 ± 1.1*** | 2995 ± 130*** | 1858 ± 246** | 9 ± 0.7*** | 9 ± 0.7*** | 2 / 12 |
| Asn/Asn | 32.9 ± 2.4 | 7.5 ± 0.9 | 9.8 ± 1.6** | 1796 ± 406*** | 2322 ± 427** | 9 ± 0.6*** | 9 ± 0.7*** | 1 / 10 |
Note: Kruskal Wallis test for the analysis of variance.**p < 0.05;**p < 0.01;***p < 0.001
Follicles and oocytes collected from OD and GR patients with the Asn/Ser variant, significantly outnumbered those collected from patients with other allelic variants (p < 0.001). Furthermore, these oocytes appeared to provide better quality embryos, compared to the Ser/Ser subgroup. Therefore, oocyte production and quality appear to vary among patients with different genotypes. Pregnancies were distributed as follows: One in OD Ser/Ser, one in PR Asn/Asn, 3 in GR Asn/Ser, two in GR Ser/Ser and one in GR Asn/Asn (Table III). Pregnancy was defined by cardiac activity.
DISCUSSION
The distribution of several allelic variants of the FSHR gene in specific populations has been described in the past (15,30). The identification of these allelic variants has led to the investigation of their potential value as predictors of ovarian response to an exogenous stimulation IVF/ICSI protocol.
In this study, we examined the clinical parameters of 125 patients who participated in an IVF/ICSI/ET program and correlated the role of Asn680Ser polymorphism with these parameters, i.e., the outcome of ovulation induction, the number of oocytes, the quality of embryos and pregnancy rates. The pregnancy rates observed for these specific patients were lower than the expected pregnancy rates in our center (28). However, these were the observed pregnancy rates at that period of time and therefore results are interpreted accordingly. We observed that genotype distribution in 44 patients with ovarian dysfunction was 45.4% Ser/Ser, 22.7% Asn/Ser, and 31.8% Asn/Asn.
Our data show that patients with ovarian dysfunction tend to carry the Ser/Ser variant. However, this tendency did not prove to be statistically significant. Likewise, in other studies no specific allelic variant was found to be prominent (14,30). Furthermore, we report that GR patients have a statistically significant tendency to carry the Asn/Ser variant (p < 0.05). This finding may reflect a better and more rapid ovarian response to exogenous stimulation, possibly due to a more efficient FSH receptor. Thus, the allocation of a candidate for an IVF/ICSI program to the Asn/Ser allelic variant might predict a better response.
The levels of serum FSH reflect the ovarian response potential on the third day of the menstrual cycle, considering the existence of intra-individual variation from cycle to cycle and the different bioactivity of FSH measured (15,16). Indeed, we show here that the gonadotrophin dose required for ovulation induction significantly correlates with day 3 FSH levels. This correlation is stronger for specific genotype variant subgroups.
Our data show that day 3 FSH levels are statistically higher in Ser/Ser and Asn/Asn subgroups compared to Asn/Ser subgroup of patients. This variation may indicate a prompt response to FSH administration in the latter subgroup, with a consequent decrease in the basal levels of FSH. This finding is further supported by the observation that estrogen levels during hCG administration and the number of collected oocytes were significantly higher in the same subgroup (Asn/Ser). Similarly, other studies have suggested that ovarian response to rFSH may depend on the FSH receptor genotype of treated patients (14). Although peak E2 levels, number of preovulatory follicles and number of oocytes retrieved were similar in all allelic variants, Perez-Mayorga et al. reported increased basal serum FSH levels in the Ser/Ser subgroup, a finding which is in agreement with our present data (14).
In the same direction, Laven et al. reported increased median serum FSH levels in women with the Ser/Ser allelic variant. However, the ovarian response after ovulation induction was similar in all genotypes (30). In the previously refered study of Perez-Mayorga et al., the dose of rFSH needed for ovulation induction was higher in the Ser/Ser genotype variant. Similarly, our data show that OD patients with the Ser/Ser genotype variant required a significantly higher recombinant gonadotrophin dose.
CONCLUSIONS
In conclusion, our study shows that OD patients tend to carry the Ser/Ser allelic variant (44.5%), whereas GR patients carry more often the Asn/Ser allelic variant (p < 0.05). This latter genotype provides more follicles and oocytes in both GR and OD patients. Furthermore, our data suggest that the Asn/Ser genotype in the OD group has a higher FSH sensitivity compared to the other two groups, even though de Castro et al. suggest that the impact of the FSH receptor genotype may be limited (31). Clearly, the FSHR polymorphism assessment is still a research approach. Together with others, it could be evaluated in an effort to understand or even better predict the ovarian response of specific, very sensitive and difficult to treat, groups of patients. In no case does the present study suggest that it could replace traditional ovarian reserve testing. In the future, studies with numerous patients should be performed, in order to assess more effective individualized regimens for ovulation induction. An array of molecular tools will be needed and hundreds of thousands of polymorphisms will have to be examined in appropriate phenotypic groups, such as PR and OD patients.
REFERENCES
- 1.Gharib SD, Wierman ME, Shupnik MA, Chin WW. Molecular biology of pituitary gonadotrophins. Endocrinol Rev. 1990;11:177–199. doi: 10.1210/edrv-11-1-177. [DOI] [PubMed] [Google Scholar]
- 2.Moyle WR, Campbell RK. Gonadotrophins. In: Adashi EY, Rock JA, Rosenwalks Z, editors. Reproductive Endocrinology, Surgery and Technology. Philadelphia: Lippincott-Raven; 1996. pp. 683–724. [Google Scholar]
- 3.Patsoula E, Loutradis D, Drakakis P, Kallianidis K, Bletsa R, Michalas S. Expression of mRNA for the LH and FSH receptors in mouse oocytes and preimplantation embryos. Reproduction. 2001;121:455–461. doi: 10.1530/rep.0.1210455. [DOI] [PubMed] [Google Scholar]
- 4.Patsoula E, Loutradis D, Drakakis P, Michalas L, Bletsa R, Michalas S. mRNA expression for the follicle stimulating hormone receptor and luteinizing hormone receptor in human oocytes and preimplantation stage embryos. Fertil Steril. 2003;79:1187–1193. doi: 10.1016/S0015-0282(03)00071-2. [DOI] [PubMed] [Google Scholar]
- 5.Dufau ML. The luteinizing hormone receptor. Ann Rev Physiol. 1998;60:461–496. doi: 10.1146/annurev.physiol.60.1.461. [DOI] [PubMed] [Google Scholar]
- 6.Segaloff DL, Ascoli M. The lutropin/choriogonadotropin receptor… 4 years later. Endocrinol Rev. 1993;14:324–342. doi: 10.1210/er.14.3.324. [DOI] [PubMed] [Google Scholar]
- 7.Simoni M, Gromoll J, Nieschlag E. The follicle-stimulating hormone receptor: Biochemistry, molecular biology, physiology, and pathophysiology. Endocrinol Rev. 1997;18:739–773. doi: 10.1210/er.18.6.739. [DOI] [PubMed] [Google Scholar]
- 8.Minegishi T, Nakamura K, Takakura Y, Miyamoto K, Hasegawa Y, Ibuki Y, Igarashi M, Minegish T. Cloning and sequencing of human FSH receptor cDNA. Biochem Biophys Res Commun. 1991;173:1125–1130. doi: 10.1016/0006-291X(91)91682-3. [DOI] [PubMed] [Google Scholar]
- 9.Sprengel R, Braun T, Nicolics K, Segaloff DL, Seeburg PH. The testicular receptor for follicle-stimulating hormone: structure and functional expression of the cloned cDNA. Mol Endocrinol. 1990;4:525–530. doi: 10.1210/mend-4-4-525. [DOI] [PubMed] [Google Scholar]
- 10.Aittomaki K, Lucena JL, Pakarinen P, Sistonen P, Tapanainen J, Gromoll J, Kaskikari R, Sankila EM, Lehvaslaiho H, Engel AR, et al. Mutation in the follicle-stimulating hormone receptor gene causes hereditary hypergonadotropic ovarian failure. Cell. 1995;82:959–968. doi: 10.1016/0092-8674(95)90275-9. [DOI] [PubMed] [Google Scholar]
- 11.Aittomaki K, Herva R, Stenman UH, Juntunen K, Ylostalo P, Hovatta O, de la Chapelle A. Clinical features of primary ovarian failure caused by a point mutation in the follicle-stimulating hormone receptor gene. J Clin Endocrinol Metabol. 1996;81:3722–3726. doi: 10.1210/jc.81.10.3722. [DOI] [PubMed] [Google Scholar]
- 12.da Fonte Kohek MB, Batista MC, Russell AJ, Vass K, Giacaglia LR, Mendonca BB, Latronico AC. No evidence of the inactivating mutation (CS66T) in the follicle-stimulating hormone receptor gene in Brazilian women with premature ovarian failure. Fertil Steril. 1998;70:565–567. doi: 10.1016/S0015-0282(98)00203-9. [DOI] [PubMed] [Google Scholar]
- 13.Takakura K, Takebayashi K, Wang HQ, Kimura F, Kasahara K, Noda Y. Follicle-stimulating hormone receptor gene mutations are rare in Japanese women with premature ovarian failure and polycystic ovary syndrome. Fertil Steril. 2001;75:207–209. doi: 10.1016/S0015-0282(00)01673-3. [DOI] [PubMed] [Google Scholar]
- 14.Perez Mayorga M, Gromoll J, Behre HM, Gassner C, Nieschlag E, Simoni M. Ovarian response to Follicle-Stimulation Hormone (FSH). Stimulation depends on the FSH receptor genotype. J Clin Endocrinol Metabol. 2000;85:3365–3369. doi: 10.1210/jc.85.9.3365. [DOI] [PubMed] [Google Scholar]
- 15.Scott RT, Hofmann GF. Prognostic assessment of ovarian reserve. Fertil Steril. 1995;63:12–14. [PubMed] [Google Scholar]
- 16.Loutradis D, Elsheikh A, Kallianidis K, Drakakis P, Stefanidis K, Milingos S, Michalas S: Results of controlled ovarian stimulation for ART in poor responders according to the short protocol using different gonadotrophins combinations. Arch Gynecol Obstet 2003, (in press) [DOI] [PubMed]
- 17.Simoni M, Nieschlag E, Gromoll J. Isoforms and single nucleotide polymorphisms of the FSH receptors gene: Implications for human reproduction. Hum Reprod Update. 2002;8:413–421. doi: 10.1093/humupd/8.5.413. [DOI] [PubMed] [Google Scholar]
- 18.Sudo S, Kudo M, Wada S, Sato O, Hsueh AJ, Fujimoto S. Genetic and functional analyses of polymorphisms in the human FSH receptor gene. Mol Hum Reprod. 2002;8:893–899. doi: 10.1093/molehr/8.10.893. [DOI] [PubMed] [Google Scholar]
- 19.McLachlan RI, Robertson DM, Healy DL, de Kretser DM, Burger HG. Plasma inhibin levels during gonadotropin-induced ovarian hyperstimulation for IVF: A new index of follicular function? Lancet. 1986;31:1233–1234. doi: 10.1016/S0140-6736(86)91385-1. [DOI] [PubMed] [Google Scholar]
- 20.Scott RT, Navot D. Enhancement of ovarian responsiveness with microdoses of gonadotropin-releasing hormone agonist during ovulation induction for in vitro fertilization. Fertil Steril. 1994;61:880–885. doi: 10.1016/s0015-0282(16)56700-4. [DOI] [PubMed] [Google Scholar]
- 21.Surrey ES, Bower J, Hill DM, Ramsey J, Surrey MW. Clinical and endocrine effects of a microdose GnRH agonist flare regimen administered to poor responders who are undergoing in vitro fertilization. Fertil Steril. 1998;69:419–424. doi: 10.1016/S0015-0282(97)00575-X. [DOI] [PubMed] [Google Scholar]
- 22.Ben-Rafael Z, Feldberg D. The poor-responder patient in an in vitro fertilization-embryo transfer program. J Assist Reprod Genet. 1993;10:118–120. doi: 10.1007/BF01207732. [DOI] [PubMed] [Google Scholar]
- 23.de Koning CH, Popp-Snijders C, Schoemaker J, Lambalk CB. Elevated FSH concentrations in imminent ovarian failure are associated with higher FSH and LH pulse amplitude and response to GnRH. Hum Reprod. 2000;15:1452–1456. doi: 10.1093/humrep/15.7.1452. [DOI] [PubMed] [Google Scholar]
- 24.Jones GS, Muasher SJ, Rosenwaks Z, Acosta AA, Liu HC. The perimenopausal patient in in vitro fertilization: The use of gonadotropin-releasing hormone. Fertil Steril. 1986;46:885–891. doi: 10.1016/s0015-0282(16)49829-8. [DOI] [PubMed] [Google Scholar]
- 25.Cameron IT, O'Shea FC, Rolland JM, Hughes EG, de Kretser DM, Healy DL. Occult ovarian failure: A syndrome of infertility, regular menses, and elevated follicle-stimulating hormone concentrations. J Clin Endocrinol Metab. 1988;67:1190–1194. doi: 10.1210/jcem-67-6-1190. [DOI] [PubMed] [Google Scholar]
- 26.Buckler HM, Evans CA, Mamtora H, Burger HG, Anderson DC. Gonadotropin, steroid, and inhibin levels in women with incipient ovarian failure during anovulatory and ovulatory rebound cycles. J Clin Endocrinol Metab. 1991;72:116–124. doi: 10.1210/jcem-72-1-116. [DOI] [PubMed] [Google Scholar]
- 27.Drakakis P, Loutradis D, Kallianidis K, Bletsa R, Milingos S, Dionyssiou-Asteriou A, Michalas S. A comparative study of the effect of ovarian stimulation protocols with different gonadotropin preparations on the biological and clinical parameters of the outcome of intracytoplasmic sperm injection. Int Clin Exp Obstet Gynecol. 2002;4:286–289. [PubMed] [Google Scholar]
- 28.Loutradis D, Drakakis P, Kallianidis K, Milingos S, Dendrinos S, Michalas S. Oocyte morphology correlates with embryo quality and pregnancy rate after intracytoplasmic sperm injection. Fertil Steril. 1999;72:240–244. doi: 10.1016/S0015-0282(99)00233-2. [DOI] [PubMed] [Google Scholar]
- 29.Loutradis D, Drakakis P, Milingos S, Stefanidis K, Michalas S. Alternative approaches in the management of poor response in controlled ovarian hyperstimulation (COH) Ann NY Acad Sci. 2003;997:112–119. doi: 10.1196/annals.1290.013. [DOI] [PubMed] [Google Scholar]
- 30.Laven JS, Mulders AG, Suryandari DA, Gromoll J, Nieschlag E, Fauser BC, Simoni M. Follicle-stimulating hormone receptor polymorphisms in women with normogonadotropic anovulatory infertility. Fertil Steril. 2003;80:986–992. doi: 10.1016/S0015-0282(03)01115-4. [DOI] [PubMed] [Google Scholar]
- 31.de Castro F, Ruiz R, Montoro L, Perez-Hernandez D, Sanchez-Casas Padilla E, Real LM, Ruiz A. Role of follicle-stimulating hormone receptor Ser680Asn polymorphism in the efficacy of follicle-stimulating hormone. Fertil Steril. 2003;80:571–576. doi: 10.1016/S0015-0282(03)00795-7. [DOI] [PubMed] [Google Scholar]