Abstract
Purpose: To evaluate the role of 3-D US measurement of the endometrium during early IVF-pregnancy and before the appearance of gestational sac in the prediction of pregnancies outcome.
Methods: 60 pregnant women following IVF treatment were included in the study. The women underwent transvaginal 3D US measurements of endometrial volume and thickness on day 15–17 post ET. Patients were followed and classified according to pregnancy outcome into 2 further groups. The group with early pregnancy loss and the group with ongoing pregnancy.
Results: While no differences were observed between those who miscarried and those who did not in gestational age, endometrial thickness or volume, spontaneous early pregnancy loss was significantly higher in patients with endometrial volume <2 mL as compared to those with endometrial volume >2 mL.
Conclusions: 3-D US measurement of endometrial volume of less than 2 mL during early IVF pregnancy and prior to the appearance of gestational sac is a powerful predictor of pregnancy loss.
Keywords: Endometrial volume, 3-D ultrasonography, Prediction, Miscarriage, IVF
Serum hCG measurements [1, 2] and pelvic ultrasound (US) imaging [3] are part of the routine follow-up after in-vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI) treatments. While hCG measurements are reliable as early as 11 or 12 days after embryo transfer (ET), pelvic US may visualize a gestational sac as early as 1 week after missed menses, and specifically when serum hCG levels exceed 1000 mIU/mL [4]. Of the IVF pregnancies, 16.7% results in clinical pregnancy loss and 2.1% in ectopic pregnancy [5].
Jauniaux et al. recently reviewed the role of US imaging in diagnosing and investigating early pregnancy failure [6]. They concluded that no single US measurement of the different anatomical features in the first trimester has been shown to have a high predictive value for determining early pregnancy outcome, and especially before the visualization of gestational sac. Similarly, Doppler studies have failed to demonstrate abnormal blood flow indices in the first-trimester uteroplacental circulation of pregnancies that subsequently end in miscarriage [7].
The recent advent of computerized three-dimensional (3D) US systems has led to improvement in the quality and precision of ultrasonographic examination. Moreover, this tool allowed endometrial volume estimation with a high degree of reproducibility [8]. While, few studies have examined the role of 3-D endometrial volume on the day of hCG administration [9], oocyte pick-up (OPU) [10] or embryo transfer (ET) [11] in the prediction of IVF outcome, no study has assessed its role during early pregnancy.
We therefore aim to evaluate the role of 3-D US measurement of the endometrium during early IVF pregnancy and before the appearance of gestational sac in the prediction of pregnancy outcome.
Patients and methods
The study population included 60 infertile women who have been treated in our IVF unit and conceived. It is our unit policy to measure serum hCG on 13–14 days after ET (which is performed 3 or 2 days after oocytes retrieval, respectively). If the hCG result reveals a positive pregnancy test (serum hCG levels ≥10 IU/L) a second hCG measurement is performed 2–3 days later. On the day of their second serum hCG measurement, patients underwent transvaginal 3D US (VDW5-8B Probe, Volusone 530D MT, Medison-Kretz) measurements of endometrial volume and thickness.
Patients were followed and classified according to pregnancy outcome into 2 further groups. The group with early pregnancy loss (EPL-group) that included preclinical abortions (pregnancy detected by hCG measurements but no gestational sac seen on transvaginal ultrasonography), first-trimester abortions, and ectopic pregnancies. The group with ongoing pregnancy (OP-group), defined as progression to >12 weeks’ gestation.
The results are expressed as means and standard deviations. Receiver operating characteristic (ROC) curve analysis was used. It represents the probability of true positive results (sensitivity) as a function of the probability of false positive results (1-specificity). The statistical analysis was performed with Student’s t-test, chi square and Pearson correlations where appropriate. P<0.05 was considered significant.
Results
The clinical characteristics of the EPL and OP groups are shown in Table 1. There were no differences between the two groups in patients’ age, estradiol and progesterone levels on day of hCG administration, gestational age, serum hCG levels, endometrial thickness or volume. Moreover, no correlation was found between serum hCG levels and endometrial volume (r = 0.1).
Table 1.
Comparison between the group with early pregnancy loss (EPL-group) and that with ongoing pregnancy (OP-group)
| EPL-group | OP-group | p values | |
|---|---|---|---|
| Age (years) | 30.5 ± 5.9 | 30.7 ± 7.6 | ns |
| # of IVF cycle attempt | 3.4 + 2.9 | 2.6 + 2.2 | ns |
| Serum estradiol level on day of hCG administration (pg/mL) | 2042 + 1051 | 2156 + 1114 | ns |
| Serum progesterone level on day of hCG administration (ng/mL) | 0.81 + 0.42 | 0.88 + 0.69 | ns |
| Gestational age on day of 3-D US (days) | 30.5 ± 2.3 | 30.4 ± 1.6 | ns |
| HCG levels on day of 3-D US (IU/L) | 176 ± 148 | 371 ± 306 | ns |
| (range) | (24–550) | (54–977) | |
| 2-D US measurement of endometrial thickness (mm) | 10.7 ± 4.4 | 12.6 ± 4.5 | ns |
| 3-D US measurement of endometrial volume (mL) | 5.7 ± 5.6 | 8.0 ± 7.7 | ns |
Spontaneous early pregnancy loss was significantly higher in patients with endometrial volume <2 mL (7/9, 77.8%), as compared to those with >2 mL (15/51, 29.4%; p<0.02). The ROC analysis for endometrial volume is shown in Fig. 1. For the threshold of 2 mL, the sensitivity, specificity, positive and negative predictive values are 32%, 95%, 78% and 71% respectively.
Fig. 1.
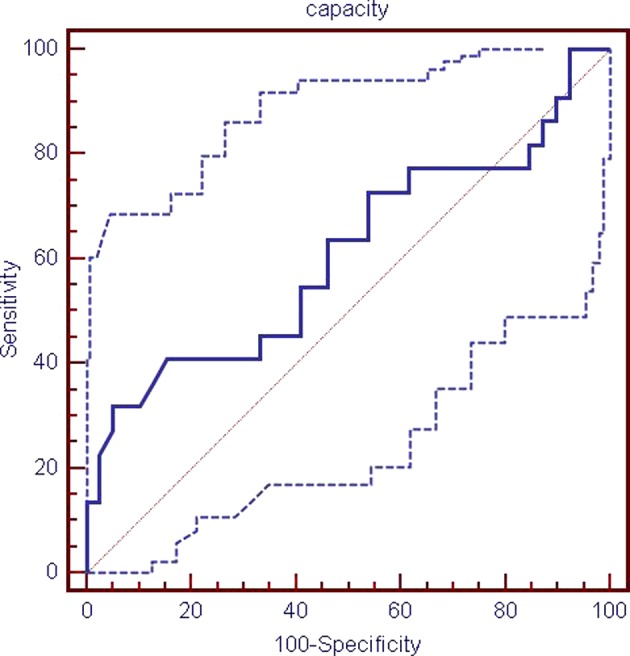
ROC curve for endometrial volume.
Discussion
To the best of our knowledge, this is the first report demonstrating that 3-D US measurement of endometrial volume of less than 2 mL during early IVF pregnancy and prior to the appearance of gestational sac is a powerful predictor of pregnancy loss.
The hitherto published studies dealt with the role of 3-D US measurement of endometrial volume in the prediction of endometrial receptivity. Yaman et al. performed 3-D US on the day of hCG administration, in an IVF-ET program [9]. They found that endometrial volume and thickness on the day of hCG administration did not predict occurrence of pregnancy. However, a minimum volume of 2.5 mL appeared to favor pregnancy.
In a prospective study, Raga et al. [11] reported a significantly lower pregnancy rate among IVF patients with endometrial volume <2.0 mL at day of ET. On the other hand, Schild et al. [10] failed to find any correlation between endometrial thickness or volume on day of OPU and pregnancy rate.
While the data from our and the aforementioned studies [9–11] on the role of 3D-US endometrial volume estimation in predicting IVF outcome, do not permit recommendation of a general concept, a minimum endometrial volume of about 2 mL appears to favor endometrial receptivity and ongoing early pregnancy.
Since endometrial volume measurement of <2 mL on day of positive hCG result is associated with high miscarriage rate, further studies are needed to evaluate the role of different pharmaceutical manipulation, such as hCG, progesterone, estrogen or aspirin, in preventing early pregnancy loss in this subgroup of patients.
References
- 1.Sugantha SE, Webster S, Sundar E, Lenton EA. Predictive value of plasma human chorionic gonadotrophin following assisted conception treatment. Hum Reprod. 2000;15:469–473. doi: 10.1093/humrep/15.2.469. [DOI] [PubMed] [Google Scholar]
- 2.Poikkeus P, Hiilesmaa V, Tiitinen A. Serum HCG 12 days after embryo transfer in predicting pregnancy outcome. Hum Reprod. 2002;17:1901–1905. doi: 10.1093/humrep/17.7.1901. [DOI] [PubMed] [Google Scholar]
- 3.Cacciatore B, Tiitinen A, Stenman UH, Ylostalo P. Normal early pregnancy: serum hCG levels and vaginal ultrasonography findings. Br J Obstet Gynaecol. 1990;97:899–903. [PubMed] [Google Scholar]
- 4.Williams Obstetrics. Cunningham EG, Leveno KJ, Bloom SL, Hauth JC, Gilstrap L, Wenstrom KD, editors 22nd ed. McGraw-Hill companies, Inc. 2005, p. 259.
- 5.SART/AMSR. Assisted reproductive technology in the United States: 2000 results generated from the American Society for Reproductive Medicine/Society for Assisted Reproductive Technology Registry. 2004;81:1207–20. [DOI] [PubMed]
- 6.Jauniaux E, Johns J, Burton GJ. The role of ultrasound imaging in diagnosing and investigating early pregnancy failure. Ultrasound Obstet Gynecol. 2005;25:613–24. doi: 10.1002/uog.1892. [DOI] [PubMed] [Google Scholar]
- 7.Frate MC, Doubilet PM, Brown DL, Benson CB, DiSalvo DN, Laing FC, Berck DJ, Hill JA. Role of Doppler ultrasonography in the prediction of pregnancy outcome in women with recurrent spontaneous abortion. J Ultrasound Med. 1996;15:557–62. doi: 10.7863/jum.1996.15.8.557. [DOI] [PubMed] [Google Scholar]
- 8.Kyei-Mensah A, Maconochie N, Zaidi J, Pittrof R, Campbell S, Tan SL. Transvaginal three dimensional ultrasound: Reproducibility of ovarian and endometrial volume measurements. Fertil Steril. 1996;66:718–722. doi: 10.1016/s0015-0282(16)58624-5. [DOI] [PubMed] [Google Scholar]
- 9.Yaman C, Ebner T, Sommergruber M, Polz W, Tews G. Role of three-dimensional ultrasonographic measurement of endometrium volume as a predictor of pregnancy outcome in an IVF-ET program: A preliminary study measurement. Fertil Steril. 2000;74:797–801. doi: 10.1016/S0015-0282(00)01493-X. [DOI] [PubMed] [Google Scholar]
- 10.Schild RL, Indefrei D, Eschweiler S, Van Der Ven H, Fimmers R, Hansmann M. Three dimensional endometrial volume calculation and pregnancy rate in an in-vitro fertilization program. Hum Reprod. 1999;14:1255–8. doi: 10.1093/humrep/14.5.1255. [DOI] [PubMed] [Google Scholar]
- 11.Raga F, Bonila-Musoles F, Casan EM, Klein O, Bonilla F. Assessment of endometrial volume by three-dimensional ultrasound prior to embryo transfer: Clues to endometrial receptivity. Hum Reprod. 1999;14:2851–4. doi: 10.1093/humrep/14.11.2851. [DOI] [PubMed] [Google Scholar]


