Abstract
Introduction: Air bubble location following embryo transfer (ET) is the presumable placement spot of embryos. The purpose of this study was to document endometrial air bubble position and migration following embryo transfer.
Design: Multicenter prospective case study.
Materials and Methods: Eighty-eight embryo transfers were performed under abdominal ultrasound guidance in two countries by two authors.(EC, FR) A single or double air bubble was loaded with the embryos using a soft, coaxial, end opened catheters. The embryos were slowly injected 10–20 mm from the fundus. Air bubble position was recorded immediately, 30 minutes later and when the patient stood up.
Results: Bubble marker location analysis revealed a random distribution without visible gravity effect when the patients stood up. The bubble markers demonstrated splitting, moving in all directions and dispersion.
Conclusion: Air bubbles move and split frequently post ET with the patient in the horizontal position, suggestive of active uterine contractions. Bubble migration analysis supports a rather random movement of the bubbles and possibly the embryos. Standing up changed somewhat bubble configuration and distribution in the uterine cavity. Gravity related bubble motion was uncommon, suggesting that horizontal rest post ET may not be necessary. This report challenges the common belief that a very accurate ultrasound guided embryo placement is mandatory. The very random bubble movement observed in this two-center study suggests that a large “window” of embryo placement maybe present.
Keywords: Air bubble migration, Embryo transfer
Introduction
Ultrasound guidance during embryo transfer has become more common in many IVF centers. It is widely accepted that ultrasound guided embryo transfer may improve clinical pregnancy rates in some IVF programs [1, 2]. Sonographic visualization of a marker air bubble loaded with the embryos in the transfer catheter allows visualization of initial placement of the embryos, assuming that the bubble represents the location of the embryos. Ultrasound tracking of the movement of air bubbles following embryo transfer concluded that very limited air bubble movement existed shortly following embryo transfer [3].
Ultrasound investigations of uterine contractility challenged the initial suggestion that air bubbles remain relatively stable following embryo transfer. Physiologic uterine contractility strongly suggested that bubble placement and location may change 30 minutes following embryo transfer [4]. If indeed uterine contractility changes the movement of embryos or disperses the marker bubble, the common belief that accurate placement of embryos is crucial for IVF success rates is challenged [5]. Analysis of bubble placement is further complicated by variations in the injection speed, the various amounts of fluid loaded into the transfer catheter, fundal proximity and different locations of the catheter tip within the uterine cavity, varying the speed of withdrawal of the transfer catheter, various duration of the procedure, and unrecognized trauma to the endometrium, possibly affecting uterine contractility, and subsequent bubble migration [7].
The purpose of this study was to prospectively evaluate initial marker placement inside the uterine cavity and tracking bubble position and configuration 30 minutes post embryo transfer and in a vertical position.
Materials and methods
Eighty-eight embryo transfers were performed under ultrasound guidance in Caracas, Venezuela and Chicago, Illinois USA by a single performer in each center. A single or double air bubble was loaded with the embryos using a soft coaxial end opened catheter. Tracking of the catheters was achieved with a semi full bladder and 3.5–5 MHz transabdominal ultrasound probe, used routinely for all transfers. The embryos were slowly injected 10–20 mm from the uterine fundus. Air bubble position was recorded immediately and 30 minutes later when the patient stood up. A final outcome parameter in this study was the 30 minute location and configuration of marker bubbles compared to their initial placement immediately following ET (Table 1). IRB was waived because all ET’s were routinely performed under ultrasound monitoring.
Table 1.
Air bubble marker movement immediately post ET and 30 minutes later in the upright position
| Bubble | Bubble | Patients | Patients |
|---|---|---|---|
| movement | splitting | horizontal | standing up |
| None | None | 10 | 12 |
| Random | None | 43 | 37 |
| Random | Double | 26 | 24 |
| All directions | Multiple | 5 | 8 |
| Undetectable | Dispersed | 4 | 4 |
| Cornual* (up) | None | 0 | 3 |
| *arcuate uteri | Total | 88 |
Results
The original intention to compare four quadrant bubble count following ET placement and 30 minutes post embryo transfer was canceled because of bubble splitting and inability to recognize and track individually every bubble. This unforeseen result made statistical comparison of bubble dynamics impossible to perform. Therefore, bubble tracking analysis was descriptive only.
The table depicts bubble movement including no bubble movement, and various degrees of bubble shifts inside the uterine cavity. Bubble movement was characterized as stationary, random or cornual. Bubble morphology movement was divided into splits, dispersion, and inability to detect the bubbles. This assessment was summarized in patients lying horizontally immediately following embryo transfer and standing up 30 minutes following embryo transfer. No bubble movement was detected in only 10/88 (11%) of patients immediately post ET (Table 1). In the standing position 12/88 (12%) of patients did not demonstrate bubble movement. A comparison of horizontal patients and standing patients reveals that there was significant movement of bubbles inside the uterine cavity over this period of time. The table demonstrates a random bubble splitting and movement over a 30 minute period of time following embryo transfer without any visible effect of gravity. Marker air bubbles split frequently post embryo transfer with the patient in the horizontal position.
Discussion
The purpose of this descriptive study was to illustrate air bubble migration patterns. Pregnancy outcome was not a target in this paper, and could not be reliably extracted from the data because of confounding variables. Previous reports suggest that air bubble placement in the transfer catheter does not impact pregnancy rates [7]. Nevertheless, the authors found air bubbles very useful as an imaging tool which allowed localization of the embryos. The presence of air bubbles next to embryos in the uterus does not cause embryo expulsion, studied during mock transfers using methylene blue marker [8]. A wide window of implantation with similar pregnancy rates was observed when the uterus was divided into upper and lower half cavities [9]. Additional support of this practice came from studies that demonstrated that 80% of embryo implantations occurred in the original area of transfer [10]. Even without unequivocal supporting evidence routine visualization of the marker bubble has become widely accepted.
US bubble tracking and US ET guidance requires an additional qualified sonographer during the embryo transfer, further encumbering the ET process and introducing yet another skill variable difficult to assess and monitor in different places and programs. The purpose of this two center observational study was to address this variation by an accumulation of similar data in two different countries, similar ultrasound and catheter equipment and minimal differences in air bubble loading technique. Multiple bubble splitting made numerical count of bubbles unreliable, therefore observational analysis focused on location and configuration of the bubbles. Data integration from two different centers validated the observations. One of the more striking observations in this series is that gravity did not affect bubble movement. Only in three arcuate uteri was bubble migration observed in the cornual area in the standing position. In the remaining patients the standing position did not affect bubble placement and location. If indeed bubble movements represent embryo migration inside the uterine cavity, the current recommendation to accurately place the embryos within an “implantation window” are challenged [11].
It is reasonable to assume that bubble movement somewhat simulates embryo movement, although the embryos are heavier and they have different surface tension. If this hypothesis is correct, the final implantation site of the embryos is highly dependent on random movement during the three days following embryo transfer. The only clearly undesirable embryo transfer location is injection of the embryos directly into the fallopian tubes, resulting in lower pregnancy success rates and higher ectopic pregnancy rates [12]. Routine U.S. guidance eliminates this complication. Additional events during embryo transfer resulting in lower pregnancy rates include unrecognized cervical placement of embryos or very low uterine segment placement resulting in an escape of embryos back into the cervical canal [13]. These undesirable events are prevented using routine US guidance. Therefore, this study does not imply that US guidance during ET is unnecessary.
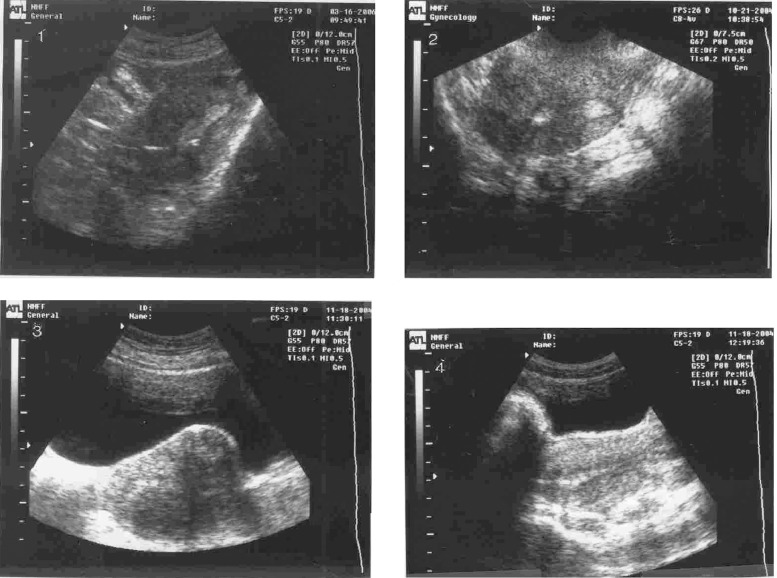
If indeed bubble movement is a random event controlled by uterine contractions, air bubble loading into the catheter may be unnecessary. Tracking the bubbles may be in fact noncontributory to improving IVF/ET success rates. Ultrasound tracking of the catheter tip will be sufficient to allow early recognition of misplaced embryo transfer catheters, folded catheters or embedded catheter tip into the fundal or cornual areas (Figs. 2–1). Elimination of real time ultrasound bubble tracking may simplify ET and allow a single operator U.S. guided ET.
Fig. 1.
(1) A single bubble in mid fundal placement. No movement detected, (2) A single bubble in standing position and an empty bladder, No movement detected, (3, 4) Two bubbles recorded 25 seconds apart changed their location
Fig. 2.
(1) The external catheter is embedded in posterior wall endometrium, (2) Right cornual migration of a bubble in a patient with an arcuate uterus, (3) One bubble split into three bubbles: a subserous anterior fibroid is visible, (4) A single bubble dispersed to several ones
References
- 1.Li R, Lu L, Hao G, Zhong K, Cai Z, Wang W. Abdominal ultrasound-guided embryo transfer improves clinical pregnancy rates after in vitro fertilization: experiences from 330 clinical investigations. J Assist Reprod Genet. 2005;22(1):3–8. doi: 10.1007/s10815-005-0813-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Coroleu B, Carreras O, Vieiga, et al. Embryo transfer under ultrasound guidance in post pregnancy rates after in vitro fertilization. Hum Reprod. 2000;215:616–620. doi: 10.1093/humrep/15.3.616. [DOI] [PubMed] [Google Scholar]
- 3.Woolcott R, Stanger J. Ultrasound tracking of the movement of embryo-associated air bubbles on standing after transfer. Hum Reprod 1998;(8):2107–9. [DOI] [PubMed]
- 4.Fanchin R, Righini C, Olivennes F, Taylor S, de Ziegler D, Frydman R. Uterine contractions at the time of embryo transfer alter pregnancy rates after in-vitro fertilization. Hum Reprod. 1998;13(7):1968–1974. doi: 10.1093/humrep/13.7.1968. [DOI] [PubMed] [Google Scholar]
- 5.Pope CS, Cook EK, Arny M, Novak A, Grow DR. Influence of embryo transfer depth on in vitro fertilization and embryo transfer outcomes. Fertil Steril. 2004;81(6):1723–1724. doi: 10.1016/j.fertnstert.2004.04.003. [DOI] [PubMed] [Google Scholar]
- 6.Karande VC, Morris R, Chapman C, Rinehart J, Gleicher N. Impact of the “physician factor” on pregnancy rates in a large assisted reproductive technology program: do too many cooks spoil the broth? Fertil Steril. 1999;71(6):998–1000. doi: 10.1016/S0015-0282(99)00139-9. [DOI] [PubMed] [Google Scholar]
- 7.Krampl E, Zegermacher G, et al. Air in the uterine cavity after embryo transfer. Fertil Steril. 1995;63(2):366–370. doi: 10.1016/s0015-0282(16)57370-1. [DOI] [PubMed] [Google Scholar]
- 8.Mansour RT, Aboulghar MA, et al. Dummy embryo transfer using methylene blue dye. Hum Reprod. 1994;9(7):1257–1259. doi: 10.1093/oxfordjournals.humrep.a138690. [DOI] [PubMed] [Google Scholar]
- 9.Franco JG, Martins AMVC, et al. Best site for embryo transfer: the upper or lower half of the endometrial cavity. Hum Reprod. 2004;19(8):1785–1790. doi: 10.1093/humrep/deh308. [DOI] [PubMed] [Google Scholar]
- 10.Baba K, Ishihara O, et al. Where does the embryo implant after transfer in humans? Fertil Steril. 2000;73(1):123–125. doi: 10.1016/S0015-0282(99)00454-9. [DOI] [PubMed] [Google Scholar]
- 11.Egbacpe-Al Sharhan M, Grudzinskas JG, et al. Entrance of the position length of the uterus on implantation and clinical pregnancy rates in IVF and embryo transfer treatment cycles. Hum Reprod. 2000;215:943–946. doi: 10.1093/humrep/15.9.1943. [DOI] [PubMed] [Google Scholar]
- 12.Frankfurter D, Trimarchi JB, Silver CP, Keith DL. Middle to lower uterine segment embryo transfer in post implantation and pregnancy rates compared with fundal embryo transfer. Fertil Steril. 2004;81(1):173–174. doi: 10.1016/j.fertnstert.2003.11.026. [DOI] [PubMed] [Google Scholar]
- 13.Lee HC, Seifer DB, Shelden RM. Impact of retained embryos on the outcome of assisted reproductive technologies. Fertil Steril. 2004;82(2):334–337. doi: 10.1016/j.fertnstert.2004.01.035. [DOI] [PubMed] [Google Scholar]