Abstract
Purpose
Fibroids may cause infertility and recurrent pregnancy loss. Studies have analysed the reproductive results after myomectomy according to the size, location and number of fibroids removed, but data are insufficient about comparison of opening the uterine cavity or not during surgery.
Materials and methods
Two hundred twenty-nine abdominal myomectomies with the indication of infertility and/or recurrent pregnancy loss were analysed retrospectively. The main purpose was to compare postoperative pregnancy, delivery and miscarriage rates according to either the uterine cavity was opened or not during the surgery. As a secondary outcome postoperative pregnancy rates were assessed by location, size and number of fibroids.
Results
There was no significant difference in reproductive results according to either the uterine cavity was opened or remained closed. Preoperative location, size and number of fibroids did not influence significantly the postoperative pregnancy rates.
Conclusion
Opening the uterine cavity does not impair postoperative pregnancy rates. Preoperative location, size and number of fibroids do not influence postoperative reproductive results.
Keywords: Abdominal myomectomy, Fibroid, Opened uterine cavity, Pregnancy rate
Introduction
Uterine fibroids are common in women of reproductive age. Reports of prevalence rates in literature range from 20 to 50% based on post mortem studies [1]. The influence of myomas on reproduction has been clearly demonstrated and the appearance of uterine fibroids has been linked to infertility. Fibroids were implicated as the sole factor of infertility in <10% of infertility cases and 43% of women presenting uterine leiomyomas were found to have experienced a history of infertility for at least 2 years [2]. Different theories have been proposed to explain the effects of fibroids on fertility. The type of the fibroid is an important factor, with submucosal, intramural and subserosal fibroids being in decreasing order of importance. Intramural and submucosal fibroids are thought to interfere with conception and reduce the effectiveness of assisted reproduction cycles [3]. Fibroids of >5 cm in diameter (size limit which appears to justify myomectomy) and those located near the cervix or near the tubal ostia are more likely to cause a problem. Those fibroids which are distorting the endometrial cavity may create an abnormal site for placental implantation and growth resulting impaired fertility and an increased risk of spontaneous abortions, preterm labor and delivery [4]. Uterine fibroids may cause implantation failure or gestation discontinuation due to focal endometrial vascular disturbance as well as endometrial inflammation, secretion of vasoactive substances or an enhanced endometrial androgen environment [5, 6]. Moreover submucosal or intramural fibroids may cause dysfunctional uterine contractility which may interfere with sperm migration, ovum transport or nidation [6–8].
Fibroids are also associated with miscarriage. The miscarriage rate is likely to be higher if implantation occurs over a submucosal fibroid or if the fibroid is close to the placenta [9]. The location of the fibroid in relation to the placenta appears to be more important than its size, as fibroids in close proximity to the placenta are more likely to cause early pregnancy bleeding and spontaneous miscarriage [10, 11].
Regarding the molecular mechanisms of infertility and pregnancy wastage several mechanisms have been suggested. In a study which examined the ultrastructure of the host myometrium of fibromyomatous uteri, the sarcolemmal dans bands of host myometrial myocytes were found to be of significantly greater length than that of normal myometria. A corresponding decrease in the number of caveolae was also found, making the host myometria structurally abnormal. These specific abnormalities may influence Ca2+ metabolism in these tissues, which may cause abnormal contractions leading to reproductive wastage or infertility [12].
It has been suggested that surgical management of fibroids improves fertility rates and reduces miscarriage rates, but the results of surgical intervention for each type of fibroids may vary.
It is well accepted that submucosal, intramural and subserosal fibroids are being in decreasing order of importance in causing infertility, however, the location of the fibroid does not appear to affect the pregnancy rate after surgery. A recent review of 27 studies by Vercellini et al. found no conclusive evidence whether the number, size or location of fibroids prior to myomectomy influenced postoperative pregnancy rates [13]. However there are evidences which suggest that pregnancy rates are significantly lower in women when multiple fibroids are removed [14].
Age was found to have a clinically significant impact on postoperative pregnancy rate, with a lower spontaneous or assisted conception pregnancy rate over 35 years [15, 16].
The purpose of our study was to assess reproductive outcome following abdominal myomectomy according to whether the uterine cavity was opened or not during the surgical procedure since literature data are insufficient in this regard. As a secondary endpoint we assessed postoperative reproductive outcomes by age, location, size and number of fibroids removed and compared our results with other studies.
Materials and methods
In a retrospective study we reviewed 423 abdominal myomectomies performed at the I. Department of Obstetrics and Gynecology, Semmelweis University, Budapest, Hungary, between January 1990 and December 2004. In these cases the removal of fibroids via laparotomy was the route of choice, because the patients had either large subserosal or intramural fibroids (>7 cm) or multiple fibroids (>3) were to be removed or entering the uterine cavity was expected. Patients’ age, indication for surgery, type, size, number of fibroids and entry into the uterine cavity during the procedure were recorded and analysed. From the 423 abdominal myomectomies the indication for myomectomy was infertility and/or recurrent pregnancy loss in 229 cases (54.1%). In this article we analyse the reproductive outcomes in these cases following abdominal myomectomy and try to determine the role of myomectomy in the treatment of infertility.
During the surgical procedure a vertical incision was performed on the uterus in order to avoid damaging the fallopian tubes and uterine arteries. In those cases where the myoma was located in a lateral position we preferred parallel incisions with the laterally running vessels. We minimized the number of serosal incisions and, if possible, enucleated more fibroids from a single incision. We performed the incision through the pseudocapsule of the fibroid with the aim not to lose valuable muscle tissue and to prevent bleeding.
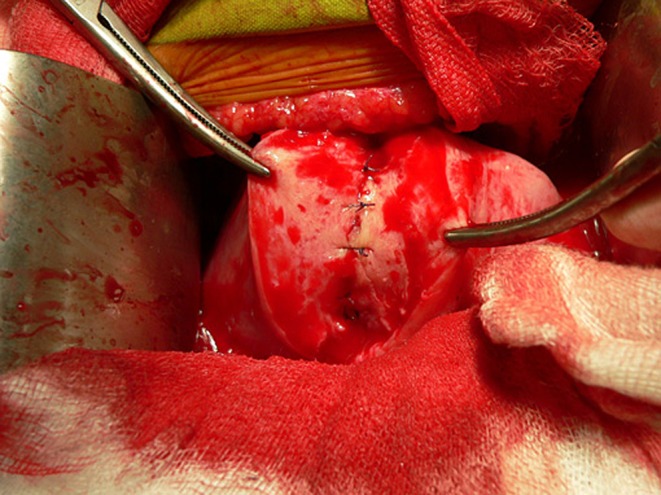
When the uterine cavity was opened during the procedure a special rain drop or tennis racket shaped drain with a cervical output was placed into the uterine cavity in order to avoid intrauterine adhesions as in the cases of metroplasty [17] (Figs. 1, 2, and 3). The endometrial cavity was closed by suturing the endometrial layer with single stitches over the drain in order to prevent its eversion (Fig. 4). The drain was removed 9 or 10 days postoperatively. When the uterine cavity was opened prophylactic antibiotics were administered.
Fig. 1.
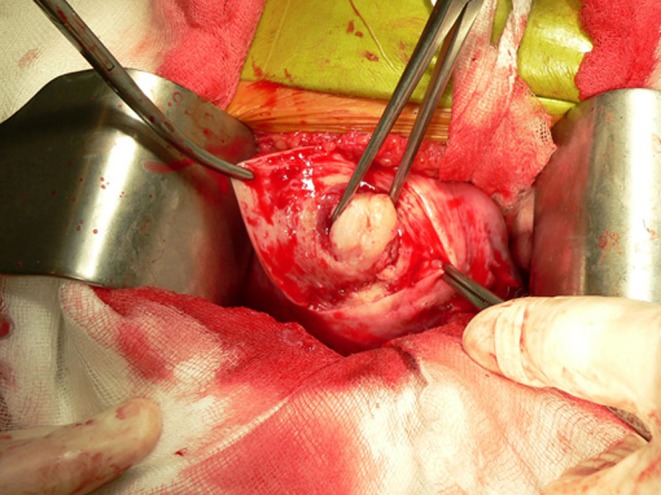
Enucleation of submucosal fibroid (angle 1)
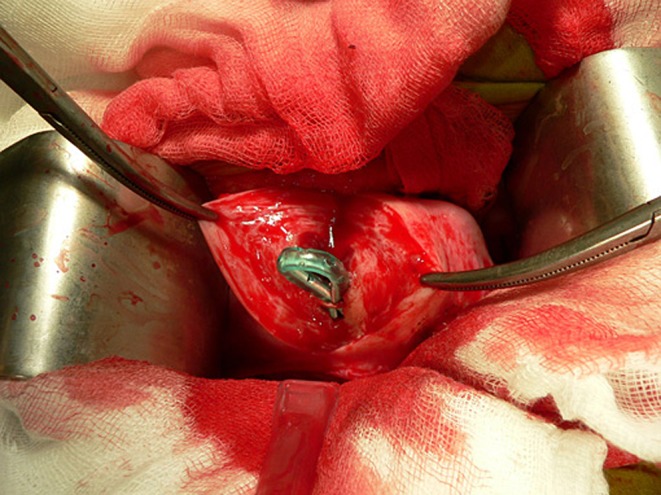
Fig. 2.

Opened uterine cavity after enucleation of submucosal fibroid (angle 2)
Fig. 3.
Insertion of a special rain drop or tennis racket shaped drain with a cervical output into the uterine cavity (angle 3)
Fig. 4.
Suturing the endometrial layer above the drain
The wound of removed fibroids was closed in two layers with 2-0 or 3-0 absorbable sutures. The outer layer was closed by using continous suture with the purpose to avoid postoperative adhesions (Fig. 5).
Fig. 5.

Suturing the outer layer of the myometrium with continuous stitches
The type, size, number of removed fibroids and the number of pregnancies conceived in 1 year after surgery, deliveries and spontaneous abortions were determined. In order to prevent complications during pregnancy and delivery due to thin scar tissue we recommended not achieving pregnancy postoperatively earlier than 6 month. Complications developed within 7–10 days after surgery were identified including necessity of pre- or postoperative transfusion, need for relaparotomy and frequency of postoperative febrile complications. Postoperative follow-up regarding reproductive outcomes was performed by sending out questionnaires.
Pregnancy, delivery and miscarriage rates as well as complication rates were compared between those cases where the uterine cavity was opened during the surgical procedure and those where the cavity remained closed. We also assessed reproductive outcomes after the surgical procedure according to age groups, type, size and number of removed fibroids and compared our results with other studies.
Statistical analyses were performed by Statistica Software (StatSoft Inc., Tulsa, OK). Student’s t test was used to compare mean values and the χ2 test for comparison of proportions. Statistical significance was set at P < 0.05.
Results—factors affecting reproductive outcome following abdominal myomectomy
Entering the uterine cavity during the surgical procedure
From the 229 abdominal myomectomies the uterine cavity was entered during the procedure in 47 (20.5%) cases and in 182 (79.5%) cases the uterine cavity remained closed.
The largest removed myoma from 229 abdominal myomectomies was subserosal in 91 cases, intramural in 152 cases, submucosal in 13 cases and intraligamental in three cases. Thirty patients had more than one type of fibroids in the uterus. In cases of subserosal and intramural fibroids the uterine cavity remained closed in a significantly higher percentage, whereas in cases of submucosal fibroids the uterine cavity was opened in a significantly higher percentage of the procedures. In all cases of intraligamental fibroids the uterine cavity remained closed.
We formed four groups according to the size of the largest removed fibroid (size of the dominant removed fibroid <30, 30–50, 50–70, and >70 mm) and compared the percentage of those cases where the uterine cavity was opened during the procedure or remained closed. None of the groups showed any significant difference in this regard.
Analyzing the complications we found that in the opened uterine cavity group significantly more patients needed postoperative blood transfusion due to intraoperative blood loss. No patient needed preoperative blood transfusion due to low hemoglobin levels in either group. The number of repeated laparotomies and the percentage of febrile complications did not differ between the compared groups. The number of treatment/ inpatient days was significantly higher in those cases where the uterine cavity was entered during the procedure.
There was no significant difference in the number of removed fibroids and patients’age between the opened and non-opened uterine cavity groups.
Analyzing the reproductive outcomes, we found no significant differences in pregnancy, delivery and miscarriage rates between the compared groups. The results are summarized in Tables 1 and 2.
Table 1.
Percentage of opened uterine cavity cases versus non-opened uterine cavity cases according to different factors
| No. of non-opened cases/total | Percent (%) | No. of opened cases/total | Percent (%) | P value | |
|---|---|---|---|---|---|
| Type | |||||
| Subserosal | 77/91 | 84.6 | 14/91 | 15.4 | 0.1178b |
| Intramural | 125/152 | 82.2 | 27/152 | 17.8 | 0.1461b |
| Submucosal | 4/13 | 30.8 | 9/13 | 69.2 | 0.00012c |
| Intraligamental | 3/3 | 100 | 0/3 | 0 | |
| Size | |||||
| <30 mm | 17/22 | 77.3 | 5/22 | 22.7 | 0.7878b |
| 30–50 mm | 74/88 | 84.1 | 14/88 | 15.9 | 0.1719b |
| 50–70 mm | 33/46 | 71.7 | 13/46 | 28.3 | 0.1461b |
| >70 mm | 58/73 | 79.5 | 15/73 | 20.5 | 0.9951b |
| Complications | |||||
| Postoperative transfusion | 10/182 | 54.9 | 11/47 | 23.4 | 0.00065c |
| Preoperative transfusion | 0 | 0 | 0 | 0 | 0 |
| Repeated laparotomy | 2/182 | 1.1 | 1/47 | 2.1 | 0.4997c |
| Fever | 11/182 | 6 | 2/47 | 4.2 | 0.4786c |
aStudent’s t-test, cPearson’s χ2-square, cFisher’s exact test, italics show significant differences
Table 2.
Mean age, number of removed fibroids, treatment days and pregnancy rate in cases of opened and non-opened uterine cavity
| Non opened cases | Opened cases | P value | |
|---|---|---|---|
| Age (mean) | 33.2 | 33.8 | 0.4798a |
| No. of removed myomas (mean) | 2.2 | 1.97 | 0.5350a |
| No. of treatment days (mean) | 6.8 | 9.5 | < 0.0001a |
| Pregnancy rate | 99/182 (54.4%) | 19/47 (40.4%) | 0.08756b |
| Delivery rate | 82/99 (82.8%) | 13/19 (68%) | 0.1464b |
| Miscarriage rate | 17/99 (17.2%) | 6/19 (37.6%) | 0.1464b |
aStudent’s t-test, bPearson’s χ2-square, cFisher’s exact test, italics show significant differences
Patients’ age
We found that age had a significant impact on pregnancy rate, with a lower pregnancy rate when the woman was over 40 years of age. Our results are in accordance with other studies which prove that those patients who conceive after surgery are significantly younger [15, 16, 18].
Location of fibroids
Most of the studies suggest that type of the fibroid and whether or not the uterine cavity is entered during the procedure does not appear to affect the pregnancy rate after the operation [14, 19–21]. We found no significant differences in pregnancy, delivery and miscarriage rates according to the type of removed fibroids. However our results suggest a trend towards lower postoperative pregnancy rates in cases of removal submucosal fibroids.
Our results also confirm that the pregnancy rate is not influenced by entering the uterine cavity.
Size of fibroid
Literature data are controversial regarding the reproductive outcomes according to the size of the fibroid prior to abdominal myomectomy. There are evidences that suggest that uterine size of >10 weeks prior to operation is associated with a poorer reproductive outcome after surgery [6] although one group suggests that the pregnancy rate after myomectomy for fibroids with a volume of >100 ml are significantly higher than those of smaller fibroids [14]. A recent review of 27 studies by Vercellini did not find any significant difference in postoperative pregnancy rates after the removal of different size fibroids [13]. Our results confirm the conclusion of Vercellini et al. as we also found no significant differences in postoperative pregnancy, delivery and miscarriage rates according to the size of the removed fibroids. However, in those cases where the size of the removed fibroid was <30 mm a trend towards higher pregnancy rates were observed.
Number of fibroids
Because of the increased number of incisions and subsequent adhesions some authors suggest that the pregnancy rate is significantly lower when more than five fibroids are removed [14, 19]. However, others noted no difference in pregnancy rate after myomectomy, irrespective of the size or number of fibroids removed [16, 20, 22]. We could also find no significant differences in postoperative pregnancy, delivery and miscarriage rates in this regard, but the results suggest that the pregnancy rate seems to decrease if the number of removed fibriods is seven or more.
The results of our study analyzed by different factors are summarized in Table 3.
Table 3.
Reproductive outcome after open myomectomy analyzed by different factors
| Pregnant n/total (%) | Non pregnant n/total (%) | Delivered n/total (%) | Miscarriage n/total (%) | |
|---|---|---|---|---|
| Age | ||||
| 20–25 | 9/9 (100%) | 0/9 | 8/9 (88.9%) | 1/9 (11.1%) |
| 26–30 | 37/58 (63.8%) | 21/58 (36.2%) | 29/37 (78.4%) | 8/37 (21.6%) |
| 31–35 | 48/88 (54.6%) | 40/88 (45.5%) | 43/48 (89.6) | 5/48 (10.4%) |
| 36–40 | 22/52 (42.3%) | 30/52 (57.7%) | 15/22 (68.2%) | 7/22 (31.8%) |
| over 40 | 2/22 (9.1%) | 20/22 (90.9%) | 0/2 (0%) | 2/2 (100%) |
| Type | ||||
| Subserosal | 48/91 (52.7%) | 43/91 (47.3%) | 39/48 (81.3%) | 9/48 (18.7%) |
| Intramural | 75/152 (49.3%) | 77/152 (50.7%) | 62/75 (82.7%) | 13/75 (17.3%) |
| Submucosal | 2/13 (15.4%) | 11/13 (84.6%) | 2/2 (100%) | 0/2 (0%) |
| Intraligamental | 2/3 (66.7%) | 1/3 (33.3%) | 2/2 (100%) | 0/2 (0%) |
| Size | ||||
| <30 mm | 13/22 (59.1%) | 9/22 (40.1%) | 9/13 (69.3%) | 4/13 (30.7%) |
| 30–50 mm | 42/88 (47.7%) | 46/88 (52.3%) | 34/42 (80.9%) | 8/42 (19.1%) |
| 50–70 mm | 26/46 (56.2%) | 20/46 (43.5%) | 19/26 (73.1%) | 7/26 (26.9%) |
| >70 mm | 37/73 (50.7%) | 36/73 (49.3%) | 33/37 (89.2%) | 4/37 (10.8%) |
| No. of removed fibroids | ||||
| 1–3 | 97/190 (51.1%) | 93/190 (48.9%) | 75/97 (77.3%) | 22/97 (22.7%) |
| 4–6 | 11/24 (45.9%) | 13/24 (54.1%) | 10/11 (90.9%) | 1/11 (9.1%) |
| 7 or more | 3/7 (42.9%) | 4/7 (57.1%) | 3/3 (100%) | 0/3 (0%) |
n: number of cases
Conclusions
The primary reason for performing myomectomy in patients of reproductive age is the preservation of the uterus for the purpose of child-bearing. Evidence suggests that most women who wish to conceive are able to do so in the first year, with pregnancy rates dropping significantly after this time. If possible therefore the surgery should be performed when a woman is ready to start a family. Data about the postoperative pregnancy rates in the literature vary between 9 and 76% depending on different types of fibroids [23]. A 49–60% average postoperative pregnancy rate is reported in women with myomas as a sole factor of infertility [14, 16, 19–22, 24–27]. Our patients beside the fibroids might have had other infertility factors and in their cases we could reach just with the removal of their fibroid 40–54% pregnancy rate.
A submucosal fibroid or an intramural fibroid distoring the uterine cavity, fibroids bigger than 5 cm and multiple fibroids are all indications for intervention in a woman considering pregnancy [9, 28]. Type, number and size of the fibroids may all influence the management option. Beside the well-accepted, overworld used abdominal myomectomy there are several treatment possibilities for fibroids linked to infertility.
Hysteroscopic myomectomy can be a safe and effective surgical procedure for the restoration of fertility. Compared with abdominal myomectomy hysteroscopic myomectomy is associated with a lower risk of scar rupture during the subsequent pregnancy as the scar tissue does not involve the whole thickness of the uterine wall. Avoiding pelvic adhesions with this procedure is also an advantage [9]. Pregnancy rates and live birth rates after hysteroscopic myomectomy reported by retrospective studies vary between 33–77 and 67–92%, respectively, [9, 29]. However there are limitations of this procedure such in cases of large type II. intramural fibroids open myomectomy may be preferable to hysteroscopic myomectomy.
As advances in surgical instruments and techniques are expanding laparoscopic myomectomy can also be the route of choice in cases of subserosal or intramural fibroids. Laparoscopic myomectomy provides a more rapid recovery compared to abdominal myomectomy and associated with less blood loss and fewer adhesions [4]. Pregnancy rates are comparable to those expected with abdominal myomectomy as the reported pregnancy rates in the literature vary between 11–75% [4, 30]. The risk of uterine rupture following appropriate suture of the uterine wall is less than 1% [4].
Uterine artery embolization (UAE) is also an option for women with symptomatic fibroids who are not candidates for surgery. Occluding the uterine arteries with a sclerosing substance causes fibroid infarction, eventually reducing the size by approximately 50% [31, 32]. Currently data are insufficient to determine whether can be UAE an option for women who wish to retain their fertility. UAE appears to increase the risk of preterm delivery, malpresentation, spontaneous abortions and postpartum haemorrhage compared to other surgical interventions [4, 33].
The safety of other treatment possibilities such as myolysis using electrical, thermal and ultrasound energy for women desiring pregnancy is unknown and need further studies to determine.
Finally we can conclude that abdominal myomectomy should be the route of choice when there are large subserosal or intramural fibroids (>7 cm), when multiple fibroids (>3) are to be removed or when entering the uterine cavity is to be expected.
In those cases where the uterine cavity is entered during the surgical procedure we recommend to place a tennis racket shaped drain into the uterine cavity in order to avoid postoperative intrauterine adhesions. It seems that entering the uterine cavity and suturing the endometrial layer does not prevent future pregnancies. The pregnancy rates are similar in those cases where the uterine cavity is opened or remains closed during the surgical intervention. Our results confirm the conclusions of major studies that reproductive outcomes are not influenced significantly by type, size and number of fibroids prior to surgical intervention.
Footnotes
Capsule Comparing postoperative pregnancy rates after abdominal myomectomy we found no significant difference according to either the uterine cavity was opened or remained closed during surgery.
References
- 1.Novak ER, Woodruff JD. Gynecologic and obstetrics pathology. 8. Philadelphia, USA: Saunders; 1979. Myoma and other benign tumors of the uterus; pp. 260–278. [Google Scholar]
- 2.Hasan F, Arumugam K, Sivanesaratnam V. Uterine leiomyomata in pregnancy. Int J Gynecol. 1990;34:45–48. doi: 10.1016/0020-7292(91)90537-F. [DOI] [PubMed] [Google Scholar]
- 3.Stovall DW, Parrish SB, Voorhis BJ, Hahn SJ, Sparks AE, Syrop CH. Uterine leiomyomas reduce the efficacy of assisted reproduction cycles: results of a matched follow-up study. Hum Reprod. 1998;13(1):192–197. doi: 10.1093/humrep/13.1.192. [DOI] [PubMed] [Google Scholar]
- 4.Hurst BS, Matthews ML, Marshburn PB. Laparoscopic myomectomy for symptomatic uterine myomas. Fertil Steril. 2005;83(1):1–23. doi: 10.1016/j.fertnstert.2004.09.011. [DOI] [PubMed] [Google Scholar]
- 5.Deligdish L, Loewenthal M. Endometrial changes associated with myomata of the uterus. J Clin Pathol. 1970;23(8):676–680. doi: 10.1136/jcp.23.8.676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Buttram VC, Jr, Reiter RC. Uterine leiomyomata: etiology, symptomatology and management. Fertil Steril. 1981;36:433–445. doi: 10.1016/s0015-0282(16)45789-4. [DOI] [PubMed] [Google Scholar]
- 7.Hunt JE, Wallach EE. Uterine factor in infertility: an overview. Clin Gynecol. 1974;17:44–64. doi: 10.1097/00003081-197412000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Vollenhoven BJ, Lawrence AS, Healy DL. Uterine fibroids: a clinical review. Br J Obstet Gynaecol. 1990;97(4):285–298. doi: 10.1111/j.1471-0528.1990.tb01804.x. [DOI] [PubMed] [Google Scholar]
- 9.Bajekal N, Li TC. Fibroids, infertility and pregnancy wastage. Hum Reprod Update. 2000;6:614–620. doi: 10.1093/humupd/6.6.614. [DOI] [PubMed] [Google Scholar]
- 10.Muram D, Gillieson M, Walter JH. Myomas of the uterus in pregnancy. Ultrasonographic follow up. Am J Obstet Gynecol. 1980;138:16–19. doi: 10.1016/0002-9378(80)90005-8. [DOI] [PubMed] [Google Scholar]
- 11.Rosati P, Bellati U, Exacoustos C, Angelozzi P, Mancuso S. Uterine myoma in pregnancy: ultrasound study. Int J Gynecol Obstet. 1989;28:109–17. doi: 10.1016/0020-7292(89)90469-4. [DOI] [PubMed] [Google Scholar]
- 12.Richards PA, Richards PD, Tiltman AJ. The ultrastructure of fibromyomatous myometrium and its relationship to infertility. Hum Reprod Update. 1998;4(5):520–525. doi: 10.1093/humupd/4.5.520. [DOI] [PubMed] [Google Scholar]
- 13.Vercellini P, Maddalena S, Giorgi O, Aimi G, Crosignani PG. Abdominal myomectomy for infertility: a comprehensive review. Hum Reprod. 1998;13:873–879. doi: 10.1093/humrep/13.4.873. [DOI] [PubMed] [Google Scholar]
- 14.Sudik R, Husch K, Steller J, Daume E. Fertility and pregnancy outcome after myomectomy in sterility patients. Eur J Obstet Gynecol Reprod Biol. 1996;65:209–214. doi: 10.1016/0301-2115(95)02363-1. [DOI] [PubMed] [Google Scholar]
- 15.Ramzy AM, Sattar M, Amin Y, Mansour RT, Serour GI, Aboulghar MA. Uterine myomata and outcome of assisted reproduction. Hum Reprod. 1998;13:198–202. doi: 10.1093/humrep/13.1.198. [DOI] [PubMed] [Google Scholar]
- 16.Li TC, Mortimer R, Cooke ID. Myomectomy: a retrospective study to examine reproductive performance before and after surgery. Hum Reprod. 1999;14:1735–1740. doi: 10.1093/humrep/14.7.1735. [DOI] [PubMed] [Google Scholar]
- 17.Papp Z. Abdominal metroplasty: 25 years experience. Orv Hetil. 2005;146(28):1471–1476. [PubMed] [Google Scholar]
- 18.Campo S, Campo V, Gambadauro P. Reproductive outcome before and after laparoscopic or abdominal myomectomy for subserous or intramural myomas. Eur J Obstet Gynecol Reprod Biol. 2003;110(2):215–219. doi: 10.1016/S0301-2115(03)00159-3. [DOI] [PubMed] [Google Scholar]
- 19.Berkeley AS, DeCherney AH, Polan ML. Abdominal myomectomy and subsequent fertility. Surg Gynaecol Obstet. 1983;156:319–322. [PubMed] [Google Scholar]
- 20.Rosenfield DL. Abdominal myomectmy for oherwise unexplained infertility. Fertil Steril. 1986;46:328–330. doi: 10.1016/s0015-0282(16)49536-1. [DOI] [PubMed] [Google Scholar]
- 21.Acien P, Quereda F. Abdominal myomectomy: results of a simple operative technique. Fertil Steril. 1996;65:41–51. doi: 10.1016/s0015-0282(16)58025-x. [DOI] [PubMed] [Google Scholar]
- 22.Vercellini P, Maddalena S, Giorgi O, Pesole A, Ferrari L, Crosignani PG. Determinants of reproductive outcome after abdominal myomectomy for infertility. Fertil Steril. 1999;72:109–114. doi: 10.1016/S0015-0282(99)00200-9. [DOI] [PubMed] [Google Scholar]
- 23.Poncelet C, Benifla JL, Batalian A, Darai E, Madelanat P. Myoma and infertility: analysis of the literature. Gynecol Obstet Fertil. 2002;29(6):450–451. doi: 10.1016/s1297-9589(01)00154-0. [DOI] [PubMed] [Google Scholar]
- 24.Garcia CR, Tureck RW. Submucosal leiomyomas and infertility. Fertil Steril. 1984;42:16–19. doi: 10.1016/s0015-0282(16)47951-3. [DOI] [PubMed] [Google Scholar]
- 25.Smith DC, Uhlir JK. Myomectomy as a reproductice procedure. Am J Obstet Gynecol. 1990;162:1476–1482. doi: 10.1016/0002-9378(90)90909-q. [DOI] [PubMed] [Google Scholar]
- 26.Verkauf BS. Myomectomy for fertility enhancement and preservation. Fertil Steril. 1992;58:1–15. doi: 10.1016/s0015-0282(16)55128-0. [DOI] [PubMed] [Google Scholar]
- 27.Gehlabch DL, Sousa RC, Carpenter SE, Rock JA. Abdominal myomectomy in the treatement of infertility. Int J Gynecol Obstet. 1993;40:45–50. doi: 10.1016/0020-7292(93)90771-N. [DOI] [PubMed] [Google Scholar]
- 28.Kolankaya A, Arici A. Myomas and assisted reproductive technologies: when and how to act? Obstet Gynecol Clin North Am. 2006;33(1):145–152. doi: 10.1016/j.ogc.2005.12.008. [DOI] [PubMed] [Google Scholar]
- 29.Sanders B. Uterine factors and infertility. J Reprod Med. 2006;51(3):169–176. [PubMed] [Google Scholar]
- 30.Griffiths A, D’Angelo A, Amso N. Surgical treatment of fibroids for subfertility. Cochrane Database Syst Rev. 2006;19(3):CD003857. doi: 10.1002/14651858.CD003857.pub2. [DOI] [PubMed] [Google Scholar]
- 31.Lumsden MA. Embolization versus myomectomy versus hysterectomy: which is the best, when? Hum Reprod. 2002;17(2):253–259. doi: 10.1093/humrep/17.2.253. [DOI] [PubMed] [Google Scholar]
- 32.Ravina JH, Herbreteau D, Ciraru-Vigneron N, Bouret JM, Houdart E, Aymard A, et al. Arterial embolisation to treat uterine myomata. Lancet. 1995;9(346):671–672. doi: 10.1016/S0140-6736(95)92282-2. [DOI] [PubMed] [Google Scholar]
- 33.Domenico L, Jr, Siskin GP. Uterine artery embolization and infertility. Tech Vasc Interv Radiol. 2006;9(1):7–11. doi: 10.1053/j.tvir.2006.08.003. [DOI] [PubMed] [Google Scholar]


