Abstract
Objective
The majority of participants drop out of pediatric obesity treatment programs; however, clinicians have little knowledge of how to address this problem. The objective of this study was to explore obesity treatment clinicians’ perceptions of contributors to attrition, as well as methods to maintain family participation.
Methods
Semi-structured interviews were conducted with 29 pediatric obesity clinicians representing primary care (PC), community-based (CB), and tertiary-care (TC) treatment programs in North Carolina. Interviews were recorded, transcribed verbatim, and coded using a multistage inductive approach. Grounded theory was used to analyze responses.
Results
Eleven themes emerged from analysis, including: the influence of program elements, family characteristics, and the variety of approaches employed to address retention. Only TC programs reported attempts to address attrition. Patients’ past experiences with obesity treatment, desire for immediate outcomes, and relationships with clinicians were perceived as important factors related to attrition. Other important themes were: families’ understanding of obesity treatment; importance of realistic expectations; and families’ value of treatment. Important differences and similarities among programs were identified. All clinicians reported families came to treatment through physician-, not self-referral.
Conclusions
Clinicians perceive attrition to be a significant problem in pediatric obesity treatment. As a result of clinical interviews, several potential avenues to address attrition were identified, including: the need for clinicians to develop relationships with families, assist in building appropriate expectations, and address families’ value of treatment. Findings of this study can inform larger investigations of attrition, and guide exploration of family impressions of and experiences in treatment.
Keywords: Obesity, attrition, treatment, qualitative
Pediatric obesity remains a significant threat to children’s health, resulting in detrimental co-morbidities1, 2, decreased life expectancy3, 4, and increased health care expenditures 5, 6. The US Preventive Services Task Force endorsed comprehensive behavioral interventions for obesity treatment in children and adolescents 7. Many children’s hospitals offer such services 8, 9 in accordance with standard pediatric obesity treatment recommendations 10, utilizing multidisciplinary approaches that often require resources not covered by insurance 11. Costs of such care are either charged to families or absorbed by sponsoring hospital systems. Attrition from treatment increases overall expense, as missed appointments and drop-outs decrease productivity of treatment professionals, and lead to an inefficient use of resources. More importantly, children who drop out of treatment are unlikely to see beneficial change in their health trajectory, and may not attempt treatment again if they have a sense of failure in weight loss.
A review of attrition from pediatric weight management found 27 to 73% of participants dropped out of treatment 12. Patient factors appear to contribute, as children who are severely obese, older, racial/ethnic minorities, or living in poverty exhibit higher attrition 12, 13. Though these studies elucidate who is at risk for attrition, a look beyond patient factors is still needed. Adherence researchers advocate for a focus on disease and treatment characteristics that may influence families’ decisions to adhere to clinical programs 14. This notion is underscored by expert recommendations for obesity treatment 10, which highlight the health care system’s role in delivering high-quality care via the Chronic Care Model 15. In an effort to improve the quality of health care, assessing the attitudes of those delivering treatment could prove beneficial. Clinician’s perception of their patients impacts both the quality of care delivered and outcomes achieved, which has been investigated in adult obesity literature16, but has not been explored in pediatric settings. Discerning attitudes and perceptions of obesity treatment clinicians may be valuable for improving treatment and outcomes, and in conjunction with approaches known to be effective in clinical trials, this type of inquiry may be a useful first step for addressing attrition.
In surveying children’s hospitals, Hampl et al sought to establish recommendations for improved practice by identifying patient-retention efforts of pediatric weight management programs17; however, there are significant limitations in this report. Study participants were identified as primary directors of treatment programs, or “program champions,” which did not capture the perspectives of all clinicians working in weight management clinics. Additionally, the study surveyed only programs within children’s hospitals, typically representative of higher intensity or tertiary-care treatments. Previous studies have focused on general pediatric practitioners, rather than those with extensive experience in pediatric obesity 18, 19. The 2007 Expert Recommendations for the treatment of pediatric obesity outline a staged-approach to treatment, progressing from primary-care settings to community-based and tertiary-care programs 10, 20. To our knowledge, there have been no studies of such community-based or primary care practices and their approaches to manage attrition. Although structural components such as scheduling and communication with families were identified in Hampl’s study, specifics of treatment approaches and their contribution to attrition and retention were not.
Given the relative nascency and diversity of pediatric obesity treatment programs, exploratory studies are needed to understand approaches to reduce attrition and improve retention. Large gaps exist in our understanding of attrition. For that reason, we have employed a qualitative approach to allow in-depth exploration of beliefs and values directly from those involved (clinicians), and provide guidance to future studies21, 22. Theoretical frameworks can assist in bridging these gaps by guiding the study design, data collection, analysis, and interpretation 23, and were instrumental in this research.
Study Objective
The objective of this study was to investigate attitudes and beliefs of pediatric obesity treatment clinicians, identifying perceived contributors to attrition and methods employed to maintain patient participation. Through in-depth phone interviews with clinicians, we sought to gain a deeper understanding of approaches to pediatric obesity treatment and broaden the scope of inquiry into attrition. We incorporated the perspectives of obesity treatment clinicians from primary care, community-based, and tertiary-care treatment settings in order to compare, contrast, and verify findings from differing sources. This approach, called qualitative triangulation24, will expand the perspective of this research, as obesity treatment occurs in a number of diverse settings, and methodologies are likely to vary.
METHODS
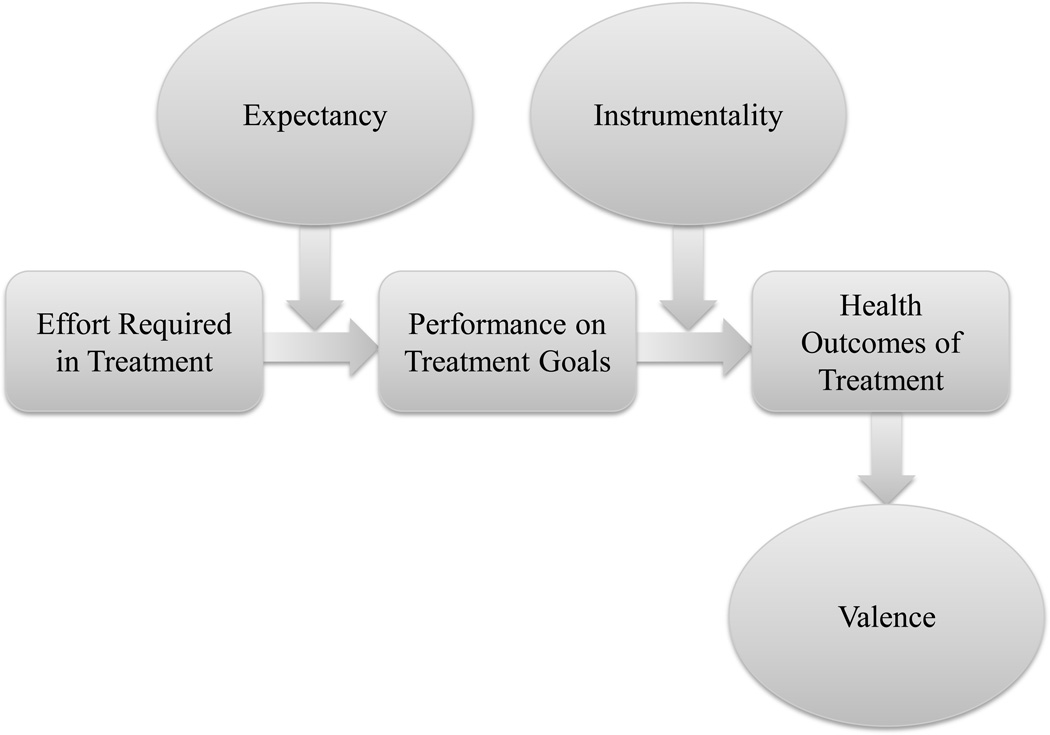
A conceptual model was developed in accordance with Expectancy Theory of Motivation (ETM) (Figure 1) 25, 26, which was instrumental in research methodology, developing interview questions, and analysis.
Figure 1. Application of Expectancy Theory to Pediatric Obesity Treatment Outcomes.
Adapted from:
Vroom VH, Jago AG. On the validity of the Vroom-Yetton model. Journal of Applied Psychology. 1978, 63: 151–162.
Expectancy Theory of Motivation
Conceptualized to explain processes of decision-making in management 27, ETM posits that individuals engage in behaviors based on expected outcomes of those behaviors and how greatly the expected outcomes are desired. ETM identifies motivation as a driving force in the relationship between effort, goals, and outcomes (Figure 1) 28. Motivation governs this process, and is a function of three variables: expectancy (increased effort will lead to increased performance), instrumentality (increased performance will yield valued outcome), and valence (value, importance placed on expected outcome). The amount of effort exerted influences performance, which affects the actual outcome achieved. Though not previously applied to pediatric obesity treatment, various studies have implicated motivation as a significant intervening variable in health behavior change 29, weight control 30, and adolescents’ ability to exert personal agency over their risk for obesity 31. Thus, we hypothesized that patient motivation in pediatric obesity treatment may be a determinant of retention, attrition, and health outcomes as perceived by clinicians.
Interview Guide
In-depth interview guides were developed based on our conceptual model (Table 1). Interviews contained 20 open-ended questions, which were reviewed for face-validity by various clinicians experienced in obesity treatment, and tested in cognitive interviews with obesity treatment clinicians external to the study. Interviews were semi-structured to allow staff to probe for detail, provide clarification, and allow new areas of inquiry to emerge; highly structured interviews may otherwise be too restrictive 32. Interviews also included a demographic questionnaire to assess providers’ role, amount of specialized training, time commitment, years of practice in obesity treatment, and characteristics of their treatment programs.
Table 1.
Semi-structured interview guide, mapped by domain, with sample items
| Semi-Structured Interview Guide | |
|---|---|
| Treatment Structure | Tell me more about your program/clinic. To help participants stay in your program and be successful, what changes would you make in your program? What skills or characteristics do staff and clinicians in your program need to effectively treat participants? If you could design the ideal pediatric weight management program, what would it look like? |
| Participant Population | Tell me about the children and families you see in your program. |
| Attrition from Treatment | Tell me about participants missing or canceling appointments. Why do you think participants miss or cancel appointments? Regarding participants that drop out, what contributes to them dropping out? |
| Expectancy | Describe to me what you do to prepare participants for your program. How do your patients define success in treatment? How does your program and program staff define success? When participants begin your program, how confident are they that they will be successful? What must participants do to be successful in your program? What does it mean for you to be successful in your job as a obesity treatment provider? |
| Instrumentality | How do participants? efforts relate to their performance in treatment? How do you help participants choose realistic, maintainable goals? How do participants perceive your efforts as a treatment provider? How are your efforts reflected in the success of participants? |
| Valence | How well do participants value their treatment? Are your efforts as a treatment provider worthwhile? |
Study Sites and Participants
Obesity treatment clinicians were recruited from a convenience sample of pediatric programs and clinics in North Carolina with the goal of having representation across the obesity treatment spectrum: primary care (PC), community-based (CB), and tertiary-care pediatric centers (TC). As qualitative research is geared towards obtaining a variety of responses and respondents, all clinicians working within a treatment program were targeted for recruitment (dietitians, exercise specialists, counselors, physicians, etc.). Via formal (university research collaborative) and informal networks (prior collaborations, familiarity), nine pediatric obesity treatment programs were identified. All programs served a racially/ethnically diverse populace and provided care to both rural and urban populations. When invited to participate, one community-based program did not return contacts, and another declined participation. Two programs from each level of care agreed to participate (six total). To keep equal representation of programs at each level (Table 2), a seventh program that had been identified (a tertiary-care center), was not asked to participate. Participants were included if they were English-speaking and had worked as a treatment provider in pediatric obesity in the past year. All obesity treatment clinicians within each program were contacted by study staff by phone and email and invited to participate. Participants who expressed interest were scheduled for a telephone call to provide consent. Verbal consent was obtained by study staff, and two copies of the consent form were mailed to the participant to be reviewed and signed, and one of the forms returned to study staff. All participants returned signed consent forms.
Table 2.
Participating Obesity Treatment Programs located in North Carolina and Composition of Participants
| Level of Treatment | Program | Staff |
|---|---|---|
| Primary Care | Private Pediatric Practice | MD, RD |
| Multi-specialty Pediatric Practice, Federally Qualified Health Center (look-alike status) | MD, RD (counselor services available) | |
| Community-Based | Group program held at YMCA | MD, C, ES, RN |
| Group program held at YMCA | RN, C, RD | |
| Tertiary Care | Multidisciplinary clinic | MD, RD, PhD, RN, PT, SW |
| Multidisciplinary clinic | MD, RD, PT, ES, C, SW |
MD- Pediatric Physician or Secondary Provider (Physician.s Assistant)
RD- Registered Dietitian or Nutritionist
RN- Nurse
PT- Physical Therapist
ES- Exercise Specialist
PhD- Psychologist (Clinical psychologist, Medical Family Therapy)
C- Counselor (clinical social worker, marriage and family therapist, licensed practical counselor)
SW- Social Worker
Data Collection
Study staff completed intensive training in qualitative interviewing by senior investigators (BMB, SDR), using the interview guide. Interviews were conducted by telephone and digitally recorded using USB Blast™ telephone audio-recording technology, and ranged from 30–90 minutes in duration. Study protocols, interview questions, and consent procedures were approved by the Wake Forest School of Medicine Health Institutional Review Board #00012961.
Data Analysis
Digital interview recordings were transcribed verbatim into Microsoft Word (Microsoft Corporation, Redmond, WA). Although ETM was used to frame the interview guide, grounded theory, an inductive approach to data analysis, was used to analyze responses. This approach focused on gathering knowledge across a wide array of experiences in order to build understanding grounded in real-world patterns 33. To minimize bias, two investigators (JAS, MBI) completed a multistage inductive interpretative thematic process by separately reviewing transcripts to identify potential codes. Investigators then created a common coding system and data dictionary, and separately assigned agreed-upon codes to relevant text. Initial codes were modified as needed, and notable quotes were included. Coding discrepancies were resolved by a third investigator (SDR), and were then compiled to compare broad categories from which to develop and interpret themes. Ongoing comparisons and revisions were continued throughout this iterative process and during analysis.
Results
Sample
A total of 35 pediatric obesity treatment clinicians were eligible from the six programs who participated; 29 clinicians consented and completed interviews. Interviews were conducted with six PC, nine CB, and fourteen TC clinicians. Participants were predominantly white females (Table 3); 34% worked full time in pediatric obesity (40+ hours per week), and 58% worked less than 20 hours a week in their programs. The majority (57%) reported to have worked in pediatric obesity five years or less. Nearly all had additional training in obesity, mostly through specialized conferences, continuing education, self-directed study, or observation.
Table 3.
Select Participant Characteristics
| N= 29 |
|---|
| Mean age ± SD |
| 38 years ± 8.9 (Range 24–56) |
| Caucasian, % |
| 93% |
| Female, % |
| 90% |
| Years experience in obesity treatment |
| 4.3 years ± 2.9 (Range 0.5–10) |
| Hours employed in obesity treatment, % |
| Full-time, 34% |
| Mean hours/week in obesity treatment |
| 22 hours ± 15 (Range 2–60) |
| Completed graduate degree, % |
| 66% |
| Clinician Type (n) |
| Physician (6) |
| Physician.s Assistant (1) |
| Social Worker (1) |
| Counselor or Psychologist (7) |
| Physical Therapist (1) |
| Dietitian/Nutritionist (9) |
| Health Educator (2) |
| Nurse (1) |
| Program Administrator (1) |
Themes
Three general themes emerged: attrition, motivation, and the elements of ETM (effort, expectations, and values). Themes, subthemes, and illustrative quotations from the interviews are provided in Table 4, and further delineated in the following paragraphs:
Table 4.
Themes
| Themes | Sub-themes | Quotations |
|---|---|---|
| Attrition | Program elements influence adherence | “We have a hard time keeping families engaged for 12 weeks.” “Having other families [in treatment], being able to hear the struggles of other people; [families] realize they are not alone in the challenges they face.” “The biggest challenge has always been trying to figure out the right time to have the program because you have a mixture of working parents and non-working parents.” “Participants come back to a place where they feel comfortable, this is the place where they come see their doctor, and this is the exact same place where they are going come for [obesity treatment].” |
| Family characteristics influence adherence | “Lower socioeconomic status brings a lot of challenges; a family living in poverty has a lot of barriers.” “Most of our families are pretty stressed in general, but some of them let that stress overwhelm them and that’s why they drop out.” “Transportation is usually hard for them; they worry about paying bills and just getting through the week. Thinking about nutrition and activities on top of that is a challenge.” |
|
| Clinicians employ different approaches to address attrition | ”The clinic that has the best show rate [does] reminder calls two days in advance…and extends the ‘no-show fee’ policy to patients. They request that if [the family is] not going to come for an appointment, that they call and cancel within a decent amount of time. If they don’t show, there is a $35 fee; they also have a ‘two no-show and you’re out’ policy.” | |
| Motivation | Past experiences with treatment influences motivation | “Many families have gone to a physician or a nutritionist and have been told negative things, so it sets them up to not want to come back onto medical grounds; they don’t want to be judged again.” “[Families] are very hopeful that they will benefit from the program…They are hopeful that they will finish the program and will make changes...it just depends on how much failure they had in the past or how much they struggled before.” “Patients say they have seen a nutritionist before, and say they didn’t help or made them feel bad about themselves.” |
| Desire for immediate outcomes affects motivation e.g., weight loss | “Lack of motivation and feeling they are never going to get better, is probably more of a contributor to dropout.” “Patients get discouraged if they don’t lose as much weight right off the bat…they get more frustrated and drop out at that point.” |
|
| Relationships and communication influence motivation | “The patients that can actually see a difference when we weigh them, that increases their motivation to change.” “We gauge motivation by really talking to families and seeing their level of concern. If both the parent and child have no desire to change, it really makes the process hard to make changes.” “[Families] become more motivated when they are in a group of their peers who are also struggling their weight, and we see the feelings of isolation start to wane.” |
|
| Incentives are used to increase motivation | “We offer a lot of different activities so [families] can find something that they like and might continue.” “We provide incentives when they bring back a goal calendar; something that shows what they did for the month.” |
|
| Effort, Expectations, Performance, and Values | Preparing families for participation varies by program | “They don’t get a lot of information [before coming to the program] other than what we verbally tell them, or sometimes they will get a handout about nutrition prior to coming.” “There is a lot of education upfront about what the program is and is not; it is not a weight loss program.” “Before they start we have an information night, where they can come learn about the program and [the clinicians].” |
| Families do not understand obesity treatment | “We try to get [families] to understand that a knowledge change happens first and behavior change will happen next.” “The [family] mindset is that if they didn’t lose pounds on the scale, then [treatment] didn’t work.” “Weight loss is good, and getting children to a healthier weight is important to me, but it’s really about the family and child understanding that a healthier lifestyle is important.” |
|
| Realistic expectations can be developed | “In younger children...they might have gained a few pounds, but they grew. Showing them the BMI chart, their weight hasn’t gone down, but they have actually thinned out. That helps them to see it in a different perspective. They get excited to see that success.” “[Families] expect weight loss. They might define it differently [after being in the program]; they might be satisfied with improved labs, but most families still want to see some visible change…to see the numbers go down on the scale and see their body change; they want their clothes to fit differently.” “The ones who stay in the program realize our expectations and realize that we don’t want them to lose a ton of weight.” “If they don’t see the progress they want to see as quickly as they want to see it, they will stop coming to the program.” |
|
| Family value of treatment influences outcomes and attrition | “Not putting importance on treatment is another reason [families miss appointments].” “Families who don’t take [treatment] as serious as others don’t tend to do as well, and don’t tend to [reach goals] because they are not putting forth the efforts to actually [make a goal become] a habit.” |
Attrition
All participants perceived attrition to be a problem in their programs, though only one program actively tracked attrition. Other programs were unable to quantify attrition or missed appointments.
Program elements influence adherence
PC clinicians felt families were more comfortable in familiar settings like their primary care office, whereas TC clinicians felt that their treatment locations (hospital settings) were an impediment to family participation. CB clinicians perceived group settings supported families, particularly since children could be among their peers; CB programs served more narrow age-ranges to ensure age-appropriate group activities. PC and TC clinicians indicated greater difficulty scheduling patients, as appointments were conducted individually and families expressly preferred appointments that would not conflict with school or work schedules. CB clinicians reported school and work schedules were not significant barriers to attendance, as their regular weekly meetings were held in the evenings. However, CB clinicians indicated that the group structure complicated participation if families had inconsistent and busy evening schedules.
Family characteristics influence adherence
All clinicians perceived family characteristics and demographics influenced attrition, specifically the at-risk nature of families: severe obesity, multiple obese family members, low socioeconomic status, racial/ethnic minorities, highly stressed, family finances, transportation, and school and work schedules. PC and TC clinicians felt parenting and a lack of community resources (e.g., activity opportunities, nutrition resources, parenting support, mental health resources) were barriers to retention, whereas CB clinicians focused on issues of family attendance, lack of commitment, and whether families made use of resources provided (e.g., free gym memberships, exercise opportunities).
Clinicians employ different approaches to address attrition
TC programs focused on improving attrition through program evaluation and modification, and felt relationships between families and staff were the most important determinant of family engagement. PC and TC clinicians felt that missed appointments, leading to longer periods between visits, resulted in lost momentum. Therefore, there were policies to terminate family participation if they missed two or more visits, and families were strongly encouraged to reschedule canceled appointments at the time of the cancellation. Respondents said these policies decreased wasted time and resources, and motivated families to attend or reschedule visits as promptly as possible. Because their programs were short term (e.g., 12 weeks), CB clinicians focused on maintaining family motivation by providing various entertaining activities, as well as providing incentives. Overall, CB clinicians did not specifically address missed visits through personal contacts, unlike clinicians from PC and TC programs.
Motivation
Clinicians identified motivation to participate in treatment as a complex issue related to attrition. All clinicians focused greatly on gauging motivation to participate, and various approaches were employed to build motivation through relationships, communication, and incentives. Clinicians consistently perceived low motivation as a contributor to attrition, as well as a general lack of value for the treatment. Interestingly, clinicians noted that nearly all families enrolled in their treatment program by referral from a physician, not on their own volition. The implications of such non-intrinsic motivation on families’ continued participation was never discussed by participants in this study.
Past experience with treatment influences motivation
Clinicians reported that families’ previous attempts at weight management influenced their motivation to participate in their current programs, noting that previous negative experiences lowered the patient’s motivation to participate in new treatments. CB clinicians believed that prior unsuccessful attempts at weight loss damaged children’s confidence and decreased motivation to begin another program. All clinicians remarked parents seemed to have greater confidence than their children.
Desire for immediate outcomes affects motivation
Clinicians felt that families lost motivation when children were not successful in losing substantial amounts of weight. Conversely, CB clinicians believed children’s successful weight loss to be a motivating factor within and between families, and felt it important to share personal weight-loss stories in attempts to enhance motivation.
Relationships and communication influence motivation
TC clinicians felt strong relationships with families were important, allowing them to be more attuned to individual stressors affecting family participation. CB clinicians worked very little with families individually, and focused on teaching and activity; these clinicians felt that interacting in a group provided support. Most clinicians specified that use of Motivational Interviewing, providing patient-centered care, and continued follow-up with goals were core components of their programs with implications for retention.
Incentives are used to increase motivation
CB clinicians detailed programmatic attempts to maintain motivation, including: fun and engaging curricula, free gym memberships, and incentives for weight loss. Of note, CB programs rewarded children with certificates for losing certain amounts of weight, as measured during weekly meetings. Such practices were not mentioned or advised by PC and TC clinicians.
Effort, Expectations, Performance and Values
The components of ETM coalesced into a single theme related to attrition, of which four subthemes emerged.
Preparing families for participation varies by program
PC clinicians offered very little preparation to families prior to the first treatment visit. CB programs offered families informational sessions, and one program employed techniques to build interest in the program through sharing clinicians’ personal weight loss stories. TC clinicians varied in their approaches, offering personal contacts through telephone calls, emails, or intensive coaching by telephone. Overall, CB and TC clinicians felt they invested significant energy in preparing families for treatment and building appropriate expectations, aiding retention and success.
Families do not understand obesity treatment
Clinicians felt families struggled with understanding the treatment process, particularly the focus on family habits, behavior change, and tracking nutrition and activity. PC and TC clinicians belived it important that families understand obesity treatment, but this was not mentioned in CB programs. Consistently in all programs, clinicians felt families focused on weight loss as the primary outcome measure of success.
Realistic expectations can be developed
All clinicians noted the importance of setting realistic goals, particularly in PC and TC programs. However, many clinicians believed unrealistic expectations for weight loss led to disappointment. Nearly all clinicians discussed their work in building appropriate expectations and the challenges of not seeing immediate results. TC clinicians expressed that unrealistic expectations were not unique to just patients, as referring physicians often held unrealistic expectations for their patient’s weight loss.
CB clinicians consistently mentioned that brief programs prevented families from seeing success, placing emphasis on behavioral modification in terms of success. However, they continued to weigh children regularly, sometimes weekly. Incentives were also offered for losing set amounts of weight, despite an expressed belief that families should not be “weight-focused.”
Value of treatment
All participating clinicians perceived that families readily dropped out if they did not value obesity treatment, particularly if the child did not have a weight-related health problem. Families who were seeking a ‘magic bullet’ typically left treatment unsatisfied, as clinicians noted that families feel programs are not working if weight is not lost.
DISCUSSION
This is the first study to investigate perceptions of pediatric obesity clinicians to better understand attrition, all of whom recognized it as a significant problem. Utilizing an in-depth qualitative approach, the findings revealed several key areas that clinicians believe influence attrition from pediatric obesity treatment. Clinicians recognized family characteristics (highly stressed, poor) and aspects of their treatment programs (scheduling, location) may contribute to attrition. There were themes of past experiences with treatment, family desire for immediate outcomes, and clinician-family relationships that influenced families’ motivation. Interestingly, many clinicians felt parents had greater confidence than their children. An unexpected finding was families rarely sought treatment on their own. This could be important since Motivational Interviewing34, 35(used in all six participating programs) requires treatment to be patient-centered as a means to build motivation for change. If children and families are not actively seeking treatment, it may take time to prepare families or explore ambivalence regarding behavior change. However, clinicians interviewed did not comment on this or discuss possible implications.
The triangulation process, engaging the different levels of obesity treatment, yielded important similarities and differences. PC and TC clinicians had many similar perceptions, primarily the importance of relationships and communication in treatment, which they felt helped families manage barriers and modify goals. CB programs focused largely on engaging families through enjoyable curricula and incentives. Through the analysis process, it became apparent that CB clinicians may be sending contradictory messages about behavior change and reasonable expectations by sharing dramatic weight loss stories with families, frequently weighing children, and rewarding weight loss. This is interesting, given that all clinicians, including those in CB programs, stated outcomes should focus on health and habits rather than “a number on the scale.” CB and TC programs were similar in they focused heavily on preparing families for treatment, whereas PC programs had no pre-treatment orientation or preparation. With varying levels of obesity treatment, outlined in the 2007 expert recommendations, more research is needed in this area to confirm these findings and explore further.
There are several implications that can be drawn from this study. Across diverse treatment settings, attrition is recognized as a problem with multiple potential contributors: location; family barriers such as poverty and stress; scheduling and timing of programs; unrealistic expectations; and lack of family motivation. Though all programs recognized similar contributors, only TC programs aggressively addressed them, presumably because of their location within academic medical centers and better access to clinical resources. Unrealistic expectations and understanding treatment are potentially important areas to concentrate in order to improve attrition. Clinicians focused on these concepts and indicated efforts to address them, but were still seen as a problem. Despite clinicians’ best efforts, alternative approaches to building expectations may be needed to better address attrition resulting from errant expectations, as present activities may not be effective. Another potential area of future inquiry and investigation is the perception that parents have greater confidence than their children. In a family-based program, effort towards building motivation, confidence, and appropriate expectations may need to be directed towards the child as well as the parent. Previous research indicates children influence a family’s decision to drop out of treatment13, 36, thus, inclusion of the child’s perspective could hold promise when determining how to address attrition.
Greater focus on these and other processes would be useful to improve obesity interventions, as they may help lower attrition rates and increase patient success in reaching goals. For instance, CB clinicians felt strongly that there are positive interactions when families receive treatment in group settings. PC and TC clinicians could enhance their treatments to provide families with more opportunities for social interaction, which has shown promise in prior research 37. Conversely, PC and TC programs felt that building relationships with children and families improves retention. Thus, CB clinicians could potentially improve their approaches by facilitating relationship building with staff and participating families, another concept proven effective 38. Finally, it is likely families who enroll in treatment solely based on physician referral may not desire weight management or be fully prepared to participate in treatment. For some families, encouragement by a physician or the opportunity to engage a needed resource could spur them to behavior change. For others, though, that may not be enough, nor be the right time. This could explain difficulties with motivation, unrealistic expectations, and under-valuing treatment (Table 4). Changing the process by which families are referred, enrolled, or prepared for treatment may potentially improve attrition and outcomes.
There are several limitations to this study. Foremost, this is a qualitative study, reporting perceptions of clinicians from a single state (North Carolina), and not participating children and families. This may not be representative of all approaches to treatment, programs in other locations, or of other patient populations. However, the study explicitly sought to collect a broad range of perspectives on attrition from various levels of treatment and clinicians. PC programs included in this study are unique: one is a large general pediatric practice that has developed a “program within a practice” with a dedicated physician and dietitian; the other program resembles a federally-qualified health center (does not receive government funding, but serves primarily a Medicaid population) and has resources not readily available to typical pediatric practices (dietitian). Therefore, this study did not engage primary care pediatricians attempting weight management in their office without other resources.
There are several avenues found in this study to explore further, both in research and clinically: the impact of preparing families for the treatment process; evaluating the effectiveness of incentives; and the value families place on treatment, in light of other life stressors. PC and TC clinicians felt strongly that developing open and trusting relationships with families may facilitate this process, as patients could be more likely to tell clinicians about barriers to treatment adherence. All clinicians perceived that families’ inaccurate expectations of treatment contributed to attrition, and reported attempts to build appropriate expectations. Treatment programs can “borrow” from each other as well: clinic-based programs could add more group programming to encourage social support, and CB programs could focus more on relationships with families in an effort to decrease attrition.
Attrition is recognized as a significant problem in pediatric obesity treatment. Clinicians that participated in this study represent the spectrum of obesity care providers, and all recognized drop out as a complicating factor in their treatment efforts. The findings of this qualitative study provide further avenues to investigate this problem: realistic expectations, importance of relationships with families, and addressing how families value treatment. This study can guide future qualitative and quantitative studies of obesity treatment programs, as a larger study of treatment programs can inform best practices. In particular, clinicians’ perceptions can assist in capturing the perceptions and experience of children and families participating in weight management programs, and has the potential to improve care and outcomes. Clinicians working in pediatric obesity can consider the experience and perceptions of the clinicians included in this study as they plan and modify their own family-based treatment programs, particularly when addressing the problem of attrition.
What’s New.
Perceptions of attrition from pediatric obesity treatment differ depending on the level of care. Increased focus on clinician-family relationships, family expectations, and factors associated with motivation, including how families are referred to treatment, are potential avenues to address attrition.
Acknowledgements
The authors would like to thank Karen Klein (Research Support Core, Office of Research, Wake Forest School of Medicine) for her assistance in editing this manuscript; and Camila Pulgar, B.S. for her assistance in the conduct of this study.
Funding sources: Dr. Skelton was supported in part through NICHD/NIH Mentored Patient-Oriented Research Career Development Award (K23 HD061597). Additional support was provided by the Kate B. Reynolds Charitable Trust Grant #2009-098 (MBI).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest: No other financial disclosures were reported by the authors of this paper.
References
- 1.Krebs NF, Himes JH, Jacobson D, Nicklas TA, Guilday P, Styne D. Assessment of child and adolescent overweight and obesity. Pediatrics. 2007 Dec;120(Suppl 4):S193–S228. doi: 10.1542/peds.2007-2329D. [DOI] [PubMed] [Google Scholar]
- 2.Jacobson MS. Medical Complications and Comorbidities of Pediatric Obesity. In: Sothern MS, Gordon ST, Von Almen TK, editors. Handbook of Pediatric Obesity: Clinical Management. Boca Raton: CRC Taylor and Francis; 2006. pp. 31–40. [Google Scholar]
- 3.Olshansky SJ, Passaro DJ, Hershow RC, et al. A potential decline in life expectancy in the United States in the 21st century. N Engl J Med. 2005 Mar 17;352(11):1138–1145. doi: 10.1056/NEJMsr043743. [DOI] [PubMed] [Google Scholar]
- 4.Franks PW, Hanson RL, Knowler WC, Sievers ML, Bennett PH, Looker HC. Childhood obesity, other cardiovascular risk factors, and premature death. N Engl J Med. 2010 Feb 11;362(6):485–493. doi: 10.1056/NEJMoa0904130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hampl SE, Carroll CA, Simon SD, Sharma V. Resource utilization and expenditures for overweight and obese children. Arch Pediatr Adolesc Med. 2007 Jan;161(1):11–14. doi: 10.1001/archpedi.161.1.11. [DOI] [PubMed] [Google Scholar]
- 6.Cawley J. The economics of childhood obesity. Health Aff (Millwood) 2010 Mar-Apr;29(3):364–371. doi: 10.1377/hlthaff.2009.0721. [DOI] [PubMed] [Google Scholar]
- 7.Whitlock EP, O'Connor EA, Williams SB, Beil TL, Lutz KW. Effectiveness of Weight Management Interventions in Children: A Targeted Systematic Review for the USPSTF. Pediatrics. 2010 Jan 25; doi: 10.1542/peds.2009-1955. [DOI] [PubMed] [Google Scholar]
- 8.Young KL, Demeule M, Stuhlsatz K, et al. Identification and treatment of obesity as a standard of care for all patients in children's hospitals. Pediatrics. 2011 Sep;128(Suppl 2):S47–S50. doi: 10.1542/peds.2011-0480C. [DOI] [PubMed] [Google Scholar]
- 9.Eneli IU, Patel D, Cunningham A, Hinton T, Stephens J, Murray R. Pediatric Academic Societies. Honolulu, Hawaii: 2008. A Comrehensive Survey of U.S. Pediatric Obesity Programs. [Google Scholar]
- 10.Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007 Dec;120(Suppl 4):S164–S192. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 11.Story MT, Neumark-Stzainer DR, Sherwood NE, et al. Management of child and adolescent obesity: attitudes, barriers, skills, and training needs among health care professionals. Pediatrics. 2002 Jul;110(1 Pt 2):210–214. [PubMed] [Google Scholar]
- 12.Skelton JA, Beech BM. Attrition in paediatric weight management: a review of the literature and new directions. Obesity Reviews. 2011 May;12(5):e273–e281. doi: 10.1111/j.1467-789X.2010.00803.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Skelton JA, Goff D, Ip E, Beech BM. Attrition in a Multidisciplinary Pediatric Weight Management Clinic. Childhood Obesity. 2011;7(3):185–196. doi: 10.1089/chi.2011.0010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rapoff MA. Adherence to Pediatric Medical Regimens. Second Edition. New York: Springer; 2010. [Google Scholar]
- 15.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness: the chronic care model, Part 2. JAMA. 2002 Oct 16;288(15):1909–1914. doi: 10.1001/jama.288.15.1909. [DOI] [PubMed] [Google Scholar]
- 16.Puhl RM, Heuer CA. The stigma of obesity: a review and update. Obesity (Silver Spring) 2009 May;17(5):941–964. doi: 10.1038/oby.2008.636. [DOI] [PubMed] [Google Scholar]
- 17.Hampl S, Paves H, Laubscher K, Eneli I. Patient engagement and attrition in pediatric obesity clinics and programs: results and recommendations. Pediatrics. 2011 Sep;128(Suppl 2)(2011):S59–S64. doi: 10.1542/peds.2011-0480E. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barlow SE, Dietz WH. Management of child and adolescent obesity: summary and recommendations based on reports from pediatricians, pediatric nurse practitioners, and registered dietitians. Pediatrics. 2002 Jul;110(1 Pt 2):236–238. [PubMed] [Google Scholar]
- 19.Barlow SE, Trowbridge FL, Klish WJ, Dietz WH. Treatment of child and adolescent obesity: reports from pediatricians, pediatric nurse practitioners, and registered dietitians. Pediatrics. 2002 Jul;110(1 Pt 2):229–235. [PubMed] [Google Scholar]
- 20.Spear BA, Barlow SE, Ervin C, et al. Recommendations for treatment of child and adolescent overweight and obesity. Pediatrics. 2007 Dec;120(Suppl 4):S254–S288. doi: 10.1542/peds.2007-2329F. [DOI] [PubMed] [Google Scholar]
- 21.Berkwits M, Inui TS. Making use of qualitative research techniques. J Gen Intern Med. 1998 Mar;13(3):195–199. doi: 10.1046/j.1525-1497.1998.00054.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Berkwits M. In defense of qualitative research: responses to the Poses and Isen perspectives article. J Gen Intern Med. 1998 Jan;13(1):66–67. author reply 69–72. [PubMed] [Google Scholar]
- 23.Alderson P. The importance of theories in health care. BMJ. 1998 Oct 10;317(7164):1007–1010. doi: 10.1136/bmj.317.7164.1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wolcott H. Ethnographic research in education. In: Jaegger R, editor. Complementary methods for research in art education. Washington, D.C.: American Education Research Association; 1988. pp. 187–206. [Google Scholar]
- 25.Jones BT, Corbin W, Fromme K. A review of expectancy theory and alcohol consumption. Addiction. 2001 Jan;96(1):57–72. doi: 10.1046/j.1360-0443.2001.961575.x. [DOI] [PubMed] [Google Scholar]
- 26.Vroom VH, Jago AG. On the validity of the Vroom-Yetton Model. Journal of Applied Psychology. 1978;63:151–162. [Google Scholar]
- 27.Vroom VH. Work and Motivation. New York: Wiley; 1964. [Google Scholar]
- 28.Klein HJ. Further evidence on the relationship between goal setting and expectancy theories. Organizational Behavior and Human Decision Processes. 1991;49:230–257. [Google Scholar]
- 29.Kelly RB, Zyzanski SJ, Alemagno SA. Prediction of motivation and behavior change following health promotion: role of health beliefs, social support, and self-efficacy. Soc Sci Med. 1991;32(3):311–320. doi: 10.1016/0277-9536(91)90109-p. [DOI] [PubMed] [Google Scholar]
- 30.Stotland S, Larocque M, Sadikaj G. Positive and negative dimensions of weight control motivation. Eating Behaviors. 2011 doi: 10.1016/j.eatbeh.2011.10.003. [DOI] [PubMed] [Google Scholar]
- 31.Contento IR, Koch PA, Lee H, Calabrese-Barton A. Adolescents demonstrate improvement in obesity risk behaviors after completion of choice, control & change, a curriculum addressing personal agency and autonomous motivation. J Am Diet Assoc. Dec;110(12):1830–1839. doi: 10.1016/j.jada.2010.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Alasuutari P. An invitation to social research. Vol 143–145. London: Sage; 1998. [Google Scholar]
- 33.Charmaz K. Constructing Grounded Theory: A Practical Guide Through Qualitative Analysis. Los Angeles: Sage; 2009. [Google Scholar]
- 34.Miller WR, Rollnick S. Motivational Interviewing: Preparing People for Change. New York, NY: Guilford Press; 2002. [Google Scholar]
- 35.Schwartz RP, Hamre R, Dietz WH, et al. Office-based motivational interviewing to prevent childhood obesity: a feasibility study. Arch Pediatr Adolesc Med. 2007 May;161(5):495–501. doi: 10.1001/archpedi.161.5.495. [DOI] [PubMed] [Google Scholar]
- 36.Barlow SE, Ohlemeyer CL. Parent reasons for nonreturn to a pediatric weight management program. Clin Pediatr (Phila) 2006 May;45(4):355–360. doi: 10.1177/000992280604500408. [DOI] [PubMed] [Google Scholar]
- 37.Kalavainen MP, Korppi MO, Nuutinen OM. Clinical efficacy of group-based treatment for childhood obesity compared with routinely given individual counseling. Int J Obes (Lond) 2007 Oct;31(10):1500–1508. doi: 10.1038/sj.ijo.0803628. [DOI] [PubMed] [Google Scholar]
- 38.Ahmed SM, Lemkau JP, Birt SL. Toward sensitive treatment of obese patients. Fam Pract Manag. 2002 Jan;9(1):25–28. [PubMed] [Google Scholar]