Abstract
The aim of this open-label, fixed-sequence study was to investigate the potential of the botanical supplement Echinacea purpurea to interact with etravirine, a nonnucleoside reverse transcriptase inhibitor of HIV. Fifteen HIV-infected patients receiving antiretroviral therapy with etravirine (400 mg once daily) for at least 4 weeks were included. E. purpurea root/extract-containing capsules were added to the antiretroviral treatment (500 mg every 8 h) for 14 days. Etravirine concentrations in plasma were determined by high-performance liquid chromatography immediately before and 1, 2, 4, 6, 8, 10, 12, and 24 h after a morning dose of etravirine on day 0 and etravirine plus E. purpurea on day 14. Individual etravirine pharmacokinetic parameters were calculated by noncompartmental analysis and compared between days 0 and 14 by means of the geometric mean ratio (GMR) and its 90% confidence interval (CI). The median age was 46 years (interquartile range, 41 to 50), and the median body weight was 76 kg (interquartile range, 68 to 92). Echinacea was well tolerated, and all participants completed the study. The GMR for etravirine coadministered with E. purpurea relative to etravirine alone was 1.07 (90% CI, 0.81 to 1.42) for the maximum concentration, 1.04 (90% CI, 0.79 to 1.38) for the area under the concentration-time curve from 0 to 24 h, and 1.04 (90% CI, 0.74 to 1.44) for the concentration at the end of the dosing interval. In conclusion, the coadministration of E. purpurea with etravirine was safe and well tolerated in HIV-infected patients; our data suggest that no dose adjustment for etravirine is necessary.
INTRODUCTION
More than half of HIV-infected patients express interest in taking some kind of complementary therapy in addition to their antiretroviral regimens at some point during the course of treatment (15, 16, 19). These patients usually choose dietary and herbal supplements and take them without medical supervision. Nonetheless, such botanical supplements may influence the activity of various enzymes and transporters involved in the absorption, distribution, and metabolism of antiretroviral drugs, putting patients at risk of potential herb-drug interactions (11, 14).
Echinacea preparations rank among the herbal remedies most commonly taken by HIV-infected patients (2, 3, 13), probably because of their hypothesized immunostimulant properties (20, 21). Constituents of Echinacea purpurea have the potential to interact with cytochrome P450, providing a reason to suspect herb-drug interactions involving CYP3A4 substrates, including many antiretroviral agents (1, 10, 18). However, we observed no significant interaction between E. purpurea and the HIV-protease inhibitor darunavir in a previous study with HIV-infected patients (17), a finding we attributed to the fact that our patients were also receiving ritonavir. Ritonavir causes nearly complete inhibition of CYP3A4 activity, possibly offsetting the potential influence of E. purpurea on CYP3A4 activity in that study.
Etravirine is a nonnucleoside reverse transcriptase inhibitor of HIV which is primarily metabolized by the hepatic CYP3A4 and, to a lesser extent, by the CYP2C family, followed by glucuronidation (12). Induction of CYP3A4 activity by E. purpurea could therefore theoretically result in inadequately low etravirine concentrations. The magnitude of this potential interaction could be ameliorated by using etravirine in combination with a ritonavir-boosted protease inhibitor (12). However, there is a growing interest in using etravirine once daily without a protease inhibitor (8; P. Echeverría, A. Bonjoch, J. Puig, R. Paredes, G. Sirera, J. R. Santos, J. Moltó, B. Clotet, and E. Negredo, presented at the 51st Interscience Conference on Antimicrobial Agents and Chemotherapy, 2011), a scenario where possible CYP3A4 induction might be more relevant.
The objective of the present study was therefore to evaluate the potential of E. purpurea to interact with etravirine in the absence of ritonavir.
MATERIALS AND METHODS
Study design.
This open-label, fixed-sequence study enrolled 15 HIV-infected patients who had been receiving antiretroviral therapy with etravirine (400 mg once daily) for at least 4 weeks and whose HIV-1 RNA load in plasma was <50 copies/ml. Patients on concomitant treatment with ritonavir or other CYP3A4 inhibitors or with a history of suboptimal treatment adherence were excluded. All patients gave written informed consent before enrollment, the protocol was approved by our hospital's ethics committee and the Spanish Medicines and Medical Devices Agency, and the study was performed according to the stipulations of the Declaration of Helsinki and registered (ClinicalTrials.gov identifier, NCT01347658).
Patients took capsules containing E. purpurea root extract (Arkocápsulas Echinácea, lot no. W064636A; Arkopharma) at a dosage of 500 mg every 8 h from days 1 to 14. All pills came from a single lot, which was externally controlled and certified to contain 100% of the labeled content of E. purpurea. Antiretroviral treatment remained unchanged. Serial blood samples to determine etravirine concentrations in plasma were collected immediately before and 1, 2, 4, 6, 8, 10, 12, and 24 h after a witnessed morning dose of etravirine on day 0 and at the same times before and after etravirine plus E. purpurea on day 14. On both days, etravirine was taken with a standard 550-kcal breakfast whose composition was 43% carbohydrate, 39% fat, and 18% protein.
Demographic and clinical variables (age, body weight and height, and use of concomitant drugs, including over-the-counter medications) were recorded. Safety was evaluated by clinical interview and physical examination, as well as by the laboratory assessments (blood counts, chemistry, CD4+ T-cell count, and HIV-1 RNA load), on days 0, 14, and 28. To enhance adherence to scheduled clinical visits and the treatment protocol, patients were provided with a visit calendar. Apart from days 0 and 14, drug intake was not directly observed; adherence was assessed by means of a diary, in which the patient recorded medication intake, and by pill count on day 14.
Analytical and pharmacokinetic analysis.
Blood samples for etravirine determinations were collected into K-ethylenediaminetetraacetic acid–containing 10-ml tubes. Plasma was isolated by centrifugation (3,200 × g for 15 min) and stored at −20°C until analysis. Etravirine concentrations were determined by high-performance liquid chromatography with a fluorescence detector (Multifluorescence detector 2475; Waters) according to a validated method. Chromatographic separation was performed on a Sunfire C18 column (particle size 5 μm, 4.6 by 150 mm; Waters) protected by a SecurityGuard C18 column (4.0 by 3.0 mm; Phenomenex). The fluorescence detector was set at 299 and 396 nm for excitation and emission wavelengths, respectively. The drug was extracted from plasma by liquid-liquid extraction with tert-butyl methyl ether. The mobile phase consisted of a gradient elution with phosphate buffer (50 mM) in acetonitrile (pH 6.70). The method was linear over the range of 0.01 to 2.40 mg/liter. The intraday and interday coefficients of variation were less than 10%. Our laboratory subscribes to the external quality assurance program organized by the Association for Quality Assessment in Therapeutic Drug Monitoring and Clinical Toxicology of Radboud University Nijmegen Medical Centre, Nijmegen, the Netherlands (6).
Etravirine pharmacokinetic parameters were calculated for each individual using a noncompartmental approach by means of WinNonlin software application (version 2.0; Pharsight, Mountain View, CA). The area under the concentration-time curve during the dose interval (AUC0–24) was calculated by means of the linear trapezoidal rule. Maximum concentrations (Cmax), and the concentrations at the end of the dosing interval (C24), were obtained by inspection of the concentration data.
Statistical analysis.
Data analysis was carried out using SPSS version 15.0 statistical software. Etravirine pharmacokinetic parameters were described by the geometric mean and compared between days 0 and 14 by the geometric mean ratio (GMR). Pharmacokinetic parameters were natural log-transformed before analysis, and confidence intervals (CIs) for means (and for the difference between two means) were constructed on the natural log scale based on an analysis of variance (ANOVA) model with treatment as a fixed effect. The results were then exponentiated and reported with 90% CIs.
A power calculation indicated that 15 patients would provide an 80% chance of detecting a 25% difference in the AUC0–24 for etravirine at a level of significance of 0.05 (P value).
RESULTS
A total of 15 Caucasian HIV-infected patients were enrolled. Overall, 10 (66.7%) were males, and 4 (26.7%) were coinfected with hepatitis C virus (HCV). The median age was 46 years (interquartile range, 41 to 50), and the median body weight was 76 kg (interquartile range, 68 to 92). Other antiretroviral drugs being taken in addition to etravirine included tenofovir-emtricitabine (10 patients) and abacavir-lamivudine (5 patients). The median CD4+ T cell count was 799 cells/mm3 (range, 541 to 946).
The echinacea preparation was well tolerated, and all participants completed the study. Patients were fully adherent to antiretroviral and echinacea treatments, none reported drug-related adverse events during the study, and all had an HIV-1 RNA load of <50 copies/ml at the end of the study.
Etravirine pharmacokinetics.
One participant displayed etravirine concentrations which were near 10 times higher than those observed in the rest of the patients in both study periods. This patient was considered to be a poor metabolizer/outlier, and he was excluded from the pharmacokinetic analysis.
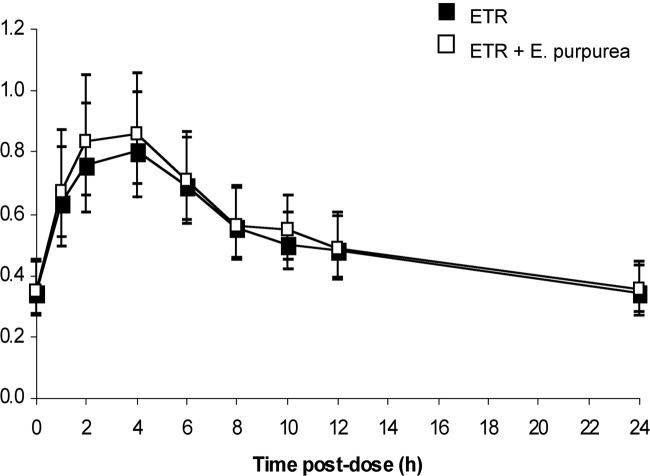
The mean plasma concentration-time curves of etravirine in the presence and absence of E. purpurea are shown in Fig. 1, and comparisons of etravirine pharmacokinetic parameters between days 0 and 14 are summarized in Table 1. Etravirine concentration curves were superimposed, and no significant treatment effects were observed for any of the primary pharmacokinetic parameters after administration of etravirine with (day 14) or without (day 0) E. purpurea. Despite once-daily dosing of etravirine without boosted protease inhibitors, etravirine trough concentrations remained consistently above the median protein-binding-adjusted 50% effective concentration (EC50) for wild-type HIV (0.004 mg/liter) (5) in all participants (Fig. 2).
Fig 1.
Geometric mean etravirine (ETR) plasma concentration profiles with or without multiple doses of Echinacea purpurea. Error bars represent 90% confidence intervals.
Table 1.
Etravirine pharmacokinetic parameters with and without the coadministration of multiple doses of E. purpureaa
| Parameter | ETR | ETR + E. purpurea | GMR (90% CI) | P value |
|---|---|---|---|---|
| Cmax (mg/liter) | 0.88 (0.72–1.07) | 0.95 (0.78–1.15) | 1.07 (0.81–1.42) | 0.667 |
| AUC0–24 (mg · h/liter) | 12.6 (10.2–15.4) | 13.2 (10.7–16.1) | 1.04 (0.79–1.38) | 0.802 |
| C24 (mg/liter) | 0.34 (0.27–0.43) | 0.35 (0.28–0.44) | 1.04 (0.74–1.44) | 0.856 |
Data are expressed as geometric mean (90% confidence interval). ETR, etravirine; GMR, geometric mean ratio; CI, confidence interval; Cmax, maximum concentration; AUC0–24, area under the concentration-time curve from 0 to 24 h after dosing; C24, concentration at the end of the dosing interval.
Fig 2.
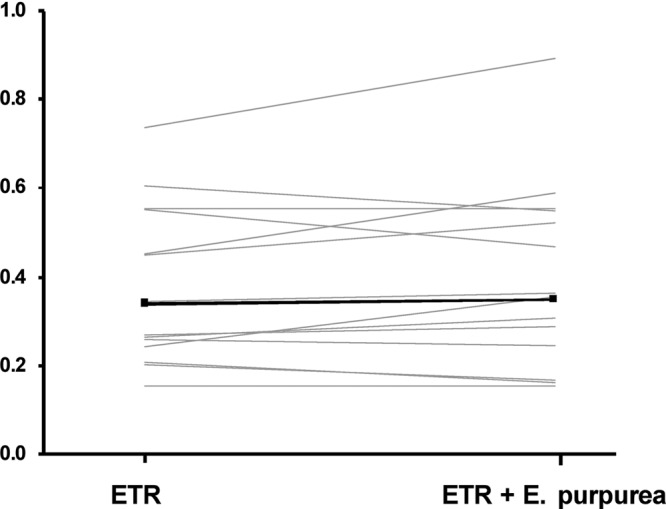
Etravirine (ETR) concentrations at the end of the dosing interval (C24) after administration of ETR with or without multiple doses of Echinacea purpurea. The gray lines represent individual values, and the black line represents the geometric mean.
DISCUSSION
Our findings show that E. purpurea does not significantly affect the pharmacokinetics of etravirine in HIV-infected patients and therefore is not likely to put the patients at a significant herb-drug interaction risk.
The concern that E. purpurea might induce CYP3A4 activity in patients on antiretroviral agents, which are metabolized by this enzyme, is based on previous studies that found that midazolam exposure decreased by nearly 25% in the presence of an echinacea preparation (10, 18). However, two recent studies in individuals taking echinacea with boosted protease inhibitors found no significant interaction (17, 18). One study was performed in healthy volunteers who received lopinavir-ritonavir (18), and the other was conducted in HIV-infected patients taking darunavir-ritonavir (17). In these studies, the lack of interaction could have been due to the coadministration of both lopinavir and darunavir with low doses of ritonavir, a potent CYP3A4 inhibitor which could have offset the CYP3A4-inducing effects of echinacea. Our findings in the present study contribute to attenuating any concerns that remain, however, given that the effect of echinacea on etravirine pharmacokinetics in our patients was negligible despite the lack of a boosted protease inhibitor. Nonetheless, it is noteworthy that the magnitude of this interaction was quite variable at the individual level, from near 25% decreases to up to 50% increases in drug concentrations, possibly supporting monitoring etravirine concentrations in plasma if possible.
Three factors are relevant to interpreting our results. First, in addition to CYP3A4 induction at the liver by E. purpurea, inhibition at the intestinal lumen has also been reported (10) and could also offset the potential induction of hepatic CYP3A4. Second, etravirine is a CYP3A4 inducer itself, and it could have masked potential induction of CYP3A by echinacea. Third, discrepancies between the labeled and the actual content of active constituents have been reported for many botanical preparations, to the extent that commercial products have not contained the labeled herb at all in some cases (7, 9). To avoid an effect of this potential limitation within our study, we purchased a single lot of E. purpurea from Arkopharma, which is a leader in the botanical supplement market in Europe. This company is externally controlled and has been granted the Good Manufacturing Practices certificate by the AFSSAPS (a French health products safety agency).
Although etravirine is licensed for twice-daily dosing and for use in combination with a boosted protease inhibitor (12), the patients in this study were receiving 400 mg of etravirine once daily without a boosted protease inhibitor. Interest in this off-label etravirine dosing regimen has emerged in the clinical setting (8; P. Echeverría, A. Bonjoch, J. Puig, R. Paredes, G. Sirera, J. R. Santos, J. Moltó, B. Clotet, and E. Negredo, presented at the 51st Interscience Conference on Antimicrobial Agents and Chemotherapy, 2011). Even though etravirine exposure is known to be lower after once-daily administration (4), it is noteworthy that all our patients showed etravirine concentrations far above the protein-binding-adjusted EC50 for wild-type HIV (5) and all had undetectable viral loads at the end of the study (although this concentration cutoff value has not been clinically validated to be used in therapeutic drug-monitoring programs).
We conclude that the coadministration of E. purpurea with etravirine is safe and well tolerated in HIV-infected patients. Our data suggest that no dose adjustment for etravirine is necessary in this scenario.
ACKNOWLEDGMENTS
We thank the staff at the clinical site where data were gathered for this study and the patients who participated. We also acknowledge the contribution of Mary Ellen Kerans, who gave her advice on English language expression in the final version of the manuscript.
We have no conflicts of interest that are directly relevant to the context of this study. This study was funded by a grant from the Spanish Health Department (Ministerio de Sanidad, Política Social e Igualdad; EC10-093) and by the Lluita contra la SIDA Foundation, Gala contra la SIDA, Barcelona, 2011. M.V. is supported by FIS through grant CP04/00121 from the Spanish Health Department in collaboration with Institut de Recerca de l'Hospital de la Santa Creu i Sant Pau, Barcelona, and she is a member of CIBERSAM (a research network funded by the Spanish Health Ministry, Instituto de Salud Carlos III).
Footnotes
Published ahead of print 6 August 2012
REFERENCES
- 1. Barnes J, Anderson LA, Gibbons S, Phillipson JD. 2005. Echinacea species [Echinacea angustifolia (DC.) Hell., Echinacea pallida (Nutt.) Nutt., Echinacea purpurea (L.) Moench]: a review of their chemistry, pharmacology and clinical properties. J. Pharm. Pharmacol. 57:929–954 [DOI] [PubMed] [Google Scholar]
- 2. Barnes PM, Powell-Griner E, McFann K, Nahin RL. 2004. Complementary and alternative medicine use among adults: United States, 2002, p 1–19 Adv. Data, no. 343 [PubMed] [Google Scholar]
- 3. Blumenthal M. 1999. Herb market levels after five years of boom, p 64–65 HerbalGram, no. 47 [Google Scholar]
- 4. Boffito M, et al. 2009. Pharmacokinetics and safety of etravirine administered once or twice daily after 2 weeks treatment with efavirenz in healthy volunteers. J. Acquir. Immune Defic. Syndr. 52:222–227 [DOI] [PubMed] [Google Scholar]
- 5. DeJesus E, et al. 2010. Pharmacokinetics of once-daily etravirine without and with once-daily darunavir/ritonavir in antiretroviral-naive HIV type-1-infected adults. Antivir. Ther. 15:711–720 [DOI] [PubMed] [Google Scholar]
- 6. Droste JA, Aarnoutse RE, Koopmans PP, Hekster YA, Burger DM. 2003. Evaluation of antiretroviral drug measurements by an interlaboratory quality control program. J. Acquir. Immune Defic. Syndr. 32:287–291 [DOI] [PubMed] [Google Scholar]
- 7. Garrard J, Harms S, Eberly LE, Matiak A. 2003. Variations in product choices of frequently purchased herbs: caveat emptor. Arch. Intern. Med. 163:2290–2295 [DOI] [PubMed] [Google Scholar]
- 8. Gazzard B, et al. 2011. Phase 2 double-blind, randomized trial of etravirine versus efavirenz in treatment-naive patients: 48-week results. AIDS 25:2249–2258 [DOI] [PubMed] [Google Scholar]
- 9. Gilroy CM, Steiner JF, Byers T, Shapiro H, Georgian W. 2003. Echinacea and truth in labeling. Arch. Intern. Med. 163:699–704 [DOI] [PubMed] [Google Scholar]
- 10. Gorski JC, et al. 2004. The effect of echinacea (Echinacea purpurea root) on cytochrome P450 activity in vivo. Clin. Pharmacol. Ther. 75:89–100 [DOI] [PubMed] [Google Scholar]
- 11. Izzo AA, Ernst E. 2009. Interactions between herbal medicines and prescribed drugs: an updated systematic review. Drugs 69:1777–1798 [DOI] [PubMed] [Google Scholar]
- 12. Johnson LB, Saravolatz LD. 2009. Etravirine, a next-generation nonnucleoside reverse-transcriptase inhibitor. Clin. Infect. Dis. 48:1123–1128 [DOI] [PubMed] [Google Scholar]
- 13. Ladenheim D, et al. 2008. Potential health risks of complementary alternative medicines in HIV patients. HIV Med. 9:653–659 [DOI] [PubMed] [Google Scholar]
- 14. Lee LS, Andrade AS, Flexner C. 2006. Interactions between natural health products and antiretroviral drugs: pharmacokinetic and pharmacodynamic effects. Clin. Infect. Dis. 43:1052–1059 [DOI] [PubMed] [Google Scholar]
- 15. Littlewood RA, Vanable PA. 2008. Complementary and alternative medicine use among HIV-positive people: research synthesis and implications for HIV care. AIDS Care 20:1002–1018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Moltó J, et al. 2012. Use of herbal remedies among HIV-infected patients: patterns and correlates. Med. Clin. (Barc). 138:93–98 (In Spanish.) [DOI] [PubMed] [Google Scholar]
- 17. Moltó J, et al. 2011. Herb-drug interaction between Echinacea purpurea and darunavir-ritonavir in HIV-infected patients. Antimicrob. Agents Chemother. 55:326–330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Penzak SR, et al. 2010. Echinacea purpurea significantly induces cytochrome P450 3A activity but does not alter lopinavir-ritonavir exposure in healthy subjects. Pharmacotherapy 30:797–805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Risa KJ, et al. 2002. Alternative therapy use in HIV-infected patients receiving highly active antiretroviral therapy. Int. J. STD AIDS 13:706–713 [DOI] [PubMed] [Google Scholar]
- 20. Shah SA, Sander S, White CM, Rinaldi M, Coleman CI. 2007. Evaluation of echinacea for the prevention and treatment of the common cold: a meta-analysis. Lancet Infect. Dis. 7:473–480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Sharma SM, Anderson M, Schoop SR, Hudson JB. 2010. Bactericidal and anti-inflammatory properties of a standardized Echinacea extract (Echinaforce): dual actions against respiratory bacteria. Phytomedicine 17:563–568 [DOI] [PubMed] [Google Scholar]