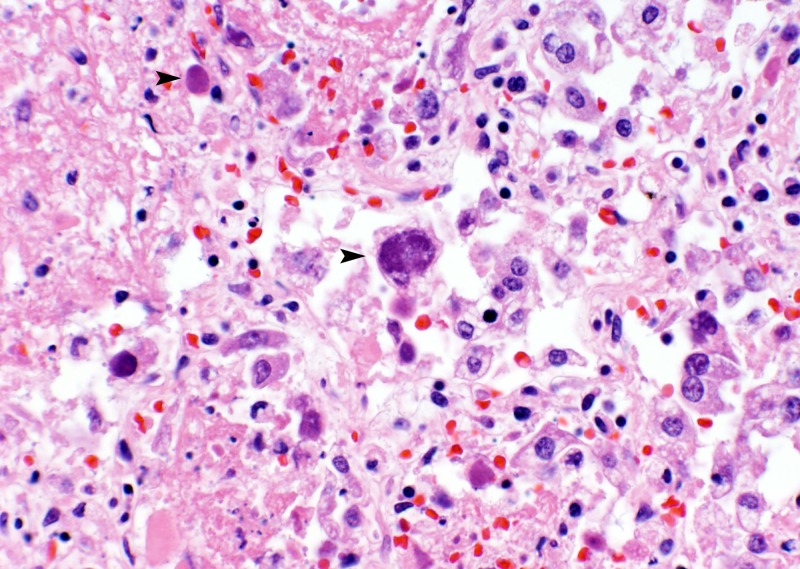
A 40-year-old obese white male with no significant past medical history presented to an outside community-based hospital with right upper abdominal quadrant pain. Imaging studies showed right lung lesions and a right pleural effusion. He was also noted to have new-onset diabetes mellitus, with hemoglobin A1c (HbA1c) levels of 13.7%. He was started on antibiotics for presumed community-acquired pneumonia. Two days later, he required a ventilator for impending respiratory failure. At the same time, his 4-year-old son was also admitted with respiratory complaints. The family lived on a farm and had significant exposure to farm animals, corn, and hay. The differential possibilities entertained were bacterial pneumonia (including pneumonic tularemia) and fungal infections. Blood, bronchoalveolar lavage (BAL), and pleural fluid cultures from the patient were negative for bacterial and fungal organisms. The results for multiplex PCR viral testing on the nasopharyngeal swabs from both father and son were positive for one target. The son was discharged in stable condition after 4 days of hospitalization. However, the father was put on extracorporeal membrane oxygen (ECMO) for his inability to maintain oxygen saturation. Episodes of hypotension ensued, and he died 11 days after his initial admission. A complete autopsy was performed, which confirmed bilateral lung consolidation and pleural effusion. Histologically, the lungs showed diffuse alveolar damage, necrotizing inflammation, and many atypical pneumocytes, as seen in Fig. 1.
Fig 1.
Hematoxylin and eosin-stained section of the lung with intra-alveolar fibrinous material and atypical pneumocytes (arrowheads).
(For answer and discussion, see page 3414 in this issue [doi:10.1128/JCM.00371-12])
Contributor Information
Vijayalakshmi Ananthanarayanan, Department of Pathology University of Chicago Chicago, Illinois, USA.
Jeffrey Mueller, Department of Pathology University of Chicago Chicago, Illinois, USA.
Jerome Taxy, Department of Pathology University of Chicago Chicago, Illinois, USA.
Vera Tesic, Department of Pathology University of Chicago Chicago, Illinois, USA.