Abstract
OBJECTIVE:
Variation in energy intake by weight status at different ages may explain inconsistencies in previous research on energy intake and obesity. Therefore, our objective was to determine the relationship between reported daily energy intake and categorized weight status across childhood.
METHODS:
We examined dietary reports of children ages 1 to 17 years by using the National Health and Nutrition Examination Survey, 2001–2008 (N = 12 648). Using measured height and weight, we categorized weight status based on weight-for-length percentile (age <2 years) or BMI percentile (ages 2–17 years) using current recommendations. Dietary intake was reported by using the repeatedly validated automated multiple pass method, a detailed 2-day 24-hour recall. We used ordinary least squares regression to examine the interactions of age and weight category on total energy intake, controlling for gender, race, ethnicity, and income.
RESULTS:
Weight status and age both have positive associations with self-reported energy intake. However, the interaction between weight and age demonstrates a negative effect throughout childhood, such that young obese/overweight children reported consuming significantly more calories and obese/overweight adolescents reported consuming fewer calories than their same-age healthy-weight peers.
CONCLUSIONS:
In a nationally representative cross-sectional sample, overweight and obese girls older than 7 years and boys older than 10 years reported consuming fewer daily calories than their healthy-weight peers. One explanation for this would be that increased energy intake in early childhood is related to the onset of obesity, but other mechanisms, such as differences in energy expenditure, may contribute more to maintaining obese/overweight status through adolescence.
Keywords: Obesity, energy intake, population-based survey, nutrition
What’s Known on This Subject:
The relationship between energy intake and obesity in children has yielded inconsistent results. Efforts to improve dietary intake as a means of improving weight status have largely yielded disappointing results.
What This Study Adds:
Self-reported energy intake for younger, but not older, overweight/obese children is higher than healthy-weight peers. In early childhood, higher (or excessive) energy intake may lead to onset of obesity, but other mechanisms may be important to maintain obesity through adolescence.
In recent years, the childhood obesity epidemic has become one of the most prominent health concerns among both the public and researchers. Despite evidence that obesity in children is related to poorer health,1–3 very few interventions have shown any significant long-term weight status improvement or gains in weight-related health outcomes.4,5
Dietary interventions aimed at overweight children have been particularly disappointing. Many of the interventions described are inadequate in terms of their breadth of behaviors, study design, and length of follow-up and have failed to yield improved weight status trajectories.6,7 While weight status is determined by the balance of energy intake and energy expenditure, interventions to reduce calories generally are based on the assumption that the primary focus for overweight and obese children should be to reduce energy intake, without considering how this may compare with their healthy-weight peers. Understanding how energy intake of children varies at different ages and by weight status can help identify what energy reduction would look like for overweight children.
Previous research indicates that consumption differences, particularly total energy intake, between overweight and healthy-weight children are minimal or nonexistent.8–10 Because children who are overweight tend to remain overweight, it may be rationalized that for a majority of these children, the onset of obesity results from excess energy intake during early childhood, but large differences in energy intake are not then needed to maintain obesity thereafter. If that were true, then early childhood interventions might focus specifically on energy intake instead of increasing energy expenditure, while those in later childhood or adolescence might focus instead on energy expenditure, which has been evidenced to be lower for overweight and obese children.11 Regardless, understanding differences in energy intake by weight status throughout childhood is necessary to design effective obesity interventions.
Our objective was to examine the relationship between energy intake and measured weight status using a nationally representative sample of children throughout the childhood years to determine if overweight children consume excess energy and if the relationship varies between boys and girls and by age. We hypothesized that energy intake would be greater among overweight and obese children, with differing magnitude of effect at varying ages.
Methods
We used the National Health and Nutrition Examination Survey (NHANES) from 2001 through 2008. NHANES is a stratified, multistage probability sample of the civilian, noninstitutionalized population of the United States. It includes an in-home questionnaire on a variety of demographic and health-related topics, a computer-assisted interview, and an examination component composed of a thorough physical examination including measured height and weight.12,13
Food consumption data (energy intake) in NHANES were collected and recorded by using the automated multiple pass method (AMPM). This method involves a computer-assisted interview with five primary steps. First, participants are asked to recall all foods and beverages consumed the day before the visit from midnight to midnight. Next, they are probed to identify foods forgotten in the first step, called the quick list. Time and eating occasion are collected for each of the foods listed. For each food listed, a detailed description of the food and amount of food is recorded. A collection of measuring devices was used to help participants estimate portion sizes. Finally, there is another probe for any additional foods that may have been forgotten. This method has been validated by using the gold-standard double-labeled water method, which tracks energy expended compared with energy reported. A detailed description of the AMPM is available elsewhere.14,15
Dietary information about the foods consumed was then determined based on the Food and Nutrient Database for Dietary Surveys.16 In this study, we used total energy intake as calculated by the National Center for Health Statistics and included with NHANES data.
Children younger than 6 years had proxies report food intake for them, usually a parent. Children aged 6 to 11 years reported food intake themselves with the assistance of an adult, again, usually a parent. Adolescents 12 years and older reported for themselves without a proxy. To assess whether the shift in methodology for who reports introduced a systematic bias into the results, we tested for differences in reported mean energy intake between children aged 5 and 6 years and again for children aged 11 and 12 years, representing the crossover points for the type of interview. There were no significant differences in total energy intake between ages in these groups of children, suggesting that the change in reporter did not bias the reported food consumption or influence energy intake calculations.
All participants in NHANES were eligible for the dietary recall. We include all participants aged 1 to 17 years. The first recall was completed during the in-person examination. A second recall was completed 3 to 10 days later via telephone. In 2001–2002, only the first-day interview was released. For 2003–2008, we use the mean value across the 2 days for each individual to represent average daily energy intake; for 2001–2002, we use only the first day. A total of 13 767 children who met all our inclusion criteria completed the first interview, while 12 648 (92%) completed the second (or were included because they had a day 1 interview in 2001–2002).
Children were categorized as obese, overweight, or healthy weight based on the BMI percentiles and current Centers for Disease Control and Prevention recommendations.17–19 For children younger than 2 years, we used weight-for-length percentiles in place of BMI percentiles. We used height and weight as measured during the examination component to calculate BMI percentile, using SAS code (SAS Institute, Inc, Cary, NC) developed for that purpose.20 Children in the ≥99th percentile were defined as very obese; ≥95th to <99th percentile, obese; ≥85th to <95th percentile, overweight; and <85th to ≥5th percentile, healthy weight according to consensus definition.17 Due to concerns about possible associated health conditions, we excluded all children who were underweight (<5th percentile), representing 3% of the population.
We used adjusted Wald tests to examine the differences in energy intake by weight status for girls and boys separately. Dietary characteristics are likely affected by demographic factors, and racial and ethnic minorities and those of low socioeconomic status are more likely to be overweight.21,22 As such, we also used multiple regression analyses to examine the relationship between energy intake and weight status. We used ordinary least squares regression to examine the relationship between weight status and total energy intake, including interactions between weight and age to examine age-based differences in the effect of weight status. We also included age-squared and interactions between age-squared and weight in our models, because of the possibility that weight did not have a linear effect by age on total energy intake. We controlled for child’s race, ethnicity, and income. Race and ethnicity were categorized as non-Hispanic white, non-Hispanic black, Mexican American or other Hispanic, or other race. Income was based on the percentage of federal poverty level (FPL) of household income, from <100% (most deprived) to ≥500% (most affluent).
All analyses were adjusted for the complex survey design of NHANES, as recommended by National Center for Health Statistics.23 Analyses were performed by using the survey estimation routines in Stata 12.0 (Stata Corp, College Station, TX). This study was deemed exempt from additional review by the institutional review board under federal regulation 45 CFR §46.101(b) because it used only deidentified secondary data.
Results
A total of 12 648 subjects had 2 days of food consumption data and were included in the final sample. Weighted to represent the US population during the study period, the majority of children were non-Hispanic white (Table 1), with 15% non-Hispanic black and 6% Hispanic. Gender was evenly distributed overall. Nearly half of children were under 200% of the FPL age. Most children (69%) were healthy weight, with 16% overweight, 12% obese, and 4% very obese.
TABLE 1.
Demographic Characteristics of the Population (N = 12 648)
| Characteristic | Percent |
|---|---|
| Age category, y | |
| 1–2 | 11.2 |
| 3–5 | 16.1 |
| 6–8 | 17.7 |
| 9–11 | 18.0 |
| 12–14 | 18.3 |
| 15–17 | 18.7 |
| Gender | |
| Female | 49.3 |
| Male | 50.7 |
| Race/ethnicity | |
| Non-Hispanic white | 61.5 |
| Non-Hispanic black | 14.6 |
| Other race | 17.9 |
| Hispanic | 6.1 |
| Income, % FPL | |
| <100 | 20.9 |
| 100–200 | 22.0 |
| 200–300 | 16.4 |
| 300–400 | 12.7 |
| 400–500 | 9.6 |
| >500% | 14.3 |
| Missing | 4.0 |
| Weight category | |
| Very obese | 3.9 |
| Obese | 11.6 |
| Overweight | 15.9 |
| Healthy weight | 68.6 |
FPL: Federal Poverty Level
For girls aged 1 to 8 years, there was a nonsignificant trend for very obese, obese, and overweight children to have increased energy intake compared with healthy-weight or underweight children (Table 2). A similar pattern was seen in boys, and the differences were strong enough to reach statistical significance for boys aged 6 to 8 years. However, beginning at age 9 to 11 years for girls and boys, children who were healthy weight had greater energy intake than children who were very obese, obese, or overweight, a pattern that was significant for girls and older boys.
TABLE 2.
Mean Self-reported Energy Intake, SE, and Range by Age, Gender, and BMI Weight Category
| Gender/Age | Very Obese | Obese | Overweight | Healthy Weight | P* |
| Girls | |||||
| 1–2 y, n = 904 | 1317 (74) [734–3673] | 1255 (71) [668–2469] | 1353 (43) [542–2915] | 1310 (21) [177–3687] | .688 |
| 3–5 y, n = 907 | 1859 (134) [1062–2962] | 1670 (80) [908–3210] | 1721 (76) [690–3117] | 1578 (31) [410–4077] | .072 |
| 6–8 y, n = 928 | 1850 (189) [976–3532] | 1802 (78) [722–4410] | 1848 (63) [1040–4496] | 1778 (29) [434–3835] | .790 |
| 9–11 y, n = 943 | 1759 (83) [747–4041] | 2018 (75) [439–4178] | 1712 (84) [440–4708] | 1959 (41) [567–5099] | .021 |
| 12–14 y, n = 1391 | 1484 (79) [401–5720] | 1783 (79) [380–4479] | 1794 (44) [243–4370] | 1893 (46) [321–6274] | <.001 |
| 15–17 y, n = 1276 | 1813 (164) [406–3084] | 1637 (95) [334–4236] | 1798 (71) [531–5254] | 1926 (37) [263–6376] | .039 |
| Boys | |||||
| 1–2 y, n = 940 | 1536 (184) [717–2714] | 1395 (66) [555–2650] | 1439 (46) [554–3077] | 1410 (23) [91–3465] | .835 |
| 3–5 y, n = 944 | 1831 (91) [783–3300] | 1775 (94) [183–4129] | 1809 (73) [567–4743] | 1668 (28) [435–4012] | .128 |
| 6–8 y, n = 878 | 2127 (152) [1132–3537] | 2037 (70) [503–3809] | 2206 (63) [847–4698] | 1978 (29) [657–4523] | .011 |
| 9–11 y, n = 903 | 2089 (90) [1052–3773] | 2203 (73) [604–4520] | 2342 (83) [478–5911] | 2131 (40) [574–5193] | .088 |
| 12–14 y, n = 1280 | 2024 (108) [609–3997] | 2117 (82) [683–5433] | 2209 (87) [614–6332] | 2291 (59) [632–6003] | .160 |
| 15–17 y, n = 1354 | 2325 (172) [397–5395] | 2304 (88) [592–5702] | 2522 (116) [465–8305] | 2897 (75) [210–9782] | <.001 |
Values are given as mean (SE) [range].
*P values are from adjusted Wald tests for differences by weight category, for each age and gender group.
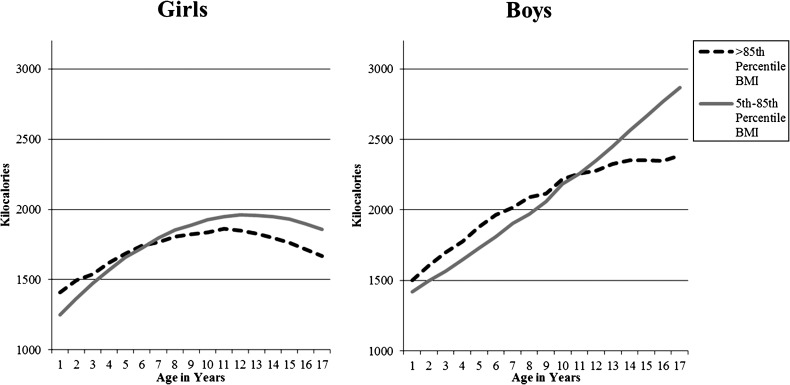
Multivariate models (Table 3) controlling for race/ethnicity and income confirm the bivariate findings. Overall, very obese, obese, and overweight children consume more calories than do healthy-weight children. However, the interactions between weight status and age and between weight status and age-squared are generally negative, indicating that each additional year of age reflects lower energy intake among overweight children, compared with healthy-weight children. Understanding the significance of the relationship between obesity and energy intake at different ages requires considering not only the coefficient on weight but also the interactions of weight with age and age-squared. For both boys and girls, joint tests of significance between these interactions (eg, obese × age and obese × age2) are significant at P < .01 for obese and overweight (but not very obese), indicating a significant difference in effect of weight at varying ages on total energy intake. Because of the multiple interactions, examining predicted values provides a more concrete demonstration of the effect. Figure 1 graphically shows the transition for children above the 85th percentile for BMI and healthy-weight and underweight children. Among girls, there is a transition at about age 6 years where healthy-weight girls report consuming more calories; this similar “crossover” occurs in boys at about age ten years. Additionally, energy intake for girls becomes lower among adolescents, with greatest intake at around age 11. In contrast, energy intake for boys increases steadily throughout adolescence.
TABLE 3.
Ordinary Least Squares Regression of the Effects of Age and BMI Weight Category on Total Self-reported Energy Intake
| Girls (N = 6349) | Boys (N = 6299) | |||||
|---|---|---|---|---|---|---|
| B | P | 95% CI | B | P | 95% CI | |
| Very obese | 452.8 | .022 | 66.5 to 839.2 | 76.7 | .673 | −285.2 to 438.5 |
| Obese | −44.3 | .665 | −247.4 to 158.9 | 10.2 | .921 | −194.6 to 214.9 |
| Overweight | 278.2 | .001 | 111.0 to 445.4 | 45.6 | .655 | −157.1 to 248.2 |
| Very obese × age | −123.3 | .064 | −254.2 to 7.6 | −2.3 | .965 | −105.8 to 101.3 |
| Obese × age | 34.8 | .255 | −25.8 to 95.3 | 50.1 | .106 | −11.0 to 111.1 |
| Overweight × age | −68.2 | .010 | −119.1 to −17.2 | 45.3 | .183 | −22.0 to 112.7 |
| Very obese × age2 | 6.2 | .118 | −1.6 to 14.1 | −0.2 | .942 | −6.3 to 5.8 |
| Obese × age2 | −3.1 | .089 | −6.6 to 0.5 | −5.1 | .008 | −8.9 to −1.4 |
| Overweight × age2 | 2.7 | .067 | −0.2 to 5.6 | −4.1 | .056 | −8.2 to 0.1 |
| Age | 134.9 | .000 | 111.0 to 158.7 | 68.6 | .000 | 38.2 to 99.1 |
| Age2 | −5.4 | .000 | −6.7 to −4.0 | 1.2 | .211 | −0.7 to 3.2 |
| Non-Hispanic black | −5.4 | .877 | −75.3 to 64.4 | −111.7 | .003 | −183.2 to −40.3 |
| Other race | −33.6 | .454 | −123.0 to 55.7 | −118.1 | .008 | −204.9 to −31.3 |
| Hispanic | 17.3 | .664 | −61.8 to 96.3 | −85.6 | .026 | −160.6 to −10.7 |
| Income, % PIR | ||||||
| <100% | 73.9 | .166 | −31.4 to 179.3 | −57.8 | .256 | −158.7 to 43.0 |
| 100%–200% | 10.0 | .852 | −97.0 to 117.0 | −47.3 | .484 | −181.4 to 86.9 |
| 200%–300% | −35.0 | .464 | −130.1 to 60.0 | −137.3 | .023 | −255.4 to −19.2 |
| 300%–400% | 49.1 | .270 | −39.2 to 137.5 | 1.4 | .982 | −122.8 to 125.6 |
| 400%–500% | 26.0 | .618 | −77.9 to 130.0 | −69.5 | .375 | −225.1 to 86.1 |
| Missing | 84.3 | .133 | −26.5 to 195.1 | −165.1 | .014 | −296.1 to −34.2 |
| Constant | 1088.9 | .000 | 993.7 to 1184.2 | 1448.7 | .000 | 1338.9 to 1558.6 |
Joint adjusted Wald tests of significance between interactions (eg, obese × age and obese × age2) are significant at P < .01 for overweight and obese BMI categories in both boys and girls. PIR, poverty income ratio (percentage of the FPL for household income).
FIGURE 1.
Energy intake values for energy intake by age, as predicted from regression models in Table 3.
Discussion
In nationally representative cross-sectional data using a previously validated measure, younger boys and girls who are overweight and obese, report greater energy intake than healthy-weight children of the same ages. However, overweight children older than 6 to 10 years reported consuming fewer daily calories than their healthy-weight peers.
We would expect, based on conventional understanding, that overweight and obese children would consume more calories than healthy-weight children. We found that differences in energy intake by weight status were dependent on age. One possible explanation is that increased energy intake in earlier childhood leads to the onset of obesity, which becomes self-perpetuating. If a child has a balance of energy consumed versus expended, an overweight child will tend to remain overweight while a healthy-weight child will remain healthy weight. This idea is supported by research demonstrating that energy intake in infancy is related to obesity in early childhood,24 while there is limited evidence of a similar pattern in older children.8
A second reason for the differences in energy intake may be that overweight children are significantly less active, therefore requiring fewer calories to maintain energy balance. Studies that simultaneously examine energy intake and activity levels have found that moderate and vigorous activity are more strongly associated than is energy intake with fat mass and obesity.9,25 Additionally, overweight and obese children have been shown to participate in significantly less physical activity than healthy-weight children,11,26,27 which would reduce the energy intake needed for them to maintain energy balance.
A third possible explanation is that our findings are solely or partly the result of a weight-dependent bias in estimating and reporting dietary intake among children. Studies of the accuracy of dietary reporting by children have found conflicting results, though those found to be inaccurate have typically used different methods of assessment than the AMPM used in NHANES.28–30 Overall precision of reporting is less important to our findings than whether precision is influenced by weight status, which must be considered a possibility. There is limited validation of the AMPM in children, but it has demonstrated better accuracy than other methods,15 although a bias previously noted of underreporting among overweight women was specifically not seen in trials involving children.31
The most significant limitation of our research is that dietary intake is self-reported, either by children or by a proxy. However, the AMPM that we used has been one of the most repeatedly validated ways to collect dietary intake data in a way suitable for large surveys.14,15,31,32 There are concerns that reporting may be biased by weight status. However, we would note that such bias might reasonably be expected even in younger children. An additional concern is that dietary intake was reported differently across ages. However, as discussed earlier, reported intake increased smoothly across age, even at ages where the reporter type changed. Importantly, we found no significant differences based solely on who was reporting: the parent, the child, or the 2 together. Another limitation is that we used cross-sectional data and are thus unable to make comments about energy intake patterns and obesity within an individual child. However, the use of a large sample of nationally representative data permits strong estimates across age not readily available in longitudinal samples.
Despite these limitations, our findings have significant implications for interventions aimed at preventing and treating childhood obesity. First, our results emphasize the importance if focusing on prevention of overweight, beginning at very early ages. During infancy and early childhood, obesity is often not recognized by parents or clinicians,33,34 yet this is potentially a time to encourage parents to recognize satiety, pay attention to portion size to avoid overfeeding, and increase nutrient density of foods chosen. Second, particularly during adolescence, focusing on activity may prove to be a more useful strategy than encouraging caloric restriction. If adolescents already have similar energy consumption to their healthy-weight peers, overweight children may find it very difficult to change their diets, and thus energy intake, significantly. Although reducing energy intake would certainly result in weight loss, maintaining this reduction may be particularly difficult if it means eating significantly less than their healthy-weight friends and peers.
Conclusions
Our findings are that on average, across a nationally representative sample, younger overweight children have greater self-reported energy intake than their healthy-weight peers, yet overweight adolescents have lower self-reported energy intake. This suggests that reducing childhood obesity may require early education on appropriate levels of energy intake and, in later childhood, a focus on non–calorie-reducing interventions such as increases in activity.
Acknowledgment
The authors would like to thank Stephanie Hasty for assistance in editing the manuscript.
Glossary
- AMPM
automated multiple pass method
- FPL
federal poverty level
- NHANES
National Health and Nutrition Examination Survey
Footnotes
Dr Skinner contributed to the conception and design, acquisition of data, and analysis and interpretation of data; drafted the article and revised it critically for important intellectual content; and gave final approval of the version to be published. Dr Steiner contributed to the conception and design, and interpretation of data; drafted the article and revised it critically for important intellectual content; and gave final approval of the version to be published. Dr Perrin contributed to the conception and design and the interpretation of data; drafted the article and revised it critically for important intellectual content; and gave final approval of the version to be published.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by UNC CTSA RR025747. Dr Skinner is currently supported by BIRCWH (K12-HD01441). Dr Perrin is supported by an NIH career development award (5 K23-HD051817). Funded by the National Institutes of Health (NIH).
References
- 1.Dietz WH. Health consequences of obesity in youth: childhood predictors of adult disease. Pediatrics. 1998;101(3 pt 2):518–525 [PubMed] [Google Scholar]
- 2.Freedman DS, Dietz WH, Srinivasan SR, Berenson GS. The relation of overweight to cardiovascular risk factors among children and adolescents: the Bogalusa Heart Study. Pediatrics. 1999;103(6 pt 1):1175–1182 [DOI] [PubMed] [Google Scholar]
- 3.Skinner AC, Mayer ML, Flower K, Weinberger M. Health status and health care expenditures in a nationally representative sample: how do overweight and healthy-weight children compare? Pediatrics. 2008;121(2). Available at: www.pediatrics.org/cgi/content/full/121/2/e269. [DOI] [PubMed] [Google Scholar]
- 4.Thomas H. Obesity prevention programs for children and youth: why are their results so modest? Health Educ Res. 2006;21(6):783–795 [DOI] [PubMed] [Google Scholar]
- 5.Summerbell C, Waters E, Edmunds LKS, Brown T, Campbell K. Interventions for preventing obesity in children. Cochrane Database Syst Rev. 2005;20(3):CD001871. [DOI] [PubMed] [Google Scholar]
- 6.Spear BA, Barlow SE, Ervin C, et al. Recommendations for treatment of child and adolescent overweight and obesity. Pediatrics. 2007;120(suppl 4):S254–S288 [DOI] [PubMed] [Google Scholar]
- 7.Foster GD, Sherman S, Borradaile KE, et al. A policy-based school intervention to prevent overweight and obesity. Pediatrics. 2008;121(4). Available at: www.pediatrics.org/cgi/content/full/121/4/e794. [DOI] [PubMed] [Google Scholar]
- 8.Moreno LA, Rodríguez G. Dietary risk factors for development of childhood obesity. Curr Opin Clin Nutr Metab Care. 2007;10(3):336–341 [DOI] [PubMed] [Google Scholar]
- 9.Patrick K, Norman GJ, Calfas KJ, et al. Diet, physical activity, and sedentary behaviors as risk factors for overweight in adolescence. Arch Pediatr Adolesc Med. 2004;158(4):385–390 [DOI] [PubMed] [Google Scholar]
- 10.Rocandio AM, Ansotegui L, Arroyo M. Comparison of dietary intake among overweight and non-overweight schoolchildren. Int J Obes Relat Metab Disord. 2001;25(11):1651–1655 [DOI] [PubMed] [Google Scholar]
- 11.Belcher BR, Berrigan D, Dodd KW, Emken BA, Chou CP, Spruijt-Metz D. Physical activity in US youth: effect of race/ethnicity, age, gender, and weight status. Med Sci Sports Exerc. 2010;42(12):2211–2221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National Center for Health Statistics. NHANES General Data Release Documentation. 2008. www.cdc.gov/nchs/nhanes/nhanes2007-2008/generaldoc_e.htm
- 13.National Center for Health Statistics. National Health and Nutrition Examination Survey: 1999-2010 Survey Contents. 2010. www.cdc.gov/nchs/data/nhanes/survey_content_99_10.pdf
- 14.Moshfegh AJ, Rhodes DG, Baer DJ, et al. The US Department of Agriculture Automated Multiple-Pass Method reduces bias in the collection of energy intakes. Am J Clin Nutr. 2008;88(2):324–332 [DOI] [PubMed] [Google Scholar]
- 15.Blanton CA, Moshfegh AJ, Baer DJ, Kretsch MJ. The USDA Automated Multiple-Pass Method accurately estimates group total energy and nutrient intake. J Nutr. 2006;136(10):2594–2599 [DOI] [PubMed] [Google Scholar]
- 16.Agricultural Research Service. USDA Food and Nutrient Database for Dietary Studies, 3.0. Beltsville, MD: Agricultural Research Service; 2008.
- 17.Barlow SE, Expert Committee . Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(suppl 4):S164–S192 [DOI] [PubMed] [Google Scholar]
- 18.Barlow SE, Dietz WH. Obesity evaluation and treatment: Expert Committee recommendations. The Maternal and Child Health Bureau, Health Resources and Services Administration and the Department of Health and Human Services. Pediatrics. 1998;102(3). Available at: www.pediatrics.org/cgi/content/full/102/3/E29. [DOI] [PubMed] [Google Scholar]
- 19.Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC growth charts for the United States: methods and development. Vital Health Stat 11. 2002;246(246):1–190 [PubMed] [Google Scholar]
- 20.National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention. A SAS program for the CDC growth charts. 2005. www.cdc.gov/nccdphp/dnpa/growthcharts/sas.htm
- 21.Chang VW, Lauderdale DS. Income disparities in body mass index and obesity in the United States, 1971-2002. Arch Intern Med. 2005;165(18):2122–2128 [DOI] [PubMed] [Google Scholar]
- 22.Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999-2002. JAMA. 2004;291(23):2847–2850 [DOI] [PubMed] [Google Scholar]
- 23.National Center for Health Statistics. Analytic and reporting guidelines: The National Health and Nutrition Examination Survey. 2006. www.cdc.gov/nchs/data/nhanes/nhanes_03_04/nhanes_analytic_guidelines_dec_2005.pdf
- 24.Ong KK, Emmett PM, Noble S, Ness A, Dunger DB, ALSPAC Study Team . Dietary energy intake at the age of 4 months predicts postnatal weight gain and childhood body mass index. Pediatrics. 2006;117(3). Available at: www.pediatrics.org/cgi/content/full/117/3/e503. [DOI] [PubMed] [Google Scholar]
- 25.Fulton JE, Dai S, Steffen LM, Grunbaum JA, Shah SM, Labarthe DR. Physical activity, energy intake, sedentary behavior, and adiposity in youth. Am J Prev Med. 2009;37(suppl 1):S40–S49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Andersen RE, Crespo CJ, Bartlett SJ, Cheskin LJ, Pratt M. Relationship of physical activity and television watching with body weight and level of fatness among children: results from the Third National Health and Nutrition Examination Survey. JAMA. 1998;279(12):938–942 [DOI] [PubMed] [Google Scholar]
- 27.Chung AE, Skinner AC, Steiner MJ, Perrin EM. Physical activity and BMI in a nationally representative sample of children and adolescents. Clin Pediatr (Phila). 2012;51(2):122–129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Black AE, Prentice AM, Goldberg GR, et al. Measurements of total energy expenditure provide insights into the validity of dietary measurements of energy intake. J Am Diet Assoc. 1993;93(5):572–579 [DOI] [PubMed] [Google Scholar]
- 29.Livingstone MB, Robson PJ, Wallace JM. Issues in dietary intake assessment of children and adolescents. Br J Nutr. 2004;92(suppl 2):S213–S222 [DOI] [PubMed] [Google Scholar]
- 30.Collins CE, Watson J, Burrows T. Measuring dietary intake in children and adolescents in the context of overweight and obesity. Int J Obes (Lond). 2010;34(7):1103–1115 [DOI] [PubMed] [Google Scholar]
- 31.Conway JM, Ingwersen LA, Vinyard BT, Moshfegh AJ. Effectiveness of the US Department of Agriculture 5-step multiple-pass method in assessing food intake in obese and nonobese women. Am J Clin Nutr. 2003;77(5):1171–1178 [DOI] [PubMed] [Google Scholar]
- 32.Conway JM, Ingwersen LA, Moshfegh AJ. Accuracy of dietary recall using the USDA five-step multiple-pass method in men: an observational validation study. J Am Diet Assoc. 2004;104(4):595–603 [DOI] [PubMed] [Google Scholar]
- 33.Huang JS, Donohue M, Golnari G, et al. Pediatricians’ weight assessment and obesity management practices. BMC Pediatr. 2009;9:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Parry LL, Netuveli G, Parry J, Saxena S. A systematic review of parental perception of overweight status in children. J Ambul Care Manage. 2008;31(3):253–268 [DOI] [PubMed] [Google Scholar]