Abstract
Homicide is seven times as common among U.S. non-Hispanic Black as among non-Hispanic White youth ages 15 to 24 years. In 83% of these youth homicides, the murder weapon is a firearm. Yet, for more than a decade, the national public health position on youth violence has been largely silent about the role of firearms, and tools used by public health professionals to reduce harm from other potential hazards have been unusable where guns are concerned. This deprives already underserved populations from the full benefits public health agencies might be able to deliver. In part, political prohibitions against research about direct measures of firearm control and the absence of valid public health surveillance are responsible. More refined epidemiologic theories as well as traditional public health methods are needed if the U.S. aims to reduce disparate Black-White youth homicide rates.
Keywords: Firearms, African Americans, public health, conflict of interest
Background: Firearms and U.S. Youth Homicide
In 2003, overall U.S. homicide rates were 6.9 times higher than homicide rates in other high-income countries, while homicide rates among U.S. 15 to 24 year olds were 42.7 times higher.1 Additionally, as noted by the U.S. Centers for Disease Control and Prevention (CDC) in its 2011 national Health Disparities and Inequalities Report, the highest homicide mortality for all races, ethnicities, and age groups occurred among non-Hispanic Blacks/African Americans ages 20 to 24 years (109.4 per 100,000 population, in contrast to 6.3 for non-Hispanic Whites).2
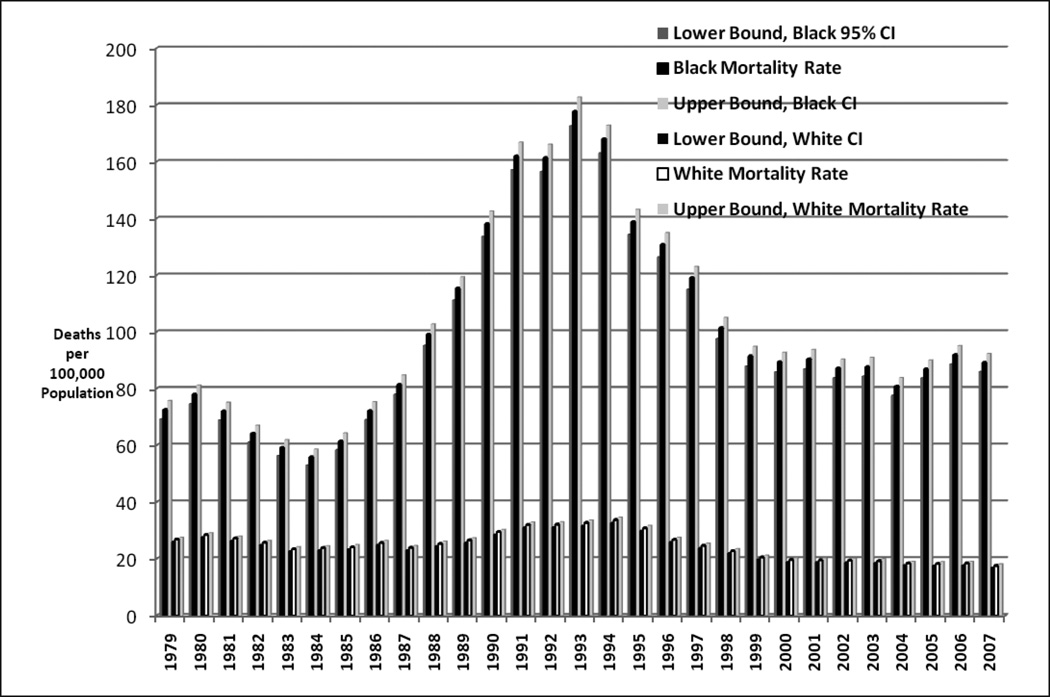
Firearms are the injury mechanism for most U.S. homicides in the 15 to 24 year age group, and most homicide victims are males. Specifically, from 1999 to 2007, the CDC noted that 83% (39,050/47,282) of homicides among 15 to 24 year olds were due to firearms, including 90% (23,826/26,620) of homicides among Blacks. In all, 40,732 (86%) of all homicides among 15 to 24 year olds occurred among males, and this figure was 90% (23,921/26,620) among Black youth.3 Figure 1 presents data (including age-race-sex-specific rates and 95% confidence intervals) for homicides due to firearms among U.S. Black and White males ages 15 to 24 from 1979 to 2007 (from the CDC’s public Internet site [Wonder]).3,4
Figure 1.
Firearm mortality and 95% confidence intervals of Black and White males ages 15 to 24 years in the U.S., 1979–2007.
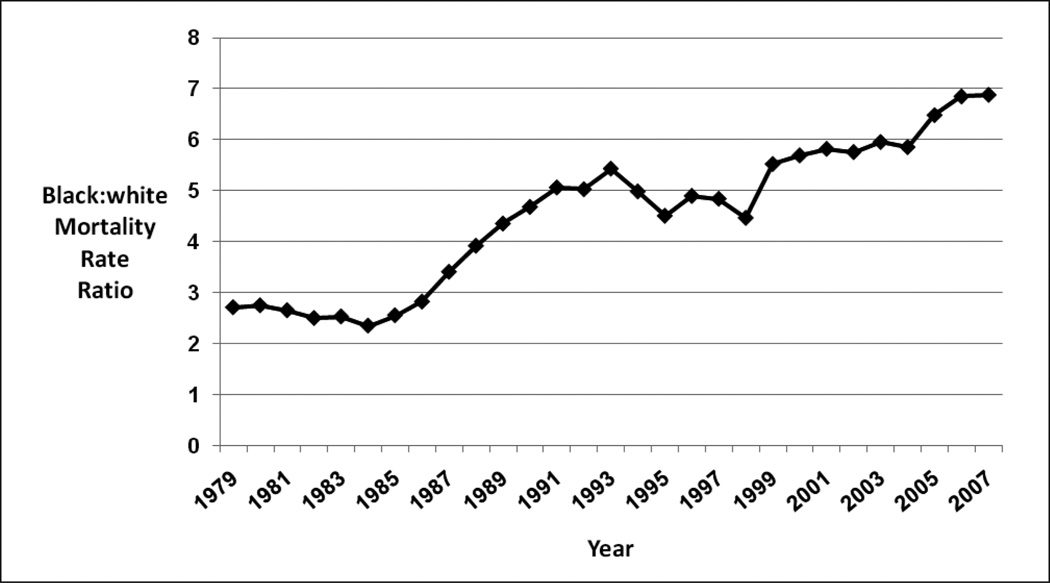
The figure shows an epidemic increase in firearm assault mortality beginning in the mid-1980s, peaking in 1993. Thereafter, each year from 1993 to 1999 brings a statistically significant decline among Black youth (i.e., no overlap in 95% confidence intervals). The same is true for White youth from 1994 through 1999. Rates are generally stable thereafter, and there is no statistically significant difference in the 1999 and 2007 rates for Blacks. However, while White homicides in 2007 stabilized at rates that are significantly lower than White pre-epidemic rates, the Black youth homicide rate for 2007 (92.3 per 100,000) was 65% higher than the pre-epidemic base of 55.8 (1984), and the differences are statistically significant. Black:White youth homicide disparities (Figure 2), increased from 2.3 in 1984 to 6.9 in 2007, the highest level in the observation period. If Black rates for firearm-related deaths had equaled White rates in every year since 1984, there would have been 29,963 fewer deaths among Black youths, and 1,348,507 fewer person-years of life lost through age 65. In summary, while epidemic firearm mortality among White youth ages 15 to 24 seems to have been brought under control, the same is not true for Blacks. Moreover, while the CDC has initiated several preventive efforts since 1999, there is no evidence that youth violence prevention programs have made a discernable overall population difference. Homicide mortality among Black youth has remained above pre-epidemic rates from 1999 to 2007, the most recent years for which data are available.
Figure 2.
Black:White mortality rate ratio of firearm deaths of males ages 15 to 24 years in the U.S., 1979–2007.
Reticence about Firearms among Federal Public Health Agencies
Despite the importance of firearms in mortality statistics, use of terms that describe the vector, including, firearm or gun are absent from the aforementioned 2011 CDC homicide disparities surveillance report.2 Similarly, a 2001 U.S. Surgeon General’s Report on Youth Violence,5 does not list guns as either a risk factor or a protective factor. While this report stresses the need to “[a]ccelerate the decline in gun use by youth in violent encounters,” the contradiction between this need and the absence of guns from the risk spectrum is not addressed. A 2002 report, Best Practices for Youth Violence Prevention6 does mention access to firearms as a risk factor or carrying a weapon as a characteristic of high-risk youth, while focusing on individual and environmental-level interventions.
Perhaps the most striking example of public health silence on the role of firearms is found in a 2009 CDC report titled, The History of Violence as a Public Health Issue.7 There are two gun-related sentences in this history—one that mentions handguns and one with the word, firearms—but the most recent reference cited for these terms is from 1993. Reasons for the apparent gap between 1993 to the publication of the report are not addressed. One of the most significant chapters in the history of violence as a public health issue—Congressional actions in the mid-1990s that targeted the existence of the CDC’s National Center for Injury Prevention and Control—is left out. Specifically, at hearings before the House of Representatives in 1996, gun advocates argued that gun control would do no good and severely criticized CDC-sponsored findings, particularly those of Kellerman,8,9 whose research findings caused him to question the safety of keeping guns in the home.
A more detailed version, as well as the thinking of CDC opponents, is provided by Faria in an article titled, “The tainted public health model of gun control.”10 Faria argues, “Public-health and CDC officials … espoused the preposterous but politically lucrative concept of guns and bullets as animated, virulent pathogens needing to be stamped out by limiting gun availability and ultimately confiscating guns from law-abiding citizens.”[p.39] He points out that “Public-health officials and researchers conveniently neglect the fact that guns and bullets are inanimate objects that do not follow Koch’s Postulates of Pathogenicity (a time-proven, simple, but logical series of scientific steps carried out by medical investigators to definitively prove a microorganism is pathogenic and directly responsible for causing a particular disease). Furthermore, he concludes, “They fail to recognize the importance of individual responsibility and moral conduct—namely, that behind every shooting there is a person pulling the trigger who should be held accountable.”[pp.39–40]
The legislative backlash against the CDC was significant. With the support of powerful politicians such as then-U.S. Senators Robert Dole and Trent Lott, Congress forbade the CDC from spending any funds to “advocate or promote gun control.”9[p.230] According to the legislators, research on direct control of firearms was, “[r]edundant,” in part, because owning a gun is “lawful.”11 Congressional interpretation of the anti-lobbying Law of 1948 made research on gun control itself a felony offence.12
The CDC’s effort to expunge this episode from the record attests to the severity of political arguments and penalties. Today, the CDC’s two major data releases on homicide are those on the nationally representative Wonder site,3,4 and the limited (17-state) NVDRS (National Violent Death Reporting System13). The former is obtained from death certificates, while the latter is a state-based surveillance system that collects facts from different sources about the same incident, including death certificates, police reports, and coroner or medical examiner reports to create a useable, anonymous database. The NVDRS data, however, is “[n]ot analyzed or chosen to provide a representative sample of the United States population and therefore, cannot be generalized to the entire U.S. population. Any changes or fluctuations in rates could be as a result of different demographic or socioeconomic fluctuations in these … states as compared to the entire U.S. population.”13[p.1] Additionally, the CDC has recently issued a report on violence-related firearm deaths, especially among 10 to 19-year old residents of metropolitan areas and cities.14,15 Central cities are identified as problem areas, but racial and ethnic differences are not mentioned. Again, proposed solutions emphasize the need to “[e]ffectively address behaviors that underlie violence among youths,”[p.577] through programs designed to enhance youth skills and motivation to behave non-violently and resolve conflicts peacefully, to promote positive parenting and mentoring and, and to facilitate social connectedness and economic opportunity. Firearms themselves are not mentioned. References to programs that directly address guns include a failed CDC-sponsored program for safe storage of guns, a Department of Justice-funded program directed against street shootings, and a notation that most, “Direct measures” to reduce firearm homicide and suicide have not been adequately evaluated. Congressional action barring the CDC from performing research to evaluate direct measures of firearm control, once again, is not addressed by the report.
Openness about Firearms among Academic Opponents of Gun Control
In contrast to public health officials and those receiving funds from CDC, academicians from criminology, law, and other disciplines have not been constrained from publishing in support of firearms. Several facets of these discussions were summarized in a 2007 review published by the Harvard Journal of Law and Public Policy and written by Donald B. Kates, Jr. and Gary Mauser.16 Kates is a prominent scholar who is also recognized as a tireless and effective advocate for the Second Amendment to the U.S. Constitution, which establishes the right to keep and bear arms.17 Kates has been an outspoken CDC critic.11 Gary Mauser is Professor Emeritus at the Faculty of Business Administration and the Institute for Urban Canadian Research Studies at Simon Fraser University in Burnaby, British Columbia.18 The Harvard Journal of Law and Public Policy, is an internationally A-ranked law journal, in an A*, A, B, C system where A* is the highest rank.19 The high academic standing, not only of the authors but also of the Journal, makes the content of this review particularly disturbing.
In their article, Kates and Mauser argue that murderers are not ordinary citizens: “There is no reason for laws prohibiting gun possession by ordinary, law-abiding responsible adults because such people virtually never murder.”16[p.670] They also review existing data showing negative correlations between gun ownership and violence: “That is ‘where firearms are most dense violent crime rates are lowest, and where guns are least dense, violent crime rates are highest.’”16[p.676] Concerning African Americans, Kates and Mauser state, “Per capita, African-American murder rates are much higher than the murder rate[s] for Whites. If more guns equal more death, and fewer guns equal less, one might assume gun ownership is higher among African-Americans than among Whites, but in fact African-American gun ownership is markedly lower than White gun ownership.”16[p.676] Difficulties in measuring gun ownership aside, Kates and Mauser go on to say (including their italics—p. 677) that murderers are, “A small minority of extreme antisocial aberrants who manage to obtain guns whatever the level of gun ownership in the African American community.”16 “Small minority” notwithstanding, the reader is left to understand that since normal people don’t commit murder and since murder cannot be explained by gun ownership, murder is more common among African Americans for one of two reasons: either “extreme antisocial aberrants” are more common among African Americans or “social aberrants” in the African American community, while not more common, are particularly lethal. Either way, the Kates-Mauser-Harvard logic appears to be built on negative racial stereotyping.
In their review, Kates and Mauser also summarize a negative gun control report from the Task Force on Community Preventive Services,20 stating that, “The CDC is vehemently anti-gun and interpreted its results to show not that the more guns equal more death equation is erroneous, but only that the scores of studies it reviewed were inconclusively done.”16[p.654,n.16] Nonetheless, the assessment of “insufficient evidence” is correct. Studies of prison inmates, for example, may be biased by such factors as declining clearance percentages for homicides on the part of law enforcement agencies. This percentage was about 64% nationally in 2002 (down from 79% in 1976), and it is negatively influenced by factors prevalent in African American communites.21 Moreover, as noted in a later Task Force review22 much available evidence about firearm control law uses ecological data. In particular, both county-level, cross-sectional time series analyses and geographic correlational studies are ecological. While ecological data may be used to generate hypotheses, serious errors can occur when ecological evidence is treated as though it were acceptable for testing hypotheses.23,24 Specifically, knowing whether or not there is a correlation between rates of gun ownership and rates of homicide in a population does not tell the investigator whether individuals with or without guns in a particular community have different risks for homicide. The latter would require individual data rather than grouped (community level) data. This is one reason ecological research is not only considered insufficient by the CDC but also by the U.S. Agency for Health Care Research and Quality (AHRQ), the Oxford Centre for Evidence-based Medicine (OCEBM), and others.25 In summary, when Kates and Mauser promote the importance of low correlations between community rates of gun ownership and community mortality rates from firearms, they are relying weak evidence which is rated unacceptable for evidence-based decision making by major health-related review groups worldwide.
The openness of writers like Faria9 and Kates/Mauser16 regarding African Americans in general and public health in particular, as well as the prestige granted by academic publication, stands in sharp contrast to the reticence of public health agencies. The present authors acknowledge that the old CDC notion of solving the homicide epidemic by “exterminating” guns was off the mark. It represented a medical model that failed to account for societal complexities. Continuing U.S. failures to bring firearm mortality under control in general and among African American youth in particular, however, belie the confidence of CDC critics. Ironically, Faria’s9 support for Koch’s postulates25,26 is conceptually similar (if not identical) to the CDC’s guns as germs model. It is unhelpful, as is the postulation that “[b]ehind every shooting there is a person pulling the trigger who should be held accountable.”9[pp.39–40] Punishing the “person pulling the trigger” has been ineffective in controlling youth violence and offers little support for innocent victims, such as children forced to witness violence.27,28
How Public Health Silence Deprives Vulnerable Populations of Public Health Care
The logic that classifies gun inquiry as “redundant” because guns are legal is difficult to understand. “Legal” and “harmless” are not synonymous, and “legal” and “scientifically valid” can have orthogonal or even opposite meanings. Lawmakers are on record as ignoring even incontrovertible scientific evidence.29 Even evidence that laws themselves may be harmful (for example secondary versus primary automobile safety belt laws) does not preclude their being on the books.30
In most cases, public health practitioners are charged to identify threats to community health and to bring scientific evidence to the attention of policymakers, even if the threats are lawful and whether or not policymakers choose to act on that evidence. Cigarettes are lawful and popular, yet they are estimated to kill 443,000 Americans each year.31,32 Alcohol is lawful and popular, yet it has been estimated to kill more than 75,000 Americans, and to lead to 2.3 million years of potential life lost per year.33 Household cleaning products are lawful and necessary, yet in 2009, they led to more than 220,000 calls to U.S. poison control centers.34 Many other examples could be named, but the point is that if bullets were cigarettes, alcohol, virulent pathogens, household chemicals, or any other potential hazard to U.S. citizens, the full force of epidemiologic and public health practice and research would be brought to bear in an effort to prevent and/or control avoidable damage. Such is not the case for firearms. Finally, the CDC’s coupling of reticence about firearms with its emphasis on strategies to modify violent behavior subtly but clearly echoes the Kates/Mauser mantra that social aberrancy is the root cause of homicide. Intentionally or not, negative racial stereotyping is thereby engrained in the current public health youth violence prevention approach. The ineffectiveness of this approach is evident in Figures 1 and 2, showing that deaths among Black youth continue to be higher than pre-epidemic levels, while disparities continue to grow.
Towards a Comprehensive Public Health Program on Firearms: Surveillance
A comprehensive public health approach to youth violence would require upgrading surveillance of external injuries to youth, and possibly other age groups as part of regular public health medical practice. Again, if bullets were alcohol, cigarettes, viruses, or anything else, the three major epidemics of firearm deaths in the U.S. (1920s–1930s, 1960s–1970s, 1980s–1990s)36 would have left no doubt about the need for better public health surveillance of homicide. Surveillance has made significant contributions to many other health problems. These include classic examples such as infectious disease control during the 20th century,37,38 as well as newer successes such as those reflected by the first 10 years of the Foodborne Diseases Active Surveillance Network (1996–2005)39 as well as recent efforts to control multidrug-resistant hospital infections.40 Reportability has made valuable contributions to the control of birth defects,41,42 and in the arena of chronic disease, the American Heart Association argues that comprehensive, accurate disease surveillance systems are critical for reducing the burden of cardiovascular disease, and it promotes the designation of out-of-hospital cardiac arrest as a reportable illness.43 Although alcohol and cigarette consumption are not reportable per se, regular surveillance activities are also integral to public health control efforts for both.44,45 As noted by Guerrero in a presentation before the National Institute of Medicine on designing violence prevention strategies, “What cannot be measured cannot be administered.”46 Reich et al.47 also call for collaboration among federal, state, public health, and law enforcement agencies to support a national system for reporting violent deaths and injuries and systematic tracing of all guns used in crimes. At a minimum, it will take high-quality science to move from “insufficient evidence” to positive recommendations; high-quality surveillance has repeatedly established its value in this connection.
A recent description of what an effective injury surveillance system might look like has been presented by Mitchell et al.48 Essential data quality characteristics include completeness, sensitivity, specificity, positive predictive value, and representativeness; operational characteristics include system purpose and objectives, data collection process, case definitions, timeliness, quality control, confidentiality, individual privacy, system security, and uniform classification systems; practical characteristics include data accessibility, routine data analysis, and guidance material to aid interpretation and usefulness. Unfortunately, the current state of injury surveillance in the U.S. bears little resemblance to such a system. In the realm of intentional injury, existing surveillance provides little or no information about the location of assaults. It also fails to link of data between victims and offenders, and does not include neighborhood characteristics, or non-fatal injury. Instead, this information is scattered across the records of health care providers, health care institutions, courts, law enforcement agencies, schools, planning departments, and social agencies. This dispersion of information obscures the truth and makes it difficult for communities and professionals alike to draw conclusions.
The problem is made more acute because behavioral outcomes measured within many public health and educational programs exclude the violent crimes they are theoretically meant to address. Gottfredson,49 for example, notes that school-based violence-prevention studies rarely measure serious, violent outcomes. Specifically, only 13 of 138 studies (7%) of school-based crime prevention measured serious crimes committed against people and only 39 (22%) assessed any criminal behavior.49 The Federal Bureau of Investigation’s annual crime reports make this even more perplexing by showing (for the 10 most recent years for which complete data are available, 2000–2009) that in single-victim, single-perpetrator homicides about whom the information is known, 80% (6,015 of 7,053) of homicide victims between 15 and 18 years of age were murdered by people over the age of 18 years.50 So while school-based efforts focus on replicating evidence-based student-to-student bullying and other violence prevention interventions, community (that is, contextual) surveillance shows that most murderers of school age youth are no longer attending school. Conceptually, it is possible to hypothesize that student-to-student programs produce community benefits by sending better prepared cohorts of future 19 to 24 year olds into the world. A more plausible hypothesis, however, is that if youth violence prevention interventions are conducted in isolation from community context, they will be unlikely to yield significant changes in community-level violence. Without good surveillance, however, it is likely that neither hypothesis will be adequately tested.
Finally, poor surveillance helps perpetuate a major flaw that Cochrane Collaborators identify in much public health intervention research. This is the routine attribution of public health outcomes to whatever intervention is being studies. In contrast, the Cochrane Collaborators note that such outcomes might also be due, in whole or in part, to pre-existing contextual community factors. This context, they note, needs to be accounted for and measured as an effect modifier. They conclude, however, that systematic measurements of this type are almost unknown in community- or organization-level randomized trials.51–53 While rarely considered in modern interventional evaluations, older epidemiologic studies show how surveillance can play a key role in separating intervention effects from community context.54,55 Ultimately, poor surveillance makes it difficult for the force that has formed the backbone of many major successes in U.S. mortality reduction during the 20th century—namely triangulation of public health, health care providers, and scientific research56—to be deployed against reduction of youth violence or youth violence-related disparities. Involvement of health care providers, for example by making injuries to youth a medically reportable disease, and empowering the linkage of information from hospitals, courts, schools, and other institutions in a single repository to be made fully available to local communities would go a long way to improve the current system. It might also provide sufficient individual-level information to overcome the aforementioned weaknesses of ecological data.
Towards a Comprehensive Public Health Program on Firearms: Neutralization
While surveillance and free inquiry are needed, it is clear that gun control is not the only issue for homicide, any more than vector control is the only issue for infectious diseases. Although easy availability of drugs, alcohol and firearms have been identified by many as important risk factors for risk of injury from violence,57 protective factors include good nutrition and health care; school attendance and connectedness; family connectedness; public service infrastructure; opportunities for participation in social, political, and economic life; and the availability of service organizations and neighborhood groups,5,57 all of which might help to rectify what Wright and Sheley have called root conditions of youth violence, namely those, “‘That breed hostility, estrangement, futility and hopelessness.’”58,59[p.669] Clearly, major societal changes are needed if major changes in youth violence are to follow.
Because such societal changes occur slowly over time, however, concurrent efforts with the potential to bring about more rapid change are also needed. Again, interventions based on classic epidemiologic principles might be useful. Neutralization of harmful agents has been widely successful, exemplified by vaccination against infectious diseases and modification of cigarette paper to reduce accidental deaths from fires caused when people fall asleep while smoking.60 Just as ways have been developed to defuse viruses and make cigarettes safer, it is reasonable to expect that scientists might develop safer weapons. Teret and Culross,61 for example, suggest that in many cases, the technology for making guns safer already exists. They add that prior experience in injury prevention suggests that changing product design is likely to be more effective than behavior change, and conclude that opposition to change among gun makers themselves is among the most important barriers to progress. Finally, if safer weapons were available, it would also take community engagement to make them successful62—another role in which public health agencies can be effective.56
Conclusions
For more than a decade, public health positions on firearm mortality among youth have been dominated by backlash to a medical model which inappropriately equated guns with germs needing extermination. As a result, the public health response to youth homicide has been shaped, in part, by a social ecology of negative racial stereotyping and an ideology that equates the right to bear arms with the right to bear unsafe arms. Both support a business status quo which promotes the profits of those who manufacture unsafe weapons. Public health services to protect against youth homicide that might have delivered to some this nation’s most vulnerable populations are severely compromised. If the U.S. aims to reduce Black-White disparities in youth homicide, there is a need for a new ecology based on more refined theories of epidemiology, such as those recently detailed by Krieger;63 better understandings of needed social change, including those provided by aforementioned citations from the U.S. Surgeon General5 and the World Bank;57 and effective use of proven public health approaches such as surveillance and neutralization. It is time for public health providers, public health academicians, and professional public health organizations to defend more vigorously their role in reducing racially disparate Black-White youth violence homicide rates involving firearms.
Notes
- 1.Richardson EG, Hemenway D. Homicide, suicide, and unintentional firearm fatality: comparing the United States with other high-income countries, 2003. J Trauma. 2011 Jan;70(1):238–243. doi: 10.1097/TA.0b013e3181dbaddf. [DOI] [PubMed] [Google Scholar]
- 2.Logan JE, Smith SG, Stevens MR, et al. Homicides—United States, 1999–2007. MMWR Surveill Summ. 2011 Jan;60(Suppl):67–70. [PubMed] [Google Scholar]
- 3.Centers Disease Control and Prevention/National Center for Health Statistics. Compressed mortality data: 1999–2007. Hyattsville, MD: Centers Disease Control and Prevention/National Center for Health Statistics; Available at: http://wonder.cdc.gov/cmf-icd10.html. [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention/National Center for Health Statistics. Compressed mortality file 1979–1998. Hyattsville, MD: Centers for Disease Control and Prevention/National Center for Health Statistics; Available at: http://wonder.cdc.gov/cmf-icd9.html. [Google Scholar]
- 5.U.S. Public Health Service. Youth violence: a report of the Surgeon General. Rockville, MD: U.S. Public Health Service; 2001. Available at: http://www.surgeongeneral.gov/library/youthviolence/ [Google Scholar]
- 6.Thornton TN, Craft CA, Dahlberg LL, et al., editors. Best practices of youth violence prevention: a sourcebook for community action. Atlanta, GA: Centers for Disease Control and Prevention/National Center for Injury Prevention and Control; 2000. [Google Scholar]
- 7.Dahlberg LL, Mercy JA. History of violence as a public health issue. AMA Virtual Mentor. 2009 Feb;11(2):167–172. doi: 10.1001/virtualmentor.2009.11.2.mhst1-0902. [DOI] [PubMed] [Google Scholar]
- 8.Kellermann AL, Rivara FP, Rushforth NB, et al. Gun ownership as a risk factor for homicide in the home. N Engl J Med. 1993 Oct;329(15):1084–1091. doi: 10.1056/NEJM199310073291506. [DOI] [PubMed] [Google Scholar]
- 9.Gallant P, Eisen JD, Kellerman Arthur L. In: Guns in American society: an encyclopedia of history, politics, culture, and law. Carter GL, editor. Santa Barbara, CA: ABC-CLIO, Inc.; 2002. pp. 329–331. (1955–). [Google Scholar]
- 10.Faria MA., Jr The tainted public health model of gun control. Freeman. 2001;51(4):38–43. [Google Scholar]
- 11.Kates D, Schaffer HE, Waters WB., IV . Public health pot shots: how the CDC succumbed to the gun “epidemic”. Los Angeles, CA: Reason; 1997. Apr. Available at: http://reason.com/archives/1997/04/01/public-health-pot-shots. [Google Scholar]
- 12.Levine RS, Rust G, Pisu M, et al. Increased Black-White disparities in mortality following lifesaving innovations: a possible consequence of U.S. federal laws. Am J Public Health. 2010 Nov;100(11):2176–2184. doi: 10.2105/AJPH.2009.170795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention. National violent death reporting system. Atlanta, GA: Centers for Disease Control and Prevention; 2008. Nov. Available at: http://www.cdc.gov/ncipc/wisqars/NVDRS/About-NVDRS. [Google Scholar]
- 14.Kegler SR, Annest JL, Kresnow M, et al. Violence-related firearm deaths among residents of metropolitan areas and cities—United States, 2006–2007. MMWR. 2011 May 13;60(18):573–578. [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention/Morbidity and Mortality Weekly Report/Anonymous. Editorial note. MMWR. 2011 May;60(18):577–578. Available at: http://www.cdc.gov/mmwr/PDF/wk/mm6018.pdf. [Google Scholar]
- 16.Kates DB, Mauser G. Would banning firearms reduce murder and suicide? A review of international and some domestic evidence. Harvard J Law Public Policy. 2007;30(2):649–694. [Google Scholar]
- 17.Kopel DB, Kates Don B., Jr . In: Guns in American society: an encyclopedia of history, politics, culture, and law. Carter GL, editor. Santa Barbara, CA: ABC-CLIO, Inc.; 2002. pp. 327–329. (1941–). [Google Scholar]
- 18.Mauser G. Gary Mauser. British Columbia, Canada: GaryMauser.net; 2011. Apr. Available at: http://www.garymauser.net/. [Google Scholar]
- 19.Australian Government/Australian Research Council. Journal ranking. Melbourne, Australia: Australian Research Council; 2010. [Google Scholar]
- 20.Hahn RA, Bilukha OO, Crosby A, et al. First reports evaluating the effectiveness of strategies for preventing violence: firearms laws. (Findings from the Task Force on Community Preventive Services.) MMWR Recomm Rep. 2003 Oct;52(RR-14):11–20. [PubMed] [Google Scholar]
- 21.Cronin JM, Murphy GR, Spahr LL, et al. Promoting effective homicide investigations. Washington, DC: Police Executive Research Forum/Community Oriented Policing Services; 2007. Available at: http://www.policeforum.org/library/homicide/homicide.pdf. [Google Scholar]
- 22.Centers for Disease Control and Prevention/Office of Surveillance, Epidemiology and Laboratory Services. The community guide to community preventive services: firearms laws. Atlanta, GA: The Community Guide; 2010. Mar. Available at: www.thecommunityguide.org/violence/firearmlaws.html. [Google Scholar]
- 23.Freedman DA. Ecological inference and the ecological fallacy. Int Encyclopedia Soc Behav Sci. 1999 Oct;549 Available at: http://www.stanford.edu/class/ed260/freedman549.pdf. [Google Scholar]
- 24.Greenland S, Robins J. Invited commentary: ecologic studies—biases, misconceptions, and counter-examples. Am J Epidemiol. 1994 Apr;139(8):747–760. doi: 10.1093/oxfordjournals.aje.a117069. [DOI] [PubMed] [Google Scholar]
- 25.Atkins D, Eccles M, Flottorp S, et al. Systems for grading the quality of evidence and the strength of recommendations I: critical appraisal of existing approaches. (The Grade Working Group.) BMC Health Serv Res. 2004 Dec;4(1):38. doi: 10.1186/1472-6963-4-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rothman KJ. Causes. Am J Epidemiology. 1976 Jan;104(2):587–592. doi: 10.1093/oxfordjournals.aje.a112335. [DOI] [PubMed] [Google Scholar]
- 27.Rothman KJ, Greenland S. Causation and causal inference in epidemiology. Am J Public Health. 2005 Jul;95(Suppl 1):S144–S150. doi: 10.2105/AJPH.2004.059204. [DOI] [PubMed] [Google Scholar]
- 28.Groves BM, Zuckerman B, Marans S, et al. Silent victims: children who witness violence. JAMA. 1993 Jan;269(2):262–264. [PubMed] [Google Scholar]
- 29.Slovak K. Gun violence and children: factors related to exposure and trauma. Health Soc Work. 2002 May;27(2):104–112. doi: 10.1093/hsw/27.2.104. [DOI] [PubMed] [Google Scholar]
- 30.Oakely GP., Jr The scientific basis for eliminating folic acid–preventable spina bifida: a modern miracle from epidemiology. Ann Epidemiol. 2009 Apr;19(4):226–230. doi: 10.1016/j.annepidem.2009.01.016. [DOI] [PubMed] [Google Scholar]
- 31.Burris S, Wagenaar AC, Swanson J, et al. Making the case for laws that improve health: a framework for public health law research. Milbank Q. 2010 Jun;88(2):169–210. doi: 10.1111/j.1468-0009.2010.00595.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Centers for Disease Control and Prevention. Smoking-attributable mortality, years of potential life lost, and productivity losses—United States, 2000–2004. MMWR Morb Mortal Wkly Rep. 2008 Nov;57(45):1226–1228. [PubMed] [Google Scholar]
- 33.National Center for Health Statistics. Health: United States, 2010: with special feature on death and dying. Hyattsville, MD: National Center for Health Statistics; 2011. [PubMed] [Google Scholar]
- 34.Centers for Disease Control and Prevention. Alcohol-attributable deaths and years of potential life lost—United States, 2001. MMWR Morb Mortal Wkly Rep. 2004 Sep;53(37):866–870. [PubMed] [Google Scholar]
- 35.Bronstein AC, Spyker DA, Cantilena LR, Jr, et al. 2009 annual report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 27th annual report. Clin Toxicol (Phila) 2010 Dec;48(10):979–1178. doi: 10.3109/15563650.2010.543906. [DOI] [PubMed] [Google Scholar]
- 36.Christoffel KK. Firearm injuries: epidemic then, endemic now. Am J Public Health. 2007 Apr;97(4):626–629. doi: 10.2105/AJPH.2005.085340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.National Center for Environmental Health/National Center for Health Statistics/National Center for Infectious Diseases/Centers for Disease Control and Prevention. Achievements in public health, 1900–1999: control of infectious diseases. MMWR Morb Mortal Wkly Rep. 1999 Jul;48(29):621–629. [Google Scholar]
- 38.Hutchins SS, Fiscella K, Levine RS, et al. Protection of racial and ethnic minority populations during an influenza pandemic. Am J Pub Health. 2009 Oct;99(Suppl 2):S261–S270. doi: 10.2105/AJPH.2009.161505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Scallan E. Activities, achievements, and lessons learned during the first 10 years of the foodborne diseases active surveillance network: 1996–2005. Clin Infect Dis. 2007 Mar;44(5):718–725. doi: 10.1086/511648. [DOI] [PubMed] [Google Scholar]
- 40.Muto CA, Jernigan JA, Ostrowsky BE, et al. SHEA guideline for preventing nosocomial transmission of multidrug-resistant strains of Staphylococcus aureus and enterococcus. Infect Control Hosp Epidemiol. 2003 May;24(5):362–386. doi: 10.1086/502213. [DOI] [PubMed] [Google Scholar]
- 41.Oakley GP., Jr Population and case-control surveillance in the search for environmental causes of birth defects. Public Health Rep. 1984 Sep-Oct;99(5):465–468. [PMC free article] [PubMed] [Google Scholar]
- 42.Sever LE, editor. Guidelines for conducting birth defects surveillance. Atlanta, GA: National Birth Defects Prevention Network Inc.; 2004. Jun. Available at: http://www.nbdpn.org/docs/NBDPN_Guidelines2008.pdf. [Google Scholar]
- 43.Nichol G, Rumsfeld J, Eigel B, et al. Essential features of designating out-of-hospital cardiac arrest as a reportable event. Circulation. 2008;117(17):2299–2308. doi: 10.1161/CIRCULATIONAHA.107.189472. [DOI] [PubMed] [Google Scholar]
- 44.Chen CM, Yi H-y, Faden VB. Surveillance report #91: trends in underage drinking in the United States, 1991–2009. Bethesda, MD: Office of Science Policy and Communications/National Institute on Alcohol Abuse and Alcoholism; 2011. Mar. Available at: http://pubs.niaaa.nih.gov/publications/surveillance91/Underage09.pdf. [Google Scholar]
- 45.Trinidad DR, Pérez-Stable EJ, White MM, et al. A nationwide analysis of U.S. racial/ethnic disparities in smoking behaviors, smoking cessation, and cessation-related factors. Am J Public Health. 2011 Apr;101(4):699–706. doi: 10.2105/AJPH.2010.191668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Guerrero R. Importance of information for designing violence prevention strategies: workshop on violence prevention in low- and middle-income countries. Washington, DC: Institute of Medicine; 2007. Jun. Available at : http://www.iom.edu/~/media/Files/Activity%20Files/Global/GlobalViolencePrev/ViolenceWSPGuerrero.pdf. [Google Scholar]
- 47.Reich K, Culross PL, Behrman RE. Children, youth, and gun violence: analysis and recommendations. Future Child. 2002 Summer-Fall;12(2):4–23. [PubMed] [Google Scholar]
- 48.Mitchell RJ, Williamson AM, O’Connor R. The development of an evaluation framework for injury surveillance systems. BMC Public Health. 2009;9:260. doi: 10.1186/1471-2458-9-260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gottfredson DC. Some thoughts about research on youth violence prevention. Am J Prev Med. 2007 Aug;33(2 Suppl):S104–S106. doi: 10.1016/j.amepre.2007.04.021. [DOI] [PubMed] [Google Scholar]
- 50.The Federal Bureau of Investigation. Uniform crime reports: crime in the United States—1995 to 2010. Washington, DC: Federal Bureau of Investigation; 2011. Available at: http://www.fbi.gov/about-us/cjis/ucr/ucr. [Google Scholar]
- 51.Hawe P, Shiell A, Riley T, et al. Methods for exploring implementation variation and local context within a cluster randomized community intervention trial. J Epidemiol Community Health. 2004 Sep;58(9):788–793. doi: 10.1136/jech.2003.014415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Eccles M, Grimshaw J, Campbell M, et al. Research designs for studies evaluating the effectiveness of change and improvement strategies. Qual Saf Health Care. 2003 Feb;12(1):47–52. doi: 10.1136/qhc.12.1.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Armstrong R, Waters E, Doyle J, Higgins JPT, Green S, editors. Cochrane handbook for systematic reviews of interventions (Chapter 21) Oxfordshire, United Kingdom: The Cochrane Collaboration; Reviews in public health and health promotion; pp. 593–606. [Google Scholar]
- 54.Chin TDY, Marine W. The changing pattern of poliomyelitis observed in two urban epidemics. Public Health Reports. 1961 Jul;76(7):553–564. [PMC free article] [PubMed] [Google Scholar]
- 55.Landrigan PJ. Epidemic measles in a divided city. JAMA. 1972 Aug;221(6):567–570. [PubMed] [Google Scholar]
- 56.Rust G, Satcher D, Fryer GE, et al. Triangulating on success: innovation, public health, medical care and cause-specific U.S. mortality rates over a half century (1950–2000) Am J Pub Health. 2010 Apr;100(Suppl 1):S95–S104. doi: 10.2105/AJPH.2009.164350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.The World Bank/Social Development Department/Conflict, Crime, and Violence Team. Violence in the city: understanding and supporting community responses to urban violence. Washington, DC: The World Bank; 2011. Apr. Available at: http://siteresources.worldbank.org/EXTSOCIALDEVELOPMENT/Resources/244362-1164107274725/Violence_in_the_City.pdf. [Google Scholar]
- 58.Kopel DB, Wright James D. In: Guns in American society: an encylopedia of history, politics, culture, and the law (Vol. 2: M–Z) Carter GL, editor. Santa Barbara, CA: ABC-CLIO Inc.; 2002. pp. 667–669. (1947–). [Google Scholar]
- 59.Wright JD, Sheley J. Teenage violence and the underclass. Peace Review. 1992 Fall;4(3):32–35. [Google Scholar]
- 60.Goldstein AO, Grant E, McCullough A, et al. Achieving fire-safe cigarette legislation through coalition-based legislative advocacy. Tob Control. 2010 Feb;19(1):75–79. doi: 10.1136/tc.2009.029538. [DOI] [PubMed] [Google Scholar]
- 61.Teret SP, Curloss PL. Product-oriented approaches to reducing youth gun violence. Future Child. 2002 Summer-Fall;12(2):118–131. [PubMed] [Google Scholar]
- 62.Nation M, Bess K, Voight A, et al. Levels of community engagement in youth violence prevention: the role of power in sustaining successful university-community partnerships. Am J Community Psychol. 2011 Sep;48(1–2):89–96. doi: 10.1007/s10464-010-9414-x. [DOI] [PubMed] [Google Scholar]
- 63.Krieger N. Epidemiology and the people’s health: theory and context. New York, NY: Oxford University Press; 2011. [Google Scholar]