Abstract
The current investigation explored the main and interactive effects of anxiety sensitivity (AS) and state anxiety in predicting acute nicotine withdrawal symptoms experienced during the initial 14 days of smoking cessation. Participants included 123 adult daily smokers (84 women; Mage = 45.93 years, SD = 10.34) undergoing psychosocial-pharmacological cessation treatment. Results indicated that after controlling for the effects of participant sex and nicotine dependence, state anxiety, but not AS, significantly predicted initial levels of nicotine withdrawal symptoms. Results also demonstrated that both state anxiety and AS were significantly related to the change in nicotine withdrawal symptoms over time. Finally, our results revealed a significant interaction between AS and state anxiety. Specifically, higher levels of AS were associated with a stronger relation between state anxiety and nicotine withdrawal symptoms experienced during the cessation attempt. Results suggest that among high AS persons, state anxiety may be more relevant, compared to those low in AS, in regard to experiencing withdrawal symptoms as more intense during the early phases of quitting.
Keywords: Tobacco, Smoking, State Anxiety, Anxiety Sensitivity, Nicotine Withdrawal, Smoking Cessation
Anxiety sensitivity (AS), defined as the extent to which individuals believe anxiety and anxiety-related sensations have harmful consequences (McNally, 2002; Reiss & McNally, 1985), is a relatively stable, yet malleable, cognitive characteristic that predisposes individuals to the development and maintenance of anxiety psychopathology (Reiss & Havercamp, 1996). Historically, AS has been studied in relation to better understanding the etiology and maintenance of anxiety and its disorders, particularly panic and posttraumatic stress disorder (Hayward, Killen, Kraemer, & Taylor, 2000; Li & Zinbarg, 2007; Maller & Reiss, 1992; Marshall, Miles, & Stewart, 2010; Schmidt, Keough et al., 2010; Schmidt, Lerew, & Jackson, 1997, 1999; Schmidt, Zvolensky, & Maner, 2006). More recent work has suggested that AS also may play a role in certain substance use disorders (Lejuez, Paulson, Daughters, Bornovalova, & Zvolensky, 2006; Norton, Rockman, Luy, & Marion, 1993; Stewart, Karp, Pihl, & Peterson, 1997; Stewart & Kushner, 2001).
One emerging and promising line of inquiry within this substance use domain has focused on the relation between AS and cigarette smoking. Here, research has indicated that this cognitive factor is related to important aspects of smoking behavior. For example, AS is positively correlated with smoking to reduce negative affect, but often not other smoking motives (e.g., pleasure, handling, taste; Battista, Stewart, Fulton et al., 2008; Comeau, Stewart, & Loba, 2001; Leyro, Zvolensky, Vujanovic, & Bernstein, 2008; Novak, Burgess, Clark, Zvolensky, & Brown, 2003; Stewart et al., 1997; Zvolensky, Bonn-Miller, Bernstein, & Marshall, 2006). Other studies have found that AS is related to smoking negative affect reduction expectancies (beliefs smoking will reduce negative affect; Brown, Kahler, et al., 2001; Gregor, Zvolensky, McLeish, Bernstein, & Morissette, 2008). Additionally, smokers high in AS perceive the prospect of quitting as both a more difficult and personally threatening experience (Zvolensky et al., 2007), possibly due to a hypersensitivity to aversive internal sensations such as nicotine withdrawal symptoms (Zvolensky et al., 2004) or elevated state anxiety (Mullane, Stewart, Rhyno, Steeves, Watt, & Eisner, 2008; Vujanovic & Zvolensky, 2009). Perhaps most notably, AS is significantly associated with less success during smoking cessation attempts (Zvolensky & Bernstein, 2005). Specifically, higher levels of AS are related to greater odds of early lapse (Brown, Kahler, Zvolensky, Lejuez, & Ramsey, 2001) and relapse during quit attempts (Zvolensky, Bernstein et al., 2007; Zvolensky, Bonn-Miller et al., 2006; Zvolensky, Stewart, Vujanovic, Gavric, & Steeves, 2009); these effects are not explained by smoking rate or nicotine dependence, nicotine withdrawal symptoms, or trait-like negative mood propensity (Zvolensky et al., 2009).
There is a limited body of work that suggests AS may be related to the severity of nicotine withdrawal symptoms (i.e., symptoms emerging from drug reduction in the body; Hughes, Higgins, & Hatsukami, 1990). One early, retrospective account of smokers’ most recent cessation attempt found that AS was significantly related to severity of withdrawal symptoms (Zvolensky et al., 2004). A subsequent, prospective study, did not find a significant association between AS and nicotine withdrawal symptom severity experienced during the first two weeks of cessation (Mullane et al., 2008). In that study, smokers undergoing psychosocial-pharmacological smoking cessation treatment were instructed to complete ratings of nicotine withdrawal symptoms, every other day, for two weeks (Mullane et al., 2008). These ratings were averaged across each of the two weeks to generate an average score for week one and week two, respectively (Mullane et al., 2008). Results demonstrated that AS was not significantly related to average ratings of nicotine withdrawal symptoms experienced during week one, nor week two (Mullane et al., 2008). More recently, Marshall and colleagues (2009) examined AS in relation to levels of acute nicotine withdrawal symptoms experienced in the first 24 hours after quit day during a self-guided quit attempt (Marshall, Johnson, Bergman, Gibson, & Zvolensky, 2009). Results of this study indicated that higher levels of AS were significantly related to greater severity of nicotine withdrawal symptoms experienced on quit day (Marshall et al., 2009).
Although available work on the association between AS and nicotine withdrawal symptom severity is promising, it is limited in a number of formative ways. First, past prospective study findings have not been fully consistent (Marshall et al., 2009; Mullane et al., 2008), possibly owing to methodological differences between studies (e.g., delivery of an ’active’ intervention versus a self-guided quit attempt without any psychosocial or pharmacological aids, assessment of withdrawal at different time points). Moreover, the cross-sectional investigation employed a retrospective measure of past withdrawal symptoms (Zvolensky et al., 2004), possibly involving reporting error due to recall or memory biases (McNally, 1996). To help clarify the nature of past discrepant findings and limitations of retrospective recall, it would be advisable to evaluate nicotine withdrawal prospectively during a cessation attempt with an active intervention and directly monitor the effect of AS on the experience of withdrawal symptoms over time.
Second, although one study did investigate AS in terms of nicotine withdrawal symptom severity across time (Mullane et al., 2008), this study did not explore how AS relates to change in withdrawal symptoms throughout the course of quitting during evidenced-based care. Such neglect is unfortunate as past work indicates that the nature and course of withdrawal symptoms often fluctuate over time (Hughes, 1992; Piasecki et al., 1997). Thus, an important extension of existing work would be to examine the role of AS in relation to a) the average level of withdrawal symptoms experienced at specified time points (e.g., baseline); and b) the rate and direction of change in withdrawal symptoms experienced throughout the duration of smoking treatment. Here, current theory suggests that individuals with high levels of AS might experience nicotine withdrawal as more severe due to a fear of the negative consequences of internal sensations (e.g., abrupt affective and bodily sensations; e.g., Zvolensky & Bernstein, 2005). For example, it may be that “high AS” smokers are more likely to avoid or suppress the distressing affective and physical sensations characteristic of smoking cessation. This type of avoidance process may contribute to a higher level of “maintained” nicotine withdrawal symptoms (i.e., withdrawal symptoms will not naturally decrease over time).
Finally, AS may theoretically interplay with negative mood states such as state anxiety to exacerbate nicotine withdrawal symptom intensity (Stewart & Kushner, 2001). For example, non-smoking research has found that the combination of elevated AS and state anxiety, relative to other combinations, can increase the future risk for anxiety psychopathology (Schmidt & Zvolensky, 2007). Other empirical research documenting profiles of nicotine withdrawal has found that measures of negative affect closely parallel withdrawal symptoms over time (Piasecki, Fiore & Baker, 1998). Specifically, changes in negative affect result in simultaneous changes in withdrawal symptom severity (Piasecki et al., 1998). Thus, there is utility in exploring the main and interactive effects of AS and state anxiety symptoms in terms of the expression of more severe nicotine withdrawal symptoms. Consistent with this theoretical framework, high AS individuals who simultaneously experience elevated levels of state anxiety during periods of smoking deprivation may become emotionally reactive to such stimuli (Zvolensky & Bernstein, 2005). Therefore, this subset of smokers may be more apt to perceive nicotine withdrawal symptoms as more intense or personally threatening (e.g., “I am losing control”).
Together, the overarching aim of the present investigation was to examine the main and interactive effects of AS and state anxiety in predicting the severity of acute nicotine withdrawal symptoms assessed daily during the first two weeks of a quit attempt among daily smokers receiving evidenced-based smoking cessation treatment. We chose to focus our analyses on the initial 14 days of the cessation attempt as previous research has documented that individuals high in AS are at an increased risk for early smoking lapse and relapse (i.e., within 2-weeks post-quit; Zvolensky et al., 2009). Drawing from theoretical models (Zvolensky & Bernstein, 2005) and extant empirical studies (Marshall et al., 2009; Mullane et al., 2008; Zvolensky et al., 2004), which suggest that high AS individuals are more apt to be fearful of and emotionally reactive to, internal states that occur during smoking discontinuation, and consequently, tend to experience more distressing emotional experiences in their attempts to quit, we developed three interrelated sets of hypotheses.
First, it was hypothesized that higher baseline levels of AS would be associated with: a) more severe withdrawal symptoms experienced at assessment 1 (i.e., baseline); and b) a significantly slower decrease in withdrawal symptoms throughout the initial two weeks of cessation. Second, it was hypothesized that a) the initial (average) levels of state anxiety would be significantly and positively related to initial levels of nicotine withdrawal symptoms; and b) daily deviations in state anxiety would be significantly associated with simultaneous changes (increases/decreases) in the severity of acute nicotine withdrawal symptoms experienced over time. This set of hypotheses was based on evidence that negative mood may influence the onset and course of nicotine withdrawal symptoms (Piasecki et al., 1997). Finally, it was hypothesized that the observed relations between state anxiety (both average and daily deviations) and nicotine withdrawal symptoms would be moderated by AS, such that state anxiety will be more strongly related to withdrawal symptoms for those with high levels of AS, than for those with low levels of AS. That is, high AS individuals may react more negatively to the interoceptive sensations (i.e., nicotine withdrawal) experienced during smoking deprivation, thereby producing more severe anxiety and nicotine withdrawal symptoms.1
Method
Participants
Participants included 123 daily cigarette smokers (84 women; Mage = 45.93 years, SD = 10.34) living in the Halifax Regional Municipality, in the Canadian province of Nova Scotia. Daily smokers were recruited for participation from among those attending a structured four-week group Tobacco Intervention Program offered through Addiction Prevention and Treatment Services, Capital District Health Authority. All of those daily smokers participating in the Program were invited to participate. Participants reported attaining the following levels of education: 41% completed high school, 31% completed college (community college or technical schooling), 13% completed university (traditional four-year schooling), 11% completed junior high school, and 4% completed elementary school. With regard to marital/relationship status, 48% of the sample reported being married/cohabiting with a partner, 35% reported being separated/divorced/widowed, and 17% reported being single.
Participants reported smoking an average of 15.46 (SD = 7.95) cigarettes per day and endorsed relatively high levels of nicotine dependence (M = 6.25, SD = 2.17), as indexed by the Fagerström Test for Nicotine Dependence (FTND; Fagerström, 1978; Heatherton, Kozlowski, Frecker, & Fagerstrom, 1991) at treatment outset. Participants reported initiating daily smoking at a mean age of 16.60 years of age (SD = 4.77) and smoking regularly for an average of 28.28 years (SD = 10.64). In terms of smoking cessation, participants endorsed an average of 2.95 (SD = 2.85) ‘serious’ lifetime quit attempts, and 5.77 (SD = 12.57) lifetime quit attempts lasting longer than 12 hours in duration. The average longest lifetime period of smoking abstinence after a quit attempt among participants was 1.14 years (SD = 2.74).
Measures
Smoking History Questionnaire (SHQ; Brown, Lejuez, Kahler, & Strong, 2002)
The SHQ is a self-report questionnaire used to assess smoking history and pattern. The SHQ includes items pertaining to smoking rate, age of onset of smoking initiation, and years of being a daily smoker. The SHQ has been successfully used in previous studies as a measure of smoking history (e.g., Zvolensky, Lejuez, Kahler, & Brown, 2004).
Fagerström Test for Nicotine Dependence (FTND; Fagerström, 1978; Heatherton et al., 1991)
The FTND is a six-item scale designed to assess gradations in tobacco dependence (Heatherton et al., 1991). The FTND has shown good internal consistency, positive relations with key smoking variables (e.g., saliva cotinine; Heatherton et al., 1991), and high degrees of test-retest reliability (Pomerleau, Carton, Lutzke, Flessland, & Pomerleau, 1994).
Minnesota Nicotine Withdrawal Scale (MNWS; Hughes & Hatsukami, 1986)
Nicotine withdrawal symptom severity was assessed daily for the initial 14-days of the cessation attempt using the MNWS, a reliable and sensitive nine-item scale (Hughes & Hatsukami, 1986). Participants were asked to rate daily, to what extent they experienced each symptom associated with nicotine withdrawal (e.g., craving, irritability), using a four-point Likert-type scale (0 = not present to 3 = severe). This measure has been successfully employed in previous smoking cessation research to capture withdrawal dynamics, including negative affect symptoms (Piasecki et al., 2000); further, it allows for the assessment of the frequency, duration, severity, and temporal variability of withdrawal symptoms experienced over time.
Anxiety Sensitivity Index (ASI; Reiss, Peterson, Gursky, & McNally, 1986)
To assess sensitivity to, and discomfort with, anxiety and related internal states, the 16-item ASI was employed. The ASI is a self-report measure on which respondents indicate, on a five-point Likert-style scale, the degree to which they fear the potential negative consequences of anxiety-related symptoms and sensations. The ASI is unique from, and demonstrates incremental predictive validity relative to, trait anxiety (McNally, 2002) and negative affectivity (Zvolensky, Kotov, Antipova, & Schmidt, 2005). Based upon previous psychometric work employing Item Response Theory, the current investigation utilized twelve of the sixteen ASI items, which have demonstrated the strongest capacity to discriminate between and provide information about various latent levels of anxiety sensitivity among smokers (Zvolensky, Strong, Bernstein, Vujanovic, & Marshall, 2009). Specifically, the following twelve items were used in the present investigation to calculate the total ASI score: (2 = “When I cannot keep my mind on a task, I worry that I might be going crazy;” 3 = “It scares me when I feel shaky;” 4 = “It scares me when I feel faint;” 6 = “It scares me when I my heart beats rapidly;” 8 = “It scares me when I am nauseous;” 10 = “It scares me when I become short of breath;” 11 = “When my stomach is upset, I worry that I might be seriously ill;” 12 = “It scares me when I am unable to keep my mind on a task;” 13 = “Other people notice when I feel shaky;” 14 = “Unusual body sensations scare me;” 15 = “When I am nervous, I worry that I might be mentally ill;” and 16 = “It scares me when I am nervous”). However, the following four items were not used to compute the total ASI score in the present analyses as they have previously demonstrated poor discriminant abililities: (1 = ;”It is important not to appear nervous;” 5 = “It is important to me to stay in control of my emotions;” 7 = “It embarrasses me when my stomach growls;” and 9 = “When I notice my heart beating rapidly, I worry that I might be having a heart attack”). It should be noted that the majority of these excluded items represent social concerns (Zvolensky et al., 2009).
State-Trait Anxiety Inventory (STAI; Spielberger, Gorsuch & Lushene, 1970)
The STAI is a 40-item self-report measure of state- and trait-level anxiety. In the present investigation, only the 20-items pertaining to state anxiety (e.g., “I am tense”) were used. Participants were asked to rate daily, during the initial 14-days of the cessation attempt, the degree to which they experienced each symptom of anxiety, in the moment. Ratings were made using a four-point Likert-type scale (1= not at all to 4 = very much so). This measure of state anxiety has been used extensively in previous research and has consistently demonstrated good psychometric properties (Spielberger, Gorsuch, & Lushene, 1983).
Procedure
The present study is a facet of a larger investigation (Zvolensky, Stewart et al., 2009). The current analyses have not been reported previously and therefore represent a novel contribution to the existing literature. The procedure of the study has been described in detail elsewhere (Zvolensky et al., 2009). The initial phase of this study recruited smokers attending an information session about the Tobacco Intervention Program offered through Capital Health. Potential participants were informed about the nature and purpose of the study and were then invited to participate in the research portion of the program. Any smoker interested in participating in the current investigation was enrolled (i.e., there was no exclusionary criteria); however, only those individuals endorsing moderate (or higher) nicotine dependence and those deemed medically appropriate for Nicotine Replacement Therapy (NTR) were offered the free NTR (please see below for an expanded discussion of compensation).
The smoking cessation program began approximately two weeks after the information session. During the first session, participants completed a demographics questionnaire and the SHQ, FTND, and ASI. In addition, participants were offered the chance to receive NRT. The program consisted of one 90-minute group session per week for four weeks, including clinical time (one hour) as well as the time for the research component (half an hour). Each session was delivered by a trained addictions counselor. The manualized treatment included both evidence-based behavioral and cognitive strategies and NRT. During this program, participants selected their own quit date within the four week window of treatment. Participants were then instructed to complete the MNWS and STAI daily for the initial 14-days of the cessation attempt. Specifically, participants were instructed to rate their overall symptoms of nicotine withdrawal and state anxiety, beginning on quit day, and continuing daily for the first two weeks following quit day. Participants were given the flexibility of completing their ratings at any point during the day, as long as the ratings were made on a daily basis. The intervention and a four-week supply of NRT were provided to program participants free of charge. Moreover, all participants were provided with a $10 movie pass as compensation for participation in the research.
Data Analytic Strategy
Longitudinal multi-level modeling (MLM), employing the program HLM 6.06 (Raudenbush & Bryck, 2002), was used to analyze the present data. MLM was chosen to perform the present analyses as it: 1) includes all participants, regardless of missing data; 2) allows for different numbers of assessments for different subjects; and, 3) is the preferred analytic tool for examining longitudinal psychiatric data (Hamer & Simpson, 2009). In the current investigation, the criterion variable was severity of nicotine withdrawal symptoms (MNWS; assessed daily during the initial 14-days of the cessation attempt). In the first set of analyses, we examined the overall growth curve of nicotine withdrawal symptoms, as well as how other potentially important variables (participant sex, anxiety sensitivity [ASI], and nicotine dependence [FTND]) are related to the growth curve of nicotine withdrawal symptoms over time. Next, we assessed whether state anxiety (STAI; assessed daily during the initial 14-days of the cessation attempt) significantly predicted the severity of nicotine withdrawal symptoms over time. Given our hypothesis that AS would moderate the relation between state anxiety and the severity of nicotine withdrawal symptoms, the interaction between AS and state anxiety was included as a central component in the model. All predictors (except Time and participant sex) were centered at their means for the initial set of analyses. Since the intercept in growth curve analysis represents the level of withdrawal symptoms at Time = 0, Time was centered at the first assessment. Thus, the intercept (and its level-2 predictors) represent withdrawal symptoms at assessment 1.
Previous research has suggested that time varying predictors (i.e., state anxiety) may be decomposed into two components: the average level of the time varying predictor, and the deviation at each time point around the participant’s average score on the predictor (Hedeker & Gibbons, 2006). Failure to isolate each of these effects may produce misleading results as the MLM model will constrain the effects to be equal (Hedeker & Gibbons, 2006). Thus, in the present investigation, state anxiety was decomposed into the between-participant effect (modeled as the average level of state anxiety reported over the 14-day cessation attempt), plus the within-participant effect (modeled as the variations in state anxiety around the participant’s average level, over time).
Results
Growth curve of nicotine withdrawal symptom severity over time
Initially, the interrelations between predictor and criterion variables were examined. Please see Table 1 for descriptive statistics and zero-order correlations. Next, we examined the trajectories of acute nicotine withdrawal symptoms over time. Given that these trajectories might be curvilinear, both Time (days since quit date) and Time2 were included as predictors of nicotine withdrawal symptoms over time. In addition, to examine the effect of theoretically-relevant variables on the growth curve, we included participant sex, nicotine dependence, and AS as level-2 predictors of all of the growth curve parameters (intercept, linear slope, and quadratic slope). Finally, since initial level of nicotine withdrawal symptoms was likely to be related to the growth curve in symptoms over time, baseline nicotine withdrawal symptoms also were included as an additional predictor of the growth curve parameters. To minimize the number of the predictors in the final analysis, we conducted backward elimination analyses, dropping non-significant variables one at a time.
Table 1.
Descriptive and Zero-Order Relations among Theoretically Relevant Variables
| 1 | 2 | 3 | 4 | 5 | Mean or % (SD) | Observed Range | |
|---|---|---|---|---|---|---|---|
| 1. Sex | 1 | .02 | .04 | −.06 | .16 | 68.3% (Female) | --- |
| 2. B-FTND | 1 | .04 | .39** | .33* | 3.72 (1.19) | 1 – 5 | |
| 3. ASI | 1 | .55** | .31* | 23.16 (8.79) | 0 – 48 | ||
| 4. B-MNWS | 1 | .60** | 9.11 (6.62) | 0 – 27 | |||
| 5. B-STAI-S | 1 | 44.04 (12.45) | 20 – 80 |
Note:
p < .05,
p < .01.
FTND = Fagerström Test for Nicotine Dependence total (Fagerström, 1978) administered at baseline; Sex = Self-reported participant sex; ASI = Anxiety Sensitivity Index total (Reiss et al., 1986); B-MNWS = Minnesota Nicotine Withdrawal Scale (Hughes & Hatsukami, 1986) administered at baseline; B-STAI-S = State-Trait Anxiety Inventory State scale (STAI-S; Spielberger, Gorsuch & Lushene, 1970) administered at baseline.
Results of our first set of analyses (examining the growth curve of symptoms over time) revealed that participant sex was not a significant predictor of any of the growth curve parameters (p’s > .37). Therefore, it was dropped from further analyses. Similarly, the quadratic trend was not significant, nor was any of the theoretically relevant predictors of the quadratic trend significant (p’s > .31). Thus, it was deleted from further analyses. In addition, initial level of nicotine dependence was not related to the slope of change in symptoms over time, so it was deleted as a level-2 predictor of slope (but not as a level-2 predictor of the intercept). Thus, our final growth curve model included baseline levels of withdrawal symptoms and AS as level-2 predictors of the intercept and slope, and baseline nicotine dependence as a level-2 predictor of the intercept (see Table 2).
Table 2.
Regression coefficients for nicotine withdrawal symptom severity
| Model 1 | Model 2 | |
|---|---|---|
| B-MNWS | 0.82*** | 0.67*** |
| B-FTND | 0.82*** | 0.68*** |
| ASI | 0.02*** | 0.02*** |
| Time | −0.08 | −0.03 |
| Time x B-MNWS | −0.03*** | −0.02*** |
| Time x ASI | 0.02** | 0.02*** |
| Average Level of STAI-S | 0.16*** | |
| Average Level of STAI-S x ASI | 0.005* | |
| Daily Changes in STAI-S | 0.18*** | |
| Daily Changes in STAI-S x ASI | −0.001 |
p ≤ .05,
p ≤ .01,
p ≤ .001.
Model 1 = growth curve of withdrawal symptoms. Model 2 = growth curve of withdrawal plus the effects of state anxiety (STAI-S).
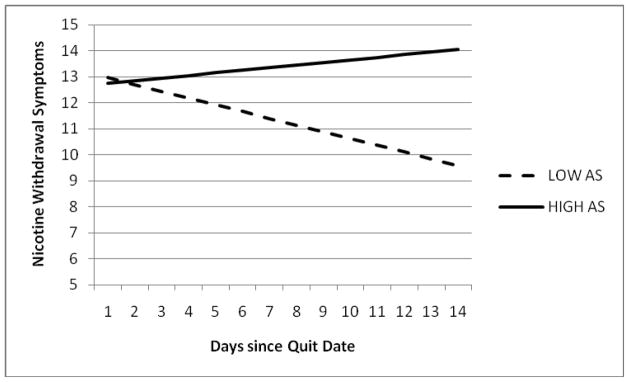
Results from this final growth curve model showed that higher levels of nicotine dependence were related to higher levels of symptoms at assessment 1, b = .82, t (93) = 3.19, p ≤ .005. Interestingly, the average linear slope of symptoms over time was not statistically significant, b = −.08, t (94) = 1.26, p = .21, indicating that those with average levels of AS and average initial withdrawal symptoms did not experience reductions in symptoms over these first 14 days after quit date. However, our results did indicate that AS was significantly related to the slope of nicotine withdrawal symptoms over time, b = .02, (94) = 3.03, p ≤ .005. The slope of decrease in withdrawal symptoms was faster (more negative) for those with lower AS. To further elucidate the effect of AS on the change in withdrawal symptoms over time, we utilized the approach developed by Aiken and West (1991), which involves creating separate regression lines for participants who are one standard deviation below the mean versus one standard deviation above the mean. We analyzed the growth curve both for participants with low baseline levels of AS (1 SD below the mean on AS) and for those with high baseline levels of AS (1 SD above the mean on AS). These growth curves are displayed in Figure 1. For participants with low baseline levels of AS, the decrease in withdrawal symptoms over time was significant, b = −.26, t (94) = 2.96, p ≤ .005, indicating that the severity of their nicotine withdrawal symptoms decreased significantly over time. For participants with high levels of baseline AS, however, the linear trend over time was not significant (actually positive), b = .10, t (94) = .99, p = .33, indicating that the severity of their nicotine withdrawal symptoms remained elevated over time.
Figure 1.
Growth curve for nicotine withdrawal symptom severity over time among participants endorsing high/low levels of anxiety sensitivity (AS).
Note: These values are estimated for those who are at the mean level of nicotine dependence and mean level of initial nicotine withdrawal symptoms
Main Effects of State Anxiety
We also hypothesized that state anxiety might exacerbate withdrawal symptoms and that the relation between state anxiety and withdrawal symptoms would be impacted by AS. To test these hypotheses, state anxiety and its interaction with AS were added as additional predictors of the growth curve of withdrawal symptoms over time. These variables were added to the growth curve (as opposed to analyzed in a separate analysis) to prevent detecting relations between anxiety and withdrawal symptoms that were simply due to both variables changing in concert over time. In addition, following the recommendations of Hedeker and Gibbons (2006), we decomposed the changes in state anxiety over time into two components: 1) the participants’ average level of anxiety over the entire 14-day study period (a between-subjects, level-2 variable) and 2) the deviation, at each assessment, from their average level of anxiety (a within-subjects, level-1, time-varying predictor of withdrawal symptoms). The interaction of AS with each component of state anxiety was also included in the analyses. Results from this analysis are presented in Table 2. Results that were already discussed for the growth curve analysis above will not be repeated below.
Our results yielded significant main effects for both indices of state anxiety (i.e., between-individual differences in average level of state anxiety and within-individual changes in state anxiety over time). Specifically, participants who reported higher average levels of state anxiety had more severe initial levels of nicotine withdrawal symptoms, b = .16, t (90) = 7.29, p ≤ .001. Similarly, increases/decreases in state anxiety over time were also associated with corresponding increases/decreases in nicotine withdrawal symptoms over time, b = .18, t (94) = 8.93, p ≤ .001.
Moderating Effects of Anxiety Sensitivity
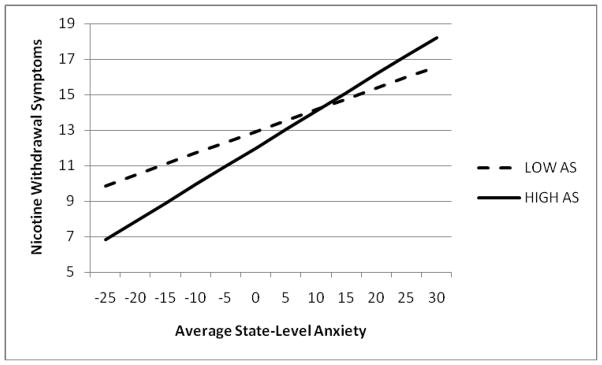
Results of our analyses also revealed a significant interaction between AS and state anxiety (average level only), b = .005, t (90) = 2.03, p ≤ .05. Specifically, greater levels of baseline AS were associated with a stronger relation between state anxiety and nicotine withdrawal symptoms experienced during the course of first two weeks of the quit attempt. Using the Aiken and West (1991) approach to interpret the interaction, we found that average level of state anxiety was more strongly related to withdrawal symptoms for those with high levels of AS, b = .21, t (90)= 6.35, p ≤ .001, than for those with low levels of AS, b = .12, t (90) = 4.24, p ≤ .001 (See Figure 2). On the other hand, AS was not a significant moderator of the effect of daily deviations in state anxiety on withdrawal symptoms (p = .83).2
Figure 2.
Anxiety sensitivity by average state anxiety predicting nicotine withdrawal symptoms.
Note: The graphed values represent initial levels of nicotine withdrawal symptoms (Day 1) for participants at the mean level of nicotine dependence and initial anxiety symptoms. The graphed relations will be identical for other times and other levels of nicotine dependence and initial anxiety symptoms. That is, only the level of nicotine withdrawal symptoms will change.
Analysis of Missing Data
To evaluate the effects of missing data within the present sample, we employed pattern mixture modeling (Hall, Delucchi, Velicer, Kahler, Ranger-Moore, Hedeker et al., 2001; Hedeker and Gibbons, 2007). Participants were coded into groups according to their missing data pattern. Consistent with the groupings established by Hall and colleagues (2001), the missing data patterns included: a) no missing data (N = 67); b) drop-out before completing the study (i.e., no data was obtained after the “drop-out date;” N = 20); and, c) sporadic missing data (N = 20). Those with some level of missing data were coded with two dummy variables (i.e., 0=drop-out; 1=sporadic missing data). Results of the pattern mixture modeling revealed that no significant differences were observed as a function of the missing data pattern. Specifically, participants with either pattern of missing data did not significantly differ from those with complete data in relation to: a) level of nicotine withdrawal symptoms; b) rate of change in nicotine withdrawal symptoms over time; and, c) the effect of state anxiety on nicotine withdrawal symptoms. Thus, overall, these analyses suggest that the missing data did not significantly impact the findings of the present study. Please see Table 3 for a summary of missing data at each assessment point.
Table 3.
Summary of missing data
| Day (Post-Quit) | N Missing Data | % Missing Data |
|---|---|---|
| Day 1 | 6 | 5.61% |
| Day 2 | 3 | 2.80% |
| Day 3 | 3 | 2.80% |
| Day 4 | 3 | 2.80% |
| Day 5 | 5 | 4.67% |
| Day 6 | 3 | 2.80% |
| Day 7 | 5 | 4.67% |
| Day 8 | 8 | 7.48% |
| Day 9 | 10 | 9.35% |
| Day 10 | 11 | 10.28% |
| Day 11 | 12 | 11.21% |
| Day 12 | 21 | 19.63% |
| Day 13 | 22 | 20.56% |
| Day 14 | 29 | 27.10% |
Discussion
The present investigation sought to address a number of key limitations in past work by investigating the main and interactive effects of AS and state anxiety in relation to acute nicotine withdrawal symptoms among daily smokers receiving a combination smoking cessation treatment. A number of theoretically and clinically important findings were observed.
In terms of main effects, contrary to hypothesis, higher initial levels of AS were not significantly associated with more severe withdrawal symptoms experienced at assessment 1 (i.e., baseline). This finding is consistent with those of Mullane et al. (2008). Yet, as predicted, our results indicated that the rate of change in withdrawal symptoms experienced during the initial 14 days of smoking cessation was significantly related to AS (see Figure 1). Specifically, withdrawal symptom severity decreased significantly over time among individuals with low levels of AS, whereas withdrawal symptom severity remained elevated over time among individuals with high levels of AS. This finding is consistent with previous empirical work demonstrating that smokers high in AS appear to be hypersensitive to interoceptive sensations, specifically, those related to nicotine withdrawal during the early phases of quitting (e.g., Marshall et al., 2009; Zvolensky et al., 2004). Moreover, our results are in accord with the theoretical prediction that smokers high in AS lapse to smoking more quickly following a quit attempt (Brown, Kahler et al., 2001; Zvolensky et al., 2009), perhaps due to their perceptions of nicotine withdrawal symptoms as being more aversive and personally harmful.
Also, consistent with prediction, both indices of state anxiety were significantly related to severity of withdrawal symptoms. That is, average levels of state anxiety were significantly associated with more severe initial levels of withdrawal symptoms. Similarly, daily deviations (increases/decreases) in state anxiety were significantly associated with simultaneous changes (increases/decreases) in severity of withdrawal symptoms experienced during the initial 14 days of smoking cessation. These findings are consistent with past work suggesting that negative mood states may influence the onset and course of nicotine withdrawal symptoms (Piasecki et al., 1997; Piasecki et al., 1998). Here, it may be that experiencing heightened levels of state anxiety while quitting smoking render one more reactive to nicotine withdrawal symptoms, thereby further exacerbating symptom severity (see below for further discussion).
Partially consistent with prediction, the interactive effect of AS by average state anxiety (but not daily deviations in state anxiety) was significantly associated with levels of nicotine withdrawal symptoms experienced during the initial 14-days of the cessation attempt. Such effects were evident above and beyond the variance accounted for by participant sex and nicotine dependence. Inspection of the form of the interaction indicated that it was in accord with the a priori theoretical formulation (see Figure 2). That is, AS significantly moderated the observed relation between average state anxiety and nicotine withdrawal symptom severity such that state anxiety was more strongly related to withdrawal symptoms for those high compared to low in AS. These findings, which are consistent with integrated theoretical smoking-AS models (Zvolensky & Bernstein, 2005; Zvolensky et al., 2003), uniquely extend past work on the AS nicotine withdrawal relation (Marshall et al., 2009; Mullane et al., 2008). Indeed, this novel pattern of findings highlights the possible clinically-relevant interplay between AS and average levels of state anxiety in regard to the experience of acute nicotine withdrawal symptoms among daily adult cigarette smokers attempting to quit. Namely, among high AS persons, state anxiety may be more relevant, compared to those low in AS, in regard to experiencing withdrawal symptoms as more intense during the early phases of quitting.
The current investigation provides a novel empirical perspective on the role of AS and state anxiety in terms of acute nicotine withdrawal among daily smokers undergoing smoking cessation treatment. Results from this study help elucidate the role of anxiety vulnerability in terms of nicotine withdrawal symptom severity experienced during the early phases of smoking cessation. This work helps to clarify putative mechanisms underlying the experience of more intense or personally problematic nicotine withdrawal symptoms among smokers characterized by elevated levels of AS and/or state anxiety. The present data add to the growing literature suggesting that smokers with emotional risk factors such as AS and state anxiety may profit from specialized treatment approaches for the purpose of attenuating problematic withdrawal symptoms in an effort to prevent early lapse and relapse (Zvolensky, Bernstein, Yartz, McLeish, & Feldner, 2008).
A number of limitations of the present investigation and points for future direction should be considered. First, the present sample is limited in that it is comprised of a relatively homogenous (e.g., primarily Caucasian; 68% female) group of adult smokers who volunteered to participate in smoking cessation treatment. Given that AS tends to be elevated among women compared to men (Peterson & Plehn, 1999; Stewart, Taylor, & Baker, 1997; Van Dam, Earleywine, & Forsyth, 2009) and that the vast majority of cigarette smokers attempt to quit on their own (70% of smokers; Levy & Friend, 2002), it will be important for researchers to draw from populations other than those included in the present study to rule out potential self-selection bias among persons with these characteristics and increase the generalizability of these findings. Second, the study focused primarily on AS and state anxiety. These emotional factors are naturally only some of many possible emotional risk candidates that may contribute to the development of more severe withdrawal symptoms. Future work could usefully continue to build multi-risk factor models of nicotine withdrawal by incorporating other promising affective-and/or cognitive-relevant variables, such as distress tolerance (e.g., ability to tolerate negative affect or related aversive psychological and physical states; Brown, Lejuez, Kahler, Strong, & Zvolensky, 2005) or specific smoking expectancies (i.e., beliefs about the effects of smoking; Brandon, Juliano, & Copeland, 1999).
Third, the present study examined whether state anxiety exacerbates the severity of nicotine withdrawal symptoms experienced during cessation. However, an alternative hypothesis may be that more severe nicotine withdrawal symptoms produce heightened levels of state anxiety. Thus, future work may benefit from testing the possible bi-directional relation between state anxiety and nicotine withdrawal symptoms. Fourth, the current findings were based upon self-reported acute nicotine withdrawal symptoms assessed once daily during the initial 14 days of the cessation attempt. An important next step in this line of inquiry would be to obtain nicotine withdrawal symptom reports at multiple time points to evaluate the consistency of the present findings throughout the course of individuals’ quit attempts. For example, future research would benefit from utilizing an ecological momentary assessment approach (EMA) to assess nicotine withdrawal symptom severity as it occurs in ‘real time.’ Finally, the current study did not include diagnostic assessments of past or present psychopathology; nor did it include an assessment of other substance use (e.g., alcohol use). Such information would be helpful in order to provide a more fine-grained analysis of the psychopathological characteristics of the sample by allowing for the comparison of diagnostic status to AS and/or state anxiety in relation to the severity of nicotine withdrawal symptom severity.
Together, the present findings uniquely extend and help clarify past discrepant work documenting a possible association between AS, state anxiety, and nicotine withdrawal symptoms among adult treatment-seeking smokers. Results suggest that among high AS persons, state anxiety may be more relevant, compared to those low in AS, in regard to experiencing withdrawal symptoms as more intense during the early phases of quitting. These findings provide novel evidence that AS and state anxiety are important factors to consider in terms of the acute experience of nicotine withdrawal symptoms during smoking cessation treatment.
Footnotes
It should be noted that although anxiety and anxiety-related symptoms overlap with symptoms of acute nicotine withdrawal, empirical research suggests that they are two distinct constructs (Myrsten, Elgerot, & Edgren, 1977; Shiffman, West, & Gilbert, 2004; West & Hajek, 1997). Moreover, within the present investigation, a significant amount of variability was observed between individuals with regard to daily deviations in state anxiety and severity of nicotine withdrawal symptoms. These results further suggest that the pattern of change in terms of state anxiety and nicotine withdrawal symptoms differs across our sample. Please contact Dr. Zvolensky for the full results of this analysis.
The final analyses (the growth curve analysis and the anxiety analysis) were rerun including anxious arousal symptoms (Mood and Anxiety Symptom Questionnaire [MASQ]: Watson et al., 1995) as an additional predictor, to verify that the obtained relations between AS and withdrawal symptoms were not merely due to AS’s relation with anxious arousal symptoms. The results from the analyses including anxious arousal symptoms were virtually identical to those reported without including anxious arousal symptoms, indicating that the obtained effects were not due to AS’s relation with anxious arousal symptoms. Please contact Dr. Zvolensky for the full results of this additional analysis.
Contributor Information
Kirsten A. Johnson, University of Vermont
Sherry Stewart, Dalhousie University
David Rosenfield, Southern Methodist University
Dan Steeves, Nova Scotia Department of Health Promotion and Protection
Michael J. Zvolensky, University of Vermont
References
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Thousand Oaks, CA, US: Sage Publications, Inc; 1991. [Google Scholar]
- Battista SR, Stewart SH, Fulton HG, Steeves D, Darredeau C, Gavric D. A further investigation of the relations of anxiety sensitivity to smoking motives. Addictive Behaviors. 2008;33(11):1402–1408. doi: 10.1016/j.addbeh.2008.06.016. [DOI] [PubMed] [Google Scholar]
- Brown RA, Kahler CW, Zvolensky MJ, Lejuez CW, Ramsey SE. Anxiety sensitivity: Relationship to negative affect smoking and smoking cessation in smokers with past major depressive disorder. Addictive Behaviors. 2001;26:887–899. doi: 10.1016/s0306-4603(01)00241-6. [DOI] [PubMed] [Google Scholar]
- Brown RA, Lejuez CW, Kahler CW, Strong DR. Distress tolerance and duration of past smoking cessation attempts. Journal of Abnormal Psychology. 2002;111:180–185. [PubMed] [Google Scholar]
- Brown RA, Lejuez CW, Kahler CW, Strong DR, Zvolensky MJ. Distress tolerance and early smoking lapse. Clinical Psychology Review. 2005;25:713–733. doi: 10.1016/j.cpr.2005.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comeau N, Stewart SH, Loba P. The relations of trait anxiety, anxiety sensitivity, and sensation seeking to adolescents’ motivations for alcohol, cigarette, and marijuana use. Addictive Behaviors. 2001;26:803–825. doi: 10.1016/s0306-4603(01)00238-6. [DOI] [PubMed] [Google Scholar]
- Fagerstrom K. Measuring degree of physical dependence to tobacco smoking with reference to individualization of treatment. Addictive Behaviors. 1978;3:235–241. doi: 10.1016/0306-4603(78)90024-2. [DOI] [PubMed] [Google Scholar]
- Gregor K, Zvolensky MJ, McLeish AC, Bernstein A, Morissette S. Anxiety sensitivity and perceived control over anxiety-related events: Associations with smoking outcome expectancies and perceived cessation barriers among daily smokers. Nicotine and Tobacco Research. 2008;10(4):627–635. doi: 10.1080/14622200801978706. [DOI] [PubMed] [Google Scholar]
- Hall SM, Delucchi KL, Velicer WF, Kahler CW, Ranger-Moore J, Hedeker D, Tsoh JY, Niaura R. Statistical analysis of randomized trials in tobacco treatment: Longitudinal designs with dichotomous outcome. Nicotine & Tobacco Research. 2001;3:193–202. doi: 10.1080/14622200110050411. [DOI] [PubMed] [Google Scholar]
- Hamer RM, Simpson PM. Last observation carried forward versus mixed models in the analysis of psychiatric clinical trials. The American Journal of Psychiatry. 2009;166(6):639–641. doi: 10.1176/appi.ajp.2009.09040458. [DOI] [PubMed] [Google Scholar]
- Hayward C, Killen JD, Kraemer HC, Taylor CB. Predictors of panic attacks in adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:207–214. doi: 10.1097/00004583-200002000-00021. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO. The Fagerstrom test for nicotine dependence: A revision of the Fagerstrom Tolerance Questionnaire. British Journal of Addiction. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Hedeker D, Gibbons RD. Wiley Series in Probability and Statistics. Hoboken, NJ, US: Wiley-Interscience; 2006. Longitudinal data analysis. [Google Scholar]
- Hughes JR. Tobacco withdrawal in self-quitters. Journal of Consulting and Clinical Psychology. 1992;60(5):689–697. doi: 10.1037//0022-006x.60.5.689. [DOI] [PubMed] [Google Scholar]
- Hughes JR, Higgins ST, Hatsukami D. Effects of abstinence from tobacco: A critical review. Research Advances in Alcohol and Drug Problems. 1990;10:317–398. [Google Scholar]
- Hughes JR, Hatsukami D. Signs and symptoms of tobacco withdrawal. Archives of General Psychiatry. 1986;43:289–294. doi: 10.1001/archpsyc.1986.01800030107013. [DOI] [PubMed] [Google Scholar]
- Lejuez CW, Paulson A, Daughters SB, Bornovalova MA, Zvolensky MJ. The association between heroin use and anxiety sensitivity among inner-city individuals in residential drug use treatment. Behavior Research and Therapy. 2006;44:667–677. doi: 10.1016/j.brat.2005.04.006. [DOI] [PubMed] [Google Scholar]
- Levy DT, Friend K. A simulation model of policies directed at treating tobacco use and dependence. Medical Decision Making. 2002;22:6–17. doi: 10.1177/0272989X0202200101. [DOI] [PubMed] [Google Scholar]
- Leyro TM, Zvolensky MJ, Vujanovic A, Bernstein A. Anxiety sensitivity and smoking motives and outcome expectancies among adult daily smokers: Replication and extension. Nicotine and Tobacco Research. 2008;10(6):985–994. doi: 10.1080/14622200802097555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li W, Zinbarg RE. Anxiety sensitivity and panic attacks: A one-year longitudinal study. Behavior Modification. 2007;31:145–161. doi: 10.1177/0145445506296969. [DOI] [PubMed] [Google Scholar]
- Maller RG, Reiss S. Anxiety sensitivity in 1984 and panic attacks in 1987. Journal of Anxiety Disorders. 1992;6:241–247. [Google Scholar]
- Marshall EC, Johnson K, Bergman J, Gibson LE, Zvolensky MJ. Anxiety sensitivity and panic reactivity to bodily sensations: Relation to quit-day (acute) nicotine withdrawal symptom severity among daily smokers making a self-guided quit attempt. Experimental and Clinical Psychopharmacology. 2009;17(5):356–364. doi: 10.1037/a0016883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall GN, Miles JNV, Stewart SH. Anxiety sensitivity and PTSD symptom severity are reciprocally related: Evidence from a longitudinal study of physical trauma survivors. Journal of Abnormal Psychology. 2010;119(1):143–150. doi: 10.1037/a0018009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNally RJ. Anxiety sensitivity and panic disorder. Biological Psychiatry. 2002;52:938–946. doi: 10.1016/s0006-3223(02)01475-0. [DOI] [PubMed] [Google Scholar]
- McNally RJ. Cognitive bias in the anxiety disorders. In: Hope DA, editor. Perspectives on anxiety, panic, and fear: current theory and research in motivation. Lincoln, NE: University of Nebraska Press; 1996. pp. 211–250. [PubMed] [Google Scholar]
- Mullane JC, Stewart SH, Rhyno E, Steeves D, Watt M, Eisner A. Anxiety sensitivity and difficulties with smoking cessation. In: Columbus AM, editor. Advances in Psychology Research. 54 A. Hauppauge, NY: Nova Science Publishers; 2008. pp. 141–155. [Google Scholar]
- Myrsten AL, Elgerot A, Edgren B. Effects of abstinence from tobacco smoking on physiological and psychological arousal levels in habitual smokers. Psychosomatic Medicine. 1977;39(1):25–38. doi: 10.1097/00006842-197701000-00004. [DOI] [PubMed] [Google Scholar]
- Norton GR, Rockman GE, Luy B, Marion T. Suicide, chemical abuse, and panic attacks: A preliminary report. Behaviour Research and Therapy. 1993;31:37–40. doi: 10.1016/0005-7967(93)90040-2. [DOI] [PubMed] [Google Scholar]
- Novak A, Burgess ES, Clark M, Zvolensky MJ, Brown RA. Anxiety sensitivity, self-reported motives for alcohol and nicotine use and level of consumption. Journal of Anxiety Disorders. 2003;17(2):165–180. doi: 10.1016/s0887-6185(02)00175-5. [DOI] [PubMed] [Google Scholar]
- Peterson RA, Plehn K. Measuring Anxiety Sensitivity. In: Taylor S, editor. Anxiety sensitivity: Theory, research, and treatment in the fear of anxiety. Mahwah, NJ: Lawrence Erlbaum Associates; 1999. pp. 61–81. [Google Scholar]
- Piasecki TM, Kenford SL, Smith SS, Fiore MC, Baker TB. Listening to nicotine: Negative affect and the smoking withdrawal conundrum. Psychological Science. 1997;8:184–189. [Google Scholar]
- Piasecki TM, Niaura R, Shadel WG, Abrams DB, Goldstein MG, Fiore MC, Baker TB. Smoking withdrawal dynamics in unaided quitters. Journal of Abnormal Psychology. 2000;109:74–86. doi: 10.1037//0021-843x.109.1.74. [DOI] [PubMed] [Google Scholar]
- Piasecki TM, Fiore MC, Baker TB. Profiles in discouragement: Two studies of variability in the time course of smoking withdrawal symptoms. Journal of Abnormal Psychology. 1998;107:238–251. doi: 10.1037//0021-843x.107.2.238. [DOI] [PubMed] [Google Scholar]
- Pomerleau CS, Carton SM, Lutzke ML, Flessland KA, Pomerleau OF. Reliability of the Fagerstrom Tolerance Questionnaire and the Fagerstrom Test for Nicotine Dependence. Addictive Behaviors. 1994;19(1):33–39. doi: 10.1016/0306-4603(94)90049-3. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical Linear Models: Applications and Data Analysis Methods. Sage Publications; 2002. [Google Scholar]
- Reiss S, Havercamp S. The sensitivity theory of motivation: Implications for psychopathology. Behavior Research and Therapy. 1996;34:621–632. doi: 10.1016/0005-7967(96)00041-1. [DOI] [PubMed] [Google Scholar]
- Reiss S, McNally RJ. Expectancy model of fear. In: Reiss S, Bootzin RR, editors. Theoretical issues in behavior therapy. Orlando, FL, US: Academic Press, Inc; 1985. pp. 107–121. [Google Scholar]
- Schmidt NB, Keough ME, Mitchell MA, Reynolds EK, MacPherson L, Zvolensky MJ, Lejuez CW. Anxiety sensitivity: Prospective prediction of anxiety among early adolescents. Journal of Anxiety Disorders. 2010;24(5):503–508. doi: 10.1016/j.janxdis.2010.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt NB, Lerew DR, Jackson RJ. The role of anxiety sensitivity in the pathogenesis of panic: Prospective evaluation of spontaneous panic attacks during acute stress. Journal of Abnormal Psychology. 1997;106:355–364. doi: 10.1037//0021-843x.106.3.355. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Lerew DR, Jackson RJ. Prospective evaluation of anxiety sensitivity in the pathogenesis of panic: Replication and extension. Journal of Abnormal Psychology. 1999;108:532–537. doi: 10.1037//0021-843x.108.3.532. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Zvolensky MJ, Maner JK. Anxiety sensitivity: Prospective prediction of panic attacks and Axis I pathology. Journal of Psychiatric Research. 2006;40:691–699. doi: 10.1016/j.jpsychires.2006.07.009. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Zvolensky MJ. Anxiety sensitivity and CO challenge reactivity as unique and interactive prospective predictors of anxiety pathology. Depression and Anxiety. 2007;24(8):527–536. doi: 10.1002/da.20267. [DOI] [PubMed] [Google Scholar]
- Shiffman S, West RJ, Gilbert DG. Recommendation for the assessment of tobacco craving and withdrawal in smoking cessation trials. Nicotine & Tobacco Research. 2004;6(4):599–614. doi: 10.1080/14622200410001734067. [DOI] [PubMed] [Google Scholar]
- Spielberger CD, Gorsuch RL, Lushene RE. Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press; 1970. [Google Scholar]
- Stewart SH, Karp J, Pihl RO, Peterson RA. Anxiety sensitivity and self-reported reasons for drug use. Journal of Substance Abuse. 1997;9:223–240. doi: 10.1016/s0899-3289(97)90018-3. [DOI] [PubMed] [Google Scholar]
- Stewart SH, Taylor S, Baker JM. Gender differences in dimensions of anxiety sensitivity. Journal of Anxiety Disorders. 1997;11(2):179–200. doi: 10.1016/s0887-6185(97)00005-4. [DOI] [PubMed] [Google Scholar]
- Stewart SH, Kushner MG, editors. Introduction to the special issue on ‘Anxiety Sensitivity and Addictive Behaviors. Addictive Behaviors. 2001;26:775–785. doi: 10.1016/s0306-4603(01)00236-2. [DOI] [PubMed] [Google Scholar]
- Van Dam NT, Earleywine M, Forsyth JP. Gender bias in the sixteen-item Anxiety Sensitivity Index: An application of polytomous differential item functioning. Journal of Anxiety Disorders. 2009;23(2):256–259. doi: 10.1016/j.janxdis.2008.07.008. [DOI] [PubMed] [Google Scholar]
- Vujanovic AA, Zvolensky MJ. Anxiety sensitivity, acute nicotine withdrawal symptoms, and anxious and fearful responding to bodily sensations: A laboratory test. Experimental and Clinical Psychopharmacology. 2009;17(3):181–190. doi: 10.1037/a0016266. [DOI] [PubMed] [Google Scholar]
- West R, Hajek P. What happens to anxiety levels on giving up smoking? The American Journal of Psychiatry. 1997;154(11):1589–1592. doi: 10.1176/ajp.154.11.1589. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Baker KM, Leen-Feldner EW, Bonn-Miller MO, Feldner MT, Brown RA. Anxiety sensitivity: Association with intensity of retrospectively-rated smoking-related withdrawal symptoms and motivation to quit. Cognitive Behaviour Therapy. 2004;33:114–125. doi: 10.1080/16506070310016969. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Bernstein A. Cigarette smoking and panic psychopathology. Current Directions in Psychological Science. 2005;14:301–305. doi: 10.1177/0963721410388642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zvolensky MJ, Bernstein A, Cardenas SJ, Colotla VA, Marshall EC, Feldner MT. Anxiety sensitivity and early relapse to smoking: A test among Mexican daily, low-level smokers. Nicotine & Tobacco Research. 2007;9:483–491. doi: 10.1080/14622200701239621. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Bernstein A, Yartz AR, McLeish A, Feldner MT. Cognitive-behavioral treatment of comorbid panic psychopathology and tobacco use and dependence. In: Stewart SH, Conrad P, editors. Comorbidity of anxiety and substance use disorders. New York: Springer; 2008. pp. 177–200. [Google Scholar]
- Zvolensky MJ, Bonn-Miller MO, Bernstein A, Marshall EC. Anxiety sensitivity and abstinence duration to smoking. Journal of Mental Health. 2006;15:659–670. [Google Scholar]
- Zvolensky MJ, Kotov R, Antipova AV, Schmidt NB. Diathesis-stress model for panic-related distress: A test in a Russian epidemiological sample. Behaviour Research and Therapy. 2005;43:521–532. doi: 10.1016/j.brat.2004.09.001. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Lejuez CW, Kahler CW, Brown RA. Nonclinical panic attack history and smoking cessation: An initial examination. Addictive Behaviors. 2004;29:825–830. doi: 10.1016/j.addbeh.2004.02.017. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Strong D, Bernstein A, Vujanovic AA, Marshall EC. Evaluation of anxiety sensitivity among daily adult smokers using item response theory analysis. Journal of Anxiety Disorders. 2009;23(2):230–239. doi: 10.1016/j.janxdis.2008.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zvolensky MJ, Stewart SH, Vujanovic A, Gavric D, Steeves D. Anxiety sensitivity and anxiety and depressive symptoms in the prediction of early smoking lapse and relapse during smoking cessation treatment. Nicotine and Tobacco Research. 2009;11:323–331. doi: 10.1093/ntr/ntn037. [DOI] [PMC free article] [PubMed] [Google Scholar]