Abstract
Objective
This trial of a randomized indicated anxiety prevention and early intervention explored initial program effects as well as the role of ethnicity and language on measured outcomes
Method
A total of 88 youth (M = 10.36 years; 45 girls, 52 Latino) received one of two protocols with varying degrees of parent involvement, and response was measured at posttest and six month follow-up.
Results
Findings showed that child anxiety symptoms improved significantly across protocols, although additional gains were found for children in the child plus parent condition. Program effects did not vary by Latino ethnicity or Spanish language use in the intervention.
Conclusions
The cognitive and behavioral strategies established for Caucasian children may be promising for Hispanic/Latino children when applied in a culturally responsive manner.
Keywords: Anxiety, prevention, therapy, child, Hispanic/Latinos
Anxiety disorders are not only among the most prevalent psychiatric disorders in children and adolescents, they are typically chronic and lead to significant impairment, including poor academic performance, depression, and the early initiation of the use of alcohol, tobacco, and other illicit drugs (Costello, Egger, & Angold, 2005, Kessler, Ruscio, Shear, & Wittchen, 2009). This constellation of negative outcomes has led to the development of evidence-based interventions aimed at preempting anxiety disorders (Fisak, Richard, & Mann, 2011) as well as treatments for clinically anxious children (Silverman, Pina, & Viswesvaran, 2008). The Arizona Anxiety Resilience Building Project builds on this past literature and aims at developing and evaluating theory-driven, culturally robust, interventions to reduce anxiety and prevent the onset and exacerbation of anxiety disorders in children. In this study, a main objective was to conduct an initial evaluation of an indicated prevention and early intervention protocol for anxiety with Hispanic/Latino and Caucasian children. Focusing on Hispanic/Latino children is important because census data show that Hispanic/Latinos comprise the largest ethnic minority group in the U.S. (Humes, Jones, & Ramirez, 2011) and also because this segment of the U.S. population appears to suffer from anxiety significantly more than Caucasians (Pina & Silverman, 2004; Roberts, Roberts, & Xing, 2006). Regrettably, there is no randomized trial evaluating anxiety program effects among Hispanic/Latino children, although evidence from secondary data analyses corresponding to highly acculturated English-speaking Cuban-American children shows that cognitive-behavior treatment is promising (Pina, Silverman, Fuentes, Kurtines, & Weems, 2003).
Building on this work, the focus of the present study was on degree of caregiver involvement and the role of ethnicity/language. In terms of caregiver involvement, evidence supporting the role of parents in child anxiety treatment appears equivocal (Barmish & Kendall, 2005), and when it comes to anxiety prevention, every program to date has included some degree of caregiver training making it unclear whether parent training enhances program effects on anxiety (Fisak et al., 2011). Why involve caregivers in child anxiety interventions? Typically, anxious children are found to have anxious parents and parents of anxious children often model and reinforce anxious behaviors (Ginsburg, Silverman, & Kurtines, 1995; Hudson & Rapee, 2005). As such, including parents in child anxiety interventions appears indispensable, at least conceptually. Moreover, when it comes to Hispanic/Latinos, qualitative data from parent focus groups and in-depth interviews (in English and Spanish) show a preference for parental involvement in child-focused interventions (Dumka, Gonzales, Wood, & Formoso, 1998; Pina, Villalta, & Zerr, 2009), perhaps because Hispanic/Latinos place great emphasis on caregiving and family (c.f. Familismo). Continuing with ethnicity (Caucasian/Latino) and language (Spanish/English), in Griner and Smith’s (2006) meta-analyses of adult psychotherapy studies, Latinos treated in Spanish appeared to benefit greatly from adapted interventions but no study has examined this issue in children. Also, some Hispanic/Latino parents involved in interventions prefer/require delivery in Spanish rendering it important for program effects to remain robust in translation. Thus, this study examined program effects for Hispanic/Latino and Caucasian children with anxiety, across two conditions with varying degrees of parent involvement, and via clinician, child, and parent measures. The role of ethnicity and language on program effects also was explored.
Method
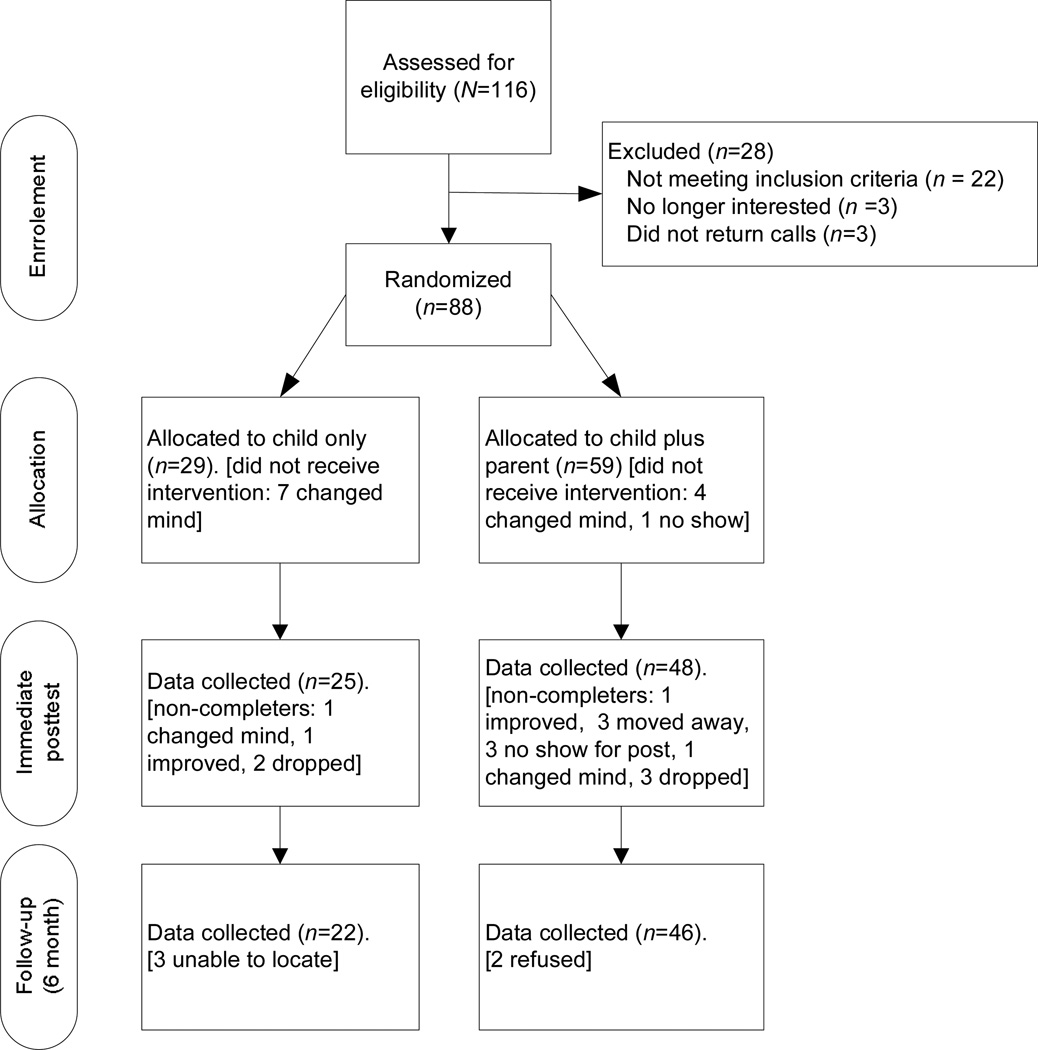
Participants were referred to the study by school staff (teachers, school counselors, nurses, school psychologist, or social workers) due to excessive anxiety. Inclusion and exclusion criteria were ascertained via the Anxiety Disorders Interview Schedule for DSM-IV: Child and Parent Versions (ADIS-C/P; Silverman & Albano, 1996). Exclusion criteria were developmental delays, psychosis, schizophrenia, suicidal ideation, or current involvement in another intervention. Inclusion criteria were anxiety symptoms or diagnoses as the primary problem. Based on the ADIS-C/P, 16 youth exhibited anxiety disorder symptoms as the principal problem but did not meet criteria for an anxiety disorder diagnosis. More specifically, 5 children showed social anxiety symptoms, 4 separation anxiety symptoms, 3 generalized anxiety symptoms, and 3 specific phobia symptoms. Turning to those who met diagnostic criteria, 32 showed separation anxiety disorder (SAD), 14 generalized anxiety disorder (GAD), 11 social anxiety disorder (SoP), and 10 specific phobia (SP). In terms of ADIS-C/P clinical severity ratings (CSR), 16 children had CSRs < 4 and 72 had CSR ≥ 4. As shown in Figure 1, 88 youth (M = 10.36 years, SD = 2.73; 45 girls) were randomized to one of two conditions. In this sample, 36 youth (40.9%) were Caucasian and 52 (59.1%) were Hispanic/Latino (mostly Mexican-origin; 48% or 25 chose/participated in Spanish; 52% or 27 in English). Median annual incomes ranged from $21K to $41K.
Figure 1.
CONSORT Flowchart: Recruitment, Randomization, and Assessments of the Prevention and Early Intervention Child Anxiety Pilot Trial
Measures included the Anxiety Disorders Interview Schedule for DSM-IV: Child and Parent Versions (ADIS-IV: C/P; Silverman & Albano, 1996), administered to children and parents as described in its manual (Albano & Silverman, 1996). The ADIS-IV: C/P yields reliable anxiety symptom counts (ICCs .78 to .95 for ADSI-C; .81 to .96 for ADIS-P), diagnoses (κ = .80 to .92), and CSR (r’s .80 to .84) (Silverman, Saavedra, & Pina, 2001). Similar to past research, the ADIS-IV: C/P was the primary anxiety measure (Kendall, Hudson, Gosch, Flannery-Schroeder, & Suveg, 2008). In addition, children completed the Revised Children's Manifest Anxiety Scale (RCMAS; Reynolds & Richmond, 1978) and the Children’s Depression Inventory (CDI; Kovacs, 1981). The RCMAS contains 28 items rated Yes or No and items are summed to yield a Total Anxiety score. Pela and Reynolds (1982) reported a retest reliability of .98 and the alpha. The CDI contains 27 items and children respond by choosing one of three options per item assessing depression. Retest reliabilities for the CDI ranged from 0.74 to 0.77 in Smucker, Craighead, Craighead, and Green (1986). In the present study, the alpha for the RCMAS was .89 and for the CDI it was .87. Both the RCMAS and CDI showed cross-ethnic/gender measurement equivalence in Pina, Little, Knight, and Silverman (2009). Parents completed the Child Behavior Checklist (CBCL; Achenbach, 1991) and the internalizing scale was used in this study. Alpha coefficients for internalizing scale scores range from .89 to .92.
Procedures were approved by the university’s Institutional Review Board. In this study, school staff corresponding to 79 public schools participated in a 2-hour student anxiety workshop. The objective of the workshop was to provide information about: (1) the various types of anxiety problems in children (SAD, GAD, SoP, SP), (2) the clinical phenomenology of anxiety in Hispanic/Latino children, and (3) referring anxious children to this study from the schools’ regular classes. A handout summarizing information from the workshop was provided to help school staff identify and refer students for this study. The handout included paraphrased stem questions from the ADIS-IV: C/P but no cut-off criterion was used. Referrals to the study were made at the discretion of the school. After parents provided consent (children assent), the ADIS-IV: C/P was administered along with the questionnaires. Children meeting the study’s criteria were invited to participate and were randomized using a 1:2 ratio (child only:child plus parent) to facilitate exploration of the role of ethnicity/language within the child plus parent condition as necessary. Assessment and intervention procedures were implemented at a university clinic with measures re-administered at posttest and 6-month follow-up (FU) by blinded research assistants.
Conditions were manualized for standardization and replication. Strategies for reducing child anxiety consisted of systematic and gradual exposures to anxiety provoking situations and cognitive-behavioral strategies to facilitate the exposures (Silverman & Kurtines, 1996). In the child only condition, the mother was involved at the end of each session to review progress (~10 minutes). In the child plus parent condition, the child and mother met together with the interventionist for the entire session (60 minutes) in the same room, with each child and mother actively engaged by the interventionist. In the plus parent condition, the focus was on reducing parental reinforcement of the child’s anxious behavior and guiding the parent to help the child practice the skills learned in session. Each condition lasted 12 weeks and was implemented based on our conceptual approach to cultural sensitivity. This cultural sensitivity approach emphasizes core therapeutic components (e.g., systematic and gradual exposures) and the use of culturally responsive implementation strategies (Pina et al., 2009). In this study, a focus was on manual development (Pina, 2006). Interventionists were seven doctoral students (two bilingual) trained by the first author, who held weekly on-site supervision meetings (licensed psychologists provided oversight). Sessions were recorded and independent evaluators rated 20% of randomly selected tapes to yield an overall rating of protocol adherence. Ratings for parent involvement yielded 100% for child plus parent and 5% for child only. Inter-rater reliability was acceptable (90%).
Results
Program Effects were evaluated using SAS 9.2 with PROC MIXED. Pre to post and pre to FU changes were estimated via RM-ANOVA on the ADIS-CSR, ADIS-C, ADIS-P, RCMAS, CDI, and CBCL-I. Decomposition of program effects were pursued using single degree of freedom contrasts (Jaccard, 1998) and clinically significant change was evaluated as suggested by Kendall and Grove (1988). Preliminary analyses showed no outliers, no attrition biases, and no significant pretest differences between conditions. Correlations among the outcomes showed no evidence of potential redundancy (no rs > .85; Kazdin, 1995). Table 1 shows least squares means and standard errors whereas Table 2 shows results from analyses of program effects. As detailed in Table 2, significant improvements across all measures for the child plus parent condition as well as significant improvements on the ADIS-C/P-CSR, ADIS-C, and CBCL-I for the child only condition were found. There was some deterioration on the CDI for some children in the child only condition, but scores remained below the clinical range. Program effects also were evidenced in terms of clinically significant change based on the CBCL-I. In the child plus parent condition, 17 children moved from the clinical to the normal range, 3 from clinical to borderline, and 2 from borderline to normal. In the child only condition, 3 moved from clinical to normal and 1 from clinical to borderline. Turning to posttest diagnoses based on the ADIS-C/P, 1 child met criteria for SAD and 5 for GAD in the plus parent condition (6/48 or 13%). One child met criteria for SAD in the child only condition (1/25 or 4%). At FU, 3 children met criteria for SAD and 2 for GAD in the plus parent condition (5/46 or 10%) whereas 1 met criteria for SAD in the child only condition (1/22 or 5%). None of the 16 children with symptoms and no diagnoses at pretest met criteria for an anxiety disorder diagnosis at posttest or FU.
Table 1.
Means and Standard Errors for the Total Sample and for Each Condition
| Measures | Total Sample | Child Only | Child plus Parent | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | FU | Pre | Post | FU | Pre | Post | FU | ||
| ADIS-CSR | M | 5.20 | 1.42 | 1.26 | 5.10 | 0.93 | 0.85 | 5.31 | 1.90 | 1.66 |
| SE | 0.25 | 0.30 | 0.37 | 0.42 | 0.53 | 0.66 | 0.26 | 0.28 | 0.34 | |
| ADIS-C | M | 4.31 | 1.29 | 0.97 | 4.35 | 0.99 | 0.52 | 4.26 | 1.58 | 1.43 |
| SE | 0.56 | 0.35 | 0.43 | 0.96 | 0.63 | 0.79 | 0.56 | 0.32 | 0.36 | |
| ADIS-P | M | 5.00 | 2.05 | 1.91 | 4.06 | 1.42 | 1.30 | 5.95 | 2.67 | 2.53 |
| SE | 0.57 | 0.61 | 0.69 | 0.98 | 1.09 | 1.22 | 0.59 | 0.56 | 0.63 | |
| RCMAS | M | 12.75 | 7.82 | 9.48 | 13.56 | 10.18 | 13.33 | 11.93 | 5.46 | 5.64 |
| SE | 1.14 | 1.32 | 1.58 | 1.99 | 2.42 | 2.95 | 1.10 | 1.04 | 1.13 | |
| CDI | M | 25.19 | 18.81 | 18.38 | 24.86 | 28.63 | 26.91 | 25.53 | 8.99 | 9.85 |
| SE | 0.45 | 1.91 | 2.06 | 0.78 | 3.49 | 3.79 | 0.45 | 1.57 | 1.63 | |
| CBCL-I | M | 21.70 | 7.53 | 12.19 | 22.70 | 7.10 | 14.53 | 20.70 | 7.95 | 9.85 |
| SE | 1.99 | 1.13 | 1.66 | 3.43 | 2.02 | 3.04 | 2.02 | 1.03 | 1.34 | |
Note. Least Squares Means are reported. Pre = pretest, Post = immediate posttest (3-month), FU = follow-up (6 months). ADIS-CSR = Anxiety Disorders Interview Schedule- Clinician’s Severity Rating, ADIS-C = Anxiety Disorders Interview Schedule Child Symptom Count, ADIS-P = Anxiety Disorders Interview Schedule Parent Symptom Count about the child, RCMAS = Revised Children’s Manifest Anxiety Scale (Total Anxiety), CDI = Children’s Depression Inventory, CBCL-I = Child Behavior Checklist – Internalizing.
Table 2.
Program Effects for the Total Sample and for Each Condition
| Measures | Total Sample | Child Only | Child plus Parent | ||||
|---|---|---|---|---|---|---|---|
| Pre to Post | Pre to FU | Pre to Post | Pre to FU | Pre to Post | Pre to FU | ||
| ADIS-CSR | PE | 3.59 | 3.79 | 4.17 | 4.25 | 3.41 | 3.65 |
| SE | 0.30 | 0.35 | 0.62 | 0.74 | 0.34 | 0.40 | |
| t-value | 12.05*** | 10.95*** | 6.77*** | 5.74*** | 9.98*** | 9.18*** | |
| Lower CI | 2.99 | 3.10 | 2.94 | 2.77 | 2.73 | 2.85 | |
| Upper CI | 4.18 | 4.48 | 5.40 | 5.73 | 4.09 | 4.44 | |
| ADIS-C | PE | 2.85 | 3.05 | 3.36 | 3.83 | 2.69 | 2.84 |
| SE | 0.57 | 0.53 | 1.16 | 1.14 | 0.65 | 0.60 | |
| t-value | 5.04*** | 5.8*** | 2.91** | 3.38** | 4.11*** | 4.73*** | |
| Lower CI | 1.72 | 2.00 | 1.05 | 1.57 | 1.38 | 1.64 | |
| Upper CI | 3.98 | 4.10 | 5.67 | 6.10 | 3.99 | 4.03 | |
| ADIS-P | PE | 3.13 | 3.26 | 2.63 | 2.76 | 3.28 | 3.42 |
| SE | 0.67 | 0.72 | 1.39 | 1.51 | 0.77 | 0.83 | |
| t-value | 4.67*** | 4.52*** | 1.89 | 1.82 | 4.26*** | 4.14*** | |
| Lower CI | 1.79 | 1.82 | −0.15 | −0.26 | 1.74 | 1.77 | |
| Upper CI | 4.46 | 4.70 | 5.41 | 5.77 | 4.81 | 5.07 | |
| RCMAS | PE | 5.93 | 5.44 | 3.39 | 0.23 | 6.47 | 6.29 |
| SE | 1.10 | 1.29 | 2.67 | 3.34 | 1.22 | 1.40 | |
| t-value | 5.41*** | 4.21*** | 1.27 | 0.07 | 5.31*** | 4.5*** | |
| Lower CI | 3.74 | 2.86 | −1.94 | −6.43 | 4.04 | 3.50 | |
| Upper CI | 8.12 | 8.03 | 8.72 | 6.90 | 8.91 | 9.09 | |
| CDI | PE | 13.07 | 12.67 | −3.77 | −2.05 | 16.54 | 15.68 |
| SE | 1.87 | 1.86 | 3.59 | 3.92 | 1.65 | 1.74 | |
| t-value | 7.01*** | 6.82*** | −1.05 | −0.52 | 10.02*** | 9.03*** | |
| Lower CI | 0.93 | 8.96 | −10.92 | −9.86 | 13.25 | 12.22 | |
| Upper CI | 16.37 | 16.37 | 3.39 | 5.77 | 19.83 | 19.14 | |
| CBCL - I | PE | 13.69 | 11.23 | 15.60 | 8.17 | 12.75 | 10.85 |
| SE | 2.87 | 2.71 | 3.85 | 3.88 | 2.17 | 1.89 | |
| t-value | 4.78*** | 4.14*** | 4.05*** | 2.11* | 5.86*** | 5.74*** | |
| Lower CI | 7.97 | 5.82 | 7.91 | 0.43 | 8.41 | 7.08 | |
| Upper CI | 19.41 | 16.64 | 23.29 | 15.91 | 17.09 | 14.63 | |
Note. RM-ANOVAs revealed overall significant effects for time across conditions on the ADIS- CSR [F (2, 70) = 86.86, p < .01], ADIS-C [F (2, 66) = 17.03, p < .01], ADIS-P [F (2, 67) = 11.32, p < .01], RCMAS [F (2, 66) = 14.65, p < .01], CDI [F (2, 69) = 24.86, p < .01], and CBCL-I [F (2, 67) = 25.23, p < .01] in the expected direction; The CDI showed a time × condition effect [F (2, 69) = 13.71, p < .01]. PE = parameter estimate. SE = standard error, CI = 95% Confidence Interval. Pre = pretest, Post = posttest (3-month), FU = follow-up (6 months). ADIS-CSR = Anxiety Disorders Interview Schedule- Clinician’s Severity Rating, ADIS-C = Anxiety Disorders Interview Schedule-Child symptom count, ADIS-P = Anxiety Disorders Interview Schedule-Parent symptom count about child, RCMAS = Revised Children’s Manifest Anxiety Scale (Total Anxiety Scale), CDI = Children’s Depression Inventory, CBCL-I = Child Behavior Checklist – Internalizing,
p<.05,
p<.01,
p < .0001.
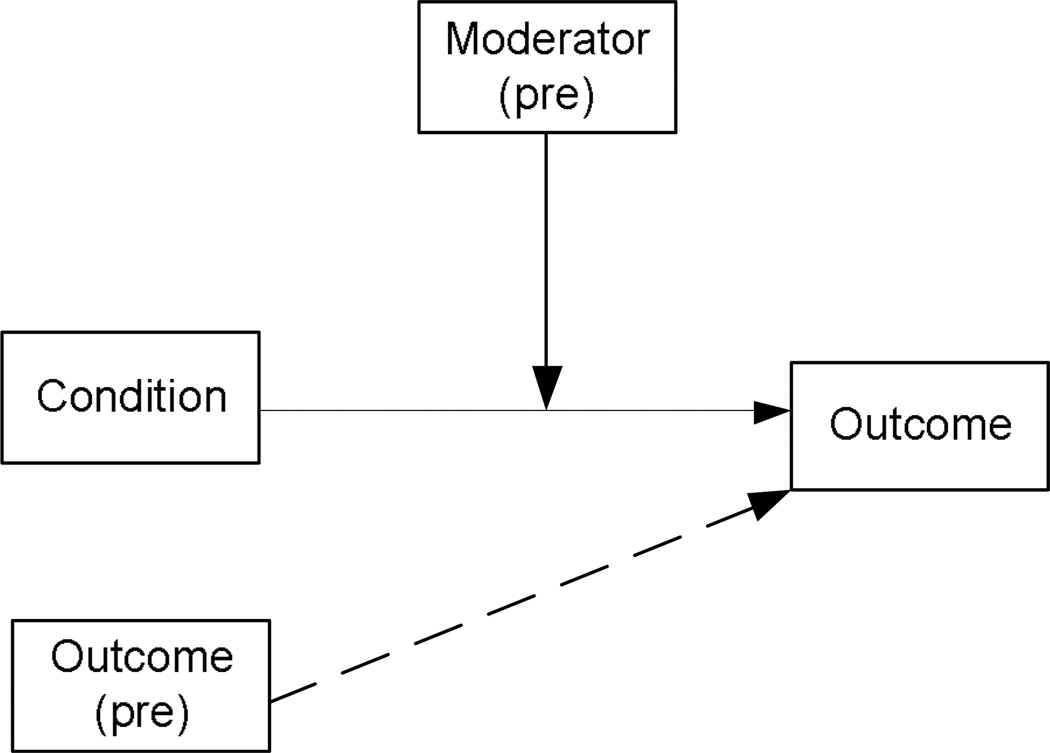
The Role of Ethnicity and Language were estimated using PROC REG with PROC MI and PROC MIANALYZE. As shown in Figure 2, moderation was explored using an interaction term between condition and the moderator variable to predict each outcome, with pretest levels of the measured outcome as a covariate (Baron & Kenny, 1986; Kraemer et al., 2002). Pretest scores were included in the models as control variables because partialling-out these variables converts the posttest scores into a residual change variable (Cole & Maxwell, 2003), which typically helps improve power (Fitzmaurice, Laird, & Ware, 2004). As shown in Table 3, neither Latino ethnicity nor Spanish language moderated program effects measured by the ADIS-C/P-CSR or anxiety symptom counts based on the ADIS-C or ADIS-P. In addition, program effects on the additional outcome measures were not moderated by Latino ethnicity or Spanish language. In other words, the cognitive and behavioral procedures applied seem as promising for Latino (including when administered in Spanish) as found for Caucasian children with anxiety symptoms or anxiety diagnoses.
Figure 2.
Moderation model with dashed lines denoting the covariate
Table 3.
Results from the Ethnicity and Language Moderation Analyses
| Pre to Post |
Pre to FU |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Intercept | Outcome (Pre) |
Ethnicity | Condition | Ethnicity × Condition |
Intercept | Outcome (Pre) |
Ethnicity | Condition | Ethnicity × Condition |
||
| ADIS-CSR | B | 0.10 | 0.30 | −0.53 | 0.66 | −0.34 | −0.73 | 0.19 | 1.10 | 1.86 | −1.75 |
| SE | 1.03 | 0.15 | 1.06 | 0.91 | 1.23 | 1.49 | 0.22 | 1.49 | 1.47 | 1.61 | |
| ADIS-C | B | 1.69 | −0.03 | −0.70 | 0.48 | 0.05 | −0.19 | 0.13 | 0.91 | 1.64 | −1.56 |
| SE | 0.95 | 0.08 | 1.28 | 1.04 | 1.46 | 1.59 | 0.11 | 1.49 | 1.56 | 1.67 | |
| ADIS-P | B | 0.52 | 0.12 | 1.52 | 1.02 | −0.80 | 0.48 | 0.14 | 1.74 | 2.48 | −3.49 |
| SE | 1.80 | 0.13 | 2.34 | 1.96 | 2.64 | 2.26 | 0.15 | 2.48 | 2.48 | 2.89 | |
| RCMAS | B | 2.67 | 0.32 | 7.37 | −0.36 | −8.41 | 7.53 | 0.34 | 2.96 | −2.88 | −7.49 |
| SE | 3.49 | 0.15 | 5.13 | 3.29 | 5.42 | 4.62 | 0.18 | 6.96 | 4.33 | 6.88 | |
| CDI | B | 28.63 | −0.10 | 0.02 | −16.43 | 0.25 | 30.86 | −0.22 | −2.02 | −16.15 | 1.77 |
| SE | 16.12 | 0.62 | 7.91 | 5.43 | 8.37 | 17.77 | 0.67 | 9.93 | 7.43 | 10.21 | |
| CBCL-I | B | 3.96 | 0.06 | −0.18 | 4.61 | −2.74 | 6.34 | 0.28 | 7.90 | −2.07 | −9.58 |
| SE | 3.54 | 0.08 | 4.50 | 3.36 | 4.94 | 5.25 | 0.12 | 6.43 | 4.73 | 6.50 | |
| Intercept | Outcome (Pre) |
Language | Condition | Language × Condition |
Intercept | Outcome (Pre) |
Language | Condition | Language × Condition |
||
| ADIS-CSR | B | 0.00 | 0.27 | −0.18 | 0.47 | 0.18 | −0.11 | 0.17 | 0.45 | 0.83 | 0.00 |
| SE | 0.95 | 0.16 | 1.61 | 0.72 | 1.72 | 1.26 | 0.22 | 2.27 | 1.05 | 2.20 | |
| ADIS-C | B | 1.38 | −0.05 | 0.09 | 0.34 | 0.53 | 0.30 | 0.11 | 0.44 | 0.78 | −0.19 |
| SE | 0.76 | 0.08 | 1.64 | 0.79 | 1.75 | 1.26 | 0.11 | 2.21 | 1.20 | 2.37 | |
| ADIS-P | B | 1.38 | 0.09 | 0.69 | 0.56 | −0.12 | 1.28 | 0.17 | 0.25 | 0.88 | −1.33 |
| SE | 1.48 | 0.13 | 3.54 | 1.62 | 3.79 | 1.65 | 0.15 | 3.83 | 1.78 | 3.97 | |
| RCMAS | B | 5.81 | 0.34 | 4.10 | −4.30 | −4.26 | −0.11 | 0.17 | 0.45 | 0.83 | 0.00 |
| SE | 3.47 | 0.15 | 7.90 | 2.86 | 8.09 | 1.26 | 0.22 | 2.27 | 1.05 | 2.20 | |
| CDI | B | 27.61 | −0.05 | −1.17 | −15.84 | −0.98 | 28.46 | −0.15 | −2.01 | −14.88 | −0.06 |
| SE | 15.72 | 0.62 | 11.72 | 5.23 | 11.92 | 16.57 | 0.68 | 13.13 | 6.81 | 13.47 | |
| CBCL-I | B | 3.65 | 0.07 | −0.10 | 3.88 | −2.36 | 11.01 | 0.25 | 2.26 | −7.07 | −1.97 |
| SE | 3.25 | 0.08 | 8.09 | 2.89 | 8.55 | 4.71 | 0.12 | 9.99 | 4.12 | 9.71 | |
Note. ADIS-C = Anxiety Disorders Interview Schedule-Child symptom count, ADIS-P = Anxiety Disorders Interview Schedule-Parent symptom count, ADIS-CSR = Anxiety Disorders Interview Schedule- Clinician’s Severity Rating, RCMAS = Revised Children’s Manifest Anxiety Scale (Total Anxiety Scale), CDI = Children’s Depression Inventory, CBCL-I = Child Behavior Checklist – Internalizing. In the analyses, ethnicity: 1= Latino, 0= Caucasian; language: 1= Spanish, 0=English; condition: 1=child plus parent, 0=child only.
Discussion
Building on a substantial body of child anxiety prevention and treatment research, this study is the first to examine the effects of an indicated anxiety prevention and early intervention protocol using a sample of anxious Hispanic/Latino and Caucasian children (Fisak et al., 2010; Silverman et al., 2008). Evaluation of the protocol showed significant improvements at posttest and short-term follow-up across clinician, child, and parent measures. In addition, gains and maintenance were most evident for children whose parents were more involved in the intervention. Although, improvements also were found for children whose parents were less involved in the intervention across three of the six outcomes measured. Findings showing variations by degree of parent involvement are noteworthy because research has been equivocal (perhaps due to variability in content, number, and format of parent sessions; Barmish & Kendall, 2005). Our findings, however, provide some evidence that training caregivers to reduce reinforcement of child anxious behaviors and to help the child practice the skills learned in session could be critical. As such, future studies should test whether changes in parent behaviors mediate response, a topic that is severely underdeveloped in the child anxiety area (Alfano, et al., 2009; Kendall & Treadwell, 2007).
Another focus of this study was to evaluate the role of ethnicity and language on program effects. In the anxiety prevention area, Barrett, Sonderegger and Xenos (2003) adapted the FRIENDS for Life anxiety program for former Yugoslavian and Chinese immigrant children whereas Cooley-Strickland, Griffin, Darney, Otte, and Ko (2011) reported on an adaptation for African American children. Both of these studies reported positive program effects for the ethnic minority children participants. This is the first controlled study, however, to focus on Hispanic/Latino children. In this study, Hispanic/Latino children (including those targeted in Spanish) benefited from the protocol as much as their Caucasian counterparts. This result is consistent with Pina et al. (2003) but unlike Pina et al. this study relied on a sample largely comprised of Mexican-origin youth, several of whom received services in Spanish. Whereas the ethnicity/language finding is encouraging, adult studies have shown that Latinos treated in Spanish respond better to culturally adapted interventions (Griner & Smith, 2006). For this reason, a stronger test of cross-ethnic equivalence of program effects might be necessary to determine whether our prevention and early intervention efforts are as robust for Hispanic/Latino children as they are for their Caucasian counterparts (a test that would require a larger sample size).
The present study is limited in several ways. First, this study relied on a relatively small sample size and a short-term follow-up. As such, null results may reflect low power for the analyses and should be viewed tentatively. Second, the small sample size for this study precluded evaluating differential child response at the indicated prevention versus treatment of diagnosable anxiety disorders levels. Third, tests of program effects relied on anxiety indicators with a restricted range (e.g., ADIS-C/P CSR), which could have limited the study’s ability to show additional significant effects. Fourth, the focus on ethnicity and language is an important first step but it shows little about possible within-group response variability to the intervention. That is, it remains unknown whether acculturation, enculturation, or cultural values impact program effects for Hispanic/Latinos. These are important issues that warrant careful consideration in future research especially as the field moves forward to secure evidence-based prevention and treatment services for all children.
Acknowledgments
This study was supported in part by award numbers K01MH086687 and L60MD001839 from the National Institute of Mental Health and the National Center on Minority Health and Health Disparities, as well as funding from the Institute for Mental Health Research awarded to the first author. The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies.
References
- Achenbach TM. Manual for the Child Behavior Checklist/4–18. Burlington, VT: University of Vermont, Department of Psychiatry; 1991. [Google Scholar]
- Albano AM, Silverman WK. Guide to the use of the Anxiety Disorders Interview Schedule for DSM-IV-Child and Parent Versions. London, UK: Oxford University Press; 1996. [Google Scholar]
- Alfano CA, Pina AA, Villalta IK, Beidel DC, Ammerman RT, Crosby LE. Mediators and moderators of outcome in the behavioral treatment of childhood social phobia. Journal of American Academy of Child and Adolescent Psychiatry. 2009;48:945–953. doi: 10.1097/CHI.0b013e3181af8216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barmish AJ, Kendall PC. Should parents be co-clients in cognitive-behavioral therapy for anxious youth? Journal of Clinical Child and Adolescent Psychology. 2005;34:569–581. doi: 10.1207/s15374424jccp3403_12. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Barrett PM, Sonderegger R, Xenos S. Using FRIENDS to combat anxiety and adjustment problems among young migrants to Australia: A national trial. Clinical Child Psychology and Psychiatry. 2003;8:241–260. [Google Scholar]
- Cole DA, Maxwell SE. Testing mediational models with longitudinal data: Questions and tips in the use of structural equation modeling. Journal of Abnormal Psychology. 2003;112:558–577. doi: 10.1037/0021-843X.112.4.558. [DOI] [PubMed] [Google Scholar]
- Cooley-Strickland MR, Griffin RS, Darney D, Otte K, Ko J. Urban African American youth exposed to community violence: A school based anxiety preventive intervention efficacy study. Journal of Prevention and Intervention in the Community. 2011;39:149–166. doi: 10.1080/10852352.2011.556573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello EJ, Egger HL, Angold A. The developmental epidemiology of anxiety disorders: Phenomenology, prevalence, and comorbidity. Child and Adolescent Psychiatric Clinics of North America. 2005;14:631–648. doi: 10.1016/j.chc.2005.06.003. [DOI] [PubMed] [Google Scholar]
- Dumka L, Gonzales N, Wood J, Formoso D. Using qualitative methods to develop contextually relevant measures and preventive interventions: An illustration. American Journal of Community Psychology. 1998;26:605–637. doi: 10.1023/a:1022145022830. [DOI] [PubMed] [Google Scholar]
- Fisak BJ, Richard D, Mann A. The prevention of child and adolescent anxiety: A meta-analytic review. Prevention Science. 2011;12:255–268. doi: 10.1007/s11121-011-0210-0. [DOI] [PubMed] [Google Scholar]
- Fitzmaurice GM, Laird NM, Ware JH. Applied longitudinal analysis. Hoboken, NJ: Wiley & Sons; 2004. [Google Scholar]
- Ginsburg GS, Silverman WK, Kurtines WK. Family involvement in treating children with phobic and anxiety disorders: A look ahead. Clinical Psychology Review. 1995;15:457–473. [Google Scholar]
- Griner D, Smith TB. Culturally adapted mental health intervention: A meta-analytic review. Psychotherapy: Theory, Research, Practice, Training. 2006;43:531–548. doi: 10.1037/0033-3204.43.4.531. [DOI] [PubMed] [Google Scholar]
- Hudson JL, Rapee RM. Psychopathology and the family. New York, NY: Elsevier Science; 2005. [Google Scholar]
- Humes K, Jones N, Ramirez R. Overview of race and Hispanic origin, 2010 census briefs. U.S. Department of Commerce, Census Bureau; 2011. Retrieved from http://www.census.gov/prod/cen2010/briefs/c2010br-02.pdf. [Google Scholar]
- Jaccard J. Interaction effects in factorial analysis of variance. Thousand Oaks, CA: Sage Publications, Inc; 1998. [Google Scholar]
- Kazdin AE. Child, parent and family dysfunction as predictors of outcome in cognitive behavioral treatment of antisocial children. Behaviour Research and Therapy. 1995;33:271–281. doi: 10.1016/0005-7967(94)00053-m. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Grove WM. Normative comparisons in therapy outcome. Behavioral Assessment. 1988;10:147–158. [Google Scholar]
- Kendall PC, Hudson JL, Gosch E, Flannery-Schroeder E, Suveg C. Cognitive-behavioral therapy for anxiety disordered youth: a randomized clinical trial evaluating child and family modalities. Journal of Consulting and Clinical Psychology. 2008;76:282–297. doi: 10.1037/0022-006X.76.2.282. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Treadwell KRH. The role of self-statements as a mediator in treatment for youth with anxiety disorders. Journal of Consulting and Clinical Psychology. 2007;75:380–389. doi: 10.1037/0022-006X.75.3.380. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Ruscio AM, Shear K, Wittchen H. Epidemiology of anxiety disorders. In: Stein MB, editor. Oxford handbook of anxiety and related disorders. New York, NY: Oxford University Press; 2009. pp. 19–33. [Google Scholar]
- Kovacs M. Rating scales to assess depression in school-aged children. Acta Paedopsychiatrica: International Journal of Child and Adolescent Psychiatry. 1981;46:305–315. [PubMed] [Google Scholar]
- Kraemer HC, Wilson GT, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Archives of General Psychiatry. 2002;59:877–883. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- Pela OA, Reynolds CR. Cross-cultural application of the Revised Children's Manifest Anxiety Scale: Normative and reliability data for Nigerian primary school children. Psychological Reports. 1982;51:1135–1138. doi: 10.2466/pr0.1982.51.3f.1135. [DOI] [PubMed] [Google Scholar]
- Pina AA. Acercamiento: Child and Adolescent Anxiety Program. Phoenix, AZ: Lulu Enterprises, Inc; 2006. [Google Scholar]
- Pina AA, Little M, Knight GP, Silverman WK. Cross-ethnic measurement equivalence of the RCMAS in Hispanic/Latino and European American youth with anxiety disorders. Journal of Personality Assessment. 2009;91:58–61. doi: 10.1080/00223890802484183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pina AA, Silverman WK, Fuentes RM, Kurtines WK, Weems CF. Exposure-based cognitive-behavioral treatment for phobic and anxiety disorders: Treatment effects and maintenance for Hispanic/Latino relative to European-American youths. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42:1179–1187. doi: 10.1097/00004583-200310000-00008. [DOI] [PubMed] [Google Scholar]
- Pina AA, Villalta IK, Zerr AA. Exposure-based cognitive behavioral treatment of anxiety in youth: An emerging culturally-prescriptive framework. Behavioral Psychology. 2009;17:111–135. [Google Scholar]
- Reynolds CR, Richmond BO. What I think and feel: A revised measure of children's manifest anxiety. Journal of Abnormal Child Psychology. 1978;6:271–280. doi: 10.1007/BF00919131. [DOI] [PubMed] [Google Scholar]
- Roberts RE, Roberts CR, Xing Y. Prevalence of youth-reported DSM-IV psychiatric disorders among African, European, and Mexican American adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45:1329–1337. doi: 10.1097/01.chi.0000235076.25038.81. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Albano AM. Anxiety Disorders Interview Schedule for DSM-IV: Child and Parent Versions. New York, NY: Oxford University Press; 1996. [Google Scholar]
- Silverman WK, Kurtines WM. Anxiety and phobic disorders: A pragmatic approach. New York, NY: Plenum Press; 1996. [Google Scholar]
- Silverman WK, Pina AA, Viswesvaran C. Evidence-based psychosocial treatments for phobic and anxiety disorders in children and adolescents. Journal of Clinical Child and Adolescent Psychology. 2008;37:105–130. doi: 10.1080/15374410701817907. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Saavedra LM, Pina AA. Test-retest reliability of anxiety symptoms and diagnoses with Anxiety Disorders Interview Schedule for DSM-IV: Child and Parent Versions. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:937–944. doi: 10.1097/00004583-200108000-00016. [DOI] [PubMed] [Google Scholar]
- Smucker MR, Craighead WE, Craighead LW, Green BJ. Normative and reliability data for the Children's Depression Inventory. Journal of Abnormal Child Psychology. 1986;14:25–39. doi: 10.1007/BF00917219. [DOI] [PubMed] [Google Scholar]
- Wood JJ, Chiu AW, Hwang W, Jacobs J, Ifekwunigwe M. Adaptive cognitive-behavioral therapy for Mexican American students with anxiety disorders: Recommendations for school psychologists. School Psychology Quarterly. 2008;23:515–532. [Google Scholar]