Abstract
Despite the promise of RNA interference (RNAi) and its potential, e.g. for use in cancer therapy, several technical obstacles must first be overcome. The major hurdle of RNAi-based therapeutics is to deliver nucleic acids across the cell’s plasma membrane. This study demonstrates that exosome vesicles derived from humans can deliver short interfering RNA (siRNA) to human mononuclear blood cells. Exosomes are nano-sized vesicles of endocytic origin that are involved in cell-to-cell communication, i.e. antigen presentation, tolerance development and shuttle RNA (mainly mRNA and microRNA). Having tested different strategies, an optimized method (electroporation) was used to introduce siRNA into human exosomes of various origins. Plasma exosomes (exosomes from peripheral blood) were used as gene delivery vector (GDV) to transport exogenous siRNA to human blood cells. The vesicles effectively delivered the administered siRNA into monocytes and lymphocytes, causing selective gene silencing of mitogen-activated protein kinase 1. These data suggest that human exosomes can be used as a GDV to provide cells with heterologous nucleic acids such as therapeutic siRNAs.
INTRODUCTION
Exosomes are nano-sized vesicles (30–90 nm in size) produced by many cell types, including dendritic cells (DC) (1), B cells (2), T cells (3), mast cells (4), epithelial cells (5) and tumor cells (6). These vesicles are formed by inward budding of late endosomes and are then released to the extracellular environment upon fusion with the plasma membrane (7). They have been detected in body fluids such as peripheral blood (8,9), urine (10), malignant effusions (11) and bronchoalveolar lavage fluid (12). The functions of exosomes are not fully understood, but it has been shown that these vesicles are involved in signal transduction, antigen presentation to T cells (13) and tolerance development (5,14).
In 2007, we demonstrated that exosomes derived from various cell types contain a substantial amount of RNA (mainly mRNA and microRNA, but little or no 18S or 28S ribosomal RNA) (15). More importantly, we discovered that the exosome vesicles shuttle RNA between cells, an activity which served as a novel means of cell-to-cell communication. The RNA present in exosomes was therefore termed ‘exosomal shuttle RNA’ (esRNA). In many subsequent studies, other investigators confirmed the presence of RNA in exosomes originating from different cell types or from patients with different diseases (9,16–22). Therefore, it has been speculated (19,20,23) that the RNA content of exosomes might be useful for the discovery of new biomarkers for early detection of diseases such as cancer.
As exosomes naturally carry RNA between cells, we hypothesized that this property might be useful in gene therapy, in which a vector is used to deliver therapeutic nucleic acids to the patient’s target cells. Two types of vectors, viral and non-viral, have commonly been used to deliver DNA or RNA molecules to cells for therapeutic purposes to mediate gene knockdown via RNA interference (RNAi). However, the methods used for gene therapy have still not proven very successful in clinical trials due to the lack of gene delivery vectors (GDV) that are safe, efficient, organ/cell-specific and which do not cause immune and inflammatory responses. Exosomes from a patient (host tissues) can practically be used as a non-immunogenic GDV for the same individual (24). Recently, Alvarez-Erviti et al. (25) have shown that exosomes from immature dendritic cells which express the surface protein Lamp2 can be used as GDV of short interfering RNA (siRNA) to microglia and oligodendrocytes in the mouse brain. They showed that siRNA against BACE1, which mediates the formation of the peptide that forms β-amyloid plaques, can be delivered to neurons via exosomes, causing down-regulation of BACE1. Consequently, this led to a significant decrease in β-amyloid levels in the brains of wild-type mice (25).
In this report, we examined whether human exosomes can deliver exogenous nucleic acids to recipient cells. Here, we show that plasma exosomes can be used as GDVs of siRNA to T cells and monocytes. These findings suggest that exosomes derived from human cells can be utilized in gene therapy to provide target cells with heterologous nucleic acids such as therapeutic siRNAs.
MATERIALS AND METHODS
In this study, we have used exosomes attached to beads only for the characterization of exosomes (e.g. western blotting and FACS for the detection of CD63, CD81 and CD9). However, exosomes coupled to beads were never used in experiments when these vesicles act as delivery-vector of siRNA to cells. To apply exosomes as delivery vectors, the ultracentrifuge pellet of exosomes were mixed with siRNA, incubated on ice for 10 min and exposed for electroporation. Samples containing exosomes and siRNA, without the electric pulse, were used as a negative control. These samples were then co-cultured with the recipient cells, e.g. monocytes and lymphocytes, in order to deliver the heterologous RNA to cells.
Cells
HeLa and lung cancer cells HTB-177 (ATCC, USA) were prepared and cultured as described by ATCC with some modifications. Peripheral blood mononuclear cells (PBMCs) were prepared from buffy coats from healthy donors (Sahlgrenska University hospital, Gothenburg, Sweden) by lymphoprep gradient centrifugation (Axis-Shield Poc As, Norway). CD14+ monocytes and CD14− cells, herein termed lymphocytes, were purified from PBMCs by positive or negative selection, respectively, using CD14 microbeads and LS column (MACS, Miltenyibiotec). PBMCs, CD14+ monocytes or CD14− lymphocytes were grown in RPMI-1640 medium supplemented with 10% foetal bovine serum (FBS) depleted from exosomes and 2 mM l-glutamine. For electroporation assays, HeLa, HTB-177, PBMC cells, monocytes or lymphocytes were plated in 24-well plates at a density of 0.5 × 106 cells/well. PBMCs, monocytes and lymphocytes were activated with phorbol myristate acetate (PMA) at a final concentration of 1 µg/ml. All cell culture mediums were supplemented with 100 µg/ml streptomycin/penicillin (Sigma Aldrich, Sweden)
Exosome purification
Exosomes were isolated by differential centrifugations and micro-filtration as previously described (9,14,15). Briefly, cell supernatants were harvested, centrifuged at 300g for 10 min to eliminate cells and at 16 500g for 30 min followed by filtration through a 0.22 µm filter. Exosomes were pelleted by ultracentrifugation at 120 000g for 70 min. Exosomes from plasma were prepared by centrifugation of buffy coat at 900g for 20 min to isolate the plasma followed by differential centrifugations and filtration as for HeLa and HTB-177 cells.
Size determination
Size determination of isolated exosomes was performed using a Zetasizer Nano ZS (Malvern Instruments) according to the manufacturer’s instructions.
Exosome bead coupling and flow cytometry
A total of 4 µm aldehyde/sulfate latex beads (Invitrogen, Sweden) were incubated with purified anti-CD63 or anti-CD9 antibody (BD Biosciences, Sweden) overnight at room temperature with gentle agitation according to manufacturer’s instructions. A total of 0.45 mg exosomes were incubated with 2 × 106 anti-CD63 or anti-CD9 beads in 80 µl PBS for 15 min at room temperature; the volume was made up to 400 µl and incubated 3 h at room temperature on a rotator. To block remaining binding sites, exosome coated beads were incubated for 30 min with 100 mM glycine. After two washes in PBS with 3% FBS, exosome coated beads were stained with FITC or PE conjugated CD81, CD9 or CD63 antibody or isotype control (BD Biosciences). For re-isolation and FACS analysis of chemically transfected or electroporated exosomes, the exosomes were incubated with aldehyde/sulfate latex beads for 3 h at room temperature with gentle shaking or 30 min at 37°C followed by overnight at 4°C, washed in PBS and analyzed. For the flow cytometry analysis of PBMCs, the cells were harvested, washed and blocked for 15 min at RT with Beriglobin 100 µg/ml (CSL Behring GmbH, Germany) followed by staining for cell surface markers performed by using antibodies against CD19-FITC, CD3-PerCP and CD14-APC (BD Biosciences). Flow cytometry analysis of isolated CD14 positive and CD14 negative cells was performed using CD19-PE, CD3-APC and CD14-PE antibodies (BD Biosciences). The viability of cells was determined by flow cytometry using LIVE/DEAD Fixable Violet Dead Cell Stain Kit (Invitrogen). All FACS data were collected on a FACSCantoII (Becton Dickinson, San Diego CA) and analyzed with FlowJo software (TreeStar).
Chemical transfection
Chemical transfection of siRNA into exosomes was carried out according to the manufacturer’s instructions in RNAi Human/Mouse Starter Kit (Quiagen, Hilden, Germany). siRNA was added to 100 µl PBS at a final concentration of 2 µmol/ml. After adding HiPerFect transfection reagent, the mixture was incubated for 10 min at RT. In order to remove the excess of micelles, the exosomes were re-isolated using aldehyde/sulfate latex beads.
Electroporation
For electroporation assays, HeLa, HTB-177 and plasma exosomes were diluted in cytomix transfection buffer. Mm/Hs mitogen-activated protien kinase 1 (MAPK1) siRNA (sense strand: 5′-GUUCGAGUAGCUAUCAAGATT-3′) or AllStars negative control siRNA Alexa flour488 (Quiagen, Hilden, Germany) at a final concentration of 2 µmol/ml were added to 100 µl of exosome sample. The mixtures were transferred into ice cold 0.4 cm electroporation cuvettes and electroporated at 0.150 kV/100 µF. Non-electroporated samples were used as negative controls. All electroporations were performed on a Gene pulser II System (Bio-Rad Laboratories).
RNA isolation
Total RNA was isolated using Trizol reagent (Invitrogen, Sweden) according to the manufacturer's instructions. Detection and quality control of RNA was performed using Agilent RNA 6000 Nano Kit on an Agilent 2100 Bioanalyzer® (www.chem.agilent.com).
Detection of siRNA in exosomes
MAPK-1 siRNA transfected exosomes were incubated with 45 × 103 aldehyde/sulfate latex beads (4 µm, 4.2 g/100 ml, Invitrogen, Sweden) at room temperature for 1 h. The mixture was washed twice in PBS. The total RNA was isolated using Trizol (Invitrogen, Sweden). For RNA detection, exosomal RNA was transferred to a nylon hybridization transfer membrane (Hybond-N+, Amersham Biosciences, Sweden) using a Bio-Dot SF (Bio-Rad). The membranes were hybridized with a Digoxigenin-labeled RNA probe (Exiqon) (5′-3′: /5DigN/CAGAGCTTTGGAGTCAGCATT/3Dig_N) complementary to the MAPK-1 siRNA. Detection of the hybridized probe was performed by using DIG Nucleic Acid Detection Kit (Roche Applied Science, USA) following the manufacturer's instructions.
Detection of siRNA in cells
Exosomes (electroporated and non-electroporated) were co-cultured with monocytes or lymphocytes during 24 h. However, the lung cancer cell line HTB-177 was used in Figure 2F. The cells were then isolated and washed three times with PBS and total RNA was isolated from the cells using Trizol. Equal amount of total RNA was applied to a nylon hybridization transfer membrane using slot-blot device. The membranes were then hybridized with the Dig-labelled siRNA-probe and the detection was performed as described above.
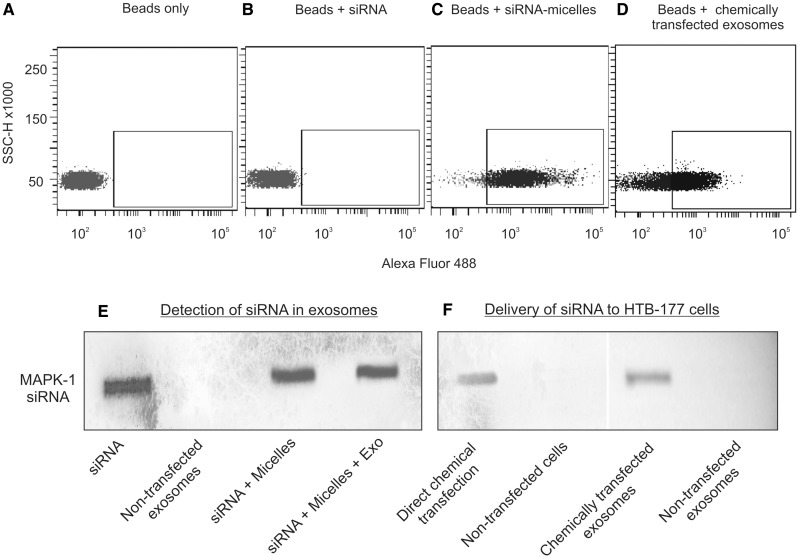
Figure 2.
Flow cytometry and northern slot blot of exosomes following chemical transfection. siRNA was embedded into lipid micelles according to the manufacturer’s instructions. The embedded siRNA was mixed with exosomes and incubated overnight. To eliminate the excess siRNA embedded in transfection complexes, the exosomes were purified using latex beads. The beads were washed twice with PBS to eliminate the excess of un-specific bound siRNA molecules. The presence of fluorescently labeled siRNA was determined by flow cytometry and northern blotting (slot blot). Panel A–D shows the results of flow cytometry for the detection of Alexa Fluor-488 labeled siRNA, beads only (A), beads plus siRNA (B), beads plus siRNA embedded in lipid micelles (negative control; C) and chemically transfected exosomes (D). Panels E and F show the results of northern blotting using a digoxigenin-labeled probe against the administered MAPK1 siRNA. Panel E shows the presence of siRNA in exosomes and micelles. The chemically transfected exosomes were mixed with their parental cells HTB-177 and the delivery of siRNA from the exosomes to cells was determined and compared with direct transfection of cells (F). Non-transfected exosomes and cells were used as negative control.
Protein isolation and detection
For detection of exosomal proteins CD9 and CD63, pellets that remained after removal of RNA and DNA following Trizol treatments, were washed three times by storing the pellets in a solution containing 0.3 M guanidine hydrochloride in 95% ethanol for 20 min at 30°C and centrifuged at 7500g for 5 min at 4°C. Protein pellets were re-suspended in 95% ethanol, vacuum dried and dissolved in 10% sodium dodecyl sulphate (SDS). Protein extraction from monocytes and lymphocytes was performed using ProteoJET Mammalian Cell Lysis Reagent (Fermentas) according to manufacturer’s protocol. Protein concentrations were determined by DC Protein Assay reagent A and B (Bio-Rad Laboratories, Sweden). For immunoblotting, equal amounts of proteins were transferred onto polyvinylidene difluoride (PVDF) membranes (Millipore, Fischer Scientific GTF AB, Sweden) using a Bio-Dot SF (Bio-Rad) using slot-blot device. Membranes were blocked and washed three times with Tris-buffered saline buffer (TBS) and incubated with purified mouse anti-human CD9, purified mouse anti-human CD63 (BD Biosciences Pharmingen, Sweden), MAPK1 specificTag-100 antibody (Qiagen) at 1:1000 dilution in TBS tween (TBST) and 5% skim milk for 1.5 h at room temperature or 4°C overnight. Monoclonal Anti-β-Actin-Peroxidase (Sigma-Aldrich) was used as a control protein. Membranes were washed in TBST and incubated with a peroxidase coupled polyclonal rabbit anti-mouse (Yoproteins, Sweden) or an IRDye 800CW (LI-COR Biosciences, GmbH) goat anti-mouse antibody for 1 h. Detection of specific bands was carried out by ECL-plus (GE Healthcare, Amersham, Sweden) visualized on a Molecular Imager ChemiDoc XRS system using Quantity One software (Bio-Rad Laboratories, Copenhagen) or Odyssey infrared imaging system (LI-COR biosciences) as recommended by the suppliers. Quantities of MAPK-1 were obtained by normalization of each assay to β-Actin and using of molecular densitometer (Bio-Rad GS-800).
Confocal microscopy
Exosomes electroporated with siRNA were bound to aldehyde/sulphate latex beads and incubated at room temperature for 2 h. Monocytes and lymphocytes were incubated with both non-electroporated (plasma exosomes + MAPK1 Alexa Fluor tagged siRNA) and electroporated plasma exosomes (plasma exosomes + MAPK1 Alexa Fluor tagged siRNA exposed to an electric pulse) for 3 days. For membrane staining, monocytes and lymphocytes were washed with PBS and stained with CellMask Deep Red Plasma Membrane stain (Invitrogen) at a final concentration of 2 µg/ml for 3 min at 37°C. Cells were washed twice with PBS and re-suspended in complete medium. For nucleus, staining cells received 2 µg/ml of Hoechst 33 342 (Invitrogen). Detection of MAPK1 siRNA Alexa Fluor 488, membrane and nucleus staining was performed using a confocal laser scanning microscope, LSM 700 (Carl Zeiss MicroImaging GmbH, Germany).
RESULTS
Insertion of foreign genetic material into exosomes
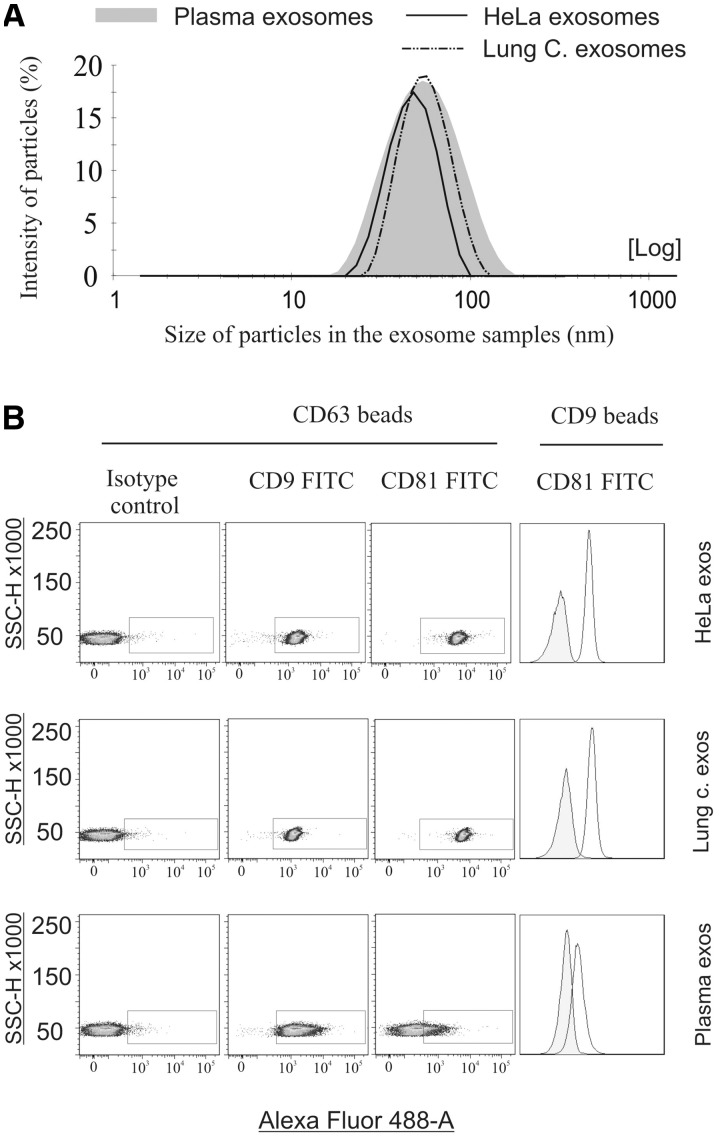
Exosomes originating from peripheral blood of healthy donors (plasma exosomes), lung cancer cells HTB-177, and HeLa cells were isolated, as described earlier (13–15). Using a Zetasizer Nano, we found that the ultracentrifuge pellets of exosomes contain spherical particles with an average size of 55 nm in diameter (ø) for the plasma exosomes, ø 48 nm for the lung cancer exosomes and ø 47 nm for the HeLa exosomes (Figure 1A), which is in the range of exosome sizes described earlier. We confirmed the identity of these vesicles as exosomes by flow cytometry analysis showing the presence of exosomal marker proteins CD9, CD63 and CD81 (Figure 1B). The vesicles were bound to aldehyde-sulfate latex beads conjugated with anti-CD9 or anti-CD63.
Figure 1.
Characterization of exosomes. Exosomes originating from peripheral blood of healthy donors (plasma exosomes), lung cancer cells HTB-177 and HeLa cells were isolated, as described earlier (13–15). The sizes of all particles between 1 and 1000 nm in diameter present in the ultracentrifuge pellets were determined using a Zetasizer Nano (A). The presence of the exosomal surface proteins CD9, CD63 and CD81 was determined using FACS (B). For the detection of exosomal markers, the exosomes were bound to aldehyde-sulfate latex beads conjugated with anti-CD9 or anti-CD63 antibodies and analyzed by FACS.
Two different strategies (electroporation and chemical transfection) were applied to introduce a double-stranded siRNA into the exosomes for therapeutic delivery into target cells. To examine the efficiency of chemical transfection, a siRNA against MAPK1 was mixed with transfection reagent to allow for the formation of transfection complexes (siRNA embedded in lipid micelles), according to the manufacturer’s instructions (RNAi Human/Mouse Starter Kit, Quiagen). The complex was then added to the exosomes (1 µg/µl) and incubated overnight. After each transfection, the exosome vesicles were purified using latex beads to eliminate the excess of free siRNA as well as siRNA embedded into the micelles. No beads were used when the vesicles were utilized as vectors for delivery of siRNA to cells. The transfer of siRNA into the exosomes was verified using flow cytometry and northern blotting (slot blotting; Figure 2). The results from flow cytometry showed that the fluorescence signal of the siRNA could be detected in exosome samples incubated with the transfection complexes (micelles; Figure 2D). However, the transfection complexes (the micelles without exosomes) also had very strong affinity for the beads (Figure 2C). Therefore, it was uncertain whether the fluorescence signals in Figure 2D originated from the exosomes or the micelles. Analysis with northern blot (Figure 2E) demonstrated, as expected, the presence of the siRNA in both micelles (siRNA + micelles) and exosomes incubated with the micelles (siRNA + Micelles + Exo). Furthermore, both samples could deliver the MAPK-1 siRNA to cells (Figure 2F). As the micelles could un-specifically be attached to the exosomes, it was indistinguishable whether the exosomes or the micelles of chemical transfection delivered exogenous nucleic acids to cells. In addition, we tested whether the excess of micelles could be separated from the exosomes using ultracentrifugation, filtration and affinity chromatography using latex beads conjugated to antibodies against the exosomal surface proteins CD63 and CD9. The results showed that it was unfeasible to separate exosome vesicles from the micelles of chemical transfection (data not shown). Therefore, chemical transfection was inapplicable for using the exosome vesicles as GDV of exogenous nucleic acids to cells.
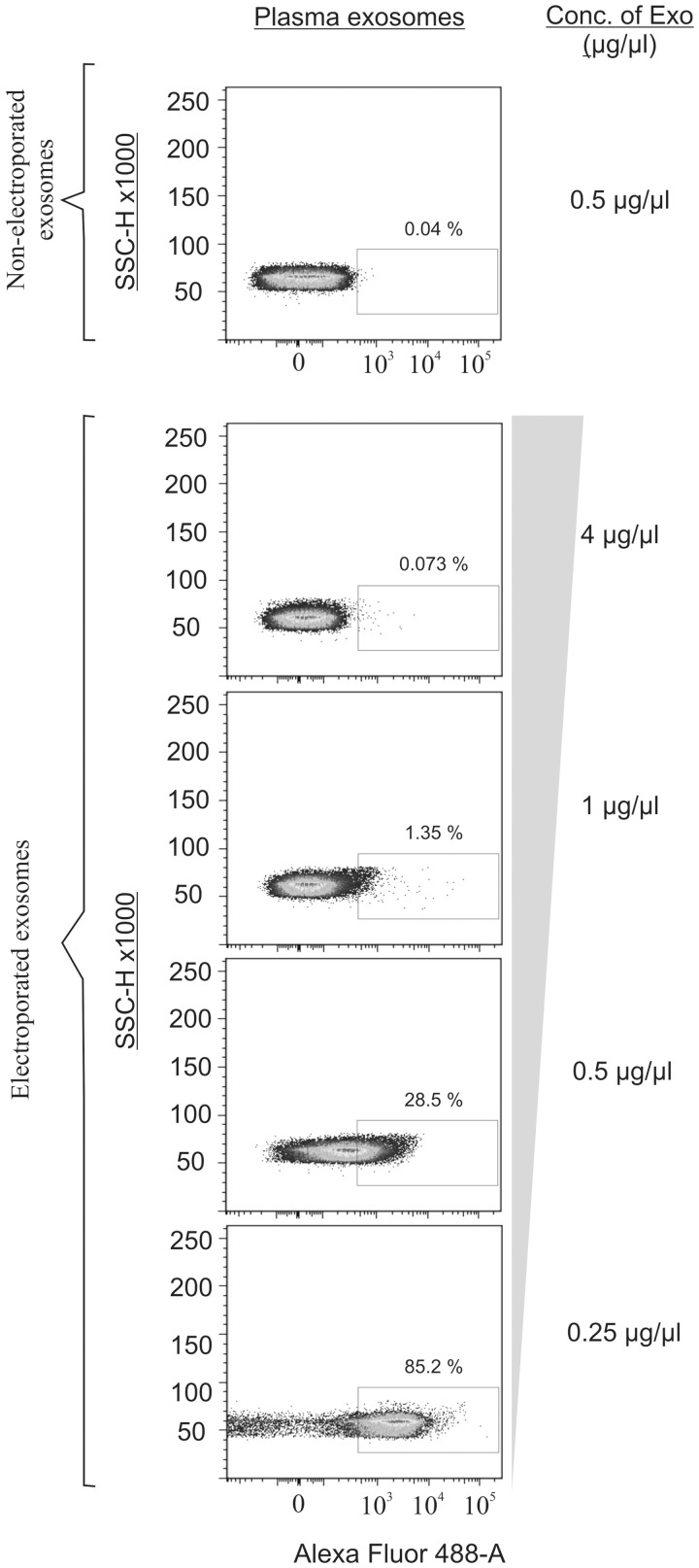
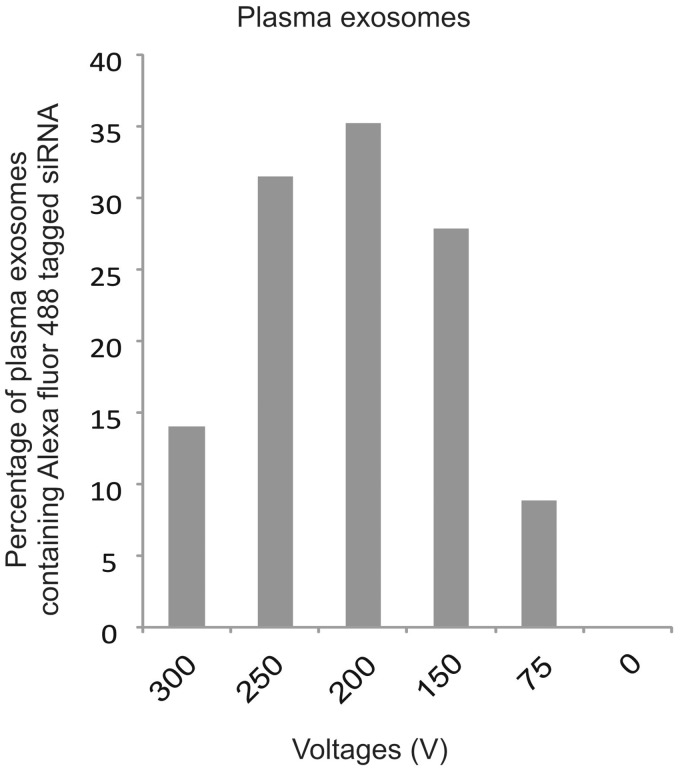
Next, the electroporation technique was used to introduce exogenous siRNAs into the exosomes. Briefly, the plasma exosome vesicles were mixed with the Alexa Fluor 488-tagged siRNA, incubated on ice for 10 min and exposed to an electric field pulse. Samples containing exosomes and siRNA but which were not exposed to the electric pulse were used as negative control. After each electroporation, the exosome vesicles were purified and washed twice to eliminate the excess free siRNA. Exosome concentrations between 0.25 and 1 µg/µl were most efficient for introducing the siRNA into the exosomes (Figure 3 and Supplementary Figure S1). Notably, the transfection efficiency was decreased at higher exosome densities. siRNA could not be detected in the non-electroporated exosome samples, confirming that the excess siRNA was depleted by purifying exosomes using latex beads. Further examination of six different voltages with constant capacitance (100 µF) revealed that voltages between 150 and 250 V were the most effective for introducing the siRNAs into the exosomes (Figure 4 and Supplementary Figure S2). In contrast, variation of capacitance (0–300 µF) and siRNA concentration (1–3 nmol/ml) did not influence the efficiency of electroporation (data not shown). The optimized parameters (Table 1) were used throughout all subsequent experiments, with the exception of the negative controls, which were not exposed to electrical pulses. The results of Table 1 are from three various kind of human exosomes (exosomes from blood plasma, the lung cancer cell line HTB-177 and HeLa cells) and the variation of exosome concentrations (5 different), voltages (5 different), capacitances (5 different) and 5 different siRNA concentrations. All the variables were tested with two different cuvettes, 0.2 and 0.4 mm gaps between the electrodes.
Figure 3.
Exosome concentration affects electroporation efficiency. To determine the optimal exosome concentration for transfection, exosomes at four different concentrations (0.25–4 µg/µl) were mixed with an Alexa Fluor 488-tagged siRNA (2 nmol/ml) and electroporated. Samples containing exosomes and siRNA, without an electric pulse, were used as a negative control. To eliminate the excess siRNA, the exosomes were purified using latex beads and the presence of siRNA in the exosomes was determined by FACS analysis.
Figure 4.
Different scenarios regarding the variation of voltages on the electroporation efficiency. The exosome vesicles were mixed with an Alexa Fluor 488-tagged siRNA against the MAPK-1 transcript, incubated on ice for 10 min, and subsequently exposed to an electric field pulse. Samples containing exosomes and siRNA, without an electric pulse, were used as a negative control. After electroporation, the exosomes were purified and the effect of varying the voltage on the electroporation efficiency was determined using FACS for the detection of the fluorescently labeled siRNA (sample 1 = 300 V and sample 5 = 75 V). Samples containing exosomes and siRNA, without an electric pulse, were used as a negative control (0 V).
Table 1.
The optimized parameters for introduction of siRNA into human exosomes using electroporation
| Concentration of exosomes | 0.25–1 µg/µl |
| Concentration of siRNA | 2 nmol/ml |
| Electroporation parameters | |
| Voltage | 150 V |
| Capacitance | 100 µF |
The presence of exogenous siRNAs inside the exosomes
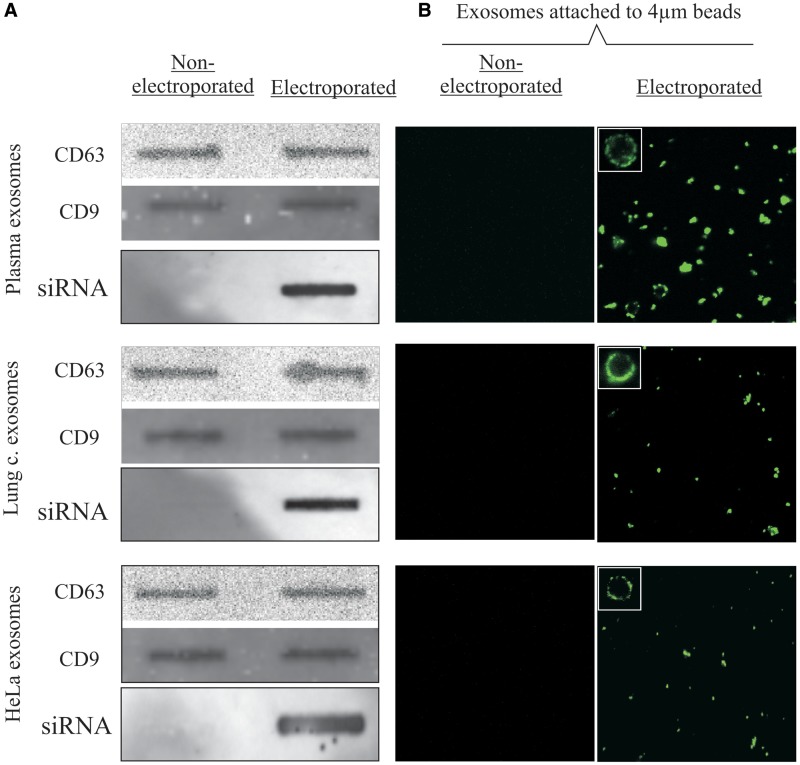
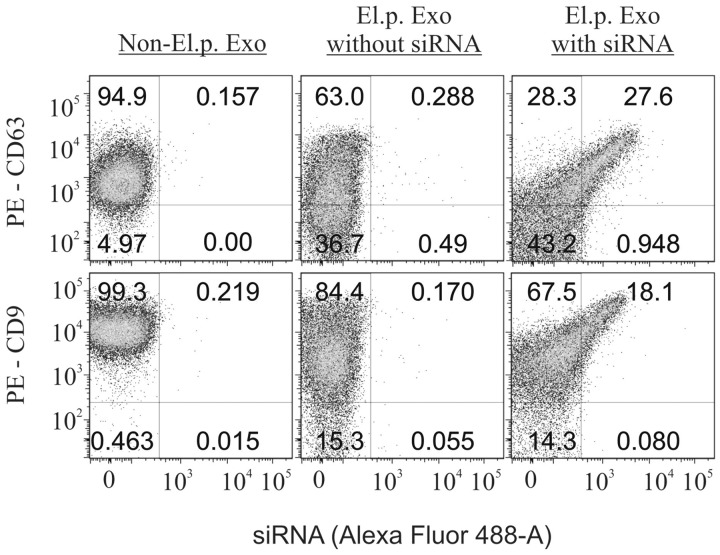
Using the optimized electroporation parameters (Table 1), the Alexa Fluor 488-tagged siRNA against MAPK1 was introduced into plasma exosomes. To confirm the presence of the exogenous siRNAs within the electroporated vesicles, total RNA and protein was extracted from the exosome samples, which had been purified by adsorption onto latex beads. The exosomal surface proteins CD9 and CD63 were detected in both the electroporated and non-electroporated samples, indicating the presence of exosome vesicles in both samples, as expected (Figure 5A). To detect whether the siRNA was inside the electroporated exosomes, total RNA was isolated from the purified exosomes, transferred to a nucleic acid transfer membrane and hybridized with a digoxigenin-labeled probe against a sequence complementary to the administered MAPK1 siRNA. This process revealed the presence of MAPK1 siRNA in the electroporated exosomes but not in the non-electroporated negative control samples (Figure 5A). Subsequent measurements by confocal microscopy (Figure 5B) confirmed the presence of the exogenous siRNA in the exosomes exposed to electroporation. The insets of microscopy images show the magnification of exosomes-beads complex. Fluorescent exosomes are attached around the beads (Figure 5B). Moreover, we counter-stained the latex beads for the fluorescent signal of siRNA and the presence of exosomal markers in order to show that (i) the fluorescent signal of siRNA is indeed associated with presence of exosomes and (ii) the differences in Alexa Fluor signal between samples do not depend on the exosome coupling to beads (e.g. if electroporation increases stickiness of exosomes for the beads compared to non-electroporated samples). The results revealed that electroporation did not improve the stickiness of exosomes to the latex beads (Figure 6). However, the electroporated exosomes had a more scattered pattern compared to non-electroporated exosomes.
Figure 5.
The presence of heterologous siRNA within the exosomes. After electroporation, the exosomes were purified using aldehyde-sulfate latex beads. Total RNA and protein was extracted from the electroporated and non-electroporated exosomes using Trizol. To determine whether exosome vesicles were present in both electroporated and non-electroporated samples, the exosomal markers CD63 and CD9 were detected by immunoblotting (A). Detection of the transfected exogenous siRNA in exosomes was performed using a digoxigenin-labeled DNA probe with a sequence complementary to the transfected MAPK1 siRNA (A). The exosome vesicles bound to the beads were examined by confocal microscopy (B).
Figure 6.
Characterization of electroporated plasma exosomes. Exosome samples (electroporated and non-electroporated) coupled to beads were counter stained for exosomal markers CD9 and CD63 conjugated to PE. Flow cytometry analyses show all events positive for AlexaFluor488 signal were positive for either CD9 or CD63 marker. To evaluate the impact of electroporation on exosomes regarding adherence to latex beads a comparison between non-electroporated and electroporated exosomes without AF488-tagged siRNA stained with PE conjugated CD9 or CD63 antibody showed a more scattered profile in electroporated exosomes.
In summary, the results from western and northern blotting, confocal microscopy and flow cytometry strongly suggest that the electroporation method was successful at introducing the heterologous siRNAs into the exosomes.
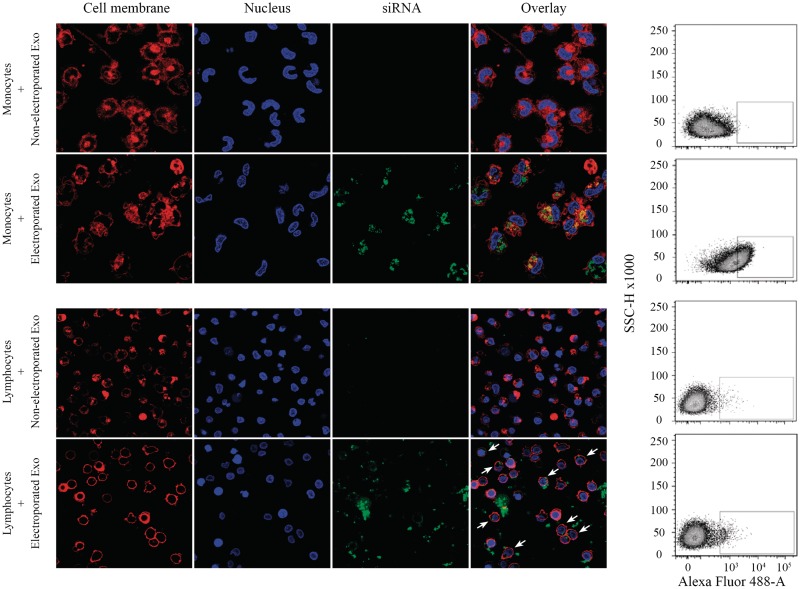
Delivery of heterologous siRNAs to PBMCs via exosomes
Given that duplex siRNAs are negatively charged polymers and therefore cannot penetrate hydrophobic cellular membranes without a carrier, we investigated whether plasma exosomes could act as a carrier to deliver heterologous genetic material to peripheral blood mononuclear cells (PBMC), and, if so, whether the siRNAs delivered via exosomes to cells would down-regulate the expression of target genes. Thus, the Alexa Fluor 488-tagged siRNA against MAPK-1 was transfected into plasma exosomes using the optimized electroporation settings (Table 1). Non-electroporated samples of exosomes and siRNA were used as a negative control. The exosomes were then co-cultured with monocytes and lymphocytes isolated from the peripheral blood of healthy donors. The purity of the monocytes and lymphocytes was determined using flow cytometry for the detection of CD14, CD3 and CD19 markers (Supplementary Figure S3). The delivery of siRNA to cells by exosomes was monitored using confocal microscopy. The cells were stained with Hoechst 33342 and CellMask Deep Red to label the nuclear and plasma membranes, respectively (Figure 7). The fluorescently labeled siRNA (green) was detected in recipient monocytes and lymphocytes following incubation with electroporated exosomes. Moreover, the exosome-delivered siRNA was mainly localized in the cytoplasm of the recipient cells. No fluorescent signal was detected in cells co-cultured with non-electroporated exosomes (Figure 7). The delivery of fluorescently labeled siRNA via exosomes to lymphocytes and monocytes was also confirmed using flow cytometry (data not shown). These results demonstrate that the plasma exosome vesicles were effective at delivering exogenous siRNA to peripheral blood mononuclear cells.
Figure 7.
Delivery of fluorescently labeled siRNA to monocytes and lymphocytes. The Alexa Fluor 488-tagged siRNA was introduced into exosomes which were subsequently co-cultured with monocytes and lymphocytes from healthy donors. Samples containing exosomes and siRNA but which were not exposed to electroporation were used as a negative control. The cells were stained with Hoechst 33342 and CellMask Deep Red to label the nuclear and plasma membranes, respectively. The localization of the fluorescently labeled siRNA within the target cells was assessed by confocal microscopy. The arrows show the location of siRNA in lymphocytes. Flow cytometry analyses show the level of Alexa Fluor 488-tagged irrelevant siRNA in the target cells.
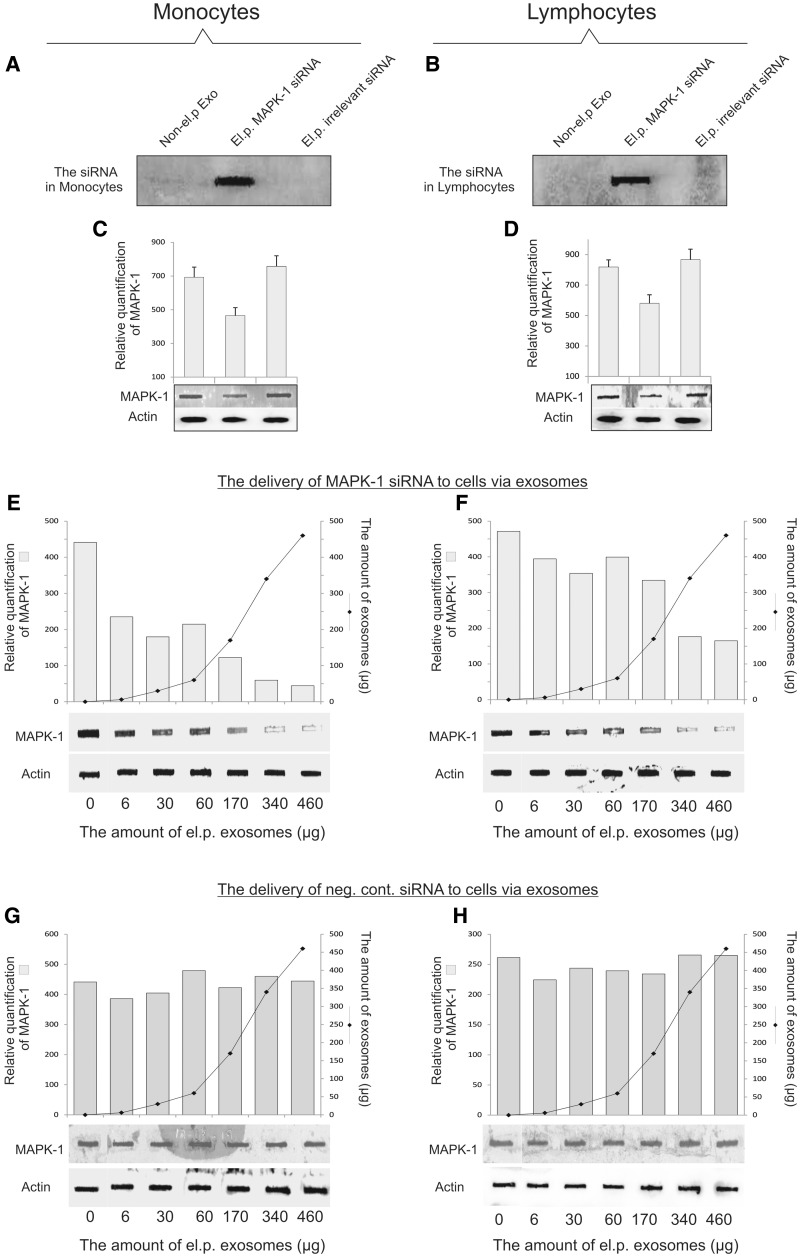
To examine whether the exosome-delivered siRNA was effective at causing post-transcriptional gene silencing in recipient cells, the gene product of MAPK1 was analyzed by immunoblotting. Thus, the siRNA against MAPK1 was transfected into plasma exosomes using the optimized electroporation settings (Table 1). Non-electroporated exosomes (exosomes + siRNA) and a non-targeting irrelevant siRNA were used as negative controls. The exosomes were then co-cultured with monocytes and lymphocytes isolated from the peripheral blood of healthy donors. The delivery of siRNA to the monocytes and lymphocytes by the exosomes was monitored using northern blotting (Figure 8A and B). To detect whether the siRNAs was inside the cells, total RNA from the recipient cells (monocytes and lymphocytes) was isolated, transferred to a nucleic acid membrane and hybridized with a digoxigenin-labeled probe against the complementary sequence of the administered MAPK1 siRNA. This process revealed the presence of MAPK1 siRNA only in monocytes and lymphocytes co-cultured with the electroporated exosomes, not in cells co-cultured with the negative control samples (Figure 8A and B). Subsequent measurements showed that the exosome-delivered siRNA caused selective gene silencing in recipient cells, based on the down-regulation of MAPK1 in recipient cells co-cultured with electroporated exosomes (Figure 8C and D). Furthermore, we investigated the kinetics of exosome-delivery of siRNA to monocytes and lymphocytes (Figure 8E–H). The results showed that high concentrations of electroporated exosomes could more effectively down-regulate the expression of MAPK-1 in both monocytes and lymphocytes (Figure 8E–H). However, the siRNA delivery to monocytes via exosomes was also feasible in lower concentrations (Figure 8E and G) but not in lymphocytes (Figure 8F and H). Using ‘LIVE/DEAD Fixable Violet Dead Cell Stain Kit’, the viability of monocytes and lymphocytes was determined after delivery of MAPK1 siRNA to the cells via exosomes. The experiments were performed twice and the results are reported as percentage of mean value (%) plus or minus standard deviation (mean ± SD), after 36 h (Table 2). The level of dead cells did not increase considerably after delivery of siRNA (siRNA against MAPK-1) to the recipient cells via exosomes.
Figure 8.
Delivery of heterologous siRNA to monocytes and lymphocytes via exosomes. Monocytes and lymphocytes from healthy donors were pulsed with exosomes electroporated with MAPK-1 siRNA. A non-targeting irrelevant siRNA was used as negative control in addition to non-electroporated exosomes (exosomes + the siRNA). The transfer of siRNA to the monocytes (A) and lymphocytes (B) was evaluated using a digoxigenin-labeled DNA-probe with a sequence complementary to the transferred MAPK-1 siRNA, two individual repeats. Post-transcriptional gene silencing of the MAPK-1 in monocytes (C) and lymphocytes (D) was evaluated using immunoblotting (slot blot) for the detection of the MAPK-1 protein. β-Actin was used as a constitutively produced protein and loading control, three individual repeats. A dose-response experiment was performed pulsing monocytes (E) and lymphocytes (F) with varying amounts of exosomes (0–460 µg) electroporated with MAPK-1 siRNA. As negative control, the same experiment was performed using a non-targeting irrelevant siRNA (G–H). Quantities of MAPK-1 were obtained by normalization of each assay to β-actin and using molecular densitometer (Bio-Rad GS-800).
Table 2.
Percentage of dead monocytes and lymphocytes (mean value ± SD) incubated with and without exosomes (electroporated exosomes, el.p. exo and non-electroporated exosomes, non-el.p. exo)
| Monocytes | Lymphocytes | |
|---|---|---|
| Untreated cells | 5.7 ± 0.35 | 4.2 ± 0.25 |
| Cells + el.p. exo | 10.3 ± 0.3 | 4.7 ± 0.5 |
| Cells + non-el.p. exo | 7.7 ± 0.07 | 4.2 ± 0.6 |
DISCUSSION
In this study, exogenous siRNAs were successfully introduced into various kinds of human exosomes and were used to deliver siRNA to human mononuclear blood cells. Plasma exosomes (exosomes from peripheral blood of healthy donors) effectively delivered the siRNA into the target cells, causing selective gene silencing of MAPK-1. Exosomes can practically be a non-immunogenic vector (they can be produced by the recipient’s own cells), which makes them an ideal candidate as vectors in gene therapy, to provide cells with heterologous nucleic acids such as therapeutic siRNAs.
We previously demonstrated that exosomes are capable of shuttling RNA between cells (15). Therefore, it was hypothesized that these vesicles might be used as GDVs to transfer heterologous nucleic acids to recipient cells. siRNA was chosen as the heterologous genetic material in this study, as these double-stranded siRNAs are small in size (21–23 nt) and lead to post-transcriptional gene silencing (26,27), which can be easily monitored experimentally. Likewise, exosomes naturally carry post-transcriptional regulator RNA (microRNA) between cells (17,18,21,22,28). To use the human exosomes as GDV, primarily the exogenous nucleic acids needed to be introduced into these vesicles. Two different strategies, electroporation and chemical transfection, were used for transferring exogenous siRNA into the human exosome. The results showed that chemical transfection of the exosomes to be used as GDV was inapplicable as the excess of micelles (siRNA embedded in lipid micelles) could not be separated from the exosomes. Therefore, it is uncertain whether the exosomes or the excess of micelles deliver the nucleic acid of interest to cells (Figure 2).
Next, electroporation was examined as a means of introducing genetic material into exosomes. This method is a physical process which depends on the field strength and time constant. Therefore, this experiment was carefully optimized with respect to voltage, capacitance, the range between electrodes in the cuvette and the concentrations of the siRNA and the exosomes. Having discovered the optimal parameters for transferring siRNA into exosomes (Table 1), siRNAs were packaged into exosomes derived from various cell types, as shown in Figures 3–5 and Supplementary Figures S1 and S2. Using immunoblotting and flow cytometry, exosomal marker proteins were detected in both electroporated and non-electroporated samples, as expected. The exogenous siRNA could only be detected in the electroporated exosome samples. Collectively, these results provide significant evidence that the heterologous siRNA was effectively introduced into exosomes using the electroporation parameters shown in Table 1. However, considering the multitude of electroporations performed during optimization of this method, it is important to note that the efficiency of transfections is varying although the settings are the same. We consider this kind of variation always present when using plasma from different donors. Furthermore, during optimization, we observed that other settings were effective yet we chose a lower voltage speculating it would be a milder treatment leaving the exosomes more intact. These observations indicate that further investigation is needed and that the method may need to be optimized for each exosome type.
Interestingly, exosomes from peripheral blood (plasma exosomes) were able to deliver heterologous siRNAs to human blood mononuclear cells. The exosome-delivered siRNA was localized in the cytoplasm of recipient cells, as determined by confocal microscopy and flow cytometry using a fluorescently labeled siRNA. Importantly, the exosome-delivered siRNA was functional and caused post-transcriptional gene silencing in recipient cells. The MAPK-1 protein was down-regulated in monocytes and lymphocytes that had been co-cultured with exosomes containing siRNA against the MAPK-1 transcript. The effect of exosome delivered MAPK-1 siRNA was increased in recipient cells with increasing amount of electroporated exosomes (Figure 8E and F). This might be because there are an excess/abundant amount of exosomes containing siRNA as gene knockdown using siRNA is transient in proliferating cells. The effect of gene knockdown was more visible in monocytes than in lymphocytes this may depend on varying ability of different cell types to absorb exosomes. This might be overcome by a second treatment with exosomes containing siRNA or by harvesting cells at different time points.
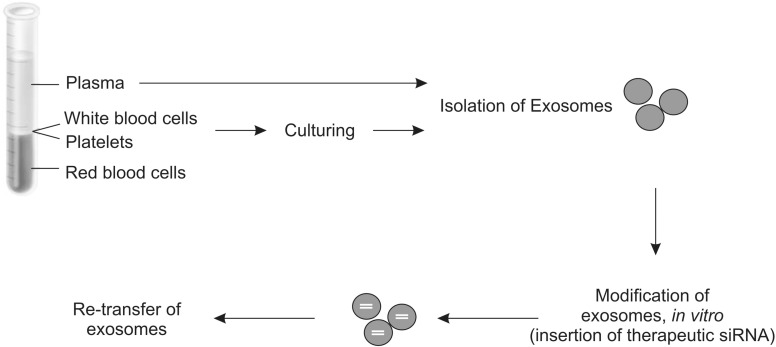
Gene therapy has the capacity to target the cause of genetic diseases rather than the symptoms. A safe and efficient vector is needed to introduce heterologous RNA/DNA molecules into target cells in vivo. Two types of vectors (viral and non-viral vectors) are already extensively used in gene therapy. An online search (December, 2010) of the National Institutes of Health database (http://clinicaltrials.gov/ct2/home), which provides access to information on clinical trials, shows that the majority of the 262 ongoing clinical trials in gene therapy utilize viral vectors. However, the current vectors have not proven successful in clinical trials because they are associated with issues such as toxicity, immunogenic concerns and targeting problems. It became more important to discover a safe vector after the death of an 18-year-old patient following treatment with an adenovirus vector to correct partial ornithine transcarbamylase (OTC) deficiency (29). The findings from this study and the study by Alvarez-Erviti et al. (25) suggest that exosomes can be used as a GDV. A strong advantage of using exosomes as carriers of genetic material to target cells such as malignant cells is that exosomes are nearly non-immunogenic, autologous exosomes given back to a patient should not provoke an immune response, especially given that the therapeutic nucleic acids neither can evoke an immunologic response in the body (Figure 9). Furthermore, exosomes may have evolved to carry different signals, including genetic material, to cells. Exosomes can easily be isolated from the patient’s body fluids or cell cultures and subsequently transferred back to the same patient after genetic modification (such as insertion or deletion of genetic material) in vitro (Figure 9). Many tumor cells also produce exosomes (30), which could presumably be used for delivering exogenous genetic material to cells. The ideal biological GDV should be able to evade immune recognition, achieve efficient cargo delivery and be cell- or tissue-specific. In 2004, the first RNAi-based drug candidate [Bevasiranib, an siRNA against vascular endothelial growth factor (VEGF)] was approved for human clinical trials (31). Since then, the list of diseases for which RNAi is being tested as a therapeutic agent has increased to include Parkinson’s disease, Lou Gehrig’s disease, HIV, wet age-related macular degeneration, type 2 diabetes, obesity, hypercholesterolemia, rheumatoid arthritis, respiratory diseases and cancers (31). However, despite the promise of RNAi, several technical obstacles must be overcome. The major hurdle of RNAi-based therapeutics is to deliver the nucleic acids across the cell’s plasma membrane (31,32). Therefore, the results of this study can be seen as ‘proof of concept’ to demonstrate the use of human exosomes as vectors in gene therapy, especially given that exosomes derived from human are nearly non-immunogenic, which makes them an ideal candidate for gene therapy, including RNAi-based therapeutics.
Figure 9.
Schematic representation of the use of exosomes as delivery vectors. Exosomes can easily be isolated from the patient’s body fluids or cell cultures, genetically modified in vitro (such as by insertion of heterologous therapeutic siRNA), and subsequently transferred back to the same patient.
SUPPLEMENTARY DATA
Supplementary Data are available at NAR Online: Supplementary Figures 1–3.
FUNDING
Funding for open access charge: The Swedish Research Council, the Swedish Heart and Lung foundation and Torsten och Ragnar Söderbergs foundations.
Conflict of interest statement. None declared.
Supplementary Material
ACKNOWLEDGEMENTS
We gratefully acknowledge Prof. Johan Bergenholz and Dr Moheb Nayeri at Chalmers technical university for the help with Zetsizer nano. We also thank Prof. Thomas Nyström and Dr. Anne Farwell for providing laboratory resources for some of the experiments at the Cell and Molecular Biology Laboratory at University of Gothenburg. We would like to express our gratitude to Mehdi Azadi for helping us with the confocal microscopy and Dr. Åsa Valadi for editing the manuscript. We also acknowledge Inga-Britt and Arne Lundbergs forskningsstiftelse for the use of Beckman Optima LE80K and the FACSCantoII (Becton Dickinson).
REFERENCES
- 1.Thery C, Regnault A, Garin J, Wolfers J, Zitvogel L, Ricciardi-Castagnoli P, Raposo G, Amigorena S. Molecular characterization of dendritic cell-derived exosomes: selective accumulation of the heat shock protein hsc73. J. Cell Biol. 1999;147:599–610. doi: 10.1083/jcb.147.3.599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Raposo G, Nijman H, Stoorvogel W, Liejendekker R, Harding C, Melief C, Geuze H. B lymphocytes secrete antigen-presenting vesicles. J. Exp. Med. 1996;183:1161–1172. doi: 10.1084/jem.183.3.1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Blanchard N, Lankar D, Faure F, Regnault A, Dumont C, Raposo G, Hivroz C. TCR activation of human T cells induces the production of exosomes bearing the TCR/CD3/[zeta] complex. J. Immunol. 2002;168:3235–3241. doi: 10.4049/jimmunol.168.7.3235. [DOI] [PubMed] [Google Scholar]
- 4.Skokos D, Le Panse S, Villa I, Rousselle J-C, Peronet R, David B, Namane A, Mecheri S. Mast cell-dependent B and T lymphocyte activation is mediated by the secretion of immunologically active exosomes. J. Immunol. 2001;166:868–876. doi: 10.4049/jimmunol.166.2.868. [DOI] [PubMed] [Google Scholar]
- 5.Karlsson M, Lundin S, Dahlgren U, Kahu H, Petterson I, Telemo E. “Tolerosomes” are produced by intestinal epithelial cells. Eur. J. Immunol. 2001;31:2892–2900. doi: 10.1002/1521-4141(2001010)31:10<2892::aid-immu2892>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 6.Mears R, Craven RA, Hanrahan S, Totty N, Upton C, Young SL, Patel P, Selby PJ, Banks RE. Proteomic analysis of melanoma-derived exosomes by two-dimensional polyacrylamide gel electrophoresis and mass spectrometry. Proteomics. 2004;4:4019–4031. doi: 10.1002/pmic.200400876. [DOI] [PubMed] [Google Scholar]
- 7.Van Niel G, Porto-Carreiro I, Simoes S, Raposo G. Exosomes: a common pathway for a specialized function. J. Biochem. (Tokyo) 2006;140:13–21. doi: 10.1093/jb/mvj128. [DOI] [PubMed] [Google Scholar]
- 8.Caby M-P, Lankar D, Vincendeau-Scherrer C, Raposo G, Bonnerot C. Exosomal-like vesicles are present in human blood plasma. Int. Immunol. 2005;17:879–887. doi: 10.1093/intimm/dxh267. [DOI] [PubMed] [Google Scholar]
- 9.Lasser C, Seyed Alikhani V, Ekstrom K, Eldh M, Torregrosa Paredes P, Bossios A, Sjostrand M, Gabrielsson S, Lotvall J, et al. Human saliva, plasma and breast milk exosomes contain RNA: uptake by macrophages. J. Transl. Med. 2011;9:9. doi: 10.1186/1479-5876-9-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pisitkun T, Shen R-F, Knepper MA. Identification and proteomic profiling of exosomes in human urine. Proc. Natl Acad. Sci. USA. 2004;101:13368–13373. doi: 10.1073/pnas.0403453101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Andre F, Schartz NEC, Movassagh M, Flament C, Pautier P, Morice P, Pomel C, Lhomme C, Escudier B, Le Chevalier T. Malignant effusions and immunogenic tumour-derived exosomes. Lancet. 2002;360:295–305. doi: 10.1016/S0140-6736(02)09552-1. [DOI] [PubMed] [Google Scholar]
- 12.Admyre C, Grunewald J, Thyberg J, Gripenback S, Tornling G, Eklund A, Scheynius A, Gabrielsson S. Exosomes with major histocompatibility complex class II and co-stimulatory molecules are present in human BAL fluid. Eur. Respir. J. 2003;22:578–583. doi: 10.1183/09031936.03.00041703. [DOI] [PubMed] [Google Scholar]
- 13.Sprent J. Direct stimulation of naive T cells by antigen-presenting cell vesicles. Blood Cells Mol.Dis. 2005;35:17–20. doi: 10.1016/j.bcmd.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 14.Eldh M, Ekstrom K, Valadi H, Sjostrand M, Olsson B, Jernas M, Lotvall J. Exosomes communicate protective messages during oxidative stress; possible role of exosomal shuttle RNA. PLoS One. 2010;5:e15353. doi: 10.1371/journal.pone.0015353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Valadi H, Ekstrom K, Bossios A, Sjostrand M, Lee JJ, Lotvall JO. Exosome-mediated transfer of mRNAs and microRNAs is a novel mechanism of genetic exchange between cells. Nat. Cell Biol. 2007;9:654–659. doi: 10.1038/ncb1596. [DOI] [PubMed] [Google Scholar]
- 16.Gibbings DJ, Ciaudo C, Erhardt M, Voinnet O. Multivesicular bodies associate with components of miRNA effector complexes and modulate miRNA activity. Nat. Cell Biol. 2009;11:1143–1149. doi: 10.1038/ncb1929. [DOI] [PubMed] [Google Scholar]
- 17.Kesimer M, Scull M, Brighton B, DeMaria G, Burns K, O'Neal W, Pickles RJ, Sheehan JK. Characterization of exosome-like vesicles released from human tracheobronchial ciliated epithelium: a possible role in innate defense. FASEB J. 2009;23:1858–1868. doi: 10.1096/fj.08-119131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Luo SS, Ishibashi O, Ishikawa G, Ishikawa T, Katayama A, Mishima T, Takizawa T, Shigihara T, Goto T, Izumi A, et al. Human villous trophoblasts express and secrete placenta-specific microRNAs into maternal circulation via exosomes. Biol. Reprod. 2009;81:717–729. doi: 10.1095/biolreprod.108.075481. [DOI] [PubMed] [Google Scholar]
- 19.Michael A, Bajracharya SD, Yuen PS, Zhou H, Star RA, Illei GG, Alevizos I. Exosomes from human saliva as a source of microRNA biomarkers. Oral Dis. 2009;16:34–38. doi: 10.1111/j.1601-0825.2009.01604.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Miranda KC, Bond DT, McKee M, Skog J, Paunescu TG, Da Silva N, Brown D, Russo LM. Nucleic acids within urinary exosomes/microvesicles are potential biomarkers for renal disease. Kidney Int. 2010;78:191–199. doi: 10.1038/ki.2010.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Palanisamy V, Sharma S, Deshpande A, Zhou H, Gimzewski J, Wong DT. Nanostructural and transcriptomic analyses of human saliva derived exosomes. PLoS One. 2010;5:e8577. doi: 10.1371/journal.pone.0008577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Skog J, Wurdinger T, van Rijn S, Meijer DH, Gainche L, Sena-Esteves M, Curry WT, Jr, Carter BS, Krichevsky AM, Breakefield XO. Glioblastoma microvesicles transport RNA and proteins that promote tumour growth and provide diagnostic biomarkers. Nat. Cell Biol. 2008;10:1470–1476. doi: 10.1038/ncb1800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Taylor DD, Gercel-Taylor C. MicroRNA signatures of tumor-derived exosomes as diagnostic biomarkers of ovarian cancer. Gynecol. Oncol. 2008;110:13–21. doi: 10.1016/j.ygyno.2008.04.033. [DOI] [PubMed] [Google Scholar]
- 24.Seow Y, Wood MJ. Biological gene delivery vehicles: beyond viral vectors. Mol. Ther. 2009;17:767–777. doi: 10.1038/mt.2009.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Alvarez-Erviti L, Seow Y, Yin H, Betts C, Lakhal S, Wood MJ. Delivery of siRNA to the mouse brain by systemic injection of targeted exosomes. Nat. Biotechnol. 2011;29:341–345. doi: 10.1038/nbt.1807. [DOI] [PubMed] [Google Scholar]
- 26.Elbashir SM, Harborth J, Lendeckel W, Yalcin A, Weber K, Tuschl T. Duplexes of 21-nucleotide RNAs mediate RNA interference in cultured mammalian cells. Nature. 2001;411:494–498. doi: 10.1038/35078107. [DOI] [PubMed] [Google Scholar]
- 27.Elbashir SM, Lendeckel W, Tuschl T. RNA interference is mediated by 21- and 22-nucleotide RNAs. Genes Dev. 2001;15:188–200. doi: 10.1101/gad.862301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nilsson J, Skog J, Nordstrand A, Baranov V, Mincheva-Nilsson L, Breakefield XO, Widmark A. Prostate cancer-derived urine exosomes: a novel approach to biomarkers for prostate cancer. Br. J. Cancer. 2009;100:1603–1607. doi: 10.1038/sj.bjc.6605058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lehrman S. Virus treatment questioned after gene therapy death. Nature. 1999;401:517–518. doi: 10.1038/43977. [DOI] [PubMed] [Google Scholar]
- 30.Koga K, Matsumoto K, Akiyoshi T, Kubo M, Yamanaka N, Tasaki A, Nakashima H, Nakamura M, Kuroki S, Tanaka M, et al. Purification, characterization and biological significance of tumor-derived exosomes. Anticancer Res. 2005;25:3703–3707. [PubMed] [Google Scholar]
- 31.Castanotto D, Rossi JJ. The promises and pitfalls of RNA-interference-based therapeutics. Nature. 2009;457:426–433. doi: 10.1038/nature07758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tiemann K, Rossi JJ. RNAi-based therapeutics-current status, challenges and prospects. EMBO Mol. Med. 2009;1:142–151. doi: 10.1002/emmm.200900023. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.