Abstract
Study Objectives:
There is a paucity of information on the epidemiology of sleep disorders among US Hispanics. This study describes the frequency of sleep disordered breathing (SDB) risk, insomnia complaints, poor sleep quality, and daytime somnolence in a clinical cohort of ethnically diverse US Hispanics living in South Florida.
Methods:
We explored the presence of sleep disorders in a cohort of Hispanics seen at primary care, pulmonary, and sleep clinics at the University of Miami and Miami Veterans Affair Medical Center. Participants completed validated questionnaires, evaluating risk of SDB, presence of insomnia symptoms, sleep quality, and daytime sleepiness. Polysomnography was completed on the majority of the sleep clinic participants.
Results:
Participants (N = 282; 62% male; mean age 54 ± 15 years; mean BMI 31 ± 6 kg/m2) included Hispanics of Cuban, Puerto Rican, Central/South American, and Caribbean heritage. Excessive daytime sleepiness was noted by 45% of participants. Poor sleep quality was reported by 49%; 76% screened high risk for SDB, and 68% had insomnia symptoms. Sleep disorders were more commonly reported in sleep clinic participants; however, 54% of non-sleep clinic participants were high risk for SDB, 35% had insomnia complaints, 28% had poor sleep quality, and 18% reported daytime sleepiness.
Conclusions:
Sleep disorders (including SDB) are common in clinical samples of Hispanics in South Florida. These findings highlight the urgent need for linguistically relevant and culturally responsive screening, awareness and education programs in clinical sleep medicine among US Hispanics.
Citation:
Shafazand S; Wallace DM; Vargas SS; Del Toro Y; Dib S; Abreu AR; Ramos A; Nolan B; Baldwin CM; Fleming L. Sleep disordered breathing, insomnia symptoms, and sleep quality in a clinical cohort of US Hispanics in South Florida. J Clin Sleep Med 2012;8(5):507-514.
Keywords: Sleep disordered breathing, insomnia, sleep quality, excessive daytime somnolence, Hispanic, ethnicity, epidemiology
Hispanics in the United States (US) are a diverse population originating from Mexico, Puerto Rico, Cuba, and countries in Central, South America, and the Caribbean. Several studies have documented increased rates of disorders traditionally associated with sleep disordered breathing (SDB), including diabetes,1,2 obesity,3,4 and cardiovascular disease5,6 among US Hispanics. Acculturation to the American diet and lifestyle, in addition to lower socioeconomic status, decreased access to health care, and increased stress associated with migration may all contribute to the increased prevalence of these disorders.3,7–9 Similar to other ethnic groups, cardiovascular disease is the leading cause of death in US Hispanics.10
A significant body of literature points to the roles that sleep quality (SQ) and sleep duration play in normal metabolism, immune function, mood, and cognitive functioning.11–14 In particular, SDB has been associated with an increased risk of stroke, hypertension, atrial fibrillation, myocardial infarction, worsening diabetes, and all-cause mortality.15–19 Given the relationship between sleep disorders and cardiovascular disease, sleep health is likely to play a significant role in the overall health and healthcare utilization of US Hispanics.15,20,21 As the largest and fastest growing minority population in the US, Hispanics will continue to have considerable social, economic, and political impact, with unique healthcare requirements that need to be recognized and addressed. Despite significant research in recent years on the prevalence and health impact of sleep disorders, there is a relative paucity of data on sleep disorders among ethnically diverse US Hispanics. This study describes the frequency of SDB risk, insomnia complaints, poor sleep quality, and daytime somnolence in a clinical cohort of ethnically diverse US Hispanics living in South Florida. We hypothesized that Hispanic participants recruited from sleep clinics would have higher prevalence of sleep complaints than those participants from non-sleep clinics.
BRIEF SUMMARY
Current Knowledge/Study Rationale: Despite significant research in recent years on the prevalence and health impact of sleep disorders, there is a relative paucity of data on sleep disorders among ethnically diverse US Hispanics. This study describes the frequency of sleep apnea risk, insomnia complaints, poor sleep quality, and daytime somnolence in a clinical cohort of ethnically diverse US Hispanics living in South Florida.
Study Impact: Our study increases the awareness that risks for sleep apnea, insomnia symptoms, poor sleep quality, and excessive daytime sleepiness are common in a clinical cohort of US Hispanics and highlights the need for increased screening and awareness by healthcare providers.
METHODS
Subjects
We enrolled consecutive adult (age ≥ 18 years), self-identified Hispanic patients referred to the University of Miami (UM) sleep, primary care (general internal medicine), and pulmonary clinics, and the Miami Veterans Affairs (VA) Medical Center sleep clinics from September 2009 to November 2010. Participants were excluded if they were unable to read English or Spanish at a fifth-grade level. Participants in the general internal medicine or pulmonary clinics had chief complaints unrelated to a primary sleep disorder. The reasons for primary care visits ranged from routine well visits to the renewal of prescription medications, monitoring chronic health conditions (diabetes, hypertension), and new patient visits. The pulmonary clinic participants were seen for follow-up of common respiratory conditions including cough, dyspnea, asthma, and emphysema. The University of Miami and the Miami VA Administrative Panel on Human Subjects in Medical Research approved the protocol, and all participants signed a written informed consent prior to enrollment.
Study Variables
Demographic characteristics and medical history were obtained from patient interview and a review of medical records. Depression and anxiety were determined by the following single question asked at the time of enrollment, “Have you ever been told by a doctor that you have depression or anxiety?” Anthropometric measures (height, weight, and neck circumference) were obtained on the day of enrollment. All participants completed validated questionnaires (available in both English and Spanish) to determine risk for SDB, insomnia symptom severity, sleep quality (SQ), and daytime somnolence. We screened for increased risk of sleep apnea using the STOP BANG questionnaire.22 A recently validated measure to determine SDB risk, the STOP BANG compares favorably to the Berlin sleep index.23,24 The validated insomnia severity index (ISI)25 was used to measure insomnia symptomatology.25,26 Sleep quality was evaluated using the Pittsburgh Sleep Quality Index (PSQI).27–29 A global PSQI score > 5 yields a diagnostic sensitivity of 89.6% and specificity of 86.5% in distinguishing good from poor sleepers.28 We evaluated subjective daytime sleepiness using the Epworth Sleepiness Scale (ESS).30–32 The internal consistency, concurrent validity, and sensitivity to clinical improvements of these questionnaires are well established.
Polysomnography
Both sleep and non-sleep clinic participants were encouraged to undergo in-laboratory video polysomnography (PSG), with most of the participants recruited from the sleep clinics agreeing to do so. We conducted PSG in accordance with the standards established by the American Academy of Sleep Medicine. Records were scored using standardized techniques and the recommended scoring rules for hypopneas.33 The oro-nasal thermistor and nasal pressure transducer channels were used to score apneas and hypopneas, respectively. An apnea-hypopnea index ([AHI], number of apneas and hypopneas/h of sleep) ≥ 5 was used to diagnose SDB.
Data Analysis
We report means and standard deviations (SD), medians and interquartile ranges (IQR) and frequencies. Participants were divided into 2 groups (sleep clinic, and non-sleep clinic participants); differences in study variables were compared using the χ2 test statistic, Fisher exact test, Student t-test, or Mann Whitney U tests. Given the small number of participants recruited from pulmonary clinics (n = 22), we have provided summary statistics for the general medicine and pulmonary clinic subgroups (non-sleep clinic group), but we did not perform comparisons between subgroups. High risk for SDB was calculated as the proportion of individuals with a STOP BANG score ≥ 3. The presence of insomnia symptoms was calculated as the proportion of individuals with ISI score ≥ 8. The frequency of poor SQ was calculated as the proportion of individuals with a PSQI ≥ 5. Excessive daytime sleepiness (EDS) was defined as proportion of participants with ESS ≥ 10. We used multivariable modeling to adjust results for gender, age, body mass index (BMI), presence of diabetes, anxiety, and depression. We accepted a 2-tailed p-value < 0.05 as statistically significant for all analyses. We analyzed data using SPSS for Windows, version 17.0 statistical software package (SPSS; Chicago, IL).
RESULTS
Characteristics of Study Participants
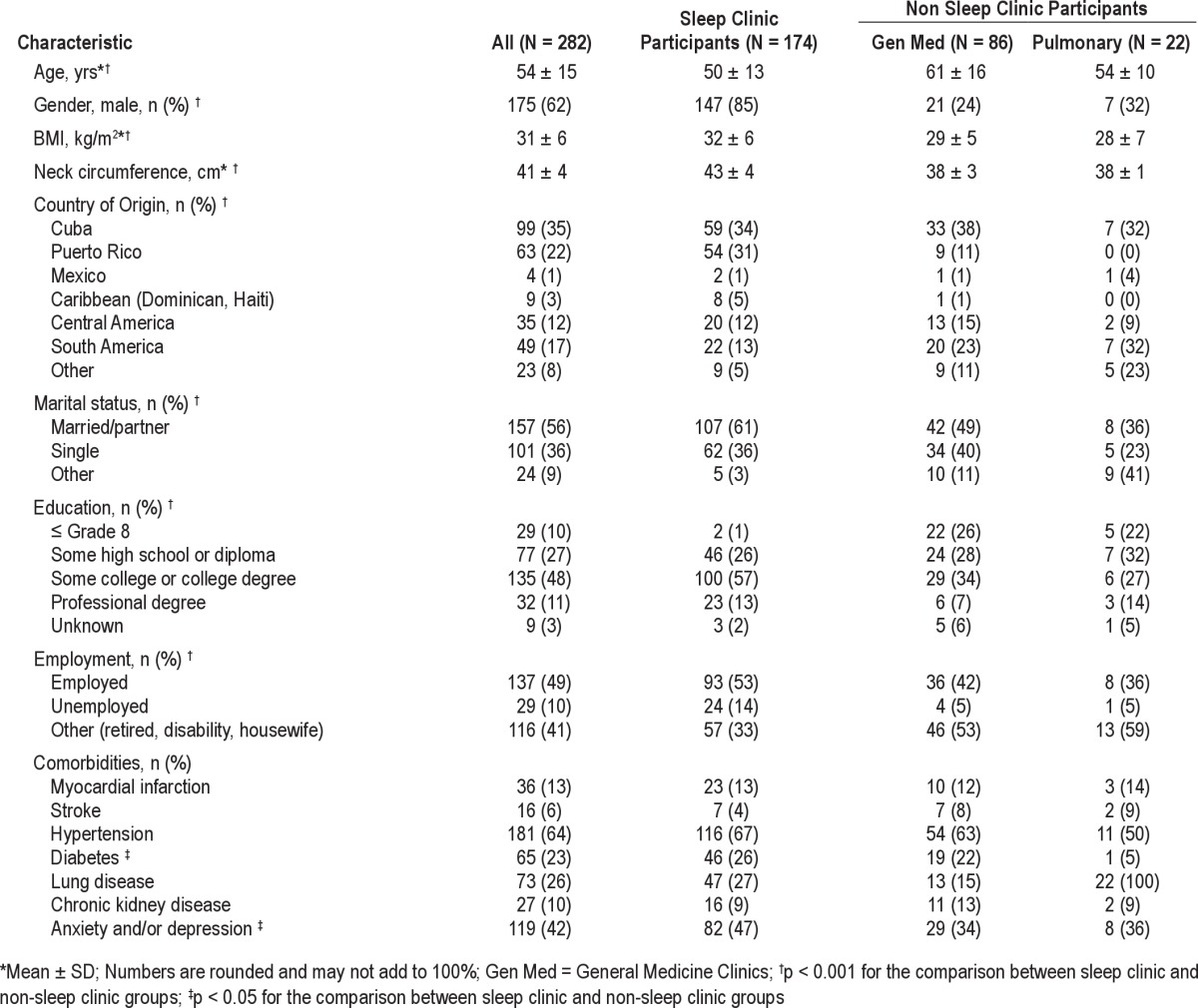
We enrolled 282 participants (174 sleep clinic,108 non-sleep clinic), 62% male with a mean age of 54 ± 15 years and mean BMI 31 ± 6 kg/m2 (Table 1). At the UM enrollment sites, Spanish was the preferred language for communication and completion of study questionnaires for 77% of participants, with 44% expressing discomfort with speaking English in day-to-day life. Cuban Americans, the largest Hispanic group in this study, constituted 35% of participants, with Puerto Ricans being the next largest group at 22%. There was a statistically significant difference in age and BMI between sleep clinic and non-sleep clinic subgroups, with the sleep clinic subjects being younger and heavier. Sleep clinic participants were more likely to be male, diabetic, and to suffer from anxiety or depression, with no other differences in comorbidities noted (Table 1).
Table 1.
Characteristics of the Study Population
Risk of Sleep Disordered Breathing and its Prevalence on Polysomnography
An increased risk of SDB using the STOP BANG measure was noted in 76% of all participants. Sleep clinic subjects were more likely to be at high risk for SDB (90% vs. 54%, p < 0.001). Baseline PSG was available for 56% of all participants; 81% of participants completing PSG had objective SDB with median AHI of 20.2 (IQR 136.7), 63% of whom had moderate to severe disease (AHI ≥ 15). Sleep apnea syndrome (SAS), defined as AHI ≥ 5 and sleepiness (ESS ≥ 10) was found in 83% of the sleep clinic population.
Insomnia Symptomatology and Severity
Symptoms suggestive of clinical insomnia (ISI ≥ 8) were reported in 68% of the group as a whole, with a significantly higher frequency in the sleep clinic participants (87% vs. 35%, p < 0.001). The mean ISI for all participants was 11.6 ± 7.8 (Table 2), indicating mild clinical insomnia in this population. There were significant group differences seen in the ISI scores with the non-sleep clinic participants reporting lower ISI scores (6.2 ± 6.4 vs.14.9 ± 6.6, p < 0.001). This difference remained significant after adjustment for age, gender, BMI, presence of diabetes, and mood disorders. The results for insomnia symptoms and severity are provided in Table 2.
Table 2.
Sleep Questionnaires
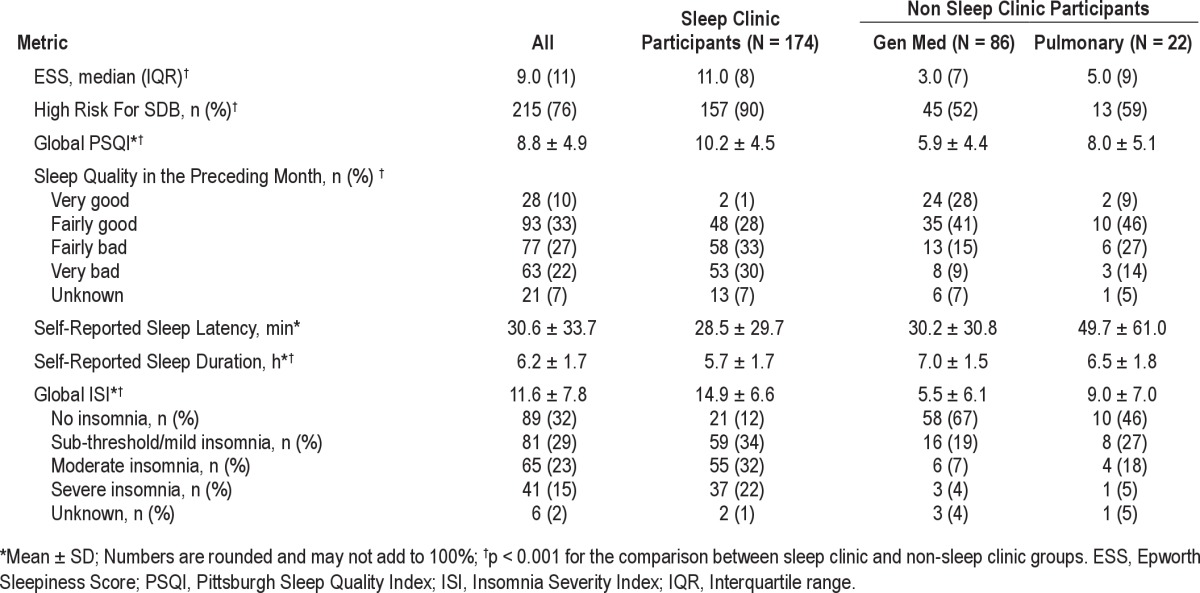
Sleep Quality and Excessive Daytime Sleepiness
The mean PSQI for all participants was 8.8 ± 4.9, indicating poor SQ; however, the non-sleep clinic group had significantly better SQ than sleep clinic subjects (6.3 ± 4.6 vs. 10.2 ± 4.5, p < 0.001) (Table 2). These comparisons remained significant between groups after adjustment for age, gender, BMI, presence of diabetes, anxiety, and depression.
When queried about sleep during the previous month, 56% of all subjects reported having nighttime arousals and 46% reported loud snoring or coughing during sleep ≥ 3 times a week. A quarter of the participants required medication (prescription or over-the-counter) ≥ 3 times a week to help initiate and/or maintain sleep. Only 10% of participants ranked their overall SQ as very good, while 49% reported fairly to very bad SQ in the previous month. Sleep clinic subjects were significantly more likely to report nighttime arousals (73% vs. 39%, p < 0.001) and loud snoring or cough (57% vs. 26%, p < 0.001) ≥ 3 times a week. Only 1% of the sleep clinic participants and 25% of the non-sleep clinic participants reported very good SQ in the preceding month. Overall, participants reported a mean 6 ± 2 h sleep per night, with a self-reported sleep onset latency of 31 ± 34 minutes. There was a significant difference in sleep duration between groups, with sleep clinic participants reporting shorter mean sleep duration.
EDS was reported by 45% of all participants. Among sleep clinic patients, the rate was 62%, while 18% of the non-sleep clinic participants reported EDS. The median Epworth score for the entire study population was 9 (IQR = 11), with a statistically significant difference noted between groups that remained significant after adjustment for age, gender, BMI, presence of diabetes, anxiety, and depression. The results for EDS are displayed in Table 2.
DISCUSSION
According to 2010 US census data, there are over 50 million Hispanics in the United States (16% of the US population) comprising the largest single minority group,34 yet little is known about the sleep disturbances experienced by this growing segment of our population. Our findings indicate that subjectively reported SDB, insomnia symptoms, poor sleep quality, and daytime somnolence are common among an ethnically diverse sample of Hispanics living in South Florida who were seen in clinical settings. The presence and range of sleep disorders among our Hispanic sleep clinic patients suggest the potential for poorer health outcomes and higher health care costs relevant to sleep-associated comorbidities. We have reviewed the limited existing general population studies on sleep disorders in Hispanics and in mixed population primary care settings. Direct comparisons between studies are difficult due to the variability in measurement tools and population comorbidities. We present these data to provide a framework for the state of the knowledge to date. Table 3 summarizes the main sleep related findings in our clinical sample and places them in the context of reports from the literature as discussed below.
Table 3.
Reported Prevalence of Sleep Disorders in Hispanics
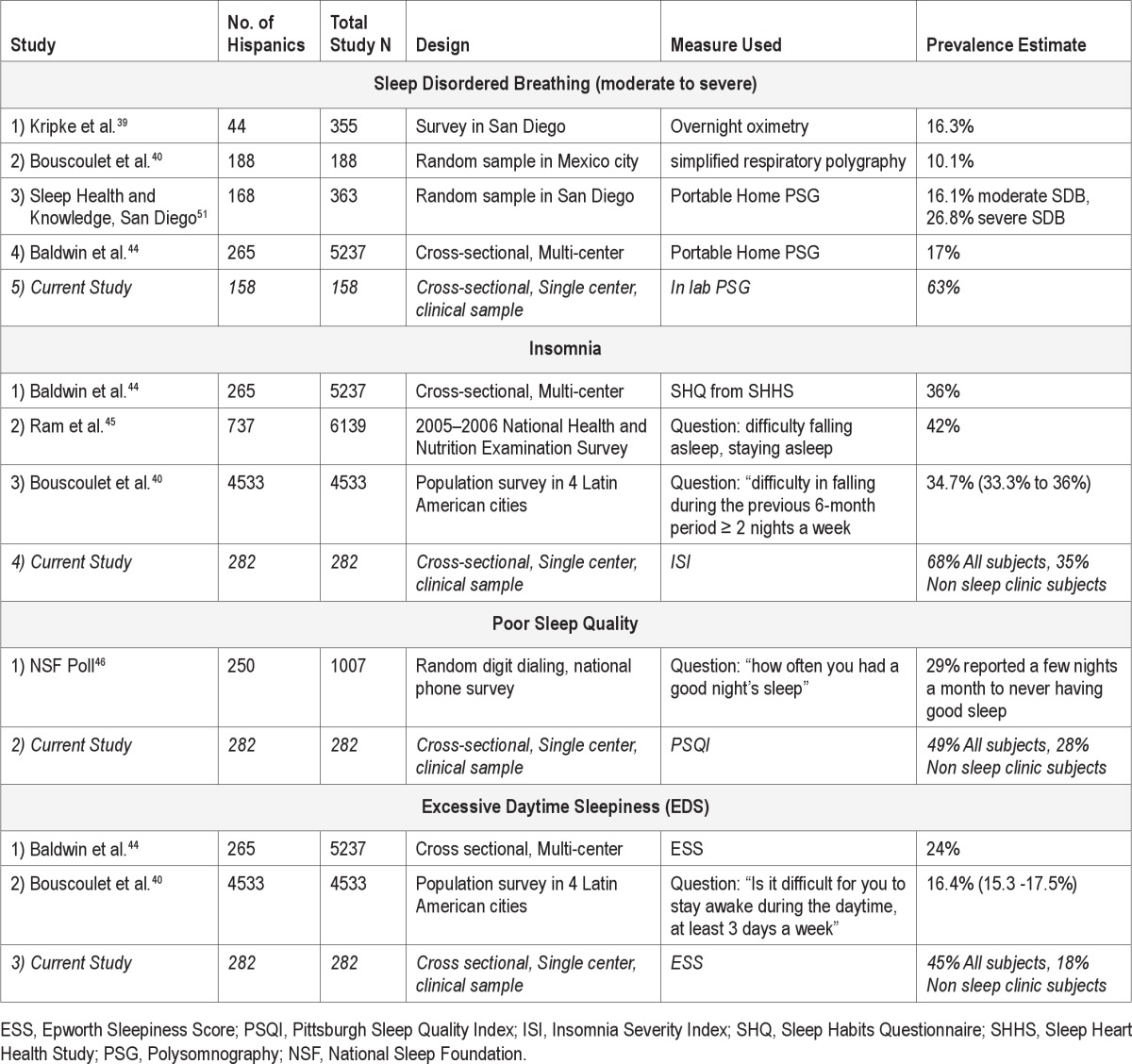
Sleep Disordered Breathing
Snoring is a focal sign of obstructive sleep apnea. Self-reported snoring rates in our study were 55% in the entire cohort, with 43% of women and 62% of men reporting loud snoring. These numbers are higher than previous reports and may reflect our recruitment strategy.35,36 One- third of the participants recruited from our non-sleep clinics reported loud snoring, including 37% of women and 22% of men, suggesting that snoring is prevalent in our Hispanic clinical group with no specific sleep complaints. Notably, elevated rates of snoring alone among Hispanic children and adults have been reported elsewhere.7,35,36 Reasons for this increased rate among Hispanics are not known. Further studies are needed given this consistent finding to determine if culture, lifestyle, physiognomy or other factors play a role.
Over two-thirds of our participants were found to be at high risk for SDB using the STOP BANG measure, including over half of the non-sleep clinic patients. Studies in multi-ethnic office based settings suggest that the prevalence of SDB in patients seen in primary care clinics is higher than general population estimates.37,38 This may be due to the increased frequency of diabetes and obesity in these settings. Netzer et al. surveyed 40 primary care offices and clinics in United States (n = 3915) and Europe (Germany and Spain [n = 2308]) using the Berlin questionnaire to determine SDB risk. The risk for SDB was higher in US (35.8%) than European primary care populations (26.3%). The SDB risk prevalence in two Florida primary care settings included in this survey ranged from 36.4% to 43.5%.37 In their study of a family practice clinic in Cleveland Ohio, Senthilvel et al. surveyed 101 patients (11% Hispanic) using several standardized sleep questionnaires, including Berlin and STOP questionnaires.38 High risk for SDB was found in 33% (Berlin) and 34% (STOP) of participants.
Comparisons between different studies are difficult due to the variability in measurement tools, ethnic diversity of the population studied, and differing comorbidities that increase the risk for sleep apnea. However, the high frequencies of snoring and overall risk of SDB in the non-sleep clinic group in our study suggest the need for an increased awareness of SDB in this population and for routine screening during patient encounters using appropriately Spanish translated measures at relevant reading and comprehension levels.
The actual prevalence of objectively diagnosed SDB in Hispanics is not well known. Kripke performed home sleep oximetry in 355 subjects, including 44 Hispanics, and estimated that 16.3% of Hispanics and other racial minorities had ≥ 20 desaturation events per hour (comparable to moderate to severe SDB), compared to 4.9% of non-Hispanic whites.39 Bouscoulet et al.40 performed home portable respiratory monitoring during sleep in 188 subjects from Mexico City and found the prevalence of moderate sleep apnea was as high as 23.5%. We report much higher estimates in our cohort of sleep clinic patients. This may be due to our use of PSG as the gold standard of SDB diagnosis, selection bias noted in sleep clinics, or may reflect a true increase in risk. Preliminary data from two ongoing population- and community-based NIH sponsored studies20,41,42 suggest that the numbers for SDB among Hispanics is higher than the general population estimates often quoted for non-Hispanic whites,43 highlighting the trend for higher rates of SDB among Hispanics that mirrors our findings.
Insomnia Symptoms
Very little is known about the prevalence of insomnia symptoms among US Hispanics. Overall, our study participants had significant (moderate to severe) insomnia complaints (38%), in keeping with the SHHS estimates for Hispanics who were primarily of Mexican heritage.44 Self-reported insomnia symptoms were particularly high among our patients with objective findings of SDB. The NHANES data suggest that 13.4% of Hispanic respondents had trouble falling asleep, 13.7% would wake up during the night with difficulty returning to sleep, and 14.7% would wake up early in the morning.45 More than a third (33%) of our general medicine subgroup reported insomnia symptoms. This is comparable to Senthilvel's multi-ethnic primary care office-based study, in which 32% of participants had symptoms suggestive of insomnia. 38
Sleep Duration and Quality
The data on sleep duration in Hispanics are variable and may reflect the impact of factors other than ethnicity on sleep duration. In the National Sleep Foundation (NSF) 2010 survey,46 Hispanics reported an average of 6 hours and 34 minutes of sleep during workdays. They slept longer than African Americans but less than Asians and non-Hispanic whites. In the1990 National Health Interview Survey,47 non-Mexican Hispanics had an increased risk for short sleep duration compared to non-Hispanic whites. The 2005-2006 National Health and Nutrition Examination Survey (NHANES) of 6139 individuals (12% Hispanic), however, reported that Hispanics (6.9 h) and Whites (7.0 h) had longer mean sleep duration than Blacks (6.5 h).45 Our data demonstrate shorter sleep duration among participants with sleep complaints seen in sleep clinics, but is consistent with the NHANES data for those individuals seen in non-sleep clinics.
Restricted or impaired sleep has a significant economic burden with conservative estimates at $107 billion.48 In our study participants reported poor SQ and even among persons without a specific sleep complaint or diagnosis, only 25% reported very good SQ. In 2010, the National Sleep Foundation (NSF) conducted a phone survey of Americans (25% Hispanic) to determine their sleep habits and knowledge.46 Nearly 40% of respondents, including 38% Hispanic, said they get a good night's sleep every night or almost every night. Rarely or never having a good night's sleep was reported by 14% of Hispanics. Although this survey is not directly comparable to our results, it corroborates our findings that many Hispanics are not satisfied with some aspect of their SQ, and very good sleep is experienced at best by less than half of those surveyed regardless of the method of evaluation.
Excessive Daytime Sleepiness
Nearly half of our study participants reported significant daytime sleepiness, a known risk factor for vehicular crashes and impaired work performance.49,50 In the multicenter, population based SHHS, 23% of Hispanic participants had EDS.44 Bouscoulet et al.40 determined EDS prevalence to be 16.4% (95% CI 15.3-17.5) among adults ≥ 40 years old, living in 4 large Latin American cities, using a single question “Is it difficult for you to stay awake during the daytime at least 3 days a week?” Our non-sleep clinic participants were seen in clinic for routine primary care or pulmonary follow-ups; the 18% EDS noted in this group is within the range of previous estimates (Table 3) and highlights a need to address this sleep complaint in Hispanics in primary care and pulmonary clinics. The impact of EDS on overall health, social, and economic domains among Hispanics has yet to be determined.
Limitations
Our study has several limitations. We are unable to make direct comparisons to other ethnic groups (non-Hispanic whites, African Americans, and Asians), as we studied Hispanic patients only. Our study cannot provide true population prevalence estimates, as we did not use randomized sampling techniques, but instead relied on a convenience sample of patients in sleep and non-sleep clinics. However, our non-sleep clinic group had no sleep disorders diagnosed at the time of enrollment and were not actively seeking help for sleep complaints. We provide data for the pulmonary and general medicine subgroups in Tables 1 and 2. However, due to the small sample size in pulmonary clinics, we refrained from subgroup analyses. Finally, SDB diagnosis was based on PSG only in the sleep clinic subjects. PSG was offered to all participants; however, the non-sleep clinic and some of the sleep clinic subjects declined testing due to lack of daytime symptoms, a belief that they did not have sleep apnea, lack of desire to use positive airway pressure therapy should the baseline test prove to be positive, or lack of insurance coverage.
Summary
Despite these limitations, our study reports the frequency of several sleep disorders in a diverse group of US Hispanics seen in clinical settings and highlights the need for increased awareness and screening by healthcare providers. Sleep and its associated disorders play an important role in health, wellness, disease, and quality of life. Hispanics are a rapidly growing segment of US society with ever growing healthcare needs. Social, socioeconomic, sociopolitical, lifestyle, cultural, or physiological characteristics may predispose Hispanic patients to an increased prevalence of sleep disorders, including sleep apnea, snoring, and poor sleep quality. Language and cultural barriers may widen health disparities. Our study increases the awareness that risk for SDB, insomnia symptoms, poor sleep quality, and excessive daytime sleepiness are common in a clinical cohort of US Hispanics living in South Florida and highlights the need for further research and education in this area.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
All authors had access to the data and contributed substantially to the design, acquisition, and analysis of data, and writing of manuscript. The work was completed at University of Miami and Miami VA Health Care System. Dr. Shafazand was supported by a grant from the American Sleep Medicine Foundation. Dr. Fleming was supported in part by the European Union ERDF Funding to the ECEHH (University of Exeter).
REFERENCES
- 1.Black SA, Ray LA, Markides KS. The prevalence and health burden of self-reported diabetes in older Mexican Americans: findings from the Hispanic established populations for epidemiologic studies of the elderly. Am J Public Health. 1999;89:546–52. doi: 10.2105/ajph.89.4.546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Flegal KM, Ezzati TM, Harris MI, et al. Prevalence of diabetes in Mexican Americans, Cubans, and Puerto Ricans from the Hispanic Health and Nutrition Examination Survey, 1982-1984. Diabetes Care. 1991;14:628–38. doi: 10.2337/diacare.14.7.628. [DOI] [PubMed] [Google Scholar]
- 3.Khan LK, Sobal J, Martorell R. Acculturation, socioeconomic status, and obesity in Mexican Americans, Cuban Americans, and Puerto Ricans. Int J Obes Relat Metab Disord. 1997;21:91–6. doi: 10.1038/sj.ijo.0800367. [DOI] [PubMed] [Google Scholar]
- 4.Sundquist J, Winkleby M. Country of birth, acculturation status and abdominal obesity in a national sample of Mexican-American women and men. Int J Epidemiol. 2000;29:470–7. [PubMed] [Google Scholar]
- 5.Crespo CJ, Loria CM, Burt VL. Hypertension and other cardiovascular disease risk factors among Mexican Americans, Cuban Americans, and Puerto Ricans from the Hispanic Health and Nutrition Examination Survey. Public Health Rep. 1996;111(Suppl 2):7–10. [PMC free article] [PubMed] [Google Scholar]
- 6.Sundquist J, Winkleby MA, Pudaric S. Cardiovascular disease risk factors among older black, Mexican-American, and white women and men: an analysis of NHANES III, 1988-1994. Third National Health and Nutrition Examination Survey. J Am Geriatr Soc. 2001;49:109–16. doi: 10.1046/j.1532-5415.2001.49030.x. [DOI] [PubMed] [Google Scholar]
- 7.Baldwin C, Reynaga-Ornelas L, Caudillo-Cisneros C, Marquez-Gamino S, Quan SF. Overview of sleep disorders among Latinos in the United States. Hispanic Health Care Int. 2010;8:180–7. [Google Scholar]
- 8.Ribisl KM, Winkleby MA, Fortmann SP, Flora JA. The interplay of socioeconomic status and ethnicity on Hispanic and white men's cardiovascular disease risk and health communication patterns. Health Educ Res. 1998;13:407–17. doi: 10.1093/her/13.3.407. [DOI] [PubMed] [Google Scholar]
- 9.Winkleby MA, Fortmann SP, Rockhill B. Health-related risk factors in a sample of Hispanics and whites matched on sociodemographic characteristics. The Stanford Five-City Project. Am J Epidemiol. 1993;137:1365–75. doi: 10.1093/oxfordjournals.aje.a116646. [DOI] [PubMed] [Google Scholar]
- 10.National Center for Health Statistics. Health, United States, 2009: with special feature on medical technology. [Accessed July 5, 2011]. http://www.cdc.gov/omhd/populations/HL/hl.htm. [PubMed]
- 11.Kapur VK, Redline S, Nieto FJ, Young TB, Newman AB, Henderson JA. The relationship between chronically disrupted sleep and healthcare use. Sleep. 2002;25:289–96. [PubMed] [Google Scholar]
- 12.Kojima M, Wakai K, Kawamura T, et al. Sleep patterns and total mortality: a 12-year follow-up study in Japan. J Epidemiol. 2000;10:87–93. doi: 10.2188/jea.10.87. [DOI] [PubMed] [Google Scholar]
- 13.Spiegel K, Knutson K, Leproult R, Tasali E, Van Cauter E. Sleep loss: a novel risk factor for insulin resistance and Type 2 diabetes. J Appl Physiol. 2005;99:2008–19. doi: 10.1152/japplphysiol.00660.2005. [DOI] [PubMed] [Google Scholar]
- 14.Van Cauter E, Holmback U, Knutson K, et al. Impact of sleep and sleep loss on neuroendocrine and metabolic function. Horm Res. 2007;67(Suppl 1):2–9. doi: 10.1159/000097543. [DOI] [PubMed] [Google Scholar]
- 15.Marin JM, Carrizo SJ, Vicente E, Agusti AG. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet. 2005;365:1046–53. doi: 10.1016/S0140-6736(05)71141-7. [DOI] [PubMed] [Google Scholar]
- 16.Peppard PE, Young T, Palta M, Skatrud J. Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med. 2000;342:1378–84. doi: 10.1056/NEJM200005113421901. [DOI] [PubMed] [Google Scholar]
- 17.Punjabi NM, Shahar E, Redline S, Gottlieb DJ, Givelber R, Resnick HE. Sleep-disordered breathing, glucose intolerance, and insulin resistance: the Sleep Heart Health Study. Am J Epidemiol. 2004;160:521–30. doi: 10.1093/aje/kwh261. [DOI] [PubMed] [Google Scholar]
- 18.Yaggi HK, Concato J, Kernan WN, Lichtman JH, Brass LM, Mohsenin V. Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med. 2005;353:2034–41. doi: 10.1056/NEJMoa043104. [DOI] [PubMed] [Google Scholar]
- 19.Young T, Finn L, Peppard PE, et al. Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin sleep cohort. Sleep. 2008;31:1071–8. [PMC free article] [PubMed] [Google Scholar]
- 20.Loredo JS, Soler X, Bardwell W, Ancoli-Israel S, Dimsdale JE, Palinkas LA. Sleep health in U.S. Hispanic population. Sleep. 2010;33:962–7. doi: 10.1093/sleep/33.7.962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry. 2002;59:131–6. doi: 10.1001/archpsyc.59.2.131. [DOI] [PubMed] [Google Scholar]
- 22.Chung F, Yegneswaran B, Liao P, et al. STOP questionnaire: a tool to screen patients for obstructive sleep apnea. Anesthesiology. 2008;108:812–21. doi: 10.1097/ALN.0b013e31816d83e4. [DOI] [PubMed] [Google Scholar]
- 23.Abrishami A, Khajehdehi A, Chung F. A systematic review of screening questionnaires for obstructive sleep apnea. Can J Anaesth. 57:423–38. doi: 10.1007/s12630-010-9280-x. [DOI] [PubMed] [Google Scholar]
- 24.Chung F, Yegneswaran B, Liao P, et al. Validation of the Berlin questionnaire and American Society of Anesthesiologists checklist as screening tools for obstructive sleep apnea in surgical patients. Anesthesiology. 2008;108:822–30. doi: 10.1097/ALN.0b013e31816d91b5. [DOI] [PubMed] [Google Scholar]
- 25.Bastien CH, Vallieres A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2:297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 26.Morin CM, Colecchi C, Stone J, Sood R, Brink D. Behavioral and pharmacological therapies for late-life insomnia: a randomized controlled trial. JAMA. 1999;281:991–9. doi: 10.1001/jama.281.11.991. [DOI] [PubMed] [Google Scholar]
- 27.Backhaus J, Junghanns K, Broocks A, Riemann D, Hohagen F. Test-retest reliability and validity of the Pittsburgh Sleep Quality Index in primary insomnia. J Psychosom Res. 2002;53:737–40. doi: 10.1016/s0022-3999(02)00330-6. [DOI] [PubMed] [Google Scholar]
- 28.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 29.Carpenter JS, Andrykowski MA. Psychometric evaluation of the Pittsburgh Sleep Quality Index. J Psychosom Res. 1998;45:5–13. doi: 10.1016/s0022-3999(97)00298-5. [DOI] [PubMed] [Google Scholar]
- 30.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 31.Johns MW. Reliability and factor analysis of the Epworth Sleepiness Scale. Sleep. 1992;15:376–81. doi: 10.1093/sleep/15.4.376. [DOI] [PubMed] [Google Scholar]
- 32.Johns MW. Sensitivity and specificity of the multiple sleep latency test (MSLT), the maintenance of wakefulness test and the Epworth sleepiness scale: failure of the MSLT as a gold standard. J Sleep Res. 2000;9:5–11. doi: 10.1046/j.1365-2869.2000.00177.x. [DOI] [PubMed] [Google Scholar]
- 33.Iber C, Ancoli-Israel S, Chesson A, Quan SF. for the American Academy of Sleep Medicine. AASM manual for the scoring of sleep and associated events: rules, terminology, and technical specifications. 1st ed. Westchester, IL: 2007. [Google Scholar]
- 34.Passel JS, D'Vera C. Pew Hispanic Center Reports: How Many Hispanics, March 30, 2011. [Accessed June 10, 2011]. Available from: http://pewhispanic.org.
- 35.O'Connor GT, Lind BK, Lee ET, et al. Variation in symptoms of sleep-disordered breathing with race and ethnicity: the Sleep Heart Health Study. Sleep. 2003;26:74–9. [PubMed] [Google Scholar]
- 36.Schmidt-Nowara WW, Coultas DB, Wiggins C, Skipper BE, Samet JM. Snoring in a Hispanic-American population. Risk factors and association with hypertension and other morbidity. Arch Intern Med. 1990;150:597–601. doi: 10.1001/archinte.150.3.597. [DOI] [PubMed] [Google Scholar]
- 37.Netzer NC, Hoegel JJ, Loube D, et al. Prevalence of symptoms and risk of sleep apnea in primary care. Chest. 2003;124:1406–14. doi: 10.1378/chest.124.4.1406. [DOI] [PubMed] [Google Scholar]
- 38.Senthilvel E, Auckley D, Dasarathy J. Evaluation of sleep disorders in the primary care setting: history taking compared to questionnaires. J Clin Sleep Med. 2011;7:41–8. [PMC free article] [PubMed] [Google Scholar]
- 39.Kripke DF, Ancoli-Israel S, Klauber MR, Wingard DL, Mason WJ, Mullaney DJ. Prevalence of sleep-disordered breathing in ages 40-64 years: a population-based survey. Sleep. 1997;20:65–76. doi: 10.1093/sleep/20.1.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bouscoulet LT, Vazquez-Garcia JC, Muino A, et al. Prevalence of sleep related symptoms in four Latin American cities. J Clin Sleep Med. 2008;4:579–85. [PMC free article] [PubMed] [Google Scholar]
- 41.Redline S, Arens R, Daviglus M, et al. Prevalence of sleep apnea, associated symptoms and comorbidities in the Hispanic Community Health Study/ Study of Latinos (HCHS/SOL) [abstract] Nutrition, Physical Activity and Metabolism and Cardiovascular Disease Epidemiology and Prevention Joint Conference; March 2011; Atlanta. [Google Scholar]
- 42.Sorlie PD, Aviles-Santa LM, Wassertheil-Smoller S, et al. Design and implementation of the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol. 2010;20:629–41. doi: 10.1016/j.annepidem.2010.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328:1230–5. doi: 10.1056/NEJM199304293281704. [DOI] [PubMed] [Google Scholar]
- 44.Baldwin CM, Ervin AM, Mays MZ, et al. Sleep disturbances, quality of life, and ethnicity: the Sleep Heart Health Study. J Clin Sleep Med. 2010;6:176–83. [PMC free article] [PubMed] [Google Scholar]
- 45.Ram S, Seirawan H, Kumar SK, Clark GT. Prevalence and impact of sleep disorders and sleep habits in the United States. Sleep Breath. 2010;14:63–70. doi: 10.1007/s11325-009-0281-3. [DOI] [PubMed] [Google Scholar]
- 46.2010 Sleep in America Poll: Summary of Findings. [Accessed June 9, 2011]. Available from: http://www.sleepfoundation.org/article/sleep-america-polls/2010-sleep-and-ethnicity.
- 47.Hale L, Do DP. Racial differences in self-reports of sleep duration in a population-based study. Sleep. 2007;30:1096–103. doi: 10.1093/sleep/30.9.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Grandner MA, Patel NP, Gehrman PR, et al. Who gets the best sleep? Ethnic and socioeconomic factors related to sleep complaints. Sleep Med. 2010;11:470–8. doi: 10.1016/j.sleep.2009.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Masa JF, Rubio M, Findley LJ. Habitually sleepy drivers have a high frequency of automobile crashes associated with respiratory disorders during sleep. Am J Respir Crit Care Med. 2000;162:1407–12. doi: 10.1164/ajrccm.162.4.9907019. [DOI] [PubMed] [Google Scholar]
- 50.Young T, Blustein J, Finn L, Palta M. Sleep-disordered breathing and motor vehicle accidents in a population-based sample of employed adults. Sleep. 1997;20:608–13. doi: 10.1093/sleep/20.8.608. [DOI] [PubMed] [Google Scholar]
- 51.Bercovitch R, Palinkas LA, Ancoli-Israel S, Dimsdale J, Loredo J. Effect of Ethnicity and Acculturation on Obstructive Sleep Apnea Prevalence and Severity in Non Hispanic Whites and Hispanics of Mexican Descent in San Diego County: Preliminary Findings. Sleep. 2011;34:A124. Abstract Supplement. [Google Scholar]


