Abstract
Taxanes are potent inhibitors of cell motility, a property implicated in their antiangiogenic and antimetastatic activity and unrelated to their antiproliferative effect. The molecular mechanism of this anti-motility activity is poorly understood. In this study, we found that paclitaxel induced tubulin acetylation in endothelial and tumor cells, at concentrations that affected cell motility but not proliferation (10-8 to 10-9 M, for 4 hours). Induction of tubulin acetylation correlated with inhibition of motility but not proliferation based on a comparison of highly and poorly cytotoxic taxanes (paclitaxel and IDN5390) and tumor cell lines sensitive and resistant to paclitaxel (1A9 and 1A9 PTX22). Consistent with the hypothesis that tubulin deacetylase activity might affect cell response to the anti-motility activity of taxanes, we found that overexpression of the tubulin deacetylase SIRT2 increased cell motility and reduced cell response to the anti-motility activity of paclitaxel. Conversely, the SIRT2 inhibitor splitomicin reduced cell motility and potentiated the anti-motility activity of paclitaxel. The inhibitory effect was further potentiated by the addition of the HDAC6 inhibitor trichostatin A. Paclitaxel and splitomicin promoted translocation into the nucleus—and hence activation—of FOXO3a, a negative regulator of cell motility. This study indicates a role for SIRT2 in the regulation of cell motility and suggests that therapies combining sirtuin inhibitors and taxanes could be used to treat cell motility-based pathologic processes such as tumor angiogenesis, invasion, and metastasis.
Introduction
Cell motility is a central event in a number of physiological and pathologic processes. Agents that perturb the finely tuned microtubule organization, stability, and dynamics inhibit cell motility and have been proposed as therapeutic inhibitors of motility-based pathologies, including cancer metastasis and pathologic angiogenesis. Among these, the antineoplastic drug paclitaxel and other taxanes have anti-motility activity for tumor and endothelial cells, a property thought to contribute to their antimetastatic and antiangiogenic activity. This effect of tubulin-targeting compounds has opened new therapeutic opportunities to target the tumor vascular compartment and the metastatic dissemination of tumor cells [1,2].
The molecular mechanisms of the anti-motility activity of taxanes is still poorly understood [3]. Three lines of evidence indicate that the effect of taxanes on cell motility is distinct from their cytotoxic activity. First, cell motility is inhibited by taxanes at concentrations lower than the cytotoxic concentrations. A short exposure to low concentrations of paclitaxel has no effect on cell proliferation or apoptosis but affects microtubule dynamics, cell motility, and morphogenesis [4–7]. Second, tumor cells harboring the A364T mutation in β-tubulin are resistant to the antiproliferative activity of paclitaxel but nonetheless remain sensitive to the anti-motility effect of taxanes [8]. Third, the seco-derivative taxane IDN5390 exhibits potent anti-motility and antiangiogenic activity but a lower cytotoxicity compared to paclitaxel [9,10], further supporting the concept that the antiproliferative and anti-motility activity of taxanes work through different pathways.
Microtubule-dependent events potentially responsible for the inhibition of cell motility—rather than proliferation—include promotion of microtubule stability, alteration of microtubule dynamics, and induction of tubulin posttranslational modifications such as acetylation. Taxanes increase tubulin acetylation [11,12], although the functional relevance of this event in inhibition of cell motility has not been clarified.
Reversible posttranslational modifications of tubulin are considered responsible for the structural and functional diversity of microtubule subpopulations, characterized by a fine spatial and temporal regulation [12,13]. Acetylation occurs at the ɛ-amino group of Lys40 in the α-tubulin, and although other acetylation sites have been recently identified [14], acetylation of this particular lysine has been correlated with changes in cell motility [12]. Tubulin acetylation is mainly regulated by a complex constituted by the class IIb histone deacetylase HDAC6 and the NAD-dependent histone deacetylase SIRT2.
Sirtuins are NAD+-dependent protein deacetylases and are implicated in a variety of biologic processes including metabolic regulation and cellular response to a variety of physiological stresses. SIRT2 is predominantly cytoplasmic but shuttles between the nuclear compartment and the cytoplasm during interphase, and it is mainly nuclear during mitosis [15]. It deacetylates molecular targets both in the nucleus and cytoplasm, such as histone H4 [16] and tubulin [17], and is involved in the regulation of cell cycle progression [18–20].
HDAC6 and SIRT2 interact in the cytoplasm, where they bind tubulin, colocalize with microtubules, and deacetylate tubulin [17,21,22]. HDAC6 and SIRT2 differ in their ability to deacetylate tubulin substrates, because SIRT2 deacetylates tubulin also as cell lysate-derived heterodimers and taxol-stabilized microtubules whereas these forms of tubulin are relatively resistant to HDAC6 [17,23].
Acetylation of α-tubulin is a marker of microtubule stability, although whether there is a causal relationship between acetylation and stability is still debated [12]. Tubulin acetylation/deacetylation participates in the regulation of cell motility: Overexpression of HDAC6 decreases tubulin acetylation and increases cell motility in fibroblast [21,24] and in breast cancer cells [25]. Conversely, reduced cell motility and increased tubulin acetylation are observed in fibroblasts and transformed cells following reduction of HDAC6 activity, either by deacetylase inhibitors [such as trichostatin A (TSA) and tubacin] [24,26] or following knockdown of the deacetylase [26,27]. Less is known on the role of SIRT2 in cell motility.
Taxanes and tubulin deacetylases share the same target, tubulin, and both induce changes in tubulin acetylation. Both tubulin acetylation and binding of taxanes are predicted to occur in the lumen of the microtubule structure [3,11,13], suggesting that these compounds modulate the transmission of signals from the lumen of the microtubules to the cytoskeleton.
Selective HDAC6 inhibitors synergize with taxanes, and combination regimens that include both classes of compounds have proven effective in preclinical studies and are currently in clinical trials in cancer patients [28,29]. Inhibitors of sirtuins have also been proposed as antineoplastic agents [23,29], although the exact sirtuin involved (SIRT1 vs SIRT2), the mechanisms of action, and the possibilities of combinations with other agents have not been investigated.
This study was designed to investigate whether modification of tubulin acetylation, particularly through the modulation of SIRT2 activity, might affect cell susceptibility to the anti-motility effect of taxanes. We describe that modulation of SIRT2 activity affects cell motility and response to the anti-motility activity of taxanes, suggesting that specific inhibitors of SIRT2 might represent a new tool to potentiate the activity of taxanes in antineoplastic combination therapies.
Materials and Methods
Reagents
Paclitaxel and IDN5390 were provided by Indena S.p.A. (Milan, Italy). Splitomicin [30], TSA, and sirtinol (Sigma, St Louis, MO) were dissolved in DMSO (1000x stock solution) and further diluted in test medium immediately before the assay (control cells received the same amount of DMSO). Nicotinamide (Sigma) was dissolved in water.
Cells
Primary cultures of endothelial cells (human umbilical vein endothelial cells [HUVECs]) were isolated from umbilical cord veins and grown on 1% gelatin-coated flasks in M199 supplemented with 10% FBS, 10% newborn calf serum, 20 mM Hepes, 2 mM glutamine, 6 U/ml heparin, 50 µg/ml endothelial cell growth factor, penicillin, and streptomycin. Cells were used between the third and fifth passages. The 1A9 human ovarian carcinoma cell line and its paclitaxel-resistant variant, 1A9 PTX22 [31], were obtained from A. Fojo (National Cancer Institute, National Institutes of Health, Bethesda, MD) and grown in RPMI with 10% FBS and 2 mM glutamine. Stocks of cell lines, authenticated by short-tandem repeat profiling (AmpFlSTR Identifiler Plus PCR Amplification Kit; Applied Biosystems, Carlsbad, CA), were stored frozen in liquid nitrogen and used within 8 weeks after thawing.
Western Blot Analysis of Tubulin Acetylation
Endothelial or tumor cells were plated in a 24-well plate in complete medium. The next day, cells were treated with the indicated compound for 4 hours. After washing with phosphate-buffered saline (PBS), cells were lysed in 100 µl of lysis buffer [20 mM Tris-HCl (pH 7.6), 170 mM NaCl, 1 mM EDTA, 1 mM DTT, 1% Triton, 5 µM TSA, and Roche Protease Inhibitor Cocktail Tablet] and centrifuged at 14000 rpm for 10 minutes. Proteins were electrophoresed on a 10% sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) gel and transferred to a nitrocellulose membrane (Schleicher & Schuell, Dassel, Germany). After blocking overnight at 4°C with ECL advance blocking agent, membranes were probed with anti-acetylated tubulin antibody (1:2000, T6793 clone 6-11B-1) or anti-total tubulin antibody (1:500, T9026), both antibodies from Sigma, in PBS/0.5% Tween, for 1 hour at room temperature, followed by peroxidase-conjugated anti-mouse IgG (Sigma) and Amersham ECL Plus Western Blotting Detection Reagent (GE Healthcare Europe GmbH, Milan, Italy). After scanning (Duoscan T1200, AGFA), densitometry was analyzed with Gel-Pro Analyzer 3.1 (Media Cybernetics, Silver Spring, MD).
Immunofluorescence Analysis of Tubulin Acetylation
Endothelial cells were plated on coverslips and incubated overnight. After treatment with IDN5390 or paclitaxel (10 nM for 4 hours), cells were fixed with methanol at -20°C for 10 minutes. Coverslips were washed in PBS and incubated in blocking solution (5% normal goat serum in PBS) for 30 minutes at room temperature. Incubation with antibodies against acetylated tubulin (1:1000, T6793, Sigma) in blocking solution was carried out for 1 hour at room temperature. After washing, tetramethylrhodamine isothiocyanate (TRITC)-conjugated rabbit anti-mouse IgG (1:300, Sigma) in blocking solution was incubated for 1 hour. Nuclei were counterstained by 4′,6-diamidino-2-phenylindole (DAPI; 100 µg/ml, Sigma). Slides were analyzed by a fluorescence microscope (OLYMPUS IX70).
Colocalization of SIRT2 with Microtubules
Endothelial cells were plated on coverslips and incubated overnight. After treatment with paclitaxel or IDN5390 (100 nM for 4 hours), cells were fixed with methanol at -20°C for 10 minutes. Coverslips were then washed in PBS and incubated in blocking solution (5% normal goat serum in PBS) for 30 minutes at room temperature. Slides were incubated with fluorescein isothiocyanate (FITC)-conjugated monoclonal anti-β-tubulin (1:25, Sigma) and chicken anti-human SIRT2 (1:50, [17]), in blocking solution for 1 hour at room temperature, followed by incubation with TRITC-conjugated rabbit anti-chicken IgG (1:50; Jackson ImmunoResearch, Newmarket, United Kingdom). Slides were analyzed with a Zeiss LSM 510 Meta confocal microscope.
Immunofluorescence Analysis of FOXO3a
HUVECs were plated on coverslips and incubated overnight. After treatment with paclitaxel (10 nM), splitomicin (1.2 mM), or TSA (1 µM) for 4 hours, cells were fixed with 3% paraformaldehyde for 20 minutes, washed in PBS, and permeabilized with 0.1% Triton X-100 in PBS. After blocking (in 5% goat serum in PBS) for 30 minutes, cells were stained with antibodies against FOXO3a (1:50, 75D8; Cell Signaling Technology, Danvers, MA) in blocking solution for 40 minutes at 37°C, followed by Alexa Fluor 546 anti-rabbit IgG (1:100; Invitrogen, Carlsbad, CA) for 45 minutes at room temperature. Nuclei were counterstained by DAPI (100 µg/ml, Sigma). Slides were analyzed with a Zeiss LSM 510 Meta confocal microscope.
Motility Assay
Chemotaxis was assessed using Boyden chambers and gelatin-coated polycarbonate nucleopore filters (8-µm pore size). The supernatant of NIH-3T3 cells was used as the attractant. Cells were resuspended in Dulbecco's modified Eagle's medium/0.1% BSA at a concentration of 1.5 x 106/ml and added to the upper compartment of the chamber. IDN5390, paclitaxel, or histone deacetylase inhibitors at the indicated concentration were added to the cells and incubated throughout the assay (4 hours). At the end of incubation, filters were stained with Diff-Quik (Marz-Dade, Dundingen, Switzerland) and the migrated cells were counted in 10 high-power fields.
Proliferation Assay
Cells (2–3 x 103 cells/well) were plated in a 96-well plate in complete medium. After 24 hours, IDN5390, paclitaxel, or histone deacetylase inhibitors at the indicated concentration were added and incubated for 4 hours. Cells were then washed and incubated in culture medium for an additional 72 hours. In parallel plates, cells were exposed to the compounds for the entire duration of the assay (72 hours). Cells were fixed and stained with 0.5% crystal violet in 20% methanol. The stain was eluted with a 1:1 solution of ethanol/0.1 M sodium citrate, and the absorbance at 540 nm was measured.
SIRT2 Stable Transfection
Human wild-type green fluorescent protein (GFP)-SIRT2 and the catalytically inactive mutant N168A plasmids were prepared as described [17]. Subconfluent 1A9 human ovarian carcinoma cells were transfected using Lipofectin Reagent (Invitrogen) following manufacturer's protocol. For selection, cells were cultured in medium containing 800 µg/ml of G418 (Invitrogen) and subsequently enriched in GFP-expressing cells by fluoresence-activated cell sorter (FACS). Western blot analysis of cell lysates with anti-SIRT2 antibody [17] confirmed that the transfected cells produced similar amounts of wild-type and mutated proteins that were barely detectable in parental cells.
SIRT2 Silencing
HUVECs were transiently transfected with siRNA for human SIRT2 (mix of Hs_SIRT2_1_HP and Hs_SIRT2_4_HP) or HDAC6 (Hs_HDAC6_6_HP, all from Qiagen, Hilden, Germany) by electroporation. Forty-eight hours later, cells were subjected to a second round of transfection, and after additional 48 hours, cells were tested for transcript expression, tubulin acetylation, and motility. Silencing of the transcripts was verified by real-time reverse transcription-polymerase chain reaction (PCR; TaqMan Gene Expression Assay Hs00247263-m1 and Hs00195869-m1; Applied Biosystems), normalizing data on 18s rRNA expression (Assay Hs99999901-s1; Applied Biosystems).
Results
We have investigated the activity of taxanes on endothelial and tumor cell motility, which represents critical events in the processes of, respectively, tumor angiogenesis and metastasis. To focus on events associated with inhibition of cell motility rather than proliferation, we used experimental conditions in which taxanes inhibited cell motility without affecting proliferation [4,8]. We also used the seco-derivative taxane IDN5390, which exhibits anti-motility activity and reduced cytotoxicity compared to paclitaxel ([9,10], summarized in Table W1).
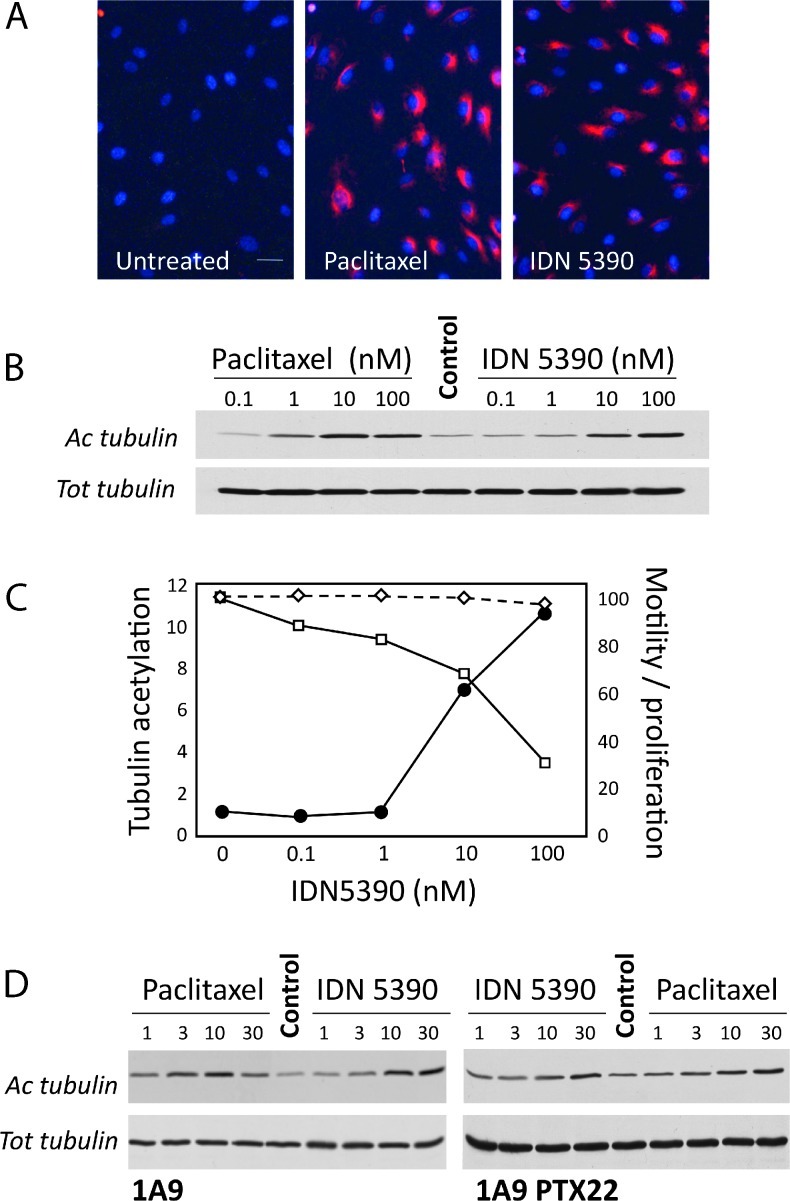
Endothelial cells were exposed to paclitaxel or IDN5390 for 4 hours, and tubulin acetylation levels were assessed. Both PTX and IDN5390 increased the levels of acetylated tubulin in treated HUVECs, using either immunofluorescence (Figure 1A) or Western blot analysis (Figure 1B). Induction of tubulin hyperacetylation paralleled the inhibition of cell motility but not of proliferation, which occurred at concentrations much higher than those required to inhibit motility (particularly for IDN5390), even when cells were treated with the taxane for longer times or cytotoxicity was assessed by quantifying the mitotic index (Figures 1C and W1).
Figure 1.
Effect of paclitaxel and IDN5390 on tubulin acetylation and motility in endothelial and tumor cells. (A) Immunofluorescence analysis of acetylated tubulin in HUVECs untreated or treated with 10 nM paclitaxel or IDN5390 for 4 hours (scale bar, 20 µm). (B) Western blot analysis of acetylated and total tubulin in HUVECs exposed for 4 hours to increasing concentrations of paclitaxel or IDN5390. (C) Increased tubulin acetylation (black circles), decreased cell motility (open squares), and unaffected cell proliferation (open diamonds, dotted line) after a 4-hour exposure to IDN5390. Tubulin acetylation is expressed as fold increase of untreated cells and was calculated as the ratio of optical density values of acetylated tubulin versus total tubulin. Migration and proliferation are expressed as percentage of control, untreated cells. (D) Western blot analysis of acetylated and total tubulin comparing the response of sensitive 1A9 and paclitaxel-resistant 1A9 PTX22 cells to a 4-hour exposure to paclitaxel or IDN5390.
To confirm the separation between the effect of taxanes on cell proliferation and motility also in cancer cells, we used 1A9 PTX22 cells, which are resistant to the antiproliferative activity of taxanes but sensitive to their anti-motility effect, as shown by the previous finding that paclitaxel and IDN5390 induced a comparable reduction of motility in paclitaxel-resistant 1A9 PTX22 cells and in the paclitaxel-sensitive parental 1A9 cells ([8,9], summarized in Table W2). Interestingly, both the highly cytotoxic paclitaxel and the low cytotoxic IDN5390 induced tubulin acetylation in 4 hours at concentrations sufficient to inhibit cell motility (∼30 nM) in both cell lines irrespective of their sensibility to inhibition of proliferation (Figures 1D and W2).
These findings support the hypothesis that tubulin acetylation might be implicated in the anti-motility activity of taxanes. To test this possibility, we first tested whether inhibitors of the tubulin deacetylases HDAC6 and SIRT2 affected the motility of endothelial cells. As reported, TSA, a broad spectrum hydroxamic acid inhibitor of class I and II HDAC (which include HDAC6), inhibited endothelial cell motility, although inhibitors of sirtuins appeared more effective (Figure 2A). Nicotinamide, sirtinol, and splitomicin inhibited endothelial cell motility in a dose-dependent manner with IC50 of 47.9 ± 0.7 mM, 43.3 ± 0.3 µM, and 1.6 ± 0.2 mM, respectively (not shown and Figure 2B). Inhibition of cell motility by splitomicin significantly correlated with induction of tubulin acetylation (P = .01; Figure 2, B and C).
Figure 2.
Effect of SIRT2 modulation in cell motility. (A) Effect of different histone deacetylase inhibitors on endothelial cell motility. Cells were exposed to splitomicin (2.4 mM), sirtinol (50 µM), nicotinamide (75 mM), or TSA (1 µM) for the duration of the assay (4 hours). Motility is expressed as percentage of control migration in the absence of inhibitors (mean and SE of values from two to four experiments). *P ≤ .01 and **P ≤ .001 compared to control (analysis of variance followed by Dunnet test). (B) Concentration-dependent inhibition of motility (open squares) and tubulin acetylation (black circles) by splitomicin. For motility, data are the percentage of control motility (mean and SE of values from six experiments). Tubulin acetylation, evaluated by Western blot, is expressed as fold increase of untreated cells, calculated as in Figure 1 (mean of four experiments). (C) Effect of splitomicin on tubulin acetylation: Western blot analysis of acetylated and total tubulin in HUVECs exposed for 4 hours to splitomicin. (D) Migration (expressed as percentage of control) and tubulin acetylation of endothelial cells transiently transfected with SIRT2 or HDAC6 siRNA. Results are from one experiment representative of two independent transfections. *P ≤ .01 compared to control (Mann-Whitney test). (E) Increased migration and reduced tubulin acetylation in 1A9 cells stably transfected to overexpress SIRT2 (1A9-S2) or catalytically inactive mutated SIRT2 (1A9-mutS2). Cell migration is expressed as percentage of control, 1A9-mutS2 cells (mean and SE of values from three experiments). *P < .01 compared to 1A9-mutS2 cells (Mann-Whitney test).
Splitomicin was not as potent as TSA in promoting tubulin acetylation (TSA induced a 26.3 ± 8.4 fold increase of acetylation, not shown), but it was more potent in inhibiting motility (Figure 2A).
Because splitomicin is not selective for SIRT2 and inhibits all sirtuins, we further tested the role of SIRT2 using siRNA knockdown in endothelial cells and SIRT2 stable overexpression in cancer cells. Silencing of SIRT2 (67% reduction measured by real-time PCR) was accompanied by decreased motility and increased tubulin acetylation compared to mock-transfected cells (Figure 2D). Consistent with the different potency of SIRT inhibitors and TSA in affecting cell motility and tubulin acetylation, silencing of SIRT2 was more effective in inhibiting cell motility than silencing of HDAC6 (62% reduction) although the latter was more effective in increasing tubulin acetylation (Figure 2D). To investigate the role of SIRT2 overexpression on cell motility, we stably transfected 1A9 cells to overexpress wild-type (1A9-S2) or catalytically inactive SIRT2 (1A9-mutS2, Figure W3). Overexpression of SIRT2 did not relevantly affect cell proliferation (doubling time was 23.1 ± 3.4 and 21.9 ± 2.3 hours for 1A9-S2 and 1A9-mutS2, respectively), morphology, or tubulin organization (Figure W4). However, overexpression of SIRT2 markedly increased cell motility and decreased the levels of tubulin acetylation (Figure 2E), further confirming that catalytically active SIRT2 regulates cell motility. Interestingly, 1A9-mutS2 cells presented a slightly increased tubulin acetylation and decreased cell motility compared to parental 1A9 cells (not shown), suggesting that in this system the catalytically inactive SIRT2 might act as an inhibitor of endogenous SIRT2.
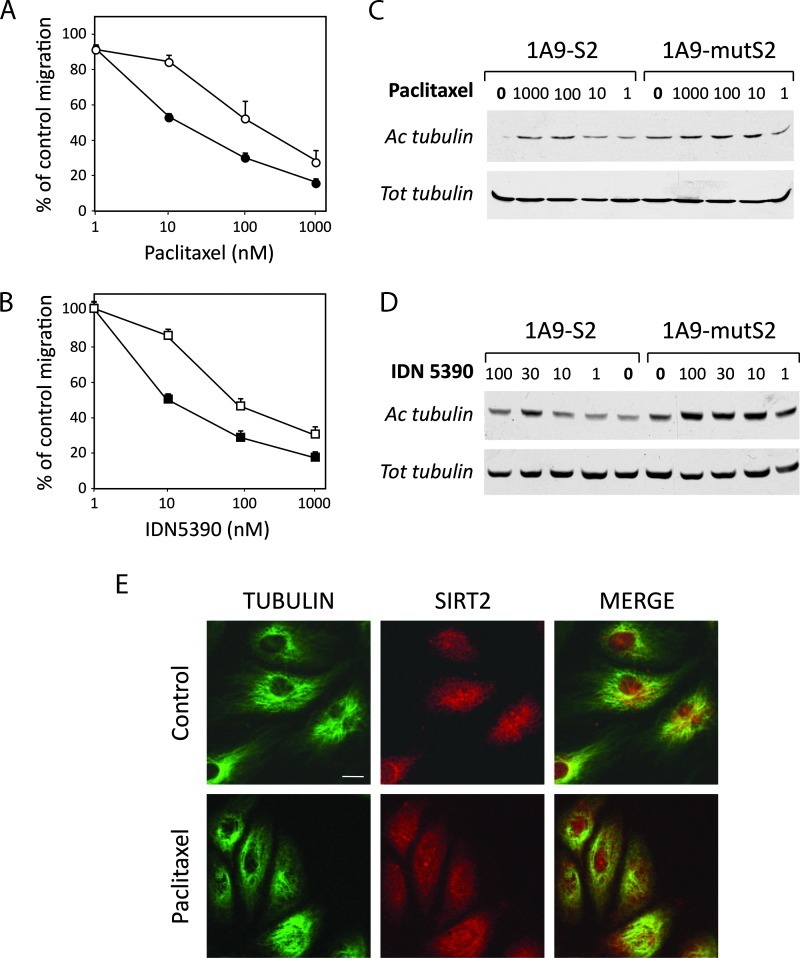
Next, we tested the role of SIRT2 in the anti-motility activity of taxanes. SIRT2-overexpressing 1A9-S2 cells were less responsive to the anti-motility activity of both paclitaxel and IDN5390 than control 1A9-mutS2 cells (Figure 3, A and B, and Table 1). Moreover, the difference in tubulin acetylation between 1A9-S2 and 1A9-mutS2 cells was maintained after taxane treatment. SIRT2-overexpressing cells exposed for 4 hours to paclitaxel or IDN5390 showed lower tubulin acetylation compared to control cells (Figure 3, C and D). Again, the differential sensitivity in terms of cell motility was dissociated from the antiproliferative response: The antiproliferative activity of both taxanes was unaffected by changes in SIRT2 activity in cells treated for either 4 or 72 hours (Table 1).
Figure 3.
Effect of SIRT2 overexpression on cell sensitivity to taxanes. Inhibition of cell motility (A, B) and induction of tubulin acetylation (C, D) by paclitaxel (A, C) or IDN5390 (B, D) in cells overexpressing SIRT2 (1A9-S2, white symbols) or control, inactive SIRT2 (1A9-mutS2, black symbols). Cell migration is expressed as the percentage of control, untreated cells. (E) No effect of paclitaxel on the colocalization of SIRT2 with microtubules. HUVECs were treated with paclitaxel (100 nM) for 4 hours, fixed, and processed for double immunofluorescence with FITC-conjugated anti-β-tubulin and anti-human SIRT2 followed by TRITC-conjugated secondary antibody. Slides were analyzed with a confocal microscope (scale bar, 10 µm).
Table 1.
Activity of Taxanes on 1A9 Cells Overexpressing Wild-type or Control, Mutated SIRT2.
| Paclitaxel | IDN5390 | |||||
| Motility | Prol (72 hours) | Prol (4 hours) | Motility | Prol (72 hours) | Prol (4 hours) | |
| 1A9-S2 | 244.3 ± 141.1 | 4.6 ± 2.5 | 22.4 ± 14.5 | 143.5 ± 53.3 | 33.1 ± 15.3 | 241.9 ± 128.6 |
| 1A9-mutS2 | 24.5 ± 4.9 | 4.6 ± 2.1 | 34.4 ± 21.8 | 18.8 ± 5.9 | 41.9 ± 25.0 | 442.3 ± 49.1 |
Data are the IC50 values (in nM) and mean and SE of values from three experiments. Proliferation (prol) was assessed by exposing cells to the compounds for 4 hours (as in the motility assay) or 72 hours.
To investigate whether SIRT2 might be a direct target of taxanes, we analyzed the effect of paclitaxel on SIRT2 cellular localization and enzymatic activity. Confocal microscopy analysis confirmed that SIRT2 colocalizes with microtubules (Figures 3E and W5). Treatment of cells with paclitaxel or IDN5390 did not affect SIRT2 colocalization with the microtubules. Similar results were observed with HDAC6 (not shown). In addition, paclitaxel did not affect SIRT2 deacetylase activity on purified tubulin (Figure W6).
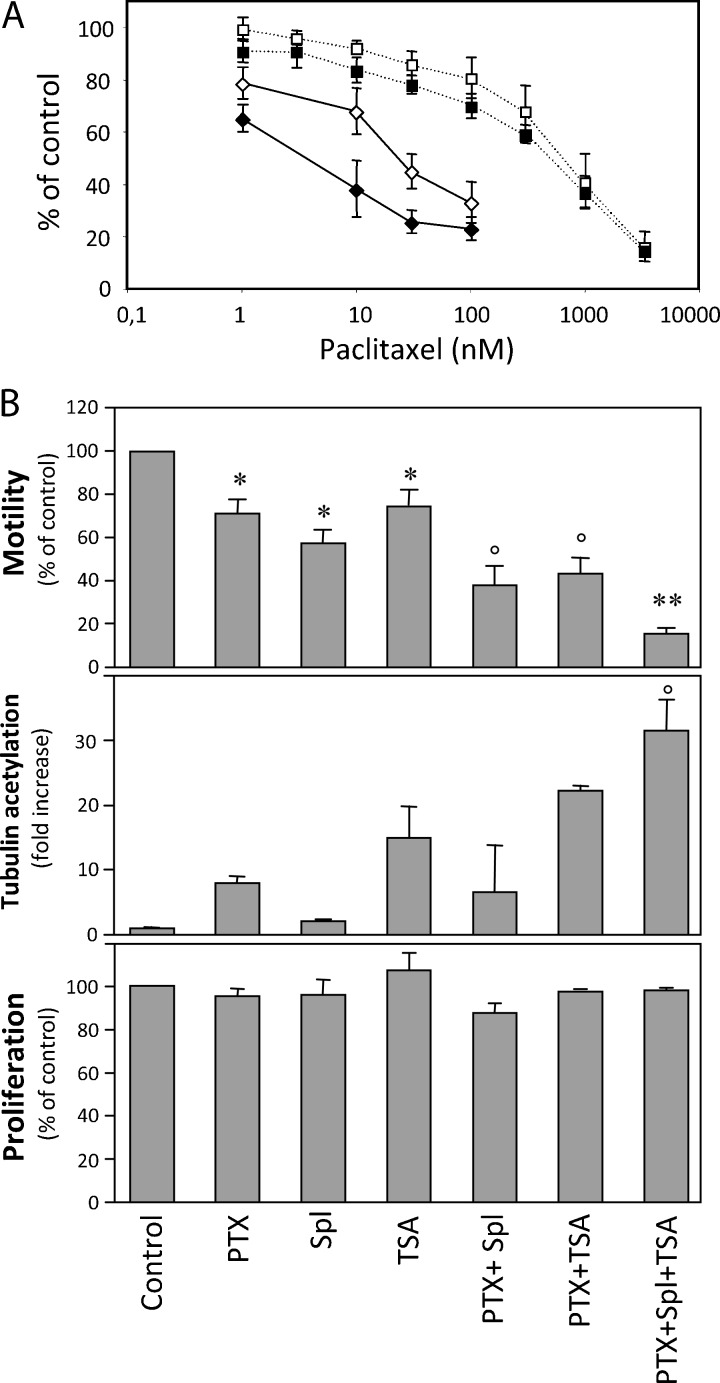
Next, we investigated the possibility that taxanes and SIRT2 inhibitors might synergize. We tested the activity of a combination of splitomicin and paclitaxel on endothelial cell motility. Splitomicin potentiated the anti-motility activity of paclitaxel (Figure 4A). The IC50 of paclitaxel was 30.5 ± 6.4 when tested alone and 10.4 ± 4.9 in the presence of splitomicin (1.2 mM). To determine whether splitomicin and paclitaxel interacted synergistically, additively, or antagonistically, we calculated the combination index (CI) [32]. The combination resulted synergistic (CI < 1) at the highest concentrations of the two agents but not at lower concentrations, suggesting that the potentiating effect of splitomicin was maximal at the most effective concentrations of the compound (Table W3). Under these conditions (4-hour exposure), the combination of the two drugs did not produce increased antiproliferative activity (Figure 4A), although a longer exposure (72 hours) to splitomicin inhibited cell proliferation (not shown), possibly through an inhibitory activity on SIRT1. A similar potentiation of paclitaxel anti-motility activity was also induced by the addition of 1 µM TSA (IC50 of paclitaxel in the presence of TSA was 13.3 ± 2.7 nM, not shown). We therefore tested whether TSA might further potentiate the activity of paclitaxel/splitomicin. The combination paclitaxel/splitomicin/TSA was even more effective in inhibiting cell motility (Figure 4B). When exposed for 4 hours to paclitaxel in combination with the two histone deacetylase inhibitors, endothelial cell motility was almost completely abolished and tubulin acetylation was highly increased, whereas proliferation was not affected.
Figure 4.
Combination of paclitaxel with tubulin deacetylase inhibitors. (A) Migration (diamonds) and proliferation (squares) of endothelial cells exposed for 4 hours to paclitaxel alone (white symbols) or in combination with 1.2 mM splitomicin (black symbols). In these experiments, splitomicin alone caused 32% inhibition of motility and 12% inhibition of proliferation. (B) Effect of a triple combination of paclitaxel (PTX, 10 nM), splitomicin (Spl, 1.2 mM), and TSA (1 µM) on endothelial cell motility, tubulin acetylation, and proliferation. Motility and proliferation are expressed as percentage of control activity (untreated cells). Tubulin acetylation is expressed as fold increase of untreated cells and was calculated as the ratio of optical density values of acetylated tubulin versus total tubulin. P < .05 compared to control (*), control and paclitaxel alone (°), and control and each inhibitor alone (**; analysis of variance followed by Bonferroni test).
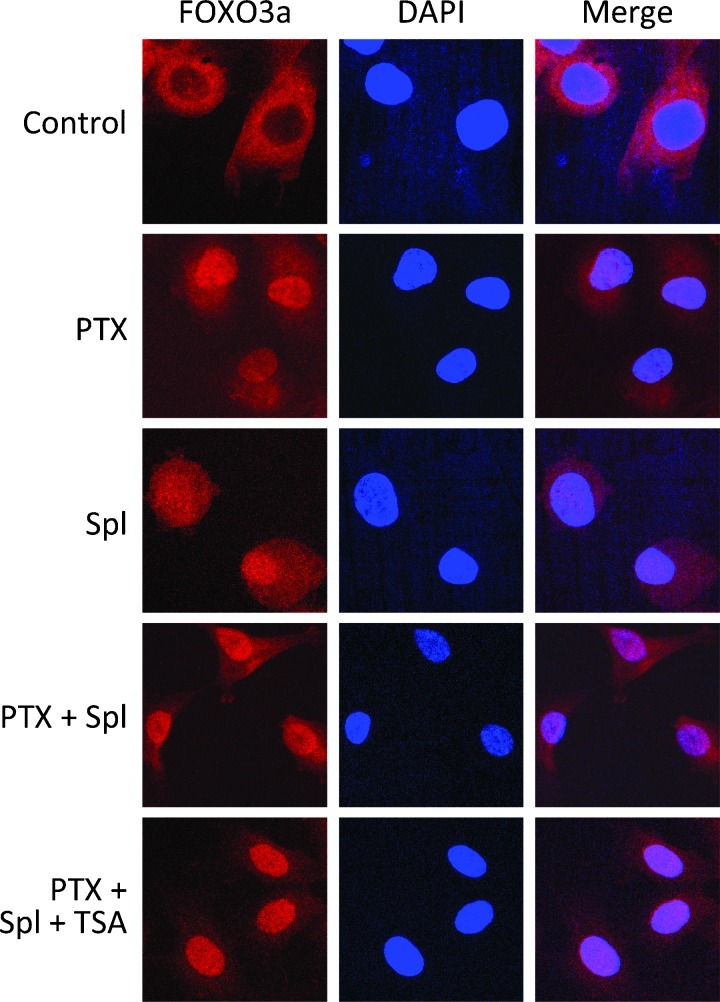
Finally, we investigated the effect of paclitaxel and splitomicin on the transcription factor FOXO3a, a negative regulator of angiogenesis and cell motility. Because the nuclear localization of FOXO3a is an indicator of its activity, we investigated whether paclitaxel and splitomicin affected FOXO3a cellular localization. Immunofluorescence analysis of untreated HUVECs showed FOXO3a mainly in the cytoplasm (Figure 5). After treatment with paclitaxel (for 4 hours, in the same conditions used in the motility assays), FOXO3a showed a predominant nuclear localization. Interestingly, splitomicin too induced translocation of FOXO3a to the nucleus, although some positivity remained in the cytoplasm. After exposure to a combination of paclitaxel and splitomicin, endothelial cells presented a higher localization of FOXO3a in the nucleus, which further increased when TSA was added to the combination (Figure 5).
Figure 5.
Confocal microscopy analysis of the effect of paclitaxel and tubulin deacetylase inhibitors on the localization of FOXO3a in endothelial cells. HUVECs were exposed to paclitaxel (PTX, 10 nM), splitomicin (Spl, 1.2 mM), and TSA (1 µM) for 4 hours, processed, and immunostained for FOXO3a as detailed in Materials and Methods. Scale bar, 10 µm.
Altogether these findings indicate that combination of SIRT2 inhibitors with taxanes increases their anti-motility activity and point to FOXO3a as a major mediator of this effect.
Discussion
Inhibitors of motility can impact on the design of therapies for cell motility-based pathologic processes such as tumor angiogenesis, invasion, and metastasis. In this study, we have demonstrated that the modulation of SIRT2 tubulin deacetylase activity affects cell response to the anti-motility activity of taxanes.
Paclitaxel increases the level of acetylated tubulin in endothelial and tumor cells. Although other studies reported similar findings, this was usually observed at high concentrations and/or long exposure times, often associated to a cytotoxic affect [33]. We provide three lines of evidence indicating that the effect of paclitaxel on tubulin acetylation is associated with inhibition of cell motility rather than proliferation. First, increase in tubulin acetylation is observed in endothelial cells treated with 10 to 30 nM paclitaxel for 4 hours, conditions associated with inhibition of cell motility but not of proliferation. Second, the same inverse association between tubulin acetylation and cell motility is also observed with the taxane IDN5390 that has the same anti-motility activity as paclitaxel but substantially lower cytotoxicity. Third, induction of tubulin acetylation by both paclitaxel and IDN5390 parallels inhibition of cell motility in a tumor model of tubulin-mutated cells resistant to the antiproliferative activity of paclitaxel. Altogether these findings indicate that tubulin acetylation induced by a brief exposure to taxanes reflects their anti-motility activity independently from their cytotoxic activity. Preliminary findings indicate that tubulin acetylation was increased also by the tubulin destabilizer combretastatin (not shown), suggesting that induction of tubulin acetylation might be a feature common to different tubulin-targeting inhibitors of cell motility.
This finding prompted us to investigate whether modulation of tubulin acetylation might affect cell response to the anti-motility activity of taxanes, focusing in particular on the two identified tubulin deacetylases HDAC6 and SIRT2. Our data indicate that SIRT2 also plays an important role in cell motility, as specifically demonstrated by the findings that overexpression of SIRT2 decreased cell motility, whereas down-regulation of SIRT2 (through siRNA) increased cell motility. This differs from the finding of Pandithage et al., who reported an anti-motility activity of SIRT2 in a scratch assay, because of a de-adhesive activity of SIRT2 that caused cell detachment [34]. The experimental conditions used in the present study (three-dimensional migration in the Boyden chamber) are quite different and less dependent on cell adhesion and crawling on the substrate. Moreover, because SIRT2 modifications, such as phosphorylation, are involved in regulating SIRT2 ability to control tubulin acetylation and motility and are regulated in a cell cycle manner, it might be hypothesized that the mechanism and outcome of SIRT2 control on motility could vary depending on stage of the cell cycle, hence justifying different results obtained in different experimental conditions.
The molecular basis for the activity of HDAC6 and SIRT2 in cell motility and in modulating the response to taxanes still needs to be clarified. The straight causal association between tubulin acetylation and motility, initially hypothesized, was apparently confuted by the finding that modulation ofHDAC6 activity by TSA or siRNA strongly affected tubulin acetylation but modestly modulated cell motility, whereas the opposite was observed with modulation of SIRT2. The apparent different potency of HDAC6 on tubulin acetylation and cell motility might depend on additional effects of HDAC6 in this cell type. It should also be considered that, although tubulin acetylation is commonly detected using the 6-11B-1 antibody that recognize acetylated Lys40, additional acetylation sites on tubulin are present [14], which could be differentially regulated by HDAC6 and SIRT2 and modulate motility in these cells.
Both taxanes and inhibitors of histone deacetylases have been reported to affect microtubule dynamic instability. In tumor cells, paclitaxel suppresses microtubule dynamics (reviewed in [3]), although in endothelial cells it surprisingly enhances dynamics at low concentrations compatible with inhibition of cell motility [35]. HDAC6 in melanoma cells regulates microtubule dynamic instability, possibly through the recruitment of kinesin-1 on microtubule and activation of c-Jun N-terminal kinase in the microtubule environment [36]. It has been proposed that enhancement of cell adhesion and inhibition of motility by the histone deacetylase inhibitors TSA and tubacin is because of a decrease in microtubule dynamics that impairs the cells' ability to mediate the focal adhesion dynamics required for cell migration [26]. Therefore, changes in microtubule dynamics might play a relevant role to the inhibition of motility by taxanes and inhibitors of tubulin deacetylases.
The acetylation status of tubulin and tubulin deacetylases might affect several molecular pathways involved in the regulation of cell motility, including microtubule-associated protein (MAP) tau [37], p58 [24], p53, heat shock protein 90 (Hsp90), HOXA10 [38], p53 [39], and the nuclear factor-kappaB (NF-κB) family of transcription factor p65 [40] and cortactin [41]. Some of these molecules, such as NF-κB [42] and Hsp90 [43], are also targeted by taxanes and therefore represent possible convergence points between the pathways affected by the two classes of compounds. Another possible candidate target is FOXO3a, a member of the family of the forkhead transcription factor FOXO, that negatively regulate cell motility [44,45]. We found that paclitaxel and splitomicin, alone and in combination, caused FOXO3a translocation to the nucleus, a requirement for its transcriptional activity. This finding is in agreement with studies showing that paclitaxel causes the translocation of FOXO3a to the nucleus of tumor cells [46]. By deacetylating FOXOs, SIRT1 and SIRT2 repress their transcriptional activity [47,48], preventing their inhibitory activity and stimulating cell motility and angiogenesis. In line with these evidences, our findings indicate that SIRT inhibitors might cooperate with paclitaxel to derepress FOXO3a, restoring its anti-motility activity.
Inhibitors of histone deacetylases are being developed as a new class of antineoplastic agents. Although the exact mechanism of their activity is still unclear, their biologic activities possibly depend on their antiangiogenic effect [47,49,50]. Our finding that SIRT2 regulates endothelial cell motility points to its potential as a new target for antiangiogenic therapies.
The therapeutic use of histone deacetylase inhibitors has been proposed in combination with chemotherapeutic agents, including taxanes [51,52]. Our findings provide a rationale for the use of SIRT2-targeting compounds in new approaches of combination therapies, particularly with taxanes. Our results are in agreement with the described activity of cambinol, an inhibitor of SIRT1 and SIRT2, that enhances the effect of TSA on tubulin acetylation and potentiates the cytotoxicity of PTX on lung cancer [53]. In addition, the farnesyl transferase inhibitor Lonafarnib increases tubulin acetylation and synergizes with paclitaxel, through a mechanism requiring a functional tubulin deacetylase [33], further supporting the connection between modulation of tubulin acetylation and response to taxanes.
In conclusion, this study has demonstrated that inhibition of tubulin deacetylases enhances sensitivity to the anti-motility activity of paclitaxel. Preclinical and clinical findings have already demonstrated that inhibitors of histone deacetylases represent a suitable addition to taxane-based therapies. This study points to the prospect of developing inhibitors of sirtuins as new agents for combination therapies with taxanes to treat motility-driven diseases.
Supplementary Material
Mitotic Index Analysis
Exponentially growing HUVECs were exposed to paclitaxel or IDN5390 for 4 or 24 hours. Cells were then washed with PBS, fixed with cold methanol (20 minutes on ice), and stained with DAPI. At least 400 nuclei per experimental condition were analyzed by a fluorescence microscope (OLYMPUS IX70).
Western Blot Analysis of SIRT2 Expression in Transfected Cells
Lysates of parental and transfected 1A9 cells were electrophoresed on a 10% SDS-PAGE gel and transferred to a nitrocellulose membrane (Schleicher & Schuell). After blocking overnight at 4°C with ECL advance blocking agent, membranes were probed with anti-SIRT2 antibody (1:2000) for 1 hour at room temperature, followed by peroxidase-conjugated anti-chicken IgG (Sigma) and Amersham ECL Plus Western Blotting Detection Reagent (GE Healthcare).
In Vitro Tubulin Deacetylation Assay
Purified recombinant SIRT2-FLAG (0.284 µg) was incubated with tubulin (10 µg; Pure, Cytoskeleton, Denver, CO) with or without IDN5390 or paclitaxel (10–1000 nM) for 2 hours at room temperature, after addition of NAD (1 mM, except in the negative control), essentially as described [1]. Reaction was stopped by adding SDS-PAGE buffer. Samples were analyzed by Western blot with antibodies against acetylated tubulin or total tubulin. Data are expressed as the ratio between optical density values of acetylated tubulin and total tubulin.
Combination Index
CI was calculated as described [2] to determine whether the drugs interacted synergistically, additively, or antagonistically. For each combination of drug concentrations (Dsplitomicin X, Dpaclitaxel X), producing in combination the effect X, CI was calculated as follows: CI = Dsplitomicin X/ICX, splitomicin + Dpaclitaxel X/ICX, paclitaxel, where ICX, splitomicin and ICX, paclitaxel are the concentrations of each individual drug that would produce the effect X if given alone. A confidence band was calculated around each mean using a t distribution at the 90% probability level. Additivity was claimed when the value CI = 1 was inside the confidence band (with the band included in the 0.8–1.2 interval), synergism when the CI with its confidence band was <1, and antagonism when the CI with its confidence band was >1.
Acknowledgments
We thank C. Manzotti from Indena S.p.A. for providing IDN5390 and constructive discussion, Maria Rosa Bani for helpful comments to the manuscript, and S. Gastoldi and F. Sangalli for assistance in confocal microscopy analysis.
Footnotes
This study was supported by grants from the Italian Ministry of Health, contract N.RO Strategici 11/07, the Italian Association for Cancer Research (AIRC), and Fondazione Cariplo. G. Taraboletti and R. Giavazzi received research support from Indena S.p.A. A. Riva is employed by Indena S.p.A. The other authors declare no potential conflict of interest.
This article refers to supplementary materials, which are designated by Figures W1 to W6 and Tables W1 to W3 and are available online at www.neoplasia.com.
References
- 1.Pasquier E, Honore S, Braguer D. Microtubule-targeting agents in angiogenesis: where do we stand? Drug Resist Updat. 2006;9:74–86. doi: 10.1016/j.drup.2006.04.003. [DOI] [PubMed] [Google Scholar]
- 2.Giavazzi R, Bonezzi K, Taraboletti G. Microtubule targeting agents and angiogenesis. In: Fojo T, editor. Microtubules as Targets for Cancer Therapies. Totowa, NJ: Humana Press; 2008. pp. 519–530. [Google Scholar]
- 3.Jordan MA, Kamath K. How do microtubule-targeted drugs work? An overview. Curr Cancer Drug Targets. 2007;7:730–742. doi: 10.2174/156800907783220417. [DOI] [PubMed] [Google Scholar]
- 4.Belotti D, Vergani V, Drudis T, Borsotti P, Pitelli MR, Viale G, Giavazzi R, Taraboletti G. The microtubule-affecting drug paclitaxel has antiangiogenic activity. Clin Cancer Res. 1996;2:1843–1849. [PubMed] [Google Scholar]
- 5.Hayot C, Farinelle S, De Decker R, Decaestecker C, Darro F, Kiss R, Van Damme M. In vitro pharmacological characterizations of the anti-angiogenic and anti-tumor cell migration properties mediated by microtubule-affecting drugs, with special emphasis on the organization of the actin cytoskeleton. Int J Oncol. 2002;21:417–425. [PubMed] [Google Scholar]
- 6.Bijman MN, van Nieuw Amerongen GP, Laurens N, van Hinsbergh VW, Boven E. Microtubule-targeting agents inhibit angiogenesis at subtoxic concentrations, a process associated with inhibition of Rac1 and Cdc42 activity and changes in the endothelial cytoskeleton. Mol Cancer Ther. 2006;5:2348–2357. doi: 10.1158/1535-7163.MCT-06-0242. [DOI] [PubMed] [Google Scholar]
- 7.Ganguly A, Yang H, Cabral F. Class III β-tubulin counteracts the ability of paclitaxel to inhibit cell migration. Oncotarget. 2011;2:368–377. doi: 10.18632/oncotarget.250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Belotti D, Rieppi M, Nicoletti MI, Casazza AM, Fojo T, Taraboletti G, Giavazzi R. Paclitaxel (Taxol®) inhibits motility of paclitaxel-resistant human ovarian carcinoma cells. Clin Cancer Res. 1996;2:1725–1730. [PubMed] [Google Scholar]
- 9.Taraboletti G, Micheletti G, Rieppi M, Poli M, Turatto M, Rossi C, Borsotti P, Roccabianca P, Scanziani E, Nicoletti MI, et al. Antiangiogenic and antitumor activity of IDN 5390, a new taxane derivative. Clin Cancer Res. 2002;8:1182–1188. [PubMed] [Google Scholar]
- 10.Taraboletti G, Micheletti G, Giavazzi R, Riva A. IDN 5390: a new concept in taxane development. Anticancer Drugs. 2003;14:255–258. doi: 10.1097/00001813-200304000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Perdiz D, Mackeh R, Pous C, Baillet A. The ins and outs of tubulin acetylation: more than just a post-translational modification? Cell Signal. 2010;23:763–771. doi: 10.1016/j.cellsig.2010.10.014. [DOI] [PubMed] [Google Scholar]
- 12.Wloga D, Gaertig J. Post-translational modifications of microtubules. J Cell Sci. 2010;123:3447–3455. doi: 10.1242/jcs.063727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Westermann S, Weber K. Post-translational modifications regulate microtubule function. Nat Rev Mol Cell Biol. 2003;4:938–947. doi: 10.1038/nrm1260. [DOI] [PubMed] [Google Scholar]
- 14.Choudhary C, Kumar C, Gnad F, Nielsen ML, Rehman M, Walther TC, Olsen JV, Mann M. Lysine acetylation targets protein complexes and co-regulates major cellular functions. Science. 2009;325:834–840. doi: 10.1126/science.1175371. [DOI] [PubMed] [Google Scholar]
- 15.North BJ, Verdin E. Interphase nucleo-cytoplasmic shuttling and localization of SIRT2 during mitosis. PLoS One. 2007;2:e784. doi: 10.1371/journal.pone.0000784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vaquero A, Scher MB, Lee DH, Sutton A, Cheng HL, Alt FW, Serrano L, Sternglanz R, Reinberg D. SirT2 is a histone deacetylase with preference for histone H4 Lys 16 during mitosis. Genes Dev. 2006;20:1256–1261. doi: 10.1101/gad.1412706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.North BJ, Marshall BL, Borra MT, Denu JM, Verdin E. The human Sir2 ortholog, SIRT2, is an NAD+-dependent tubulin deacetylase. Mol Cell. 2003;11:437–444. doi: 10.1016/s1097-2765(03)00038-8. [DOI] [PubMed] [Google Scholar]
- 18.Dryden SC, Nahhas FA, Nowak JE, Goustin AS, Tainsky MA. Role for human SIRT2 NAD-dependent deacetylase activity in control of mitotic exit in the cell cycle. Mol Cell Biol. 2003;23:3173–3185. doi: 10.1128/MCB.23.9.3173-3185.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Inoue T, Hiratsuka M, Osaki M, Yamada H, Kishimoto I, Yamaguchi S, Nakano S, Katoh M, Ito H, Oshimura M. SIRT2, a tubulin deacetylase, acts to block the entry to chromosome condensation in response to mitotic stress. Oncogene. 2007;26:945–957. doi: 10.1038/sj.onc.1209857. [DOI] [PubMed] [Google Scholar]
- 20.North BJ, Verdin E. Mitotic regulation of SIRT2 by cyclin-dependent kinase 1-dependent phosphorylation. J Biol Chem. 2007;282:19546–19555. doi: 10.1074/jbc.M702990200. [DOI] [PubMed] [Google Scholar]
- 21.Hubbert C, Guardiola A, Shao R, Kawaguchi Y, Ito A, Nixon A, Yoshida M, Wang XF, Yao TP. HDAC6 is a microtubule-associated deacetylase. Nature. 2002;417:455–458. doi: 10.1038/417455a. [DOI] [PubMed] [Google Scholar]
- 22.Zhang Y, Li N, Caron C, Matthias G, Hess D, Khochbin S, Matthias P. HDAC-6 interacts with and deacetylates tubulin and microtubules in vivo. EMBO J. 2003;22:1168–1179. doi: 10.1093/emboj/cdg115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Saunders LR, Verdin E. Sirtuins: critical regulators at the crossroads between cancer and aging. Oncogene. 2007;26:5489–5504. doi: 10.1038/sj.onc.1210616. [DOI] [PubMed] [Google Scholar]
- 24.Haggarty SJ, Koeller KM, Wong JC, Grozinger CM, Schreiber SL. Domain-selective small-molecule inhibitor of histone deacetylase 6 (HDAC6)-mediated tubulin deacetylation. Proc Natl Acad Sci USA. 2003;100:4389–4394. doi: 10.1073/pnas.0430973100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Saji S, Kawakami M, Hayashi S, Yoshida N, Hirose M, Horiguchi S, Itoh A, Funata N, Schreiber SL, Yoshida M, et al. Significance of HDAC6 regulation via estrogen signaling for cell motility and prognosis in estrogen receptor-positive breast cancer. Oncogene. 2005;24:4531–4539. doi: 10.1038/sj.onc.1208646. [DOI] [PubMed] [Google Scholar]
- 26.Tran AD, Marmo TP, Salam AA, Che S, Finkelstein E, Kabarriti R, Xenias HS, Mazitschek R, Hubbert C, Kawaguchi Y, et al. HDAC6 deacetylation of tubulin modulates dynamics of cellular adhesions. J Cell Sci. 2007;120:1469–1479. doi: 10.1242/jcs.03431. [DOI] [PubMed] [Google Scholar]
- 27.Gao YS, Hubbert CC, Lu J, Lee YS, Lee JY, Yao TP. Histone deacetylase 6 regulates growth factor-induced actin remodeling and endocytosis. Mol Cell Biol. 2007;27:8637–8647. doi: 10.1128/MCB.00393-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nolan L, Johnson PW, Ganesan A, Packham G, Crabb SJ. Will histone deacetylase inhibitors require combination with other agents to fulfil their therapeutic potential? Br J Cancer. 2008;99:689–694. doi: 10.1038/sj.bjc.6604557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mai A, Altucci L. Epi-drugs to fight cancer: from chemistry to cancer treatment, the road ahead. Int J Biochem Cell Biol. 2009;41:199–213. doi: 10.1016/j.biocel.2008.08.020. [DOI] [PubMed] [Google Scholar]
- 30.Bedalov A, Gatbonton T, Irvine WP, Gottschling DE, Simon JA. Identification of a small molecule inhibitor of Sir2p. Proc Natl Acad Sci USA. 2001;98:15113–15118. doi: 10.1073/pnas.261574398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Giannakakou P, Sackett DL, Kang YK, Zhan Z, Buters JT, Fojo T, Poruchynsky MS. Paclitaxel-resistant human ovarian cancer cells have mutant beta-tubulins that exhibit impaired paclitaxel-driven polymerization. J Biol Chem. 1997;272:17118–17125. doi: 10.1074/jbc.272.27.17118. [DOI] [PubMed] [Google Scholar]
- 32.Naumova E, Ubezio P, Garofalo A, Borsotti P, Cassis L, Riccardi E, Scanziani E, Eccles SA, Bani MR, Giavazzi R. The vascular targeting property of paclitaxel is enhanced by SU6668, a receptor tyrosine kinase inhibitor, causing apoptosis of endothelial cells and inhibition of angiogenesis. Clin Cancer Res. 2006;12:1839–1849. doi: 10.1158/1078-0432.CCR-05-1615. [DOI] [PubMed] [Google Scholar]
- 33.Marcus AI, Zhou J, O'Brate A, Hamel E, Wong J, Nivens M, El-Naggar A, Yao TP, Khuri FR, Giannakakou P. The synergistic combination of the farnesyl transferase inhibitor lonafarnib and paclitaxel enhances tubulin acetylation and requires a functional tubulin deacetylase. Cancer Res. 2005;65:3883–3893. doi: 10.1158/0008-5472.CAN-04-3757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pandithage R, Lilischkis R, Harting K, Wolf A, Jedamzik B, Luscher-Firzlaff J, Vervoorts J, Lasonder E, Kremmer E, Knoll B, et al. The regulation of SIRT2 function by cyclin-dependent kinases affects cell motility. J Cell Biol. 2008;180:915–929. doi: 10.1083/jcb.200707126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pasquier E, Honore S, Pourroy B, Jordan MA, Lehmann M, Briand C, Braguer D. Antiangiogenic concentrations of paclitaxel induce an increase in microtubule dynamics in endothelial cells but not in cancer cells. Cancer Res. 2005;65:2433–2440. doi: 10.1158/0008-5472.CAN-04-2624. [DOI] [PubMed] [Google Scholar]
- 36.Zilberman Y, Ballestrem C, Carramusa L, Mazitschek R, Khochbin S, Bershadsky A. Regulation of microtubule dynamics by inhibition of the tubulin deacetylase HDAC6. J Cell Sci. 2009;122:3531–3541. doi: 10.1242/jcs.046813. [DOI] [PubMed] [Google Scholar]
- 37.Ding H, Dolan PJ, Johnson GV. Histone deacetylase 6 interacts with the microtubule-associated protein tau. J Neurochem. 2008;106:2119–2130. doi: 10.1111/j.1471-4159.2008.05564.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bae NS, Swanson MJ, Vassilev A, Howard BH. Human histone deacetylase SIRT2 interacts with the homeobox transcription factor HOXA10. J Biochem. 2004;135:695–700. doi: 10.1093/jb/mvh084. [DOI] [PubMed] [Google Scholar]
- 39.Peck B, Chen CY, Ho KK, Di Fruscia P, Myatt SS, Coombes RC, Fuchter MJ, Hsiao CD, Lam EW. SIRT inhibitors induce cell death and p53 acetylation through targeting both SIRT1 and SIRT2. Mol Cancer Ther. 2010;9:844–855. doi: 10.1158/1535-7163.MCT-09-0971. [DOI] [PubMed] [Google Scholar]
- 40.Rothgiesser KM, Erener S, Waibel S, Luscher B, Hottiger MO. SIRT2 regulates NF-κB-dependent gene expression through deacetylation of p65 Lys310. J Cell Sci. 2010;123:4251–4258. doi: 10.1242/jcs.073783. [DOI] [PubMed] [Google Scholar]
- 41.Zhang X, Yuan Z, Zhang Y, Yong S, Salas-Burgos A, Koomen J, Olashaw N, Parsons JT, Yang XJ, Dent SR, et al. HDAC6 modulates cell motility by altering the acetylation level of cortactin. Mol Cell. 2007;27:197–213. doi: 10.1016/j.molcel.2007.05.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bergstralh DT, Ting JP. Microtubule stabilizing agents: their molecular signaling consequences and the potential for enhancement by drug combination. Cancer Treat Rev. 2006;32:166–179. doi: 10.1016/j.ctrv.2006.01.004. [DOI] [PubMed] [Google Scholar]
- 43.Murtagh J, Lu H, Schwartz EL. Taxotere-induced inhibition of human endothelial cell migration is a result of heat shock protein 90 degradation. Cancer Res. 2006;66:8192–8199. doi: 10.1158/0008-5472.CAN-06-0748. [DOI] [PubMed] [Google Scholar]
- 44.Srivastava RK, Unterman TG, Shankar S. FOXO transcription factors and VEGF neutralizing antibody enhance antiangiogenic effects of resveratrol. Mol Cell Biochem. 2010;337:201–212. doi: 10.1007/s11010-009-0300-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhang H, Pan Y, Zheng L, Choe C, Lindgren B, Jensen ED, Westendorf JJ, Cheng L, Huang H. FOXO1 inhibits Runx2 transcriptional activity and prostate cancer cell migration and invasion. Cancer Res. 2011;71:3257–3267. doi: 10.1158/0008-5472.CAN-10-2603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sunters A, Fernandez de Mattos S, Stahl M, Brosens JJ, Zoumpoulidou G, Saunders CA, Coffer PJ, Medema RH, Coombes RC, Lam EW. FoxO3a transcriptional regulation of Bim controls apoptosis in paclitaxel-treated breast cancer cell lines. J Biol Chem. 2003;278:49795–49805. doi: 10.1074/jbc.M309523200. [DOI] [PubMed] [Google Scholar]
- 47.Potente M, Ghaeni L, Baldessari D, Mostoslavsky R, Rossig L, Dequiedt F, Haendeler J, Mione M, Dejana E, Alt FW, et al. SIRT1 controls endothelial angiogenic functions during vascular growth. Genes Dev. 2007;21:2644–2658. doi: 10.1101/gad.435107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zhao Y, Yang J, Liao W, Liu X, Zhang H, Wang S, Wang D, Feng J, Yu L, Zhu WG. Cytosolic FoxO1 is essential for the induction of autophagy and tumour suppressor activity. Nat Cell Biol. 2010;12:665–675. doi: 10.1038/ncb2069. [DOI] [PubMed] [Google Scholar]
- 49.Ellis L, Hammers H, Pili R. Targeting tumor angiogenesis with histone deacetylase inhibitors. Cancer Lett. 2009;280:145–153. doi: 10.1016/j.canlet.2008.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Shim JS, Matsui Y, Bhat S, Nacev BA, Xu J, Bhang HE, Dhara S, Han KC, Chong CR, Pomper MG, et al. Effect of nitroxoline on angiogenesis and growth of human bladder cancer. J Natl Cancer Inst. 2010;102:1855–1873. doi: 10.1093/jnci/djq457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Qian X, LaRochelle WJ, Ara G, Wu F, Petersen KD, Thougaard A, Sehested M, Lichenstein HS, Jeffers M. Activity of PXD101, a histone deacetylase inhibitor, in preclinical ovarian cancer studies. Mol Cancer Ther. 2006;5:2086–2095. doi: 10.1158/1535-7163.MCT-06-0111. [DOI] [PubMed] [Google Scholar]
- 52.Ramalingam SS, Maitland ML, Frankel P, Argiris AE, Koczywas M, Gitlitz B, Thomas S, Espinoza-Delgado I, Vokes EE, Gandara DR, et al. Carboplatin and paclitaxel in combination with either vorinostat or placebo for first-line therapy of advanced non-small-cell lung cancer. J Clin Oncol. 2010;28:56–62. doi: 10.1200/JCO.2009.24.9094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Heltweg B, Gatbonton T, Schuler AD, Posakony J, Li H, Goehle S, Kollipara R, Depinho RA, Gu Y, Simon JA, et al. Antitumor activity of a small-molecule inhibitor of human silent information regulator 2 enzymes. Cancer Res. 2006;66:4368–4377. doi: 10.1158/0008-5472.CAN-05-3617. [DOI] [PubMed] [Google Scholar]
References
- 1.North BJ, Marshall BL, Borra MT, Denu JM, Verdin E. The human Sir2 ortholog, SIRT2, is an NAD+-dependent tubulin deacetylase. Mol Cell. 2003;11:437–444. doi: 10.1016/s1097-2765(03)00038-8. [DOI] [PubMed] [Google Scholar]
- 2.Naumova E, Ubezio P, Garofalo A, Borsotti P, Cassis L, Riccardi E, Scanziani E, Eccles SA, Bani MR, Giavazzi R. The vascular targeting property of paclitaxel is enhanced by SU6668, a receptor tyrosine kinase inhibitor, causing apoptosis of endothelial cells and inhibition of angiogenesis. Clin Cancer Res. 2006;12:1839–1849. doi: 10.1158/1078-0432.CCR-05-1615. [DOI] [PubMed] [Google Scholar]
- 3.Taraboletti G, Micheletti G, Rieppi M, Poli M, Turatto M, Rossi C, Borsotti P, Roccabianca P, Scanziani E, Nicoletti MI, et al. Antiangiogenic and antitumor activity of IDN5390, a new taxane derivative. Clin Cancer Res. 2002;8:1182–1188. [PubMed] [Google Scholar]
- 4.Belotti D, Rieppi M, Nicoletti MI, Casazza AM, Fojo T, Taraboletti G, Giavazzi R. Paclitaxel (Taxol®) inhibits motility of paclitaxel-resistant human ovarian carcinoma cells. Clin Cancer Res. 1996;2:1725–1730. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.