Abstract
Herbal medicines have been widely used all over the world since ancient times and have been recognized by physicians and patients for their better therapeutic value as they have fewer adverse effects as compared with modern medicines. Phytotherapeutics need a scientific approach to deliver the components in a sustained manner to increase patient compliance and avoid repeated administration. This can be achieved by designing novel drug delivery systems (NDDS) for herbal constituents. NDDSs not only reduce the repeated administration to overcome non-compliance, but also help to increase the therapeutic value by reducing toxicity and increasing the bioavailability. One such novel approach is nanotechnology. Nano-sized drug delivery systems of herbal drugs have a potential future for enhancing the activity and overcoming problems associated with plant medicines. Hence, integration of the nanocarriers as a NDDS in the traditional medicine system is essential to conflict more chronic diseases like asthma, diabetes, cancer, and others.
Keywords: Herbal drugs, nanotechnology, novel drug delivery systems
INTRODUCTION
Since ancient time, herbal remedies and natural products are being used to cure the diseases. Unlike widely used allopathic system, the herbal remedies have thousands of constituents that all work simultaneously against the diseases.[1] Phytotherapeutics need a scientific approach to deliver the components in a sustained manner to increase patient compliance and avoid repeated administration. This can be achieved by designing novel drug delivery systems (NDDSs) for herbal constituents. NDDSs not only reduce the repeated administration to overcome non-compliance, but also help to increase the therapeutic value by reducing toxicity and increasing the bioavailability, and so on.[2,3]
Incorporation of the herbal extracts into novel formulation systems have certain added advantages, such as their bulk dosing and less absorption can be overcome which is the major problem being faced, enticing the attention of major pharmaceutical corporations.
Nanotechnology is a field of applied science and technology which aims to develop devices and dosage forms in the range of 1 to 100 nm. The applications of nanotechnology for treatment, diagnosis, monitoring, and control of biological systems have recently been referred to as nanomedicine. The nanocarriers have been made of safe materials, including synthetic biodegradable polymers, lipids, and polysaccharides.
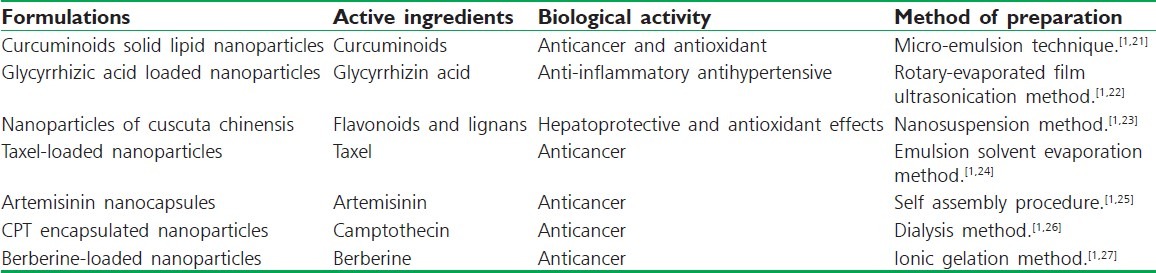
The activity of herbal medicines depends on overall function of a variety of active components, as all the constituents provide synergistic action and thus enhance the therapeutic value. Each active constituent plays an important role and they are all related to each other. However, most of the herbal origin drugs possess insoluble character leading to lower bioavailability and increased systemic clearance requiring repeated administration or higher dose, which makes the drug as a poor candidate for therapeutic use. In phyto-formulation research, developing nano dosage forms (Polymeric Nanoparticles [Nanospheres and Nanocapsules], Liposomes, Proliposomes, Solid Lipid Nanoparticles [SLNs], Nanoemulsion, etc.) has large number of advantages for herbal drugs, including enhancement of solubility and bioavailability, protection from toxicity, enhancement of pharmacological activity, enhancement of stability, improving tissue macrophages distribution, sustained delivery, protection from physical and chemical degradation, etc. Thus, the nano-sized drug delivery systems of herbal drugs have a potential future for enhancing the activity and overcoming problems associated with plant medicines. Hence, integration of the nanocarriers as a NDDS in the traditional medicine system is essential to conflict more chronic diseases like asthma, diabetes, cancer, and others.[1] The various herbal nanoparticles delivery system has been summarized in Table 1.
Table 1.
Some herbal drug nanoparticles
HISTORY AND DEVELOPMENT
Since ancient days, natural products, including plants, have been the basis of treatment of human diseases. The basis of concept of modern medicine development remains rooted in traditional medicine and therapies.[4,5] In different parts of the world like ancient China, Egypt, Africa, America, and India, plants had been used for medicinal purposes long before recorded history. Chemical analysis first became available in the early 19th century which started the extraction and modification of herbal ingredients.[4,6] For a long time, herbal medicines were not considered for development as novel formulations owing to lack of scientific justification and processing difficulties, such as standardization, extraction, and identification of individual drug components in complex polyherbal systems. However, modern phytopharmaceuticals research solves the scientific needs for herbal medicines as in modern medicine, which gives way for developing novel formulations such as nanoparticles, microemulsions, matrix systems, solid dispersions, liposomes, SLNs, and so on. Nanomicellar system,[7] nanotubes,[8] and colloidal nanogels have been developed for curcumin to be used alone as well as in combination with other chemotherapeutic agents like paclitaxel.[1]
NEED FOR NOVEL DRUG DELIVERY SYSTEM “NANO CARRIERS” FOR “HERBAL REMEDIES”
Before reaching to the blood, many constituents of the herbal drugs will be smashed in the highly acidic pH of the stomach and other constituents might be metabolized by the liver. Resultant, the optimum quantity of the herbal drugs may not reach the blood. If the drug does not reach in the optimum amount to the infected region at “minimum effective level,” then there will be no means to show the therapeutic effect of the drug. Nanocarriers applying to herbal remedies will carry optimum amount of the drug to their site of action bypassing all the barriers such as acidic pH of stomach, liver metabolism and increase the prolonged circulation of the drug into the blood due to their small size.[1,9]
Herbal remedies were selected as feasible drug candidate for delivery through a nano delivery system because of the following properties:
Effective chloroform, petrol, acetone, and methanolic extracts are available which may not be suitable for delivery as such.
These are the bulk drugs so dose reduction is intended.
Currently marketed formulations lack target specificity for various chronic diseases.
Some other side effects are associated with currently marketed formulations.
Patient non-compliance due to large doses and less effectiveness with the available formulations.
STRATEGIES OF NANOTECHNOLOGY AS NOVEL DRUG DELIVERY SYSTEM
Drug delivery system fetched a NDDS, a novel approach to overcome the drawbacks of the traditional drug delivery systems.
Nano-sized delivery system was selected because of the following reasons:
They appear to be able to deliver high concentrations of drugs to disease sites because of their unique size and high loading capacities.[1]
Deliver the drug in the small particle size that enhances the entire surface area of the drugs allocating quicker dissolution in the blood.
The concentration seems to persist at the sites for the longer periods.[1]
Shows EPR (enhanced permeation and retention) effect, i.e., enhanced permeation through the barriers because of the small size and retention due to poor lymphatic drainage such in tumor.[1]
Exhibits passive targeting to the disease site of action without the addition of any particular ligand moiety.[1]
Decrease in the side effects.[1]
Decrease in the dose of the drug formulation.[1]
TECHNIQUES
The techniques commonly used for the formulation are:
High-pressure homogenization method
In this method, the lipid is pushed with high pressure (100 to 2 000 bar) through a very high shear stress, which results in disruption of particles down to the submicrometer or nanometer range. High-pressure homogenization method is a very reliable and powerful technique for the large-scale production of nanostructured lipid carriers, lipid drug conjugate, SLNs, and parenteral emulsions.[10,11]
Complex coacervation method
This is a spontaneous phase separation process of two liquid phases in colloidal systems, which results by the interaction of two oppositely charged polyelectrolytes upon mixing in an aqueous solution.[10]
Co-precipitation method
This method is a modification of the complex coacervation method for the preparation of nanoscale core-shell particles. This method has been reported to provide good dispersion stability to poorly water-soluble drugs.[10]
Salting-out method
This method is based on the phenomenon that the solubility of a non-electrolyte in water is decreased upon addition of an electrolyte.[10]
Nanoprecipitation method or solvent displacement method
This method is based on interfacial deposition of a polymer after displacement of a semipolar solvent miscible with water from a lipophilic solution, thereby resulting in a decrease in the interfacial tension between the two phases, which increases the surface area with a subsequent formation of small droplets of organic solvent even without any mechanical stirring.[10,12]
Solvent emulsification–diffusion method
The method involves preparation of an o/w emulsion using oil phase containing polymer and oil in an organic solvent, which is emulsified with the aqueous phase, containing stabilizer, in high shear mixer, followed by addition of water to induce the diffusion of organic solvent, thus resulting in formation of nanoparticles.[10]
Supercritical fluid methods
This method can be used to prepare submicrometer-sized and nano-sized formulations. A supercritical fluid (SCFs) can either be a liquid or gas and used above its thermodynamic critical point of temperature and pressure. The most commonly used SCFs are carbon dioxide and water.[10,13]
Self-assembly methods
Self-assembly is the physical process wherein pre-existing disordered components, atoms, or molecules organize themselves into regulated nanoscale structures by physical or chemical reactions without any contribution from any external source.[10]
TYPES OF NANOPHARMACEUTICALS
Polymeric nanoparticles
Solid lipid nanoparticles
Magnetic nanoparticles
Metal and inorganic nanoparticles
Quantum dots
Polymeric micelles
Phospholipids micelles
Colloidal nano-liposomes
Dendrimers
RECENT DEVELOPMENT
The nanoparticles have come forward as the capable approach in drug delivery systems for the well-organized delivery of drugs utilized in the treatment of various diseases such as cancer by crossing the reticuloendothelial system, enhanced permeability and retention effect, and tumor-specific targeting.
Recently, pharmaceutical scientists have shifted their focus to designing a drug delivery system for herbal medicines using a scientific approach. Cuscuta chinensis is a commonly used traditional Chinese medicine to nourish the liver and kidney. Due to the poor water solubility of its major constituents such as flavonoids and lignans, its absorption upon oral administration could be limited. So, the nanoparticles for the same were developed.[1,14] A recent experimental study of polylactic acid nanoparticles of lipophilic anti-cancer herb drug (Cucurbitacins and Curcuminoids) using a precipitation method have been developed.[1,15] Work has also been carried out in the development and characterization of SLNs for the traditional Chinese medicine for their targeted delivery and increased bioavailability and efficacy.[1,16] In the recent years, nanostructured carrier system like polymeric nanoparticles, liposomes, SLNs, polymeric micelles, nanoemulsions, etc., have been investigated for their potential to deliver anticancer drugs by oral route.[1,17,18] Moreover, the oral route offers great potential for delivery of cytotoxic agents and therefore the attention has focused on the development of oral chemotherapy in oncology.[1,19,20]
TOXICITY ISSUES
Although nanopharmaceuticals may promise endless opportunities in the field of drug delivery for the diagnosis and treatment of various diseases, their safety should not be ignored.[10]
The change in the physicochemical and structural properties of engineered nano-sized materials with a decrease in size could be responsible for a number of material interactions that could lead to toxicological effects. At present, scientists must accept that it is still very early in the toxicological evaluation for nanomaterials and nanomedicines, and there are only few data on the safety and toxicity.
FUTURE PROSPECTIVE
All over the world, the research has been going on herbal remedies and natural products. The development of herbal remedies in the drug delivery system in a number of institutes is being carried out at basic and clinical trial levels. The only requirement is to develop the better systems for the proper delivery of such drugs at the sites and in the whole body in the doses which will not compromise with the existing treatment. Something that would not only give relieve from side effects like toxicity and hypersensitive reactions but also will increase the patient's strength from inside is very much desirable. In the future, the concept of herbal nanoparticles for cancer drug delivery may also fascinate some potential research groups and potentially create attention-grabbing results.
Hence, using “herbal remedy” in the nanocarriers will increase its potential for the treatment of various chronic diseases and health benefits. Many successful examples with experienced evidences are present among us in the direction of nano research. Herbal remedies are also prosperous resources of advantageous compounds holding antioxidants and constituents that can be made use in purposeful foods.[28] This type of collaborative research among the traditional “Herbal remedies” and newer approaches of modern drug delivery system, i.e., “Nanotechnology” has established the attractive therapies to the pharmaceutical in near future that will enhance health of people. It is anticipated that the effectual and valuable relevance of the natural products and herbal remedies being applied with the nanocarrier will enhance the significance of existing drug delivery systems.[1]
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
REFERENCES
- 1.Yadav D, Suri S, Choudhary AA, Sikender M, Hemant, Beg NM, et al. Novel approach: Herbal remedies and natural products in pharmaceutical science as nano drug delivery systems. Int J Pharm Tech. 2011;3:3092–116. [Google Scholar]
- 2.Singh RP, Singh SG, Naik H, Jain D, Bisla S. Herbal excipients in novel drug delivery system. Int J Comprehensive Pharm. 2011;2:1–7. [Google Scholar]
- 3.Sungthongjeen S, Pitaksuteepong T, Somsiri A, Sriamornsak P. Studies on Pectins as Potential Hydrogel Matrices for Controlled-Release Drug Delivery. Drug Develop Ind Pharm. 1999;25:1271–6. doi: 10.1081/ddc-100102298. [DOI] [PubMed] [Google Scholar]
- 4.Sharma AT, Mitkare SS, Moon RS. Multicomponent herbal therapy: A review. Int J Pharm Sci Rev Res. 2011;6:185–7. [Google Scholar]
- 5.Patwardhan B, Vaidya AD, Chorghade M. Ayurveda and natural products drug discovery. Curr Sci. 2004;86:789. [Google Scholar]
- 6.Currier SJ, Johnston PD, Gorelick KJ. Complementary and Alternative Medicine-Herbal Medicines. Sci Med. 2000;7:40–3. [Google Scholar]
- 7.Bisht S, Feldmann G, Soni S, Ravi R, Karikar C, Maitra A, et al. Polymeric nanoparticle-encapsulated curcumin (“nanocurcumin”): A novel strategy for human cancer therapy. J Nanobio. 2007;5:1–18. doi: 10.1186/1477-3155-5-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zheng L, Song JF. Curcumin multi-wall carbon nanotubes modified glassy carbon electrode and its electrocatalytic activity towards oxidation of hydrazine. Sens Actuators B Chem. 2009;135:650–5. [Google Scholar]
- 9.Bairwa NK, Sethiya NK, Mishra SH. Protective effect of stem bark of Ceiba pentandra Linn. against Paracetamol-induced hepatotoxicity in Rats. Pharmacognosy Res. 2010;2:26–30. doi: 10.4103/0974-8490.60584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sahni JK, Baboota S, Ali J. Promising Role of Nanopharmaceuticals in Drug Delivery. Pharma Times. 2011;43:16–8. [Google Scholar]
- 11.Mueller RH, Maeder K, Gohla S. Solid lipid nanoparticles (SLN) for controlled drug delivery – a review of the state of the art. Eur J Pharm Biopharm. 2000;50:161–77. doi: 10.1016/s0939-6411(00)00087-4. [DOI] [PubMed] [Google Scholar]
- 12.Fessi H, Puisieux F, Devissaguet JP, Ammoury N, Benita S. Nanocapsule formation by interfacial polymer deposition following solvent displacement. Int J Pharm. 1989;55:R1–4. [Google Scholar]
- 13.Jung J, Perrut M. Particle design using supercritical fluids: Literature and patent survey. J Supercrit Fluids. 2001;20:179–219. [Google Scholar]
- 14.Yen FL, Wu TH, Lin GT, Cham TM, Lin CC. Nanoparticles formulation of Cuscuta chinensis prevents acetaminophen-induced hepatotoxicity in rats. Food Chem Toxicol. 2008;46:1771–7. doi: 10.1016/j.fct.2008.01.021. [DOI] [PubMed] [Google Scholar]
- 15.Zhang JF, Hou SX, Liu HL. Comparison of preparing two polylactide nanoparticles loaded lipophilic anti-cancer herb drug by nanoprecipitation method. Zhongguo Zhong Yao Za Zhi. 2007;32:303–6. [PubMed] [Google Scholar]
- 16.Li Y, Dong L, Jia A, Chang X, Xue H. Preparation and characterization of solid lipid nanoparticles loaded traditional chinese medicine. Int J Biol Macromol. 2006;38:296–9. doi: 10.1016/j.ijbiomac.2006.03.006. [DOI] [PubMed] [Google Scholar]
- 17.Robinson JR. Introduction: semi-solid formulations for oral drug delivery. Bull Tech Gattefosse. 1996;89:11–3. [Google Scholar]
- 18.Aungst BJ. Novel formulation strategies for improving oral bioavailability of drugs with poor membrane permeation or presystemic metabolism. J Pharm Sci. 1993;82:979–87. [PubMed] [Google Scholar]
- 19.DeMario MD, Ratain MJ. Oral chemotherapy: rationale and future directions. J Clin Oncol. 1998;16:2557–67. doi: 10.1200/JCO.1998.16.7.2557. [DOI] [PubMed] [Google Scholar]
- 20.Pouton CW. Formulation of self-emulsifying drug delivery systems. Adv Drug Del Rev. 1997;25:47–58. [Google Scholar]
- 21.Mukerjee A, Vishwanathan JK. Formulation, characterization and evaluation of curcumin-loaded PLGA nanospheres for cancer therapy. Anticancer Res. 2009;29:3867–75. [PubMed] [Google Scholar]
- 22.Hou J, Zhou SW. Formulation and preparation of glycyrrhizic acid solid lipid nanoparticles. ACTA. 2008;30:1043–5. [Google Scholar]
- 23.Yen FL, Wu TH, Tzeng CW, Lin LT, Lin CC. Curcumin nanoparticles improve the physicochemical properties of curcumin and effectively enhance its antioxidant and antihepatoma activities. J Agric Food Chem. 2010;58:7376–82. doi: 10.1021/jf100135h. [DOI] [PubMed] [Google Scholar]
- 24.Li D, Zhong X, Zeng Z, Jiang J, Li L, Zhao M, et al. Application of targeted drug delivery system in Chinese medicine. J Control Rel. 2009;138:103–12. doi: 10.1016/j.jconrel.2009.05.008. [DOI] [PubMed] [Google Scholar]
- 25.Chen Y, Lin X, Park H, Greever R. Study of artemisinin nanocapsules as anticancer drug delivery systems Nanomedicine: Nanotechnology. Biol Med. 2009;5:316–22. doi: 10.1016/j.nano.2008.12.005. [DOI] [PubMed] [Google Scholar]
- 26.Min KH, Park K, Kim YS, Bae SM, Lee S, Jo HG, et al. Hydrophobically modified glycol chitosan nanoparticles-encapsulated camptothecin enhance the drug stability and tumor targeting in cancer therapy. J Control Release. 2008;127:208–18. doi: 10.1016/j.jconrel.2008.01.013. [DOI] [PubMed] [Google Scholar]
- 27.Lin AH, Li HY, Liu YM. Preparation and release characteristics of berberine chitosan nanoparticles in vitro. China Pharm. 2007;18:755–7. [Google Scholar]
- 28.Sethiya NK, Trivedi A, Patel MB, Mishra SH. Comparative pharmacognostical investigation on four ethanobotanicals traditionally used as Shankhpushpi in India. J Adv Pharm Tech Res. 2010;1:388–95. doi: 10.4103/0110-5558.76437. [DOI] [PMC free article] [PubMed] [Google Scholar]


