Abstract
Background/objectives
To develop an online patient education resource for use in spinal cord injury rehabilitation.
Participants
The development process involved more than 100 subject-matter experts (SMEs) (rehabilitation professionals and consumers) from across Canada. Preliminary evaluation was conducted with 25 end-users.
Methods
An iterative development process was coordinated by a project team; SMEs (including patients) developed the content in working groups using wiki-based tools. Multiple rounds of feedback based on early prototypes helped improve the courses during development.
Results
Five courses were created, each featuring more than 45 minutes of video content and hundreds of media assets. Preliminary evaluation results indicate that users were satisfied by the courses and perceived them to be effective.
Conclusions
This is an effective process for developing multimedia patient education resources; the involvement of patients in all parts of the process was particularly helpful. Future work will focus on implementation, integration into clinical practice and other delivery formats (smart phones, tablets).
Keywords: Disability, Patient education, Rehabilitation, Physical, Spinal cord injuries
Introduction
Effective patient education is a critical part of rehabilitation for people with spinal cord injury (SCI). Providing patients with the information they need to care for themselves can help prevent or minimize secondary complications over time. However, two key barriers can limit the effectiveness of patient education initiatives: staff availability and patient readiness.
Rehabilitation professionals value the spontaneous opportunities for one-on-one patient education that arise in the course of their clinical practice, but patient care workloads and staffing shortages can allow staff very little time for education.1 Furthermore, average length of stay (LOS) in SCI rehabilitation has declined substantially over the past three decades. This has increased the necessity of patient education even as it has reduced the time available.2 Reduced LOS limits the time during which spontaneous, ad hoc education opportunities occur; there is no indication that this reduction in spontaneous learning opportunities has been offset by a substantial increase in formal education programs. As a result, people may be discharged before they can master self-care skills.3–6 Patient readiness can be an additional barrier to effective education during rehabilitation. SCI is a difficult, life-changing transition with great emotional impact, and patients may at times be unready to take up the challenge of learning new information. Patients show different levels of readiness, which are likely to depend on factors like age at injury, level of injury, and time since injury, as well as other personal characteristics. Effective patient education needs to take into account these factors of readiness, and provide different kinds of educational support to accommodate different learning styles at different stages of rehabilitation.7
Letts et al.8 suggest that patients might require more direction early on and become more self-directed over time. Certain topics, such as those related to body functioning, may be appropriate early on in the rehabilitation process, while others (e.g. related to community integration) may best be introduced at later time periods.9
There is no evidence that current patient education practices in SCI rehabilitation are substantially different from when LOS was substantially longer than now. Typically, there is some combination of print resources (brochures, binders) and classroom instruction, complemented by informal one-on-one learning opportunities with rehabilitation professionals. However, there is little information available for gauging the relative effectiveness of these approaches and it is uncertain what other approaches might better equip individuals to better manage their health post-SCI. The effectiveness of patient education could be increased if patient education resources were available where and when they are needed, in an accessible and appealing format.
E-learning in patient education
E-learning is the application of information technology to education. It has the potential to improve the effectiveness and reach of education initiatives while reducing costs. E-learning has been used as an effective tool for educational delivery in corporate and healthcare environments. In corporate settings, e-learning has been widely adopted for staff training. In healthcare, e-learning is well established as a sound approach for medical education10 and is also used in staff training, particularly for compliance-related topics. In patient education, applications of e-learning are more commonly found in larger disease populations. Studies have demonstrated improved outcomes in both diabetes and breast cancer.11,12 By bringing information to the patient at the place and time of their choosing, e-learning has the potential to broaden the reach of existing services and is a promising intervention for outpatients.13 It is possible that e-learning could be an effective means of delivering patient education to people with SCI both in the rehabilitation setting and in the community. It is well documented that the internet is a preferred means of accessing information for people with SCI,8,14–18 and one study demonstrated that a single viewing of an e-learning program on pressure ulcer prevention can improve knowledge.19
E-learning can be used to create engaging learning experiences. The use of multiple media can lead to higher perceived usefulness and improved user concentration.20 In addition, presentations combining text and spoken word are more highly valued by users than those containing only text.3,21
Many SCI rehabilitation programs offer print-based resources and classes, but these both have important limitations.3 E-learning offers the possibility of educational interventions that are more engaging and effective than print resources, and more widely accessible than classes. Adult learners often have a preference for digital media,22 and e-learning presentations can be tailored to fit their attention span and visual orientation. E-learning gives learners the ability to control the experience.23 This interactivity enhances learner engagement and improves learning effectiveness.24
Designing e-learning interventions
When designing educational interventions that target adults with SCI, it is important to be informed by adult learning theory.25 Autonomy is a key characteristic of adult learners, and patient education programs must enhance patient autonomy and empowerment in order to facilitate self-directed care.26,27 This means creating learning experiences that can be self-directed, which is consistent with the development of self-management skills. Different patients have different learning styles, and require appropriate learning strategies;28,29 therefore, the design of education interventions must take into account the differences among learners and engage more than one learning style.
The changing needs of patients across different settings require a variety of methods and messengers, e.g. different media and modes of instruction.8 Rather than a single mode of instruction or an uncoordinated mix of methods, the use of multiple methods in structured format has been shown to enhance the effectiveness of patient education.30 For the purposes of SCI rehabilitation, a blended model of instruction is the best option, combining e-learning and other resources with in-person instruction.24 One user requirement is of particular note: patients want to see real depictions of peers in educational programs rather than actors or healthcare professionals, as the latter lack credibility.31 A study of YouTube videos designed to support self-management in SCI showed that viewers found content more accessible when they were able to view a peer doing the task they wished to accomplish.32
Objectives
The purpose of this study is four-fold:
provide the background and rationale for the development and evaluation of an innovative patient education resource using a new technological approach;
characterize the developmental process used to create the SCI-U courses;
describe the main features of the courses themselves;
present the preliminary results of an evaluation, focusing on usability and perceived effectiveness.
Methods
SCI-U was conceived of from the outset as a collaboration given the need to engage participants from across the continuum of care. Partnerships were formed with healthcare organizations providing inpatient SCI rehabilitation in Ontario (Toronto Rehab, now part of University Health Network) and Alberta (Glenrose and Foothills Hospitals). These organizations agreed to make an in-kind contribution of the time and expertise of their clinical staff, who participated in content development working groups. These partners also subsequently supported the usability testing and evaluation of the courses.
In order to access expertise on community integration, we partnered with the Canadian Paraplegic Association Ontario (CPA Ontario), a community service organization serving people living with SCI. Community service workers participated in the working groups, as did some peer support staff (who are typically people with SCI). In addition, this organization helped identify people with SCI for recruitment as content working group members (to contribute their expertise about living with SCI), video presenters and testimonial subjects.
Finally, we partnered with the Lawson Health Research Institute in London, Ontario, for the evaluation component of the project, focusing on the first three courses.
Design
The target audience for the courses is people who live with SCI, particularly in the first 1 to 2 years after injury. There are also several secondary audiences who could benefit from the courses: family members, caregivers, and health care professionals. The goal was to support self-management by providing information and developing problem-solving skills.
A needs assessment was performed in order to inform planning for several patient education initiatives including SCI-U. Eighty-three consumers and 99 clinicians and staff from Toronto Rehab and CPA Ontario participated in the survey. Common issues and themes were identified (Tables 1 and 2), and this informed the choice of topics for SCI-U courses.
Table 1.
Most important topics on which people with SCI require information
| Topic | Ranking by consumers | Ranking by staff |
|---|---|---|
| Body functioning | 3.68 | 2.72 |
| Community services and resources | 4.05 | 3.92 |
| General health and wellness | 4.14 | 4.1 |
| Emotional adjustment | 4.47 | 2.54 |
| Recreation and community integration | 4.59 | 5.66 |
| Research | 4.86 | 7.13 |
| Equipment | 5 | 4.02 |
| Education and career | 5.21 | 5.92 |
Topics ranked by importance (1 = most important; 8 = least important)
Table 2.
Most important issues on which people with SCI require information
| Issue | Reponses by consumers | Responses by staff |
|---|---|---|
| Options/choice of equipment | 72 | 41 |
| Update on research | 65 | 43 |
| Bowel and Bladder | 59 | 32 |
| Recreation options | 55 | 57 |
| Education and employment services | 49 | 48 |
| Caregiver adjustment and support* | 41 | 37 |
| Nutrition | 37 | 27 |
| Health promotion | 28 | 15 |
| Physical aspects of SCI | 25 | 23 |
| Access to information and research | 18 | 7 |
Most frequent responses (percentage of respondents)
*Identified as an issue for family members
To help publicize the project and encourage uptake, a brand was developed, including a name, a logo and a motto (“For healthy living”). The program was called Spinal Cord Injury University, or SCI-U.
A rapid e-learning authoring application called Articulate was used to produce the courses. One benefit of courses produced with Articulate is the clean, attractive, and professional-looking user interface that frames the content on the screen and allows the user to navigate and control the courses. The choice was made to allow (indeed, encourage) users to navigate freely within the courses, rather than forcing them to view the content in a prescribed sequence.
The need to provide visual representations of key concepts was addressed by developing a library of more than 200 icons, using symbolic or stylized representations. The icons can be used to designate complicated terms (“autonomic dysreflexia” is represented by a spiking blood pressure gauge) or sensitive issues (“bowel accident” is indicated by a large exclamation point superimposed on a stylized pair of buttocks). These icons are useful for visual reinforcement and way finding within the courses.
Development process
The SCI-U courses were produced using a four-step development process as shown in Fig. 1: content specification, content development, production and population, and finally, review and revision. Developing multimedia education resources is complex, time-consuming, and expensive, and requires the coordination of many stakeholders.33,34 Typically, the expertise of varied disciplines is required, from medical research and script writing to instructional design and video production.23 The development process was designed to facilitate the collaboration of these different contributors.
Figure 1.

Process map of SCI-U development. The SCI-U course topics for phase 1 were defined by the Steering Committee and Project Team following a formal needs assessment. The first three courses in the series were defined as SCI and You, Bladder and Bowel. Separate working groups (composed of SMEs, consumers, and project team members) were created for content development in each of the courses. After finalization and medical review of the course script, multimedia elements were developed and then populated into the software tool used to complete the online course. Results from usability testing and formal evaluation were used to modify or revise the course content.
The project was governed by a steering committee with senior-level representatives of the partner organizations who met initially to agree on resource commitments and choose course topics. The day-to-day work of the project was coordinated by a project team including project staff (lead, project manager, and art director) and representatives from key partner organizations. The project team met on a weekly basis throughout the project, over a period of 12 months.
Content development was undertaken by working groups, one for each course, comprising subject-matter experts (SMEs) of various kinds: researchers, clinical and community service staff, and consumers. Project team members led the working group meetings and facilitated collaboration between working group members. Teams met concurrently on-site at the TRI/UHN Lyndhurst Centre (where rehabilitation and community service professionals are co-located) and virtually, using a web-conferencing service to permit cross-country participation.
Multimedia production and population of multimedia assets into the finished courses was undertaken by the project team, engaging the skills of specialists as required (video camera and teleprompter, postproduction, etc). Video presenters were selected and coached, then filmed as they read the script from a teleprompter (essential because of the long, detailed script).
Review and revision was the last stage of the development process and incorporated quality control, usability testing and medical review.
Testing and improvement
Course development incorporated continuous testing at all stages. During content development, the use of a wiki-based collective authoring application (PBWorks) enabled working group members to respond to each others' contributions as the script was in development. At the outset and several times during the production and population phases, design options were evaluated by team members and project participants using rapid prototyping.
A beta version of the first course (containing the first section and a few quiz questions and tabs) was produced for early-stage usability testing, looking in particular at issues of accessibility and interface design with a person with high-level tetraplegia, and ease of understanding with a non-native English speaker.
Each course underwent medical review twice during the development process. Before shooting the presenter video, each script was reviewed to ensure accuracy, conformity with best evidence and comprehensiveness. A second round of medical review followed the production of each course, focusing in particular on the illustrations, photos, and other visual elements.
Evaluation
The evaluation plan for this study involved three components:
Early development usability testing: An initial heuristic evaluation conducted using a mid-level Think Aloud technique to identify usability problems in the user interface during the first iterative development cycle.35 This was conducted by the project lead and involved having end users (n = 2) “walk through” various early prototypes while describing in detail their perceptions of the usability and design of the interface.
Perceived utility and satisfaction: A custom-designed survey, called the PUMPS (perceived utility measure and participant satisfaction) tool, was administered closely after participant review of the module following the initial development cycle. This tool examined participant perceptions using a 5-point Likert scale to indicate degree of agreement to specific statements along four domains ((1) general satisfaction, (2) effectiveness (i.e. degree to which users felt this could assist in their health management), (3) design (ease of use, features, engagement), and (4) personal relevance). Survey items were adapted from a tool used for the Information Literacy e-learning Modules Project36 and included statements such as, “colour was used effectively”; “language was concise and clearly written”; and “the module was easy to navigate”. Scores were summed and overall means were calculated within each domain.
Knowledge acquisition and retention: Participants were asked to complete a brief pre–post set of questions of a similar format (multiple-choice) but with slightly altered content as those within the e-learning courses. As this study focuses on the developmental aspects of SCI-U, this aspect of the evaluation will be described in a subsequent study.
Ethics approval for the evaluation of SCI-U was obtained from the University of Western Ontario. The evaluation focused on the first three modules that were developed: SCI and You, Bladder, and Bowel.
Three separate groups of participants were recruited for the evaluation: persons with an SCI (n = 10), persons naive to SCI (n = 10), and clinicians with experience in caring for persons with SCI (n = 5). Inclusion/exclusion criteria were as broad as possible to mirror the potential eventuality of any person sustaining an SCI. Persons with SCI could have either traumatic or non-traumatic SCI, including damage to the cauda equina, although were required to have sufficient limb function or access to assistive technologies to enable successful navigation of the courses. Persons with SCI or clinicians were required to have a minimum of 6 months “experience” in dealing with SCI. Persons naive to SCI were not permitted to have exposure to SCI, whether through direct experience, education, or practice, including having a friend or family member with SCI.
As this study represents a preliminary report of evaluation results, the data are presented across these groups for only those participants completing all aspects of the study (i.e. 7 SCI, 8 naïve, 4 clinicians, for a total of 19 participants).
Results
By using the development process shown in Fig. 1, the project team was able to coordinate the activities of multiple participants to create five courses (the first three were evaluated). The first, called “SCI and You,” is an introduction to the physical and emotional effects of SCI and an orientation to the rehabilitation process. The next three (called “Bladder,” “Bowel” and “Skin”) cover important aspects of body function and self-care. The last course (“Nutrition”) gives practical information on healthy eating to prevent the secondary consequences of SCI.
Each course contains approximately 15 “slides” arranged into three sections. Each slide covers a specific issue, and features a video presenter who delivers the text (Fig. 2). At the same time, visual elements (illustrations, photos, and animations) illustrate and reinforce the material, while a bullet-point summary highlights key points from the spoken script. Slides typically last from 30 seconds to 2 minutes.
Figure 2.
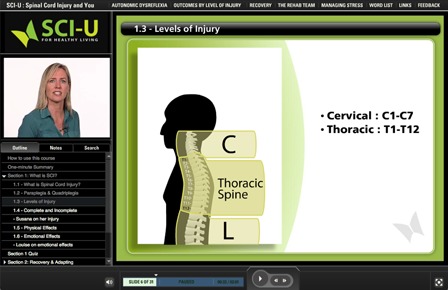
Screenshot of the “Spinal Cord Injury & You” course.
In addition to the didactic material contained in the slides, each course includes a number of tabs, which provide detailed information users may want to refer to (a word list, a recipe video or a how-to guide for a self-care activity like digital stimulation). Every course contains a word list tab, which opens an illustrated searchable glossary of key terms. In addition, all slides have a searchable text of the presentation script in the “Notes” section.
Following each section is a quiz, designed to recapitulate important material and reinforce learning, rather than evaluate it (see example list of quiz questions in Table 3).
Table 3.
Representative quiz questions from SCI-U
| Questions | Answers |
|---|---|
| SCI and You | |
| 1. Please match the following words with the Right definitions: | - Loss of movement and sensation in the upper AND lower body |
| - Quadriplegia (or Tetraplegia) | - Loss of movement and sensation affecting the lower body ONLY |
| - Paraplegia | |
| 2. During rehab you should set your goals according to: | a. Your values and goals in life |
| b. Media images of people with SCI | |
| (Choose the one best answer) | c. The progress you see other people making |
| d. What your family thinks you should do | |
| Bladder | |
| 1. Arrange the steps involved in problem solving. | 1. Identify the problem |
| 2. Gather information | |
| (Drag and drop in the correct order) | 3. List possible solutions |
| 4. Try a solution and evaluate results | |
| 5. Know when to ask for help | |
| 2. Which of the following signs may indicate that you have a urinary tract infection? | a. Your muscle spasms and muscle tone increase |
| (Choose all three correct answers) | b. You have constipation |
| c. Your urine is smelly, cloudy or dark | |
| d. You have fever, chills or fatigue | |
| Bowel | |
| 1. After a spinal cord injury, what are the goals of your bowel program? | a. Empty your bowel completely at a predictable time |
| (Choose both of the correct answers) | b. Never change the way you do your bowel program |
| c. Prevent accidents and complications | |
| d. Have the same bowel program as everyone else | |
| 2. What are some ways you can prevent constipation? | a. Get more exercise |
| b. Eat foods that contain probiotics | |
| (Choose all three correct answers) | c. Drink plenty of water |
| d. Cut down on fibre | |
Note: Correct answers shown in bold
The material in each course is delivered by video presenters, who are all people living with SCI (each section has a different presenter); this enhances credibility. Special efforts were made to select video presenters and testimonial subjects who reflect the diversity found in the SCI community, with respect to injury level and time since injury, as well as other demographic characteristics (age, sex, cultural background). In addition to the video presenters, there is a video host for SCI-U overall: a professional TV journalist and presenter who introduces and summarizes each course, and helps users navigate between parts of the course.
The SCI-U courses are very content-rich and media-rich. Each course contains more than 45 minutes of original audiovisual content, with hundreds of illustrations, animations, photos, and videos. The large number of media assets helps make the courses engaging and visually appealing.
The extensive use of custom-developed illustrations and animations makes it possible to depict things that would be too costly or impossible to film; they can show cutaway views, blowups and other representations that are useful when showing anatomical features. Illustrations and animations can be made as explicit as is required for educational purposes while remaining tasteful and pleasant to view.
Another important feature of each course is a set of 25 “testimonials;” video clips running for about 2–3 minutes each in which people living with SCI discuss their real-world experiences in a way that reinforces the points covered in the presentation (see list of topics in Table 4). Each course features three to five testimonials, which discuss particular topics and are placed immediately following the slides where those topics are introduced.
Table 4.
Testimonial topics from SCI-U
| SCI and You |
| Physical and sensory effects of SCI |
| Incomplete vs. complete |
| Starting rehabiitation and transitioning |
| Emotional effects of SCI |
| Communication with family and friends |
| Career changes |
| Tough questions, e.g. finances, physical recovery |
| Moving forward with relationships |
| Life after rehabilitation |
| Bladder |
| Catheterizing in a public place |
| Using good technique and cleanliness |
| Prevention and management of bladder and urinary tract infections |
| Developing PARTnerships and working with your healthcare providers |
| Bowel |
| Challenges of adapting following SCI |
| Transitioning from the rehab faciity to the community |
| Choosing a commode |
| Building a bowel routine and maintenance |
| Sensations/pressure |
| Importance of diet |
| Dealing with accidents and problems, e.g., hemorrhoids |
| Problem solving |
PART, prepare – ask – repeat – take action.
Preliminary evaluation
To date, preliminary evaluation data are available for participant perceived utility and satisfaction, and average time to completion for the three courses undergoing evaluation. These initial results are based on data captured through the PUMPS tool with average time to completion being measured by participant self-report as an item within. For the SCI & You course, average time to completion across all participants was 47.5 minutes; 39.4 minutes for the Bladder course; and 42.0 minutes for the Bowel course.
Preliminary domain scores from the PUMPS tool (i.e. satisfaction, effectiveness, personal relevance, design) averaged across participants are shown in Fig. 3.
Figure 3.

Preliminary evaluation results. Overall mean domain scores for perceived utility and satisfaction. Scores of 5 would indicate the highest possible level of agreement with statements associated with (A) general satisfaction, (B) effectiveness, (C) personal relevance and (D) design and usability. Scores related to each of the three modules are indicated on the vertical axis. Note: relevance and effectiveness scores reflect data only from the consumer participant group whereas satisfaction and design scores are comprised of data from the consumer, naïve-user, and clinician groups.
Participants were provided a free-text area and asked to report specific things liked/disliked about each course under evaluation. Themes generated from within-group written responses for all three evaluated courses that were unrelated to technical issues were identified. Consumer report themes included (i) clarity of content, (ii) credible messengers with whom they identified, and (iii) an appreciation for multimodal concept reinforcement (e.g. quizzes, animation, illustration). Naive-users discussed similar themes: (i) clarity of content, (ii) appeal of consumers as presenters, (iii) multimodal reinforcement, and (iv) acquisition of novel information. Clinicians themes included (i) appealing layout of software, (ii) approval of education design in line with principles of adult learning, and (iii) relevant and honest patient testimonials. The majority of negative feedback across all courses related to technical issues experienced during course navigation and to the need for clarifications of specific information. This feedback was used to improve both the courses under evaluation as well as future courses as they are produced.
Discussion
The aim of this project was to pilot the development of an online patient education resource. This involved the design both of the online courses themselves and of the process used to develop them. The basic approach was to enlist an instructional method (e-learning) in common use in another context (employee/staff training) and apply it to the requirements of patient education in SCI rehabilitation. In so doing, we were able to benefit from the use of a relatively inexpensive and commonly used software application (Articulate) designed for use in the creation of e-learning resources. We were also able to adopt certain practices in common use in commercial e-learning (such as storyboarding).
For almost all participants, this was a new and unusual kind of project. There was a significant amount of learning by doing, meaning that progress was initially slow but that there were significant gains in productivity as the team moved through the process.
Although it is typical for the production of online patient education resources to be outsourced (to a multimedia agency, for example), we found it was very helpful to have all of the disciplines involved in each stage right from the beginning, with the project team coordinating. There were many occasions where SMEs were able to work directly with the production team to ensure that visual details (anatomy, mobility devices) were accurately rendered. By guiding the process from start to finish, the project team was able to ensure that all aspects of the courses (language, design, images, usability) were aligned to create an effective learning experience.
Wherever possible, evidence-based guidelines were used as the basis for script development. The content development process was made more challenging by the need to include a great deal of information that goes beyond what is covered by guidelines. Within this domain of tacit knowledge, the role of the content working groups was to provide informed experience from a number of different perspectives. Across the board, working group members were enthusiastic in their participation. As rehabilitation professionals and patients, they were able to see the value in this kind of resource and were excited by the opportunity to participate in an innovative venture.
The extensive participation of persons with SCI in all aspects of development was a key principle from the outset. This involvement was necessary to generate the content, in that people living with SCI are clearly SMEs with respect to living with SCI. It also helped shape the language and appearance of the courses. Having persons with SCI involved at all stages also provided a continuous stream of user feedback. It helped ground the courses in the reality of community (rather than hospital) life; real-world examples and testimonials helped to illustrate lessons that were considered relevant by evaluation participants.
Great care was taken to ensure that the courses were attractive and appealing, and that they provide a positive, realistic image of life with SCI. Illustrations and images helped to convey important facts and ideas; they also helped positively re-frame images of disability.
There were a number of challenges that had to be faced over the course of the project; some are inherent in an undertaking of this type, others were matters of circumstance. The task of coordinating a large number (>100) of participants across different disciplines, locations and institutional affiliations proved formidable; the use of productivity tools like web conferencing (GoToMeeting) and collaborative authorship (PBWorks) was essential. The production process was itself very complex, requiring the development of thousands of multimedia assets of various kinds while several courses were being completed simultaneously, but at different rates. Hiring a project manager early in the production process was key to keeping the process on track.
Finally, there were constraints imposed by the limited financial resources available to undertake multimedia work that is inherently expensive. As much as possible, we tried to find creative solutions (such as partnering with a college design program to develop low-cost animations) that allowed us to stretch out the project's budget.
Overall, the work undertaken through the development process appears to have resulted in the creation of a credible, relevant and user-friendly resource that will be effective for persons with SCI to better understand the consequences of their injury and self-manage their condition. The preliminary evaluation results are encouraging and will be used to inform future development of these and additional courses.
Further research
This project was undertaken with the intent of continuing (contingent on success) past the development and evaluation of the first five courses. A second phase kicked off in 2011, with the objective of developing another five courses covering topics that are more complicated or may be of interest to people at a later stage of their rehabilitation (wheelchair skills, pain, sexuality, fertility and parenting, and physical activity).
Having successfully piloted the development of the courses, we are now studying their uptake. Our hypothesis is that the most effective means of dissemination is via health care professionals; accordingly, we intend to provide them with training in how to use this kind of resource with their patients, as well as referral tools. We hope to gather as much feedback as possible from clinicians who use SCI-U with their patients. An important ongoing consideration will be the best way of integrating this kind of online resource within a multimodal patient education program, to create a blended learning model.
We plan to make the content from the SCI-U courses available in a number of other formats: mini-courses, YouTube videos, tablet/smart phone versions. We are also considering the possibility of developing silent versions of the SCI-U courses, for display on large screens in public areas (PT gym, waiting room).
A subsequent manuscript will report final data from the preliminary evaluation along with group differences. Building on the preliminary evaluation, we intend to conduct a larger-scale evaluation using a LMS (learning management system) to register participants and track their use of the courses (portions viewed, time spent, quiz answers, etc).
Finally, this project is like many other education initiatives in that it is very difficult to measure or demonstrate the relationship between knowledge acquisition, behavior change and health outcomes. Future work on online patient education will need to be informed by developments in this area.
Limitations
There are circumstances that may limit the value of this initiative for certain potential users. Because they contain a large amount of multimedia, the course files are very large (>50 GB). Although these data are not downloaded at once, users who have limited-bandwidth Internet connections or who use an older PC or OS version may encounter difficulties (such as delays) in viewing the courses.
In addition, the Articulate software used to create the courses produces output in Adobe Flash format, which means the courses cannot be used on devices (such as iPhones and iPads) that cannot display Flash files.
Finally, efforts have been made through usability testing to ensure that the courses can be viewed by people with limited upper-body mobility or who use assistive technology to access computers; nonetheless, there may be aspects of the courses (quizzes and tabs) that some of these users may have difficulty with.
Addressing these issues is a priority in future development.
Conclusion
The courses developed for SCI-U show the potential for online patient education. Preliminary evaluation indicates that they are appreciated by end-users; further evaluation will focus on knowledge acquisition and retention. The collaboration required to develop content was essential, and was facilitated by the use of IT tools. In particular, the extensive participation of patients was crucial.
SCI-U demonstrates a promising approach; further research will need to study how to integrate this kind of resource into clinical practice and how to drive consumer uptake. This is a domain where technological innovation is currently happening at a rapid pace, opening up new possibilities; future work will need to be attuned to these developments.
Attribution
Rehabilitation Engineering Laboratory, Toronto Rehabilitation Institute/University Health Network and Lawson Health Research Institute, Parkwood Hospital.
Acknowledgements
This article is based the award-winning abstract in Education presented at the 5th National SCI Conference in Toronto, Ontario, in October 2012. London, Ontario, Canada. The study was funded by Rick Hansen Institute. Partners: Toronto Rehab/University Health Network (Toronto, ON), Spinal Cord Injury Ontario (previously CPA Ontario, Toronto, ON), Alberta Health Services (Edmonton & Calgary, AB), Lawson Health Research Institute (London, ON).
References
- 1.Monsivais D, Reynolds A. Developing and evaluating patient education materials. J Contin Educ Nurs 2003;34(4):172–6 [DOI] [PubMed] [Google Scholar]
- 2.Wolfe D, Hsieh J, Curt A, Teasall R, et al. Neurological and functional outcomes associated with SCI rehabilitation. Top Spinal Cord Inj Rehabil 2007;13(1):11–31 [Google Scholar]
- 3.Hoffman J, Salzman C, Garbaccio C, Burns SP, Crane D, Bombardier C. Use of on-demand video to provide patient education on spinal cord injury. J Spinal Cord Med 2011;34(4):404–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Manns PJ, May LA. Perceptions of issues associated with the maintenance and improvement of long-term health in people with SCI. Spinal Cord 2007;45(6):411–9 [DOI] [PubMed] [Google Scholar]
- 5.Potter PJ, Wolfe DL, Burkell JA, Hayes KC. Challenges in educating individuals with spinal cord injury to reduce secondary conditions. Top Spinal Cord Inj Rehabil 2004;10(1):30–40 [Google Scholar]
- 6.Boschen KA, Tonack M, Gargaro J. Long-term adjustment and community reintegration following spinal cord injury. Int J Rehabil Res 2003;26(3):157–64 [DOI] [PubMed] [Google Scholar]
- 7.Olinzock BJ. A model for assessing learning readiness for self-direction of care in individuals with spinal cord injuries: a qualitative study. SCI Nurs 2004;21(2):69–74 [PubMed] [Google Scholar]
- 8.Letts L, Martin Ginis KA, Faulkner G, Colquhoun H, Levac D, Gorczynski P. Preferred methods and messengers for delivering physical activity information to people with spinal cord injury: a focus group study. Rehabil Psychol 2011;56(2):128–37 [DOI] [PubMed] [Google Scholar]
- 9.Gélis A, Stéfan A, Colin D, Albert T, Gault D, Goossens D, et al. Therapeutic education in persons with spinal cord injury: a review of the literature. Ann Phys Rehabil Med 2011;54(3):189–210 [DOI] [PubMed] [Google Scholar]
- 10.Chumley-Jones HS, Dobbie A, Alford CL. Web-based learning: sound educational method or hype? A review of the evaluation literature. Acad Med 2002;7710 Suppl:S86–93 [DOI] [PubMed] [Google Scholar]
- 11.Austin Boren S, Gunlock TL, Krishna S, Kramer TC. Computer-aided diabetes education: a synthesis of randomized controlled trials. AMIA Annu Symp Proc 2006;2006:51–5 [PMC free article] [PubMed] [Google Scholar]
- 12.Gibbons MC, Wilson RF, Samal L, et al. Impact of consumer health informatics applications. Evid Rep Technol Assess (Full Rep). 2009;(188):1–546 [PMC free article] [PubMed] [Google Scholar]
- 13.Chou HK, Lin IC, Woung LC, Tsai MT. An empirical study on outpatients' health education needs and the effectiveness of e-learning. Health Promot Pract 2012;13(1):133–9 [DOI] [PubMed] [Google Scholar]
- 14.Hauber RP, Vesmarovich S, Dufour L. The use of computers and the Internet as a source of health information for people with disabilities. Rehabil Nurs 2002;27(4):142–5 [DOI] [PubMed] [Google Scholar]
- 15.Burkell JA, Wolfe DL, Potter PJ, Jutai JW. Information needs and information sources of individuals living with spinal cord injury. Health Inf Libr J 2006;23(4):257–65 [DOI] [PubMed] [Google Scholar]
- 16.Matter B, Feinberg M, Schomer K, Harniss M, Brown P, Johnson K. Information needs of persons with spinal cord injuries. J Spinal Cord Med 2009;32(5):545–54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Edwards L, Krassioukov A, Fehlings MG. Importance of access to research information among individuals with spinal cord injury: results of an evidence-based questionnaire. Spinal Cord 2002;40(10):529–35 [DOI] [PubMed] [Google Scholar]
- 18.Goodman N, Jette AM, Houlihan B, Williams S. Computer and internet use by persons after traumatic spinal cord injury. Arch Phys Med Rehabil 2008;89(8):1492–8 [DOI] [PubMed] [Google Scholar]
- 19.Brace JA, Schubart JR. A prospective evaluation of a pressure ulcer prevention and management e-learning program for adults with spinal cord injury. Ostomy Wound Manage 2010;56(8):40–50 [PubMed] [Google Scholar]
- 20.Liu S, Liao H, Pratt J. Impact of media richness and flow on e-learning technology acceptance. Computers Educ 2009;52:599–607 [Google Scholar]
- 21.Heinrich E, de Nooijer J, Schaper NC, Schoonus-Spit MH, Janssen MA, de Vries NK. Evaluation of the web-based diabetes interactive education programme (DIEP) for patients with type 2 diabetes. Patient Educ Couns 2012;86(2):172–8 [DOI] [PubMed] [Google Scholar]
- 22.Smith-Stoner M, Willer A. Video streaming in nursing education: bringing life to online education. Nurse Educ 2003;28(2):66–70 [DOI] [PubMed] [Google Scholar]
- 23.Ruiz JG, Teasdale TA, Hajjar I, Shaughnessy M, Mintzer MJ. The consortium of e-learning in geriatrics instruction. J Am Geriatr Soc 2007;55(3):458–63 [DOI] [PubMed] [Google Scholar]
- 24.Zhang D, Zhou L, Briggs R, Nunamaker J. Instructional video in e-learning: assessing the impact of interactive video on learning effectiveness. Inf Manage 2006;43:15–27 [Google Scholar]
- 25.May L, Day R, Warren S. Evaluation of patient education in spinal cord injury rehabilitation: knowledge, problem-solving and perceived importance. Disabil Rehabil 2006;28(7):405–13 [DOI] [PubMed] [Google Scholar]
- 26.Kelly M, Lyng C, McGrath M, Cannon G. A multi-method study to determine the effectiveness of, and student attitudes to, online instructional videos for teaching clinical nursing skills. Nurse Educ Today 2009;29(3):292–300 [DOI] [PubMed] [Google Scholar]
- 27.Wolfe DL, Potter PJ, Sequeira KAJ. Overcoming challenges: the role of rehabilitation in educating individuals with SCI to reduce secondary conditions. Top Spinal Cord Inj Rehabil 2004;10(1):41–50 [Google Scholar]
- 28.Chase TM. Learning styles and teaching strategies: enhancing the patient education experience. SCI Nurs 2001;18(3):138–41 [PubMed] [Google Scholar]
- 29.Schubart JR, Hilgart M, Lyder C. Pressure ulcer prevention and management in spinal cord-injured adults: analysis of educational needs. Adv Skin Wound Care 2008;21(7):322–9 [DOI] [PubMed] [Google Scholar]
- 30.Cooper H, Booth K, Fear S, Gill G. Chronic disease patient education: lessons from meta-analyses. Patient Educ Couns 2001;44:107–17 [DOI] [PubMed] [Google Scholar]
- 31.Barnes E, Simpson S, Griffiths E, Hood K, Craddock N, Smith DJ. Developing an online psychoeducation package for bipolar disorder. J Ment Health 2011;20(1):21–31 [DOI] [PubMed] [Google Scholar]
- 32.Libin A, Schladen M, Ljungberg I, Tsai B, Jacobs S, Reinauer K, Minnick S, Spungen M, Groah S, et al. YouTube as an on-line disability self-management tool in persons with spinal cord injury. Top Spinal Cord Inj Rehabil 2011;16(3):84–92 [Google Scholar]
- 33.Elwyn G, Kreuwel I, Durand MA, Sivell S, Joseph-Williams N, Evans R, Edwards A, et al. How to develop web-based decision support interventions for patients: a process map. Patient Educ Couns 2011;82(2):260–5 [DOI] [PubMed] [Google Scholar]
- 34.Hawthorne K, Prout H, Kinnersley P, Houston H. Evaluation of different delivery modes of an interactive e-learning programme for teaching cultural diversity. Patient Educ Couns 2009;74(1):5–11 [DOI] [PubMed] [Google Scholar]
- 35.Nielsen J. Heuristic evaluation. In: Nielsen J, Mack RL, (eds.) Usability inspection methods. New York: John Wiley & Sons; 1994 [Google Scholar]
- 36.Keen D, Ritson-Jones W, Coburn D, Hegarty B, McDonald J. Evaluation plan for usability testing of module prototypes for the project called: information literacy e-Learning modules: reusable and portable across a college of education, a polytechnic and a university [online document]. 2006. [Accessed 16 August 2012]. Available from http://wikieducator.org/images/b/b6/ModifiedDECAEGfinalusability_EVALPLAN_vers1-1-.2.pdf .


