Abstract
Objective
To determine which trunk inclination directions most accurately predict multidirectional-seated limits of stability among individuals with spinal cord injury (SCI).
Design
Predictive study using cross-sectional data.
Setting
Pathokinesiology Laboratory.
Participants
Twenty-one individuals with complete or incomplete sensorimotor SCI affecting various vertebral levels participated in this study.
Interventions
Participants were instructed to lean their trunk as far as possible in eight directions, separated by 45° intervals, while seated on an instrumented chair with their feet positioned on force plates.
Outcomes measures
Eight direction-specific stability indices (DSIs) were used to define an overall stability index (OSI) (limits of stability).
Results
All DSIs significantly correlated with the OSI (r = 0.816–0.925). A protocol that only tests the anterior, left postero-lateral, and right lateral trunk inclinations accurately predicts multidirectional-seated postural stability (R2 = 0.98; P < 0.001).
Conclusion
Multidirectional-seated postural stability can be predicted almost perfectly by evaluating trunk inclinations performed toward the anterior, left postero-lateral, and right lateral directions.
Keywords: Movement; Outcome assessment; Postural balance; Rehabilitation; Spinal cord injuries, Paraplegia; Tetraplegia
Introduction
Although optimizing seated postural stability generally figures among the key rehabilitation objectives for individuals with spinal cord injury (SCI), quantifying multidirectional-seated postural stability remains extremely challenging in clinical practice and laboratory environments. Over the last few years, some studies have attempted to quantify seated postural stability among individuals with SCI using laboratory-based outcome measures obtained using various biomechanical approaches (e.g. kinematics, kinetics, and electromyography).1–8 However, these laboratory-based outcome measures require the use of various sophisticated measurement instruments generally not readily available to rehabilitation professionals in clinical practice. Consequently, rehabilitation professionals have traditionally favored the use of various clinical tests to quantitatively assess seated postural stability among individuals with SCI.9–12 However, a substantial number of rehabilitation professionals still only qualitatively evaluate seated postural stability13–15 due to time constraints/productivity standards or the lack of precise guidelines or evidence-based knowledge on how to best quantify seated postural stability among individuals with SCI.
Maintaining seated postural stability is challenging for individuals with SCI who generally experience sensory and motor impairments that can affect, to varying degrees, their trunk, lower extremities (L/Es), or upper extremities (U/Es). Such a challenge may become insurmountable at times and results in a loss of balance or in a fall that may have deleterious consequences in this population. Theoretically, maintaining seated postural stability requires direction-dependent muscle activation synergies of the trunk and L/E muscles, especially of the hip muscles.5,7 The majority of these muscles have been found to have mechanical advantages (preferential activation) when trunk movements occur in a specific plane, whereas movements generated in combined planes (e.g. left anterolateral trunk inclination) recruit multiple muscles contributing to multidirectional movements occurring in various planes.16 Passive properties of the trunk and L/Es also contribute to seated postural stability.7
Despite the fact that trunk movements are rarely isolated in a single plane of movement during the performance of functional activities, most of the studies to date have used modified seated functional reach tests that focus on forward (anterior), and, to a lesser extent, lateral trunk inclinations, or U/E reaching tests to estimate seated postural stability. To overcome these limits, an approach comparable to the one proposed by Preuss and Popovic,6 a multidirectional-seated postural stability test that estimates dynamic sitting balance in individuals with SCI, was recently proposed.17 When this test is performed, individuals with SCI lean their trunk in eight different directions in an attempt to obtain the best estimate of the limits of stability within the available base of support (BOS) (detailed information is available in the Methods section). While the multidirectional-seated postural stability test thoroughly assesses eight directions, one may question the need to test all these directions separately in an effort to minimize the time required to acquire and process the data. This may also facilitate eventual implementation transition of a modified version of this test into clinical practice.
The main objective of this study was to determine which specific trunk inclination directions of the multidirectional-seated postural stability test most accurately predict multidirectional-seated postural stability (limits of stability) among individuals with a SCI. It is hypothesized that a subset of trunk inclination directions will provide sufficient information to accurately characterize multidirectional-seated postural stability in this population. This study should therefore provide rehabilitation professionals and scientists with valuable information about which directions should be prioritized when quantifying multidirectional-seated postural stability in this population.
Methods
Participants
A convenience sample of 21 individuals who had sustained a complete or incomplete SCI (American Spinal Injury Association Impairment Scale (AIS A–D))18 at least 3 months prior to the study volunteered to participate in this study after having met the inclusion criteria (Table 1). To be eligible, participants had to be able to independently maintain an unsupported short-sitting position with their feet resting on the floor for 1 minute and had to have been clinically stable for at least 4 weeks prior to the study. Participants were excluded if they were experiencing secondary musculoskeletal impairments affecting their trunk or extremities, secondary skin integrity impairments underneath their buttocks, or any other conditions (i.e. severe visual, auditory, or vestibular impairments) that may have limited their ability to maintain a seated position or see the visual feedback placed 2 m in front of them.
Table 1.
Description of individuals with SCI
| Participants | Age (years) | Height (m) | Weight (kg) | Time since injury (years) | Neurologic level of injury | AIS | Motor Score (100) | Sensory Score (220) | BOS area (m2) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 57 | 1.68 | 98.3 | 3 | T4 | A | 50 | 96 | 0.35 |
| 2 | 23 | 1.68 | 86.3 | 1 | C3 | D | 93 | 187 | 0.33 |
| 3 | 52 | 1.63 | 88.4 | 2 | C6 | B | 28 | 72 | 0.31 |
| 4 | 47 | 1.83 | 109.1 | 5 | L1 | C | 70 | 176 | 0.39 |
| 5 | 49 | 1.73 | 84.5 | 2 | C5 | D | 78 | 153 | 0.37 |
| 6 | 53 | 1.78 | 129.6 | 5 | T10 | A | 50 | 144 | 0.36 |
| 7 | 44 | 1.7 | 73.8 | 3 | T10 | A | 50 | 140 | 0.27 |
| 8 | 58 | 1.88 | 98.2 | 3 | T10 | B | 50 | 140 | 0.33 |
| 9 | 26 | 1.63 | 46.8 | 3 | T11 | A | 50 | 148 | 0.25 |
| 10 | 33 | 1.75 | 65.1 | 3 | C7 | B | 48 | 156 | 0.25 |
| 11 | 25 | 1.8 | 52.9 | 3 | T4 | A | 51 | 96 | 0.25 |
| 12 | 30 | 1.88 | 98.1 | 3 | T10 | A | 50 | 140 | 0.34 |
| 13 | 50 | 1.8 | 78.1 | 26 | T7 | B | 51 | 194 | 0.31 |
| 14 | 25 | 1.83 | 67.9 | 2 | C5 | B | 14 | 58 | 0.32 |
| 15 | 40 | 1.7 | 59.3 | 2 | C8 | C | 69 | 110 | 0.24 |
| 16 | 33 | 1.73 | 88.6 | 1 | T11 | C | 54 | 182 | 0.27 |
| 17 | 27 | 1.83 | 61.4 | 1 | T5 | A | 50 | 102 | 0.25 |
| 18 | 21 | 1.78 | 77.3 | 1 | T9 | A | 55 | 153 | 0.22 |
| 19 | 35 | 1.88 | 75 | 1 | T10 | A | 50 | 138 | 0.28 |
| 20 | 40 | 1.42 | 61.4 | 1 | C8 | D | 69 | – | 0.28 |
| 21 | 29 | 1.72 | 59.1 | 1 | T5 | C | 53 | 109 | 0.26 |
| Mean ± SD | 38 ± 12 | 1.75 ± 0.11 | 79.0 ± 20.4 | 3 ± 5 | 54 ± 16 | 134 ± 38 | 0.30 ± 0.05 |
AS, American Spinal injury Association (ASIA) Impairment Scale: BOS, Base of support.
The study was conducted at the Pathokinesiology Laboratory of the Center for Interdisciplinary Research in Rehabilitation of Greater Montreal (CRIR) located at the Institut de réadaptation Gingras-Lindsay-de-Montréal (IRGLM). Ethical approval was obtained from the Research Ethics Committee of the CRIR (CRIR456-0809). All participants reviewed and signed the informed consent form before entering the study.
Laboratory assessment
Center of pressure assessment
Participants were seated on a height-adjustable instrumented seat, consisting of two force plates, to record reaction forces (sampling frequency = 600 Hz) underneath the right and left buttock, respectively. Reaction forces underneath the right and left foot were recorded (sampling frequency = 600 Hz) using two separate force plates embedded into the floor.19,20 Tri-axial components of the ground reaction forces on each force plate were continuously recorded to compute the center of pressure (COP) time series with respect to the starting point within the force plate coordinate system. Participants were positioned with approximately 75% of the length of their thighs in contact with the instrumented seat and with their knees flexed at approximately 85°. Participants sat upright with both hands placed on their thighs (starting position) to support part of their body weight (head, U/E, and trunk segments) and to optimize seated postural stability and control during the laboratory assessment.
BOS assessment
A motion capture system, incorporating six synchronized motion analysis camera bars (4× Optotrak model 3020 and 2× Optotrak model Certus; NDI Technology Inc., Waterloo, ON, Canada), recorded at a sampling frequency of 60 Hz the three-dimensional (3D) coordinates of 10 infrared light-emitting diodes (LEDs) fixed on the instrumented seat to locate it within the global referential (laboratory referential). Additionally, the 3D coordinates of 18 skin-fixed LEDs used to define the head, trunk, pelvis, U/E, and L/E segments (including the feet) were recorded. Moreover, 24 specific bony landmarks were digitized using a 6-marker probe to further define principal axes of the rigid segments, whereas 16 specific points were probed to model the contour of the feet and buttocks used to define the BOS. The area of the BOS reflects the convex area enclosing the contour of the feet and buttock segments (peripheral points) projected into the horizontal plane of the COP (Fig. 1).
Figure 1.
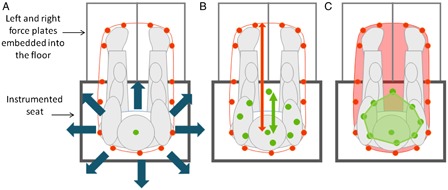
Schematic representation of the eight trunk inclination directions tested (dark blue arrows) (A) and the calculations of the anterior DSI (B), and the OSI (C). In figure 1B, the dark red arrow represents the maximal theoretical position the COP could have moved to reach the boundary of the BOS in the anterior direction (COPMaximal). The dark green arrow represents the real distance travelled by the COP (COPFinal). In figure 1C, the smaller area represents an ellipse fitting the mean peak COP excursion (COPArea) reached in each of the eight tested directions (limits of stability), whereas the bigger area represents the BOS (BOSArea).
All references to colour in this article refer to the online version of the paper.
Experimental tasks
Following a familiarization period, participants were asked to lean their axial skeleton (head and trunk segments) as far as possible from the starting position at a self-selected speed in eight specific directions, each separated by 45°. In each direction tested, participants were instructed to reach as far as possible (i.e. stability limit) and to return to their initial position within a 15-second period. Participants were asked to place and maintain their hands on their thighs and to refrain from anchoring themselves or grabbing their clothes or body segments (i.e. thighs). A flat computer screen, placed 2 m in front of the participants, highlighted the tested direction and the boundaries in which they had to move their COP while providing the real-time position of the COP (visual feedback). Each of the eight movement directions was tested twice for a total of 16 trials, and performed in a random order predetermined by the computer and locked into the program prior to the start of the test. One researcher associate remained next to the participants to ensure optimal safety and to prevent loss of balance or a fall during these tasks. If loss of balance occurred during one or more trial(s), the trial(s) were not repeated due to the constraint of the predetermined testing sequence generated by the computer program. Consequently, the(se) trial(s) can neither be repeated nor included in the analysis. Another researcher associate coordinated the computerized data acquisition and storage at all times.
Outcome measures
Direction-specific stability index
For each of the eight tested directions, the coordinates of the initial position of the COP (COPStart), the farthest position reached by the COP in the indicated trajectory (COPFinal), and the maximal theoretical potential position the COP could have reached to attain the boundary of the BOS in the indicated trajectory (COPMaximal) were calculated. Then, the direction-specific stability index (DSI), expressed as a percentage (%), was calculated for each of the eight directions using this equation:
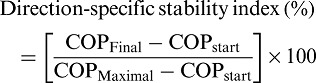 |
Overall stability index
An overall stability index (OSI) representing the area defined by an ellipse fitting the mean peak COP excursion (COPArea) reached in each of the eight tested directions (limits of stability), normalized against the area of the BOS (BOSArea), was calculated and expressed as a percentage (%):
 |
Statistical analyses
Descriptive statistics (mean and standard deviation (SD)) were calculated for participants’ characteristics as well as for all DSIs and OSI. Pearson product-moment correlation coefficients were calculated between each of the eight DSIs and with the OSI to assess the degree of linear association between the specific DSIs (independent variables) and the OSI (dependent variable). A good-to-excellent relationship was confirmed by a correlation coefficient (r) equal or above 0.75.21 Then, the DSIs that were found to have good-to-excellent association with the OSI (P < 0.01) were introduced into a stepwise multiple regression analysis model. All statistical analyses were performed using SPSS statistical package version 17.0 for Windows.
Results
Seated postural stability measures
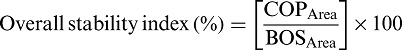
Eight DSIs and the OSI were calculated for each of the participants. The mean and SD (±1SD) for the eight DSIs are shown in a polar coordinate diagram (Fig. 2). The DSIs ranged between 22.62 ± 9.60 and 38.93 ± 12.87% recorded in the anterior and left directions, respectively. The mean OSI (OSI = 9.94 ± 6.74%) varied between individuals (range: 2.00–24.24%).
Figure 2.
Polar plot diagram summarizing the group mean (dark red line) ± 1 SD (light blue area) for the DSI (expressed as a percentage) measured in the eight tested directions.
Correlation analysis
Correlation coefficients for all DSIs and the OSI are reported in Table 2, whereas the association between these variables is further confirmed in Fig. 3. When specifically looking at the associations among the DSIs (r = 0.540–0.925), only 11 out of the 28 possible associations (39.3%) achieved good-to-excellent relationships. Alternatively, all DSIs (100%) achieved good-to-excellent relationships with the OSI. The highest and lowest associations with the OSI were found with the DSIs measured in the anterior (r = 0.925; P ≤ 0.0001) and posterior directions (r = 0.802; P ≤ 0.0001), respectively.
Table 2.
Summary of correlation coefficients obtained between the eight DSIs and the OSI
| DSI | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| DSI | 1. Ant | 2. Post | 3. R Lat | 4. L Lat | 5. R Ant-Lat | 6. L Ant-Lat | 7. R Post-Lat | 8 L Post-Lat | OSI |
| 1 | 1 | 0.622* | 0.691* | 0.666* | 0.818* | 0.700* | 0.701* | 0.671* | 0.925* |
| 2 | 1 | 0.819* | 0.706* | 0.566* | 0.600* | 0.900* | 0.847* | 0.802* | |
| 3 | 1 | 0.816* | 0.698* | 0.725* | 0.854* | 0.844* | 0.870* | ||
| 4 | 1 | 0.621* | 0.876* | 0.737* | 0.925* | 0.846* | |||
| 5 | 1 | 0.696* | 0.746* | 0.612* | 0.838* | ||||
| 6 | 1 | 0.691* | 0.815* | 0.816* | |||||
| 7 | 1 | 0.796* | 0.846* | ||||||
| 8 | 1 | 0.866* | |||||||
| OSI | 1 |
*Significant correlation; P < 0.01.
Figure 3.
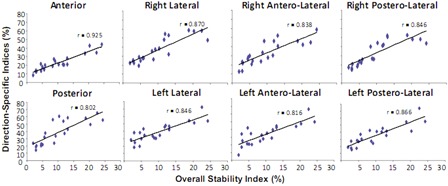
Graph summarizing the association between each direction-specific index and the OSI.
Multiple regression analysis
The results of the multiple regression analysis are outlined in Table 3. All DSIs were initially entered into the model as they all achieved a good-to-excellent association with the OSI (r = 0.816–0.925). The stepwise regression analysis carried out generated three statistically significant hypothetical models to predict the OSI. The model only included measurement of the DSI in the anterior direction and explained 85.6% of the variance of the OSI. Adding the left postero-lateral direction to the first model (Model 2) increased the proportion of explained variance of the OSI to 96.6%. Hence, the best OSI prediction model (Model 3) was obtained by combining weighted DSIs measured in the anterior, left postero-lateral, and right lateral directions (Model 3) as explained by 98.0% of variance. Using this last model, the OSI can be computed using the following formula:
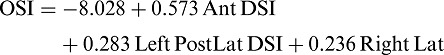 |
Table 3.
Summary of three hypothetical models explaining multidirectional-seated postural stability measures
| Models | R | R2 | SE | P value |
|---|---|---|---|---|
| 1. Ant | 0.925 | 0.856 | 2.619 | <0.00 |
| 2. Ant + L Post-Lat | 0.983 | 0.966 | 1.313 | <0.00 |
| 3. Ant + L Post-Lat + R Lat | 0.990 | 0.980 | 1.027 | <0.00 |
SE, standard error.
Discussion
The aim of this study was to determine if multidirectional-seated postural stability in individuals with SCI could be accurately predicted using a subset of DSI outcome measures. A substantial number of good-to-excellent associations exist across the eight DSIs. All DSIs present good-to-excellent association with the OSI, reflecting multidirectional-seated postural stability. However, the anterior, left postero-lateral, and right lateral DSIs were found to best predict the OSI and explained a very high proportion (R2 = 98%) of the variance observed.
Comprehensive movement assessment
The selection of three DSIs in the final model may be explained, in part, by the fact that they require distinct movement strategies and specific neuromuscular strategies. Interestingly, the selection of isolated (i.e. anterior and right side) and coupled trunk inclination directions (i.e. left postero-lateral), included in the final predictive model tests the limits of stability in the four principal directions of movement in the frontal and sagittal planes. These trunk inclination directions also require concentric and eccentric muscle effort for a specific muscle group depending on the direction of the movements.5,7 Moreover, assessing the limits of stability in a diagonal direction is expected to solicit a larger set of muscles as movements are coupled.7
Since the neurological level affected by the SCI is frequently thoracic or cervical, many individuals with SCI will experience a complete or incomplete sensorimotor paralysis affecting their abdominal and back muscles as well as their L/E muscles. These individuals will need to develop various compensatory strategies,8,22,23 including the use of non-postural muscles (i.e. thoracohumeral muscles such as the serratus anterior and the pectoralis major) to secure seated postural stability depending on their neurological level and the completeness of the lesion. Fortunately, individuals with SCI included in the present study presented with various neurological levels (C3–L1) and various degrees of completeness (AIS A–D) as seen in clinical practice, which may strengthen the generalizability of our results.
Clinical decision-making process
Although few clinical measurement instruments have been proposed to investigate seated postural stability in individuals with SCI, their use remains restricted in clinical practice for different reasons. Rehabilitation professionals frequently voice concerns with respect to time constraints they encounter when conducting comprehensive assessments of individuals with SCI, especially during the initial intensive rehabilitation phase. In that context, rehabilitation professionals will often decide to only carry out an anterior functional reach test as a surrogate measure of multidirectional-seated postural stability for individuals with SCI. According to the results of this study, this single measure, which can be administered rapidly and requires very little equipment, definitively provides a good estimation of multidirectional-seated postural stability (R2 = 85.6%) and its use should be encouraged in clinical practice.12,13 However, the accuracy of this estimation can be substantially improved without drastically increasing the burden of the rehabilitation professionals in light of the results obtained. Adding at least one measure of trunk inclination direction (i.e. left postero-lateral direction), or even two trunk inclination directions (i.e. left postero-lateral and right lateral direction), may best estimate multidirectional-seated postural stability at the expense of limited therapy time.
Future directions
Most studies that have focused on seated postural stability among individuals with SCI have used different U/E positions and weight-bearing roles.24 In fact, some researchers have assessed seated postural stability without any support of the U/Es and with both U/Es crossed over the chest or using forward reaching.1,5,11,13,22 Some researchers have allowed unilateral U/E support while the other U/E was used to reach. Lastly, some researchers have allowed bilateral U/E support.13,25 In the present study, we observed that most of the participants could not lean in the proposed directions in a sitting position without the assistance of their U/Es (unsupported reaching). Although no clear consensus on standardized testing protocols has yet emerged, we do acknowledge that the bilateral U/E support may have reduced the complexity of the task, especially for individuals with full or partial motor control of their abdominal and low-back muscles.17 Since individuals with SCI frequently anchor one U/E on a fixed object (i.e. wheelchair handle or backrest) to stabilize their trunk and avoid loss of balance or a fall when leaning or reaching with the other U/E in daily life, unilateral U/E support when the other U/E reaches in the proposed directions may represent a trade-off to favor in the future when performing multidirectional-seated postural stability assessments.
As this study involved a relatively small sample size, future studies should include a larger number of individuals with SCI to increase the strength of the results obtained in the present study. Moreover, a larger number of participants with SCI would allow researchers to better assess the effects of the sensori-motor impairments on multidirectional-seated limits of stability. Verifying the association between the multidirectional-seated limits of stability and the performance of functional activities (e.g. sitting pivot transfers, manual wheelchair propulsion) is also warranted in the future. Given that rehabilitation professionals have restricted access to sophisticated measurement instruments required to perform a multidirectional-seated postural stability assessment, that measurement instruments are available and that rehabilitation professionals do not necessarily fully master the testing protocol and lack the time needed to perform the tests, it is difficult to translate the protocol used in this study in clinical practice. Since a good association between the COP displacement and the movement excursion of the spinous process of the 7th cervical vertebra (C7) was recently documented by Field-Fote and Ray1 measuring movement excursion of this last anatomical reference with a laser rangefinder when leaning in the three key directions identified (anterior, left postero-lateral, and right lateral) while sitting, may represent an alternative to quantify multidirectional-seated postural stability in clinical practice. This approach is also promising as it may also allow clinicians to assess individuals with tetraplegia or severe U/E impairments. Further studies documenting the psychometric properties of such an alternative approach within a large cohort of individuals with SCI are necessary before it can be used in clinical practice or research protocols. Meanwhile, rehabilitation professionals are encouraged to use methods currently available (e.g. use of a yardstick) to measure movement excursion in the three key directions highlighted in the present study when assessing multidirectional-seated postural stability.
Conclusion
Findings from the current study suggest that multidirectional-seated postural stability can be almost perfectly predicted from the results obtained when individuals with SCI lean in the anterior, left postero-lateral, and right lateral directions. The results obtained when leaning in these last three directions may become useful outcome measures to characterize change over time or the impact of various treatments on multidirectional-seated postural stability. Findings from the current study also have implications for rehabilitation professionals and scientists as the time required to estimate multidirectional-seated postural stability can be considerably reduced when assessing only three of the eight directions.
Acknowledgements
This article is based on the award-winning student abstract presented at the National Spinal Cord Injury Conference in Toronto, Ontario, Canada in October 2012. Special thanks to Murielle Grangeon, Philippe Gourdou, Youssef El Khamlichi, and Guillaume Desroches for data collection and analysis. Cindy Gauthier received a Summer Research Award from the Quebec Rehabilitation Research Network (REPAR). Dany Gagnon holds a Junior 1 Research Career Award from the Fonds de la recherche en santé du Québec (FRSQ). The Pathokinesiology Laboratory was financed in part by the Canada Foundation for Innovation (CFI). This project was financed in part by the REPAR and the Craig Neilson Foundation. Dany Gagnon, Cyril Duclos, Géraldine Jacquemin, and Milos Popovic are members of the Quebec-Ontario Spinal Cord Injury Mobility (SCI-MOB) Research Group financed by the REPAR and the Ontario NeuroTrauma Foundation.
References
- 1.Field-Fote EC, Ray SS. Seated reach distance and trunk excursion accurately reflect dynamic postural control in individuals with motor-incomplete spinal cord injury. Spinal Cord 2010;48(10):745–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kamper D, Barin K, Parnianpour M, Reger S, Weed H. Preliminary investigation of the lateral postural stability of spinal cord-injured individuals subjected to dynamic perturbations. Spinal Cord 1999;37(1):40–6 [DOI] [PubMed] [Google Scholar]
- 3.Kerr HM, Eng JJ. Multidirectional measures of seated postural stability. Clin Biomech (Bristol, Avon) 2002;17(7):555–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grigorenko A, Bjerkefors A, Rosdahl H, Hultling C, Alm M, Thorstensson A. Sitting balance and effects of kayak training in paraplegics. J Rehabil Med 2004;36(3):110–6 [DOI] [PubMed] [Google Scholar]
- 5.Masani K, Sin VW, Vette AH, Thrasher TA, Kawashima N, Morris A, et al. Postural reactions of the trunk muscles to multi-directional perturbations in sitting. Clin Biomech (Bristol, Avon) 2009;24(2):176–82 [DOI] [PubMed] [Google Scholar]
- 6.Preuss RA, Popovic MR. Quantitative analysis of the limits of stability in sitting. J Appl Biomech 2010;26(3):265–72 [DOI] [PubMed] [Google Scholar]
- 7.Preuss R, Fung J. Musculature and biomechanics of the trunk in the maintenance of upright posture. J Electromyogr Kinesiol 2008;18(5):815–28 [DOI] [PubMed] [Google Scholar]
- 8.Seelen HA, Potten YJ, Drukker J, Reulen JP, Pons C. Development of new muscle synergies in postural control in spinal cord injured subjects. J Electromyogr Kinesiol 1998;8(1):23–34 [DOI] [PubMed] [Google Scholar]
- 9.Boswell-Ruys CL, Sturnieks DL, Harvey LA, Sherrington C, Middleton JW, Lord SR. Validity and reliability of assessment tools for measuring unsupported sitting in people with a spinal cord injury. Arch Phys Med Rehabil 2009;90(9):1571–7 [DOI] [PubMed] [Google Scholar]
- 10.Boswell-Ruys CL, Harvey LA, Barker JJ, Ben M, Middleton JW, Lord SR. Training unsupported sitting in people with chronic spinal cord injuries: a randomized controlled trial. Spinal Cord 2010;48(2):138–43 [DOI] [PubMed] [Google Scholar]
- 11.Sprigle S, Maurer C, Holowka M. Development of valid and reliable measures of postural stability. J Spinal Cord Med 2007;30(1):40–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lynch SM, Leahy P, Barker SP. Reliability of measurements obtained with a modified functional reach test in subjects with spinal cord injury. Phys Ther 1998;78(2):128–33 [DOI] [PubMed] [Google Scholar]
- 13.Jorgensen V, Elfving B, Opheim A. Assessment of unsupported sitting in patients with spinal cord injury. Spinal Cord 2011;49(7):838–43 [DOI] [PubMed] [Google Scholar]
- 14.Ardolino EM, Hutchinson KJ, Pinto Zipp G, Clark M, Harkema SJ. The ABLE scale: the development and psychometric properties of an outcome measure for the spinal cord injury population. Phys Ther 2012;92(8):1046–54 [DOI] [PubMed] [Google Scholar]
- 15.Medley A, Thompson M. Development, reliability, and validity of the Sitting Balance Scale. Physiother Theory Pract 2011;27(7):471–81 [DOI] [PubMed] [Google Scholar]
- 16.Stokes IA, Gardner-Morse M. Quantitative anatomy of the lumbar musculature. J Biomech 1999;32(3):311–6 [DOI] [PubMed] [Google Scholar]
- 17.Gauthier C, Gagnon D, Grangeon M, Jacquemin G, Nadeau S, Masani K, et al. Comparison of multidirectional seated postural stability between individuals with spinal cord injury and able-bodied individuals. J Rehabil Med (In press) [DOI] [PubMed] [Google Scholar]
- 18.Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, et al. for American Spinal Injury Association International Standards of Neurological Classification of the Spinal Cord Injury (ISNCSCI) revised 2011. J Spinal Cord Med 2011;34(6):535–46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nadeau S, Desjardins P, Briere A, Roy G, Gravel D. A chair with a platform setup to measure the forces under each thigh when sitting, rising from a chair and sitting down. Med Biol Eng Comput 2008;46(3):299–306 [DOI] [PubMed] [Google Scholar]
- 20.Gagnon D, Nadeau S, Desjardins P, Noreau L. Biomechanical assessment of sitting pivot transfer tasks using a newly-developed instrumented transfer system among long-term wheelchair users. J Biomech 2008;41:1104–10 [DOI] [PubMed] [Google Scholar]
- 21.Portney LG, Watkins MP. Correlation. In: Cohen M, (ed.) Foundations of clinical research: applications to practice. 3rd ed New Jersey: Pearson Prentice Hall; 2009. p. 523–38. [Google Scholar]
- 22.Seelen HA, Potten YJ, Huson A, Spaans F, Reulen JP. Impaired balance control in paraplegic subjects. J Electromyogr Kinesiol 1997;7(2):149–60 [DOI] [PubMed] [Google Scholar]
- 23.Minkel JL. Seating and mobility considerations for people with spinal cord injury. Phys Ther 2000;80(7):701–9 [PubMed] [Google Scholar]
- 24.Grangeon M, Gagnon D, Gauthier C, Jacquemin G, Masani K, Popovic MR. Effects of upper limb positions and weight support roles on quasi-static seated postural stability in individuals with spinal cord injury. Gait Posture 2012;36(3):572–9 [DOI] [PubMed] [Google Scholar]
- 25.Shirado O, Kawase M, Minami A, Strax TE. Quantitative evaluation of long sitting in paraplegic patients with spinal cord injury. Arch Phys Med Rehabil 2004;85(8):1251–6 [DOI] [PubMed] [Google Scholar]


