Abstract
Objective
This study aimed at analyzing the rate of self-exclusion at the Regional Blood Bank in Montes Claros.
Methods
Data of self-excluding donors from August 2008 to August 2010 were analyzed. The following variables were considered: age, marital status, gender, ethnical background, blood group, Rh factor, number of donations, type of donation and serologic results.
Results
During the analyzed period, 34,778 individuals donated blood, 215 (0.62%) of which were self-excluded; 12% of donors did not answer, 6.3% ballots were spoilt and 13.6% of the responses were considered non-compliant. The profile of the donors was: male (81.9%), single (50.7%), aged between 19 and 29 years old (52.1%), Mulatto (48.3%), blood group O (32.1%) and positive Rh (32.1%). Most individuals were donating for the 2ndto 5th time (43.7%) and had negative serology (94.4%).
Conclusion
It was not evident that self-excluding donors had higher rates of seropositivity.
Keywords: Blood donors, Blood safety, Donor selection
Introduction
The use of blood, its components and derivatives, has long been considered a very important therapeutic resource. Since very early times, blood has played an important role in the history of mankind and has always been linked to the concept of life. Blood transfusion is a process that, even if carried out within recommended guidelines, involves risks to health with the possibility of transfusion incidents including risk related to infectious and parasitic diseases. Surveillance of the entire transfusion process, from donation to the blood transfusion itself, is essential to prevent these diseases.(1)
The increasing use of blood requires an increase in the number of the blood donors. In the interests of both the transfused patient and the physician who prescribes treatment, a high level of concern for the safety of blood transfusion is essential in to reduce risks.(2) Hemotherapy is characterized by the development and adoption of new technology to minimize transfusion risk and especially to prevent the spread of infectious agents.
The transmission of infectious agents by the transfusion of whole blood, blood components and blood products is characterized by higher risk of late adverse reactions in transfused patients. The continuous effort to reduce transfusion-related risk, particularly in regards to the transmission of diseases, has stimulated the organization of services and procedures to select donors.
Minimizing the possibility of disease transmission by blood transfusion requires specific actions to ensure the safety of the blood to be transfused. Pre-transfusion measures involve the selection of donors, which together with serological screening tests, significantly decreases the possibility of disease transmission; even so the procedure is never totally risk-free.(3) The safety of blood transfusion depends on multiple factors, including the epidemiological profile of the population from which donation candidates are chosen, the selection of these candidates in the clinic and serologic screening for blood-borne diseases.(1)
The strategy of confidential unit exclusion was initiated with the aim of increasing transfusion safety by offering the donor an opportunity to confidentially state whether he/she thinks that the donation is appropriate for use in blood transfusion. When it was recommended by the US Food and Drug Administration (FDA) in the 1980s with the aim of increasing blood transfusion safety, self-exclusion was adopted by several countries to avoid the use of blood bags that, even with negative serology, may still be in the 'window' period for blood-borne diseases.(4,5) Using selfexclusion, donors have the opportunity to convey to transfusion services their possible exposure to risk factors for infectious diseases and confidentially excluded themselves.
According to the Brazilian government resolution of December 16, 2010 that defines health regulations for services involved in activities related to the production of human blood components and to transfusion procedures, blood transfusion services can offer donors the opportunity to confidentially exclude themselves.(6) Confidential unit exclusion has been studied by several authors to try to understanding its use and its effectiveness.(7-12)
The Hemocentro Regional de Montes Claros -Fundação Hemominas, was created in the 1980s to implement the guidelines of the National Blood Program in Minas Gerais. The Montes Claros Regional Blood bank began its operations in 1987 and today collects about 1900 bags of blood per month to meet the demand for blood and blood components of 29 transfusion services in 22 counties.(13) Confidential unit exclusion at the Fundação Hemominas, called the Confirmation of Donation, is available to all blood donors and employs a standard paper ballot that is placed in an urn after donation.
This study aimed to analyze the rate of self-exclusion at the Regional Blood bank in Montes Claros and to correlate this to donor characteristics such as age, marital status, gender, ethnical background, blood group (ABO), Rh factor, number of donations, type of donation and serologic results.
Methods
This study was approved by the Ethics Committee of the Fundação Hemominas (registration #266). A crosssectional study was conducted by surveying the blood bags that were discarded between August 2008 and August 2010 due to confidential unit exclusion. Using the database of the Fundação Hemominas, the profiles of self-excluding donors were evaluated in terms of gender (male, female), age (less than 29 years of age or over 29 years), self-reported ethnical background (White, Mulatto, Black), marital status (married, single, other), blood group (A, B, O, AB), Rh factor (positive, negative), type of donation (first donation, return donation), the result of serologic screening of the current and previous donations (released for use, not released).
The data were analyzed using absolute frequencies and percentages. The Pearson Chi-Square test in the Statistical Package for Social Sciences 18.0 was used to identify associations between the characteristics of interest. The significance level for all tests was set for an alpha error of 5% (p-value < 0.05).
Results
In this period, 34,778 individuals donated blood at the Regional Blood bank in Montes Claros, 215 (0.62%) of which were self-excluded. The self-exclusion option was offered to all donors, whereupon 12% of donors did not answer, 6.3% ballots were spoilt and 13.6% of the responses were considered non-compliant. By frequency analysis, the profile of the self-excluding donors was investigated (Table 1). They are mostly men (81.9%), single (50.7%) and aged between 19 and 29 years old (52.1%). The donors were from Montes Claros, Minas Gerais, Brazil (42.8%), other municipalities of Minas Gerais (49.8%) and other states (7.4%).
Table 1.
Profile of self-excluding blood donors (n = 215) between August 2008 and August 2010 at the Regional Blood Bank in Montes Claros
| Variable | n | % |
| Gender | ||
| Male | 176 | 81.9 |
| Female | 39 | 18.1 |
| Age group (years) | ||
| 19-29 | 112 | 52.1 |
| 30-39 | 56 | 26.0 |
| 40-49 | 34 | 15.8 |
| 50-60 | 13 | 6.0 |
| Self-reported ethnical background | ||
| Mulatto | 102 | 48.3 |
| Black | 83 | 39.3 |
| White | 26 | 12.3 |
| Marital status | ||
| Single | 109 | 50.7 |
| Married | 80 | 37.2 |
| Other | 26 | 12.1 |
| Origin | ||
| Montes Claros, MG | 92 | 42.8 |
| Other cities, MG | 107 | 49.8 |
| Other states | 16 | 7.4 |
| Blood group | ||
| A | 69 | 32.1 |
| B | 28 | 13.0 |
| AB | 9 | 4.2 |
| O | 109 | 50.7 |
| Rh factor | ||
| Positive | 191 | 88.8 |
| Negative | 24 | 11.2 |
| Type of donation | ||
| First donation | 66 | 30.7 |
| Repeat donation | 149 | 69.3 |
In regards to the self-reported ethnical background of the donors, 48.3%, 39.3% and 12.3% considered themselves Mulattos, Blacks and Whites, respectively. The age of donors ranged from 19 to 60 years old, with an average of 32 years old and a standard deviation of 9.8 years. Self-exclusion predominated in donors who were donating for the 2nd to 5th time (43.7%), who were blood type O (50.7%) and who were Rh positive (88.8%).
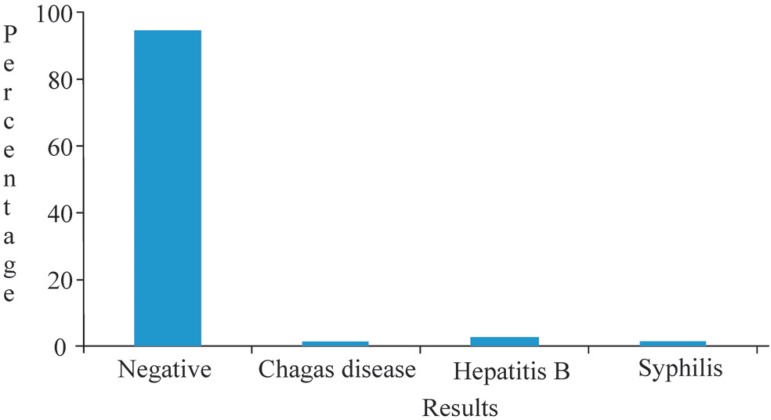
Table 2 shows that most self-excluding donors were donating for the 2nd to 5th time (43.7%) followed by first-time donors (23.3%). Of the discarded blood products, 94.4% were serologically negative while 5.6% were positive. Of these, 1.4% of the cases were positive for syphilis or Chagas disease and 2.8% for Hepatitis B (Figure 1).
Table 2.
Distribution of study participants (n = 215) according to the number of donations, results of serological screening of the current donation and results of previous donations
| Variable | n | % |
| Number of donations | ||
| 1 | 50 | 23.3 |
| 2 - 5 | 94 | 43.7 |
| 6 - 10 | 29 | 13.5 |
| 11-20 | 30 | 14.0 |
| 21 -46 | 12 | 5.6 |
| Result of serological screening of current donation | ||
| Negative | 203 | 94.4 |
| Chagas disease | 3 | 1.4 |
| Syphilis | 3 | 1.4 |
| Hepatitis B | 6 | 2.8 |
| Results of previous donations | ||
| Negative | 169 | 78.6 |
| Risky behavior for sexually transmitted diseases | 28 | 13.1 |
| Infectious disease | 8 | 3.7 |
| Positive first sample | 10 | 4.7 |
Figure 1.
Results of serological screening of self-excluding donors
In relation to previous donations, of 215 selfexcluding donors, 169 (78.6%) were considered suitable for donation, 13.0% were considered unfit due to risky behavior linked to sexually transmitted diseases (STDs), 3.7% for having a history of disease and 4.7% for having presented a positive serological screening test. The result of the chi-square test showed no significant relationship between the previous result and the current results of donation (p-value = 0.862).
The chi-square test was used in an attempt to identify associations between the aforementioned covariates. At one time the majority of self-excluding donors were believed to be male, perhaps reflecting gender differences in the frequency of total donations, but in the current study there was no correlation between genders (p-value = 0.701). Other correlations considered were first donation or return donation in relation to marital status and donor age at first donation or return donation; these variables also showed no associations (p-value = 0.842 and p-value 0.592, respectively). It was also believed that self-exclusion may be more common in donors whose previous donations had been problematic. Thus, the previous serology screening was compared with the current serology and again no correlation was found.
Discussion
The intention of confidential unit exclusion in screening blood donors is to prevent the use of blood products that may be in the window period for blood-borne diseases. In Brazil, the technical standards in blood transfusion were first mandated by the Ministry of Health in 2004.(1) However according to current legislation, the transfusion service can offer donors the opportunity to confidentially exclude their donation from the transfusion system.(6) According to Ferreira,(14) this mechanism provides additional safety because the use of self-exclusion will prevent 2 to 17 blood bags, that had previously been transfused annually, from being used during the window period.
In this period, the self-exclusion rate was 0.62% at the Regional Blood bank in Montes Claros. A similar result was reported by Korelitz et al.(15) This percentage is considered low when compared to other studies which reported selfexclusion rates of up to 2.71%.(4,8,16,17) The self-excluding donors in this study sample had the following profile: male, single, aged between 19 and 29 years old, Mulattos, coming from municipalities in Minas Gerais State, blood group O and Rh positive. Self-exclusion also prevailed in return donors who were donating for the 2nd to 5th time.
The present study showed no higher rate of seropositivity among self-excluding donors, but 5.6% of them were serologically positivity for serological markers of HBV, Chagas disease or syphilis. Some authors had found a higher seroconversion rate among self-excluding donors.(4,7,17) Zou et al.,(7) in assessing the prevalence of positive serological markers in blood donors between 1995 and 2001, correlated this to self-exclusion. These authors showed a higher prevalence of HIV, HBV, HCV and syphilis in selfexcluding donors, although use of confidential unit exclusion had low predictive value and sensitivity. Another study performed with 176,097 units of blood demonstrated that 2.72% of the collected bags were discarded as a result of self-exclusion also with a higher prevalence of HIV1, HIV2 and HCV.(4)
These results demonstrate that the rate of self-exclusion presented at the Regional Blood Bank in Montes Claros is about 4.5 times less than the rate reported in other studies. Such pre-transfusion measures as the use of confidential unit exclusion together with serological screening tests reduce the chance of disease transmission through transfusions.
Conclusion
It was not evident that self-excluding donors had higher rates of seropositivity.
Table 3.
Comparison between variables in respect to the type of donation
| Type of donation | |||
| Variable | First donation (%) | Return donation (%) | p-value* |
| Gender | 0.701 | ||
| Female | 17.9 | 82.1 | |
| Male | 24.4 | 75.6 | |
| Marital status | 0.842 | ||
| Single | 31.2 | 68.8 | |
| Married | 28.8 | 71.2 | |
| Other | 9.0 | 81.0 | |
| Age group (years) | 0.592 | ||
| 19-29 | 53.0 | 51.7 | |
| 30-39 | 22.7 | 27.5 | |
| 40-49 | 15.2 | 16.1 | |
| 50-60 | 9.1 | 4.7 | |
* Chi-squares
Acknowledgments
The Fundação de Amparo à Pesquisa do Estado de Minas Gerais (FAPEMIG) gave financial support for this study.
Footnotes
Conflict-of-interest disclosure: The authors declare no competing financial interest
Study carried out at Hemocentro Regional de Montes Claros, Fundação Hemominas, Montes Claros, MG, Brazil
References
- 1. Brasil. Ministério da Saúde. Agência Nacional de Vigilância Sanitária Manual técnico para investigação da transmissão de doenças pelo sangue. Brasília (DF): Ministério da Saúde; 2004. p.110 [Google Scholar]
- 2. Araújo ES, Barone AA.Sangue seguro: mito ou realidade? Rev Bras Hematol Hemoter. 2008; 30(5): 347-51 [Google Scholar]
- 3. Carrazzone CF, Brito AM, Gomes YM.Importância da avaliação sorológica pré- transfusional em receptores de sangue. Rev Bras Hematol Hemoter. 2004; 26(2): 93-8 [Google Scholar]
- 4. Martins PR, Martins RA, Souza HM, Barbosa VF, Pereira GA, Eustáquio JM, et al. Perfil do doador de sangue autoexcluído no Hemocentro Regional de Uberaba-MG (HRU) no período de 1996 a 2006. Rev Bras Hematol Hemoter. 2009; 31(4): 222-7 [Google Scholar]
- 5. Castro VO.papel do voto de autoexclusão na segurança transfusional. Rev Bras Hematol Hemoter. 2009; 31(4): 213-4 [Google Scholar]
- 6. Brasil. Ministério da Saúde. Agência Nacional de Vigilância Sanitária RDC 57 de 16/12/2010. Brasília (DF): Diário Oficial da União; 2010. [Google Scholar]
- 7. Zou S, Notari EP, Musavi F, Dodd RY, ARCNET Study Group Current impact of the confidential unit exclusion option. Transfusion. 2004; 44(5): 651-7 [DOI] [PubMed] [Google Scholar]
- 8. O'Brien SF, Fan W, Xi G, Yi QL, Goldman M.Evaluation of the confidential unit exclusion form: the Canadian Blood Services experience. Vox Sang. 2010; 98(2): 138-44 [DOI] [PubMed] [Google Scholar]
- 9. Sümnig A, Konerding U, Kohlmann T, Greinacher A.Factors influencing confidential unit exclusions in blood donors. Vox Sang. 2010; 98(3Pt 1): e231-40 [DOI] [PubMed] [Google Scholar]
- 10. Jorge GM, Borges MO, Matéria NS, Silva NI, Sekiya EJ, Alves, et al. Avaliação do entendimento do voto de auto-exclusão [abstract]. Rev Bras Hematol Hemoter. 2004; 26(Supl2): 221-2 [Google Scholar]
- 11. Santos EC, Silva AC, Lavezzo AV, Norcia AM, Souza JF.Avaliação do entendimento do doador de sangue no Núcleo de Hemoterapia de Presidente Prudente quanto ao procedimento de auto-exclusão [abstract]. Rev Bras Hematol Hemoter. 2007; 29 (Supl3): 288 [Google Scholar]
- 12. Herrera P, Fernandes AT, Ferreira O, Ubiáli EM, Covas DT.Avaliação do entendimento do doador de sangue no Hemocentro de Ribeirão Preto quanto ao procedimento de auto-exclusão. Rev Bras Hematol Hemoter. 2006; 28(2): 279 [Google Scholar]
- 13. Fundação Hemominas: 1985-2007. Belo Horizonte: Fundação Hemominas; 2007. p.222 [Google Scholar]
- 14. Ferreira O.Estudo de doadores de sangue com sorologia reagente para hepatites B e C, HIV e sífilis no Hemocentro de Ribeirão Preto (dissertation). Ribeirão Preto: Faculdade de Medicina de Ribeirão Preto; 2007. [Google Scholar]
- 15. Korelitz JJ, Willians AE, Bush MP, Zuck TF, Ownby HE, Matijas LJ.Demographic characteristics and prevalence of serologic markers among donors who use the confidential unit exclusion process: the Retrovirus Epidemiology Donor Study. Transfusion. 1994; 34(10): 870-6 [DOI] [PubMed] [Google Scholar]
- 16. Rodríguez EA.Autoexclusión confidencial inefectivaendonadores de sangre. Rev Mex Pat Clin. 1999; 46(3): 147-50 [Google Scholar]
- 17. Newman B.Blood donor suitability and allogeneic whole blood donation. Transfus Med Rev. 2001; 15(3): 234-44 [DOI] [PubMed] [Google Scholar]