Abstract
Objective
The aim of this work was to establish reference values for methemoglobin levels in 6 to 10-year-old children.
Methods
Methemoglobin concentrations were studied in clinically healthy children. The method for methemoglobin measurement used, neither uses highly toxic chemical compounds nor expensive enzymatic methods, thus it is feasible in the laboratory routine.
Results
The results showed higher reference values for clinically healthy children (from 3.61 to 6.44%) than for adults (from 1.9 to 3.8%).
Conclusion
The higher concentrations of methemoglobin in children may be explained by smaller amounts of soluble cofactor cytochrome b5 and reduced activity of the cytochrome b5 reductase enzyme in red blood cells which make children particularly susceptible to the development of methemoglobinemia. Methemoglobin concentrations in children are higher than in normal adult subjects thus, adult reference values cannot be used to interpret infant methemoglobinemia.
Keywords: Methemoglobin, Methemoglobinemia, Reference values, Oxidative stress, Child
Introduction
During their life span, red blood cells are exposed to multiple endogenous and exogenous agents that oxidize hemoglobin to methemoglobin. Without an efficient enzymatic reduction system of methemoglobin, daily accumulations of 2 to 3% of pigment can occur. However, under efficient systems, human red blood cells accumulate less than 0.6% of methemoglobin.(1)
Methemoglobin is a derivative of hemoglobin in which the iron ion is in its oxidized form (Fe+3).(2) The spontaneous formation of methemoglobin is normally neutralized by protecting enzymatic systems the most important being via cytochrome b5 reductase, which catalyzes the transfer of one electron from NADPH to the heme group. Another mechanism involves the direct transfer of ascorbic acid and glutathione to the heme group.(3) In spite of the existence of other mechanisms that reduce methemoglobin, the NADPH-dependent reaction catalyzed by cytochrome b5 reductase is of physiologically importance.(2)
Excesses of methemoglobin occur when the iron heme is oxidized to the ferric form at speeds that exceed its reduction to the ferrous form, thereby characterizing methemoglobinemia. The main causes of increases in methemoglobin are deficiency of red blood cell enzymes involved in the redox system of the iron-heme group, oxidative stress caused by chemical compounds and molecular defects of hemoglobin that cause continuous oxidation.(4) Unstable hemoglobins, such as the hemoglobins Zurich (β63His → Arg), Hammersmith (β42Phe → Ser) and Freiburg (β23 → Val0), can also cause cyanosis.
The rapid production of methemoglobin by exogenous agents depends on several factors including the amount of agent that enters the circulation, the metabolism of these compounds in the body, the conversion rates of these compounds into highly oxidizing intermediate forms, excretion of the compound and the rate at which red blood cells can reduce methemoglobin to hemoglobin. Different chemicals used both domestically and in industries and different therapeutic agents increase the heme oxidation rate by up to 1000 times, surpassing the capacity of red blood cells to maintain hemoglobin in its reduced state.(4)
Methemoglobinemia can also be of a genetic cause with the most common being cytochrome b5 reductase enzyme deficiency; in the absence of this enzyme, the methemoglobin concentration can increase by up to 40%.(2) Another rare genetic cause is the hemoglobin mutant known as hemoglobin M, which is characterized by the maintenance of oxidized iron.(5) Several abnormal hemoglobins, collectively called hemoglobin M, have been described. In the majority of them, the genetic abnormality happens by the replacement of a proximal tyrosine and a distal histidine. Hemoglobin M Boston, described in several countries including Brazil, is the most common.(6)
Methemoglobinemia should be suspected in any patient with unexplained cyanosis.(7) In cases of acute poisoning due to the ingestion of drugs or exposure to toxin, patients may present clinical symptoms of anemia in addition to cyanosis.(8)
The evaluation of the methemoglobin concentration is an important marker of biological processes of oxidative damage but its measurement is little requested in the laboratory routine. This fact can be explained by the lack of knowledge of the hematological symptoms of methemoglobinemia and by technical factors.(4) The method proposed by Evelyn & Maloy(9) uses highly toxic chemical compounds which discourage its use. The enzymatic methods are expensive and thus are infrequently employed.
Naoum et al.(4) proposed a quantitative test for the measurement of methemoglobin without the use of toxic compounds, which has provided an alternative in the diagnosis of methemoglobinemia and has established reference values for the normal adult population (ranging from 1.9 to 3.8%).
The aim of this work was to establish reference values for methemoglobin in 6- to 10-year-old children using a method to measure methemoglobin that neither uses highly toxic chemical compounds nor is expensive.
Methods
The blood samples used in this work were collected from children who participated in the university extension project "Occurrence of parasitic infections and anemia in school age children of the Ayrton Senna Municipal school, Curitiba, Parana" registered in Pro-Reitoria de Extensão e Cultura (PROEC), Universidade Federal do Paraná (# 472/ 08). Blood collections were performed after parents or legal guardians signed informed consent forms.
Blood samples of 78 children were collected in EDTA K3 anticoagulant for blood tests (whole blood test, leukogram and platelet count) carried out in a Coulter T-890 Hematology Analyzer with spectrophotometric measurement of the methemoglobin concentration. All the children included in this study were considered to be clinically healthy and had normal blood counts and no clinical history of cyanosis. Methemoglobin concentrations of an adult population aged from 21 to 60 years old and considered clinically healthy due to normal blood counts and no clinical history of cyanosis were also measured.
The technique proposed to determine red blood cell methemoglobin, as a percentage, is based on stabilization at 60 moles/L using a phosphate buffer solution followed by hemolysis with 1% saponin; methemoglobin and oxyhemoglobin are measured by spectrophotometry using wavelengths of 630 nm and 540 nm, respectively.(4) Absorbance measurements were carried out in a Cintra 10 Spectrometer (GBC Scientific Equipment; Melbourne, AUS)
Results
Means and reference values of hematological parameters and methemoglobin concentrations are described for children in Table 1 and for adults in Table 2.
Table 1.
Means and reference ranges of hematological variables* including methemoglobin concentration in seventy-eight 6- to 10-year-old children
| Analytes | Mean | Reference values | |
| Red blood cells (x 109/L) | 4.83 | 4.05 | 5.6 |
| Hemoglobin (g/dL) | 13.57 | 10.7 | 15.6 |
| Hematocrit (%) | 38.99 | 33.7 | 44.2 |
| Mean corpuscular volume (fL) | 81.19 | 63.4 | 90.7 |
| Mean corpuscular hemoglobin (pg) | 28.29 | 20.2 | 31.3 |
| Mean corpuscular hemoglobin concentration (g/dL) | 34.62 | 31.3 | 37.2 |
| Platelets (x 109/L) | 310.10 | 148 | 583 |
| Methemoglobin (%) | 4.61 | 3.61 | 6.44 |
*Data obtained with two replicates
Table 2.
Means and reference ranges hematological variables* including methemoglobin concentration in fifteen 21- to 60-year-old adults
| Analytes | Average | Reference values | |
| Red blood cells (x 109/L) | 4.90 | 4.55 | 5.27 |
| Hemoglobin (g/dL) | 15.40 | 14.34 | 16.38 |
| Hematocrit (%) | 42.60 | 40.04 | 45.16 |
| Mean corpuscular volume (fL) | 87.20 | 85.47 | 88.83 |
| Mean corpuscular hemoglobin (pg) | 31.30 | 30.58 | 31.94 |
| Mean corpuscular hemoglobin concentration (g/dL) | 35.70 | 35.16 | 36.22 |
| Platelets (x 109/L) | 246.20 | 212.60 | 279.70 |
| Methemoglobin (%) | 3.44 | 2.51 | 3.90 |
*Data obtained with two replicates
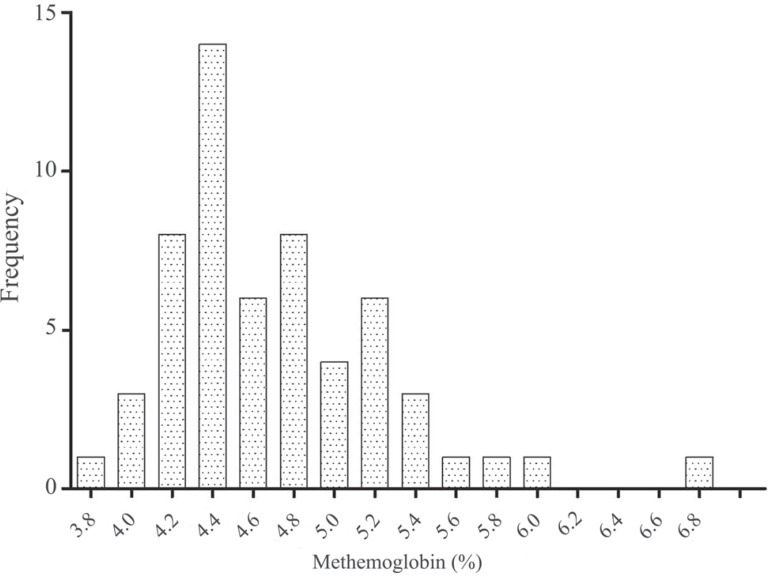
Figure 1 illustrates the percentage distribution of methemoglobin in children. All the calculations to determine references values were based on the guidelines of the National Council of Clinical Laboratory Services.(10) References ranges were obtained with 2.5 and 97.5 percentiles using the Statistica 8.0 (StatSoft) statistics package.
Figure 1.
Percentage distribution of methemoglobin in children
Discussion
The correct interpretation of laboratory results depends on establishing reliable reference values. Both State and private laboratory services must set up reference values for the population that they serve using their own techniques and equipment.(11) Although reference values have been known since the late 1940s and despite it being an important marker of oxidative metabolism, the introduction of the measurement of methemoglobin in the routine laboratory has always been difficult, mainly due to the potentially toxic technique created by Evelyn & Maloy(9) and by the high cost of techniques based on enzymatic quantification.
With a new technique developed by Naoum et al.,(4) that does not use sodium cyanide but is based on the specific light absorbance of oxyhemoglobin and methemoglobin, the determination of methemoglobin concentrations has become more feasible in the laboratory routine, thereby simplifying studies on cyanosis and associated conditions. The authors of this method demonstrated a positive correlation with the technique of Evelyn & Maloy(9) with the correlation coefficient r = 0.903.
Reference values for children (Table 1) ranged from 3.61 to 6.44% while for normal adults, using the method by Naoum et al.,(4) the values ranged from 1.9 to 3.8%. Thus, the results obtained in this work for children are higher than the reference values for adults. Our results therefore provide important information to correctly assess methemoglobin concentrations in children.
In addition to genetic causes and enzymatic deficiencies, the most frequent cause of high methemoglobin concentration is the ingestion of oxidizing agents, particularly in children. In childhood, the risk of developing toxic methemoglobinemia is greater, which can be explained by the smaller amount of soluble cofactor cytochrome b5 and the reduced activity of the cytochrome b5 reductase enzyme in red blood cells. Concentrations of the cytochrome b5 reductase enzyme is only about 60% of the concentration found in adult red blood cells.(12,13) This fact corroborates with the methemoglobin reference values described here.
Footnotes
Conflict-of-interest disclosure: The authors declare no competing financial interest
References
- 1. Bunn FH.Human hemoglobins: normal and abnormal; methemoglobinemia In: Nathan DG, Oski FA.Hematology of infancy and childhood. 4th ed Philadelphia: WB Saunders; 1993. p.698-731 [Google Scholar]
- 2. Prchal JT, Gregg XT.Red cell enzymes. Hematology Am Soc Hematol Educ Program. 2005: 19-23 [DOI] [PubMed] [Google Scholar]
- 3. Lee R, Foerster J, Lukens J, Paraskevas F, Greer J, Rodgers G.Wintrobe's clinical hematology. 10th ed Baltimore: Lippincott Williams & Wilkins; 1999. [Google Scholar]
- 4. Naoum PC, Radispiel J, Moraes MS.Dosagem espectométrica de metahemoglobina sem interferentes químicos ou enzimáticos. Rev Bras Hematol Hemoter. 2004; 26(1): 19-22 [Google Scholar]
- 5. Vives Corrons JL.Introducción al estudio de la anemia. Aspectos generales del diagnóstico In: Sans Sabrafen J, Besses Raebel C, Vives Corrons JL.Hematología clínica. 3rd ed Barcelona: Harcourt, 1994. p. 222 [Google Scholar]
- 6. Naoum PC.Diagnóstico das hemoglobinopatias. São Paulo: Sarvier, 1987. [Google Scholar]
- 7. Hoffman R, Benz Jr EJ, Shattil SJ, Furie B, Cohen HJ, Silberstein LE, et al. Hematology basic principles and practice. 4th ed Philadelphia: Elsevier; 2005. [Google Scholar]
- 8. Kaushansky K, Lichtman MA, Beutler E, Kipps TJ, Seligsohn U, Prchal J.Williams hematology. 8th ed New York: McGraw Hill; 2011. [Google Scholar]
- 9. Evelyn KA, Malloy HT.Microdetermination of oxyhemoglobin, methemoglobin and sulfhemoglobin in single simple of blood. J Biol Chem. 1938; 126: 655-7 [Google Scholar]
- 10. Tetrault GA.Laboratory statistics In: Harry JB.Clinical diagnosis and management by laboratory methods. 20th ed Philadelphia: Saunders; 2000. p.138-47 [Google Scholar]
- 11. Bain BJ.Células sangüíneas. 3rd ed Porto Alegre: Artes Médicas, 2004. [Google Scholar]
- 12. Bartos HR, Desforges JF.Red blood cells DPNH-dependent diaphorase levels in infants. Pediatrics. 1966; 37(6): 991-3 [PubMed] [Google Scholar]
- 13. Ross JD.Deficient activity of DPNH-dependent methemoglobin diaphorase in cord blood red blood cells. Blood. 1963; 21: 51-62 [PubMed] [Google Scholar]