It has become increasingly common for UK patients to travel to malarial regions: in 2004 over 2.5 million visits were made by UK individuals to countries in which malaria is endemic, representing a 300% increase since 1987.1 Malaria prophylaxis routinely provided in general practice comprises atovaquone–proguanil, mefloquine, doxycycline, or chloroquine plus proguanil. This article describes two cases of malaria that presented 8 months after foreign travel, despite adherence to antimalarial prophylaxis.
CASE REPORT
Two 16-year-old boys presented to the same UK hospital during the same week. Both had a 2-week history of unexplained fever and myalgia. They had travelled together to a malarious area of Kenya for a fortnight 8 months previously on a school trip, and had shared a tent. Both pupils reported adherence to a complete course of atovaquone–proguanil (Malarone®, GSK) on this trip, and had not been to any other malarious regions subsequently. Neither patient reported symptoms at the time of the trip or on initial return to the UK; nor were any other pupils or staff member on the Kenya trip unwell.
Apart from fever, routine physical examination was normal. Thick and thin blood films confirmed the presence of malarial parasites, but rapid antigen detection tests (RDTs) were negative. The diagnosis was confirmed as Plasmodium ovale, with a parasitaemia of 1–2%, by the Hospital for Tropical Diseases in London.
These cases raised two questions: how likely is P. ovale to occur after an asymptomatic latency of 8 months; and how likely is P. ovale to occur in travellers who have completed the recommended course of chemoprophylaxis?
DISCUSSION
In most places where P. ovale is found (usually West Africa, Indonesia, and the Philippines) its prevalence remains relatively low. Field surveys in Africa suggest between 0.5–2.4% of all malaria cases are due to P. ovale.2 It is rarely life-threatening, but there are case reports of severe sequelae from P. ovale infection such as pericarditis,3 acute respiratory distress syndrome,4 and very rarely splenic rupture,5 which can be fatal. P. ovale, along with P. vivax, may cause recurrent or relapsing flu-like symptoms, due to either low grade parasitaemia from a primary attack or to relapses from dormant hypnozoite stages in the liver.
The key to early diagnosis of P. ovale infection is for GPs to consider the diagnosis when the patient presents to primary care, and to request the appropriate laboratory test when the history is suggestive of malaria. Routinely available diagnostic tests such as RDTs and light microscopy are not very sensitive for P. ovale. It is important to request thick and thin blood films daily for 3 days before exclusion of the diagnosis of malaria and, if malaria is still suspected at that point, to discuss with a tropical disease unit. When P. ovale is suspected, sensitivity may be increased considerably if films are reviewed by experienced staff in an expert laboratory.6 Polymerase chain reaction further enhances diagnostic sensitivity.
P. ovale and P. vivax can remain dormant in hepatocytes as hypnozoites: a latent stage that may reactivate some months later. In some cases, there is no detectable primary infection, but relapses (defined as hypnozoite-induced peripheral blood parasitaemia) can occur up to 45 months after an asymptomatic primary infection.7 Thus 8 months latency is compatible in P. ovale and reinforces the importance of primary care clinicians obtaining a travel history that extends back beyond recent holidays.
A further feature leading to delayed diagnosis may be the patient’s history of taking appropriate antimalarials. P. falciparum is the main target for malaria chemoprophylaxis in travellers, and all the commonly prescribed antimalarials such as atovaquone–proguanil, mefloquine, doxycycline, and chloroquine plus proguanil are ineffective against hypnozoites of P. ovale or P. vivax. The only agent known to be effective against liver-stage hypnozoites is primaquine, which is contraindicated in pregnancy and glucose-6-phosphate dehydrogenase deficiency. Since presumptive terminal prophylaxis with primaquine is not routinely recommended in returning travellers, it is important to obtain a prompt diagnosis when clinical symptoms do arise and to treat appropriately.
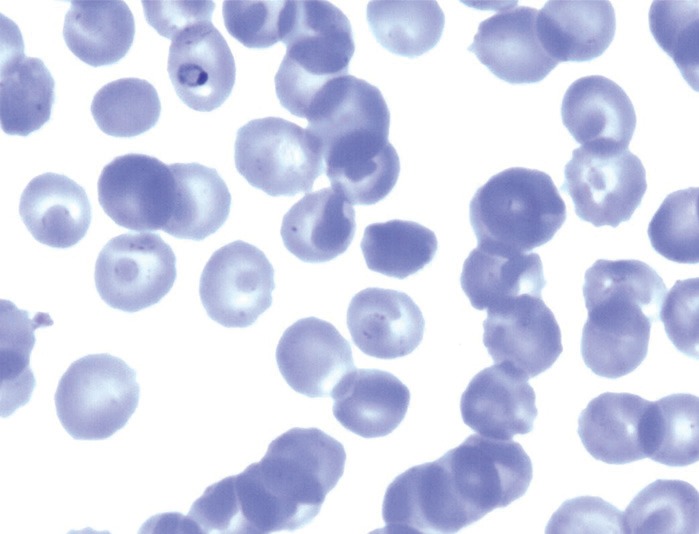
Isolates of Plasmodium ovale in culture.
Credit: Sharan Atwal & Colin Sutherland, LSHTM.
With the potential for long latency, low rapid test sensitivity, and ineffectiveness of standard chemoprophylaxis against hypnozoites, it is important that GPs consider the diagnosis of relapsing malaria species when assessing the febrile traveller. P. ovale infection is clinically less severe than P. falciparum, yet morbidity from recurring symptoms and rare complications can occur. Prescribers should be reminded that the most important aim of the antimalarial guidelines7 is to prevent deaths from P. falciparum infection and the chemoprophylactic agents deployed are not effective against delayed primary attacks or true relapses of P. ovale or P. vivax.
In the cases reported here letters were sent to others on the same school trip, and to advise their GPs of the potential for similar presentations by students and staff from the trip. To date, the authors are not aware of any who have done so.
Consent statement
The patients have provided written consent for this article to be published.
Provenance
Freely submitted; externally peer reviewed.
Discuss this article
Contribute and read comments about this article on the Discussion Forum: http://www.rcgp.org.uk/bjgp-discuss
REFERENCES
- 1.Smith AD, Bradley DJ, Smith V, et al. Imported malaria and high risk groups: observational study using UK surveillance data 1987–2006. BMJ. 2008;337:a120. doi: 10.1136/bmj.a120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Collins WE, Jeffery GM. Plasmodium ovale: parasite and disease. Clin Microbiol Rev. 2005;18(3):570–581. doi: 10.1128/CMR.18.3.570-581.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Coton T, Debourdeau P, Schoenlaub P, et al. [Acute pericarditis associated with Plasmodium ovale malaria] Med Trop (Mars) 2011;71(1):79–80. [PubMed] [Google Scholar]
- 4.Rojo-Marcos G, Cuadros-González J, Mesa-Latorre JM, et al. Acute respiratory distress syndrome in a case of Plasmodium ovale malaria. Am J Trop Med Hyg. 2008;79(3):391–393. [PubMed] [Google Scholar]
- 5.Patel M. Spontaneous rupture of a malarial spleen. Med J Aust. 1993;159(11–12):836–837. doi: 10.5694/j.1326-5377.1993.tb141386.x. [DOI] [PubMed] [Google Scholar]
- 6.Brent AJ, Angus BJ. Not all that is malaria is falciparum. Lancet Infect Dis. 2008;8(3):208. doi: 10.1016/S1473-3099(08)70044-6. [DOI] [PubMed] [Google Scholar]
- 7.Trager W, Most H. A long-delayed primary attack of ovale malaria. Am J Trop Med Hyg. 1963;12(6):837–839. doi: 10.4269/ajtmh.1963.12.837. [DOI] [PubMed] [Google Scholar]


