Abstract
Purpose
To evaluate the outcome of visual internal urethrotomy with a holmium:yttrium-aluminum-garnet laser along with intralesional triamcinolone injection.
Materials and Methods
Patients with an anterior urethral stricture less than 3 cm in length were evaluated by clinical history, physical examination, uroflowmetry, and retrograde urethrogram preoperatively. All patients were treated with holmium laser urethrotomy and intralesional triamcinolone (80 mg) injection under general or regional anesthesia. An 18 F urethral catheter was placed for 5 days. All patients were followed up for 12 months postoperatively by history, uroflowmetry, and if required, retrograde urethrogram or urethroscopy every 3 months.
Results
The mean age of the patients was 42.9 years (range, 14 to 70 years). The overall recurrence rate was 24%. The success rate in patients with strictures less than 1 cm in length was 95.8%, whereas that in patients with strictures of 1 to 3 cm in length was 57.7% (p=0.002). The outcome did not depend on age, duration of symptoms, etiology, or location of stricture.
Conclusions
Holmium laser urethrotomy with intralesional triamcinolone is a safe and effective minimally invasive therapeutic modality for urethral strictures. This procedure has an encouraging success rate, especially in those with stricture segments of less than 1 cm in length.
Keywords: Lasers, Laser therapy, Solid state, Triamcinolone acetonide, Urethral stricture
INTRODUCTION
Urethral stricture disease has always been a challenge for urologists. Many different treatment modalities are available for the treatment of urethral stricture disease, such as dilatation, urethrotomy, stent placement, and single or two-stage urethroplasty. Endoscopic treatment is usually advocated before various forms of urethroplasty are contemplated. Visual internal urethrotomy (VIU) is simple and safe, causes minimum inconvenience to the patient, and requires a short time off work. Holmium:yttrium-aluminum-garnet (Ho:YAG) laser endourethrotomy has an encouraging success rate, especially in those with short stricture segments and in those with primary strictures [1]. The reported success rates after single VIU range from 20 to 60% [2]. VIU does not provide an epithelial approximation but rather aims to separate the scarred epithelium so that healing occurs secondarily. If epithelialization progresses completely before wound contraction significantly narrows the lumen, the internal urethrotomy may be successful. If wound contraction significantly narrows the lumen before the completion of epithelialization, the stricture recurs [3]. Injection of steroids at the site of urethrotomy ostensibly prevents scar formation by enhancing endogenous collagenase and thus reducing the contracture rate. In this study we present our results for the use of intra-urethral steroid application simultaneously with Ho:YAG urethrotomy.
MATERIALS AND METHODS
After we received approval from the institutional ethical committee, a total of 50 patients with symptomatic urethral stricture (primary or secondary) presenting at our institute from July 2009 to June 2010 were treated by Ho:YAG urethrotomy with intralesional triamcinolone injection. Patients with completely obliterated urethral stricture and stricture length of more than 3 cm were excluded from the study. All patients were evaluated by complete history and physical examination, urine culture, uroflowmetry, and retrograde urethrography. Patients presenting for the first time for treatment were referred to as primary, whereas those who had undergone some procedure for the treatment of stricture prior to reporting to us were referred to as secondary. The procedure was done under general or regional anesthesia. All patients received antibiotic prophylaxis preoperatively. A Holmium laser at an energy of 1,200 to 1,400 mJ with a frequency of 10 to 15 Hz was used. This setting of energy and frequency was chosen because it seems to result in a satisfactory compromise of low depth of tissue penetration and low coagulation effect. By use of a 22 F cystoscope and Ho:YAG laser, the stricture site was completely incised while sparing healthy mucosa. After laser urethrotomy, 80 mg of triamcinolone (diluted with normal saline to 10 ml) was injected by using a Williams cystoscopic injection needle (5 F size and 23 G needle size, Cook Medical Inc, Bloomington, IN, USA) at 10 sites, 1 ml each, along the site of urethrotomy and circumferentially. An indwelling 18 F silicone catheter was left in place for 5 days. Antibiotic was continued until catheter removal. Post-procedure evaluation was done by history and uroflowmetry. The urine cultures were again repeated after the surgery on the second postoperative day. The patients with positive cultures received sensitive antibiotics. Retrograde urethrography was done in the postoperative period if the patient developed obstructive voiding symptoms or the flow rate was below 15 ml/sec. Follow-up was done at regular intervals for up to 12 months postoperatively. Any symptoms pertaining to recurrence were noted, such as reduced stream of urine, retention of urine, and burning micturition. The procedure was considered successful if the patient did not report any voiding difficulty and had a maximum flow rate >15 ml/sec for a voided volume of at least 150 ml. Urethral calibration or urethroscopy was done in case of voiding symptoms or reduction in maximum flow.
Chi-square tests of independence (with Fisher exact test where required) were used to test the association of intervention groups with various categorical variables. A p-value of less than 0.05 was considered significant.
RESULTS
The mean age of the patients was 42.9 years (range, 14 to 70 years). The mean duration of symptoms was 8.5 months (±10.5 months). The baseline characteristics of the patients including etiology, type, location, and length of the stricture are given in Table 1. The mean preoperative Qmax was 4.19 ml/sec and postoperative Qmax was13.2 ml/sec. We found that decreased stream of urine, frequency, and burning micturition were the most common symptoms with which patients presented.
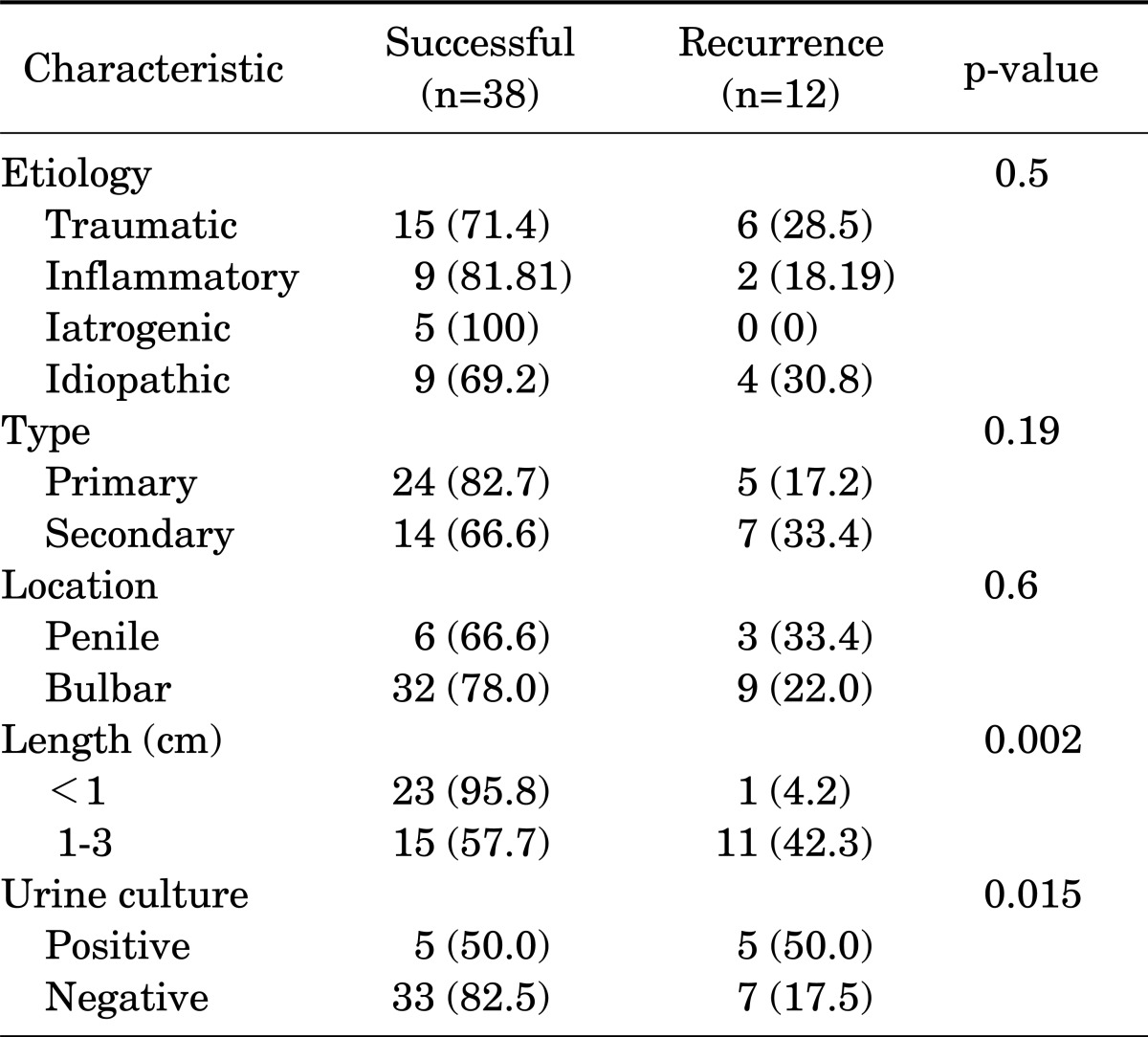
TABLE 1.
Comparison of stricture characteristics between those who had a successful outcome and those who experienced recurrence
Values are presented as number (%).
The overall success rate after Ho:laser urethrotomy and triamcinolone in our study was 76%. There were no significant perioperative complications related to the procedure. Of the 12 patients who experienced recurrence, 11 (42.3%) were patients with strictures of 1 to 3 cm in length and only 1 (4.2%) was a patient with a stricture length <1 cm (Table 1). Thus, the success rate was significantly better in patients with a stricture length <1 cm than in those with a stricture length of 1 to 3 cm (p=0.002). Among the 12 patients in whom recurrence was seen, urine cultures were sterile in 7 of those (58.3%), whereas 33 of 38 successful cases (86.8%) had sterile urine cultures. This was found to be statistically significant by applying Pearson's chi-square test (p=0.015).
In the logistic regression analysis, only the length of stricture was associated with stricture recurrence (p=0.011). All other factors were insignificant (p-value>0.05).
DISCUSSION
The estimated incidence of male urethral stricture disease is as high as 0.6% [4]. In addition to the burden of the disease itself, therapy for strictures can be associated with further complications, the most important being recurrence [5]. Etiologic factors for urethral stricture disease include perineal trauma, urethral catheterization, urologic instrumentation, chronic inflammatory diseases such as lichen sclerosus, and sexually transmitted diseases. However, most cases of urethral strictures are idiopathic, and most patients probably have unrecognized childhood trauma [6]. The first identifiable change in urethral stricture disease is a change in the nature of the urethral epithelium from a pseudo-stratified columnar epithelium to a columnar epithelium that lacks the waterproofing quality of the pseudo-stratified variant. Consequently, urine can extravasate and induce fibrosis [7]. If any medication or intervention can delay wound contraction at this stage, the probability of recurrent stricture may decrease. Steroids are known to decrease the amount of collagen fibers and fibroblasts and to inhibit the proliferation of fibroblasts in wound tissue [6]. This was the basis for including intralesional triamcinolone injection in our study.
Endoscopic urethrotomy was introduced 37 years ago by Sachse, who used the cold knife technique [8]. Success rates are unsatisfactory owing to scar tissue, and recurrence rates between 35% and 60% have been reported [1]. In our study including 50 male patients with urethral stricture disease, the success rate was 76%, being 95.8% for strictures less than 1 cm and 57.7% for strictures of 1 to 3 cm.
The length of follow-up is very important when assessing the success of internal urethrotomy and the rate of stricture recurrence. Several authors have shown that there is an attrition rate of 10 to 20% per year, which could continue for up to 5 years after VIU. Most reports show that if recurrence occurs it is most likely to do so within 3 to 12 months [2]. Rapp et al. [9] in their survey on management trends of urethral strictures found that when stricture length is less than 1 cm, 70% of urologists prefer VIU, whereas in cases with stricture lengths of 3 cm or more, most urologists (56%) proceed directly to urethroplasty. For a stricture less than 1 cm with minimal associated spongiofibrosis, VIU can have a long-term success rate. On the other hand, stricture excision and primary anastomosis as the initial treatment for a similar 2-cm stricture is highly efficacious (greater than 95%) but unfortunately incurs a higher initial surgical cost [10]. It has been shown that the most cost-effective strategy for the management of short, bulbar urethral strictures is to reserve urethroplasty for patients in whom a single endoscopic attempt fails. For longer strictures for which the success rate of VIU is expected to be less than 35%, urethroplasty as the primary therapy is cost-effective [11]. The use of lasers in urology started with the study by Parsons et al. [12], which investigated the effect of lasers in canine bladder. Over the past two decades, the use of lasers in urology has grown tremendously. Matsuoka et al. [13] commented on the use of Holmium lasers for antegrade incisions for various stricture lengths and stated that the lasers can ablate tissue through vaporization with minimal thermal damage to adjacent healthy tissue. Introduction of the Holmium laser as a treatment modality for urethral stricture disease has produced good results. Kural et al. [14] in their study on 13 patients reported a success rate of 69% and Matsuoka et al in their study on 31 patients reported a success rate of 74%. Hayashi et al. [15] reported successful treatment of recurrent vesicourethral strictures after radical prostatectomy with a holmium laser. Xiao et al. [16] in 2008 performed Ho:YAG laser urethrotomy on 38 patients with male urethral stricture disease and after 18 months of follow-up in 32 of those patients, recurrence was noted in only 6 patients, thus giving a success rate of 84%. In a randomized clinical trial, Atak et al. [17] demonstrated the superiority of Ho:YAG laser urethrotomy over cold knife VIU (81% vs. 53% success rate at 12 months, p=0.04).
Previously, results have varied pertaining to the role of etiology in the outcome of laser urethrotomy. Higher success rates have been achieved with iatrogenic strictures than with posttraumatic or post-inflammatory etiology [5]. In our study, the etiology of stricture was not found to be associated with the outcome of laser urethrotomy. In our study, the recurrence rate was found to be independent of the age of the patient, duration of symptoms, etiology of stricture, type of stricture (whether primary or secondary), and location of stricture (whether penile or bulbar urethra), whereas the factors that affected outcome were length of stricture and urinary infection. Long strictures are often associated with inflammatory diseases, repeated urethral dilations and instrumentations, history of prolonged urethral catheterization, and/or traumatic urethral distraction. Ninety-five percent of the total recurrences in our study were seen in patients with strictures of 1 to 3 cm in length. In the study by Kamp et al. [1], most of the recurrences were seen in patients with long-segment strictures of >1.5 cm. Our result of better outcome in strictures less than 1 cm is in accordance with a study done by Rourke and Jordan [10], who showed that initial therapy with direct urethrotomy would be beneficial in strictures less than 1 cm, with minimal associated spongiofibrosis. Hosseini et al. [18] also reported better outcome in short strictures of <1 cm (recurrence 4.2%) as compared with longer ones (recurrence 42.9%). Several studies have shown that shorter strictures respond to endoscopic intervention more readily than do longer strictures, and success rates as high as 85 to 87% have been reported for strictures shorter than 1 cm [5]. Our study had a success rate of 95.8% in strictures shorter than 1 cm. We included patients with strictures longer than 1 cm in our study only when they refused urethroplasty because of preference for minimally invasive surgery or socioeconomic reasons after the pros and cons of both options had been fully explained. Stricture recurrence has been shown to be directly proportional to stricture length. Pansadoro and Emiliozzi [19] demonstrated a high recurrence rate for strictures greater than 1 cm in size. Recurrence rates range from 51 to 72% in the various studies [20-22]. Compared with these studies, our recurrence rate was 42.3% in strictures of more than 1 cm in length. The vaporization of the fibrotic segments by laser may have played a role in the lower recurrence than in other studies. However, these results need to be reproduced in other studies to validate the utility of this modality in the treatment of long-segment strictures.
Urinary tract infection in the perioperative period was found to affect the results in our study. Five out of 12 total recurrences had positive urine cultures (41.7%), whereas only 5 of 38 successful patients had positive urine cultures (13.2%). Boccon Gibod and Le Portz [20] reported that length, location, cause of stricture, and urinary tract infection were factors affecting the outcome. Some of our patients continued to have positive urine cultures despite being treated with culture-specific antibiotics, because the stricture itself was the cause of the persistence of bacteriuria. It remains to be seen whether inserting a temporary suprapubic catheter to clear urinary tract infection before urethrotomy will improve success rates. The presence of prior colonization in the face of multiple interventions or the infection-related reaction of the local tissues may influence the extent of injury and reaction of the spongiosa and thus increase the incidence of spongiofibrosis. Thus, we feel the presence of infection increases the chances of recurrence.
Previous interventions in the form of dilatations or urethrotomy have a significant effect on the outcome as shown in studies by Niesel et al. [5] and Boccon Gibod and Boccon Gibod [20]. In our study of 29 primary cases, recurrence was seen in 5 patients (17.4%), whereas among 21 secondary cases, recurrence was seen in 7 patients (33%). However, the difference was not statistically significant. Moreover, 62% of the primary strictures were of <1 cm, whereas only 28.6% of secondary strictures were <1 cm. This could well explain the small difference in outcome in the patients with primary and secondary strictures.
The reported recurrence rates with VIU are high, ranging from 30 to 58%. Various attempts have been made to reduce the recurrence noted with VIU, such as repeated multiple incisions in the circumference of the stricture, combining urethrotomy with hydraulic self-dilatation, endoscopic resection of callus, intraurethral mitomycin C [23], intraurethral captopril gel [24], intraurethral hyaluronic acid [25], and urethrotomy combined with postoperative intermittent dilatation by clean intermittent self-catheterization [26]. One such attempt was injection of steroids, such as of triamcinolone acetonide [27]. The mechanism of action of topical steroids remains largely unknown; the effect is probably due to the inhibition and down-regulation of collagen synthesis. Also, steroids increase the activity of collagenase enzyme, which breaks down collagen so that scars become less thick. Topical corticosteroids improve meatal elasticity, which in turn facilitates calibration/dilatation, and prevents the formation of meatal stenosis [28]. Nabi and Dogra [29] supported the use of intralesional steroid with the Nd:YAG laser in the treatment of traumatic prostatic and supraprostatic strictures. In their study at a mean follow-up of 23 months, all three patients were asymptomatic and voiding well and were found to have normal results on cystoscopy, urethroscopy, and uroflowmetry done at 3 months. Hosseini et al. [18] compared patients undergoing clean intermittent catheterization with or without triamcinolone ointment following internal urethrotomy. At a follow-up of 12 months, recurrence was noted in 30% in the triamcinolone group compared with 44% in the other. In a small series of 24 patients, Eltahawy et al. [30] used Holmium laser bladder neck incision combined with steroid injection for anastomotic stenosis after radical prostatectomy and had a success rate of 83%.
In our study, 21 patients had received treatment earlier in the form of dilatation or VIU. Those patients had a reasonable success rate of 66%, thus proving the role of Ho:YAG laser and intralesional steroids in recurrent strictures also. The limitations of our study include a relatively small number of patients and a relatively short follow-up period. The mean follow-up of 16.4 months covered the critical period of stricture recurrence in the study by Gucuk et al. [6], because the majority of recurrences were seen at 18 months. A further limitation is the absence of control groups. A larger, randomized controlled study with longer follow-up is required to confirm these findings and to establish the overall efficacy of triamcinolone and Ho:YAG laser urethrotomy.
CONCLUSIONS
Ho:YAG laser urethrotomy with intralesional triamcinolone is a safe and effective minimally invasive therapeutic modality for urethral strictures. The addition of triamcinolone to Ho:laser therapy is easy and of low cost. This procedure has an encouraging success rate especially in those with short-segment strictures (<1 cm). The outcome of Ho:YAG laser urethrotomy does not depend on age, duration of symptoms, type of stricture, or location of stricture. Stricture length and preoperative positive urine culture have an important bearing on the outcome. For curative, long-term effects, this technique deserves to be tested on a large group of patients with special emphasis on objective verification of the safety and efficacy profile. The 66% success rate in patients who had received prior treatment in the form of dilatation or urethrotomy in our study shows that Ho:YAG laser urethrotomy can be reasonably effective in secondary strictures also. The precise tissue ablative property of the Ho:YAG laser along with the scar-preventing activity of triamcinolone by virtue of down-regulating collagen synthesis makes up an effective treatment modality for short-segment urethral stricture disease.
Footnotes
The authors have nothing to disclose.
References
- 1.Kamp S, Knoll T, Osman MM, Kohrmann KU, Michel MS, Alken P. Low-power holmium:YAG laser urethrotomy for treatment of urethral strictures: functional outcome and quality of life. J Endourol. 2006;20:38–41. doi: 10.1089/end.2006.20.38. [DOI] [PubMed] [Google Scholar]
- 2.Naude AM, Heyns CF. What is the place of internal urethrotomy in the treatment of urethral stricture disease? Nat Clin Pract Urol. 2005;2:538–545. doi: 10.1038/ncpuro0320. [DOI] [PubMed] [Google Scholar]
- 3.Jordan G, Schlossberg S. Urethral stricture disease. In: Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Campbell-Walsh urology. 9th ed. Philadelphia: Saunders; 2007. pp. 1054–1074. [Google Scholar]
- 4.Santucci RA, Joyce GF, Wise M. Male urethral stricture disease. J Urol. 2007;177:1667–1674. doi: 10.1016/j.juro.2007.01.041. [DOI] [PubMed] [Google Scholar]
- 5.Niesel T, Moore RG, Alfert HJ, Kavoussi LR. Alternative endoscopic management in the treatment of urethral strictures. J Endourol. 1995;9:31–39. doi: 10.1089/end.1995.9.31. [DOI] [PubMed] [Google Scholar]
- 6.Gucuk A, Tuygun C, Burgu B, Ozturk U, Dede O, Imamoglu A. The short-term efficacy of dilatation therapy combined with steroid after internal urethrotomy in the management of urethral stenoses. J Endourol. 2010;24:1017–1021. doi: 10.1089/end.2009.0233. [DOI] [PubMed] [Google Scholar]
- 7.Andrich DE, Mundy AR. Urethral strictures and their surgical treatment. BJU Int. 2000;86:571–580. doi: 10.1046/j.1464-410x.2000.00878.x. [DOI] [PubMed] [Google Scholar]
- 8.Sachse H. Treatment of urethral stricture: transurethral slit in view using sharp section. Fortschr Med. 1974;92:12–15. [PubMed] [Google Scholar]
- 9.Rapp DE, Chanduri K, Infusino G, Hoda ZA, Orvieto MA, Elliott SP, et al. Internet survey of management trends of urethral strictures. Urol Int. 2008;80:287–290. doi: 10.1159/000127343. [DOI] [PubMed] [Google Scholar]
- 10.Rourke KF, Jordan GH. Primary urethral reconstruction: the cost minimized approach to the bulbous urethral stricture. J Urol. 2005;173:1206–1210. doi: 10.1097/01.ju.0000154971.05286.81. [DOI] [PubMed] [Google Scholar]
- 11.Wright JL, Wessells H, Nathens AB, Hollingworth W. What is the most cost-effective treatment for 1 to 2-cm bulbar urethral strictures: societal approach using decision analysis. Urology. 2006;67:889–893. doi: 10.1016/j.urology.2005.11.003. [DOI] [PubMed] [Google Scholar]
- 12.Parsons RL, Campbell JL, Thomley MW, Butt CG, Gordon TE., Jr The effect of the laser of dog bladders: a preliminary report. J Urol. 1966;95:716–717. doi: 10.1016/S0022-5347(17)63525-0. [DOI] [PubMed] [Google Scholar]
- 13.Matsuoka K, Inoue M, Iida S, Tomiyasu K, Noda S. Endoscopic antegrade laser incision in the treatment of urethral stricture. Urology. 2002;60:968–972. doi: 10.1016/s0090-4295(02)01994-5. [DOI] [PubMed] [Google Scholar]
- 14.Kural AR, Coskuner ER, Cevik I. Holmium laser ablation of recurrent strictures of urethra and bladder neck: preliminary results. J Endourol. 2000;14:301–304. doi: 10.1089/end.2000.14.301. [DOI] [PubMed] [Google Scholar]
- 15.Hayashi T, Yoshinaga A, Ohno R, Ishii N, Watanabe T, Yamada T, et al. Successful treatment of recurrent vesicourethral stricture after radical prostatectomy with holmium laser: report of three cases. Int J Urol. 2005;12:414–416. doi: 10.1111/j.1442-2042.2005.01053.x. [DOI] [PubMed] [Google Scholar]
- 16.Xiao J, Wu B, Chen LW, Qi L, Zhu YP, Su H, et al. Holmium laser urethrotomy for male urethral stricture. Zhonghua Nan Ke Xue. 2008;14:734–736. [PubMed] [Google Scholar]
- 17.Atak M, Tokgoz H, Akduman B, Erol B, Donmez I, Hancı V, et al. Low-power holmium:YAG laser urethrotomy for urethral stricture disease: comparison of outcomes with the cold-knife technique. Kaohsiung J Med Sci. 2011;27:503–507. doi: 10.1016/j.kjms.2011.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hosseini J, Kaviani A, Golshan AR. Clean intermittent catheterization with triamcinolone ointment following internal urethrotomy. Urol J. 2008;5:265–268. [PubMed] [Google Scholar]
- 19.Pansadoro V, Emiliozzi P. Internal urethrotomy in the management of anterior urethral strictures: long-term followup. J Urol. 1996;156:73–75. [PubMed] [Google Scholar]
- 20.Boccon Gibod L, Le Portz B. Endoscopic urethrotomy: does it live up to its promises? J Urol. 1982;127:433–435. doi: 10.1016/s0022-5347(17)53849-5. [DOI] [PubMed] [Google Scholar]
- 21.Ishigooka M, Tomaru M, Hashimoto T, Sasagawa I, Nakada T, Mitobe K. Recurrence of urethral stricture after single internal urethrotomy. Int Urol Nephrol. 1995;27:101–106. doi: 10.1007/BF02575227. [DOI] [PubMed] [Google Scholar]
- 22.Zehri AA, Ather MH, Afshan Q. Predictors of recurrence of urethral stricture disease following optical urethrotomy. Int J Surg. 2009;7:361–364. doi: 10.1016/j.ijsu.2009.05.010. [DOI] [PubMed] [Google Scholar]
- 23.Ayyildiz A, Nuhoglu B, Gulerkaya B, Caydere M, Ustun H, Germiyanoglu C, et al. Effect of intraurethral Mitomycin-C on healing and fibrosis in rats with experimentally induced urethral stricture. Int J Urol. 2004;11:1122–1126. doi: 10.1111/j.1442-2042.2004.00959.x. [DOI] [PubMed] [Google Scholar]
- 24.Shirazi M, Khezri A, Samani SM, Monabbati A, Kojoori J, Hassanpour A. Effect of intraurethral captopril gel on the recurrence of urethral stricture after direct vision internal urethrotomy: Phase II clinical trial. Int J Urol. 2007;14:203–208. doi: 10.1111/j.1442-2042.2007.01693.x. [DOI] [PubMed] [Google Scholar]
- 25.Da-Silva EA, Sampaio FJ, Dornas MC, Damiao R, Cardoso LE. Extracellular matrix changes in urethral stricture disease. J Urol. 2002;168:805–807. [PubMed] [Google Scholar]
- 26.Bødker A, Ostri P, Rye-Andersen J, Edvardsen L, Struckmann J. Treatment of recurrent urethral stricture by internal urethrotomy and intermittent self-catheterization: a controlled study of a new therapy. J Urol. 1992;148(2 Pt 1):308–310. doi: 10.1016/s0022-5347(17)36580-1. [DOI] [PubMed] [Google Scholar]
- 27.Heyns CF, Steenkamp JW, De Kock ML, Whitaker P. Treatment of male urethral strictures: is repeated dilation or internal urethrotomy useful? J Urol. 1998;160:356–358. doi: 10.1016/s0022-5347(01)62894-5. [DOI] [PubMed] [Google Scholar]
- 28.Radojicic ZI, Perovic SV, Stojanoski KD. Calibration and dilatation with topical corticosteroid in the treatment of stenosis of neourethral meatus after hypospadias repair. BJU Int. 2006;97:166–168. doi: 10.1111/j.1464-410X.2006.05870.x. [DOI] [PubMed] [Google Scholar]
- 29.Nabi G, Dogra PN. Endoscopic management of post-traumatic prostatic and supraprostatic strictures using Neodymium-YAG laser. Int J Urol. 2002;9:710–714. doi: 10.1046/j.1442-2042.2002.00540.x. [DOI] [PubMed] [Google Scholar]
- 30.Eltahawy E, Gur U, Virasoro R, Schlossberg SM, Jordan GH. Management of recurrent anastomotic stenosis following radical prostatectomy using holmium laser and steroid injection. BJU Int. 2008;102:796–798. doi: 10.1111/j.1464-410X.2008.07919.x. [DOI] [PubMed] [Google Scholar]