Abstract
Purpose
Bipolar hemiarthroplasty (BHA) for idiopathic osteonecrosis of the femoral head (ONFH) is performed at our institution. The purpose of this study was to evaluate the clinical and radiographic findings after BHA for the treatment of steroid -induced ONFH.
Methods
Thirty-seven hips in 27 patients were assessed (seven men, 11 hips; 20 women, 26 hips), average patient age at the time of surgery of 42.6 (range 20–83) years, with steroid-induced ONFH treated with BHA between 1995 and 2005. The mean follow-up duration was approximately ten (range five to15) years. Patients were evaluated according to the Japan Orthopaedic Association (JOA) hip score. Kaplan–Meier survivorship was calculated to examine revision arthroplasty failure rate. Radiographic analysis of loosening included radiolucent lines and osteolysis of the acetabulum or femur. Causes of loosening were analysed using multiple logistic regression.
Result
JOA hip score increased from 53 points (preoperative) to 87 points (final follow-up). Survival rates were 96.8 % and 78.6 % at ten and 15 years, respectively. Prosthesis loosening occurred on the acetabular side in five hips (13.5 %). No femoral-component loosening was observed. BHA had poor results in patients with Association Research Circulation Osseous (ARCO) stage IV ONFH and in patients under 40 years of age.
Conclusion
BHA, with strict surgical indications, may be a good option for treating ONFH. Based on these results, total hip arthroplasty is recommended for patients with ARCO stage IV ONFH or for patients under 40 years of age.
Introduction
Idiopathic osteonecrosis of the femoral head (ONFH) occurs frequently in young and middle-aged patients. In the natural course of ONFH, progressive destruction of the hip joint occurs in more than half of the cases, resulting in secondary osteoarthritis and causing severe hip pain and serious functional disorders [1, 2], often necessitating surgical treatment. The primary therapeutic strategy for ONFH in our institute is aimed at preserving the femoral head. In most cases of ONFH that are less than stage III of the Association Research Circulation Osseous (ARCO) [1, 3] classification, surgical interventions consist of osteotomy operations, such as transtrochanteric rotational osteotomy [4] and varus femoral osteotomy [5]. However, bipolar hemiarthroplasty (BHA) has been performed in cases with a wide necrotic area and in which collapse of the femoral head is expected. Indications for BHA and total hip arthroplasty (THA) vary slightly among hospitals, and there is controversy about which of the two procedures has a superior outcome [6–9]. For example, unfavourable clinical results after BHA have been reported, especially with mid- to long-term follow-up [8, 10–13]. Problems such as durability and persistent pain have been described, and physicians in Western countries more often select THA [6, 14–16]. To date, the protocol in our institute has been to perform BHA for ARCO stage III or below ONFH based on the concept that BHA is a less invasive procedure, preserves range of motion of the hip joint, is associated with a low incidence of dislocation, and can spare more of the acetabular bone compared to THA.
However, in patients with steroid-induced ONFH, there is a concern for early proximal migration of the BHA due to steroid-induced secondary osteoporosis. To date, there have been no reports on the outcomes of BHA for treating ONFH that specifically focus on steroid-induced ONFH. The purpose of this study was to evaluate clinical and radiographic findings after BHA when treating patients with steroid-induced ONFH or to investigate risk factors associated with component loosening after BHA in these patients.
Materials and methods
The study was approved by the institutional review board, and informed consent was obtained from all patients. Between January 1995 and May 2004, 42 hips in 31 patients with steroid-induced ONFH underwent BHA. Five hips were excluded from analysis either due to the death of the patient related to medical causes (four hips ) or secondary to early transfer to another institution and loss to follow-up (one hip). The remaining 37 hips in 27 patients were included in this study (seven men, 11 hips; 20 women, 26 hips) with an average age at the time of surgery of 42.6 (range 20–83) years. Mean follow-up was 10.2 [standard deviation (SD) ± 2.9 ] years (range five to 15 years). The underlying diseases associated with steroid -induced ONFH included systemic lupus erythematosus (SLE) (18 patients), Vogt-Koyanagi-Harada disease (three patients), rheumatoid arthritis, polyarthritis (two patients), polyarteritis nodosa (one patient), brain tumour (one patient), reflux nephropathy (one patient), and other (one patient). The diagnosis of ONFH was made based on clinical history, preoperative radiographic evaluation that included anteroposterior (AP) and lateral radiographs, bone scans, and magnetic resonance imaging (MRI), and was confirmed after surgery using histological examination. ONFH was staged preoperatively according to the ARCO staging system. In our institute, BHA has been performed for ARCO stages II and III, in which the articular cartilage plate is preserved. BHA was also performed on two hips with apparent partial narrowing of the joint space consistent with ARCO stage IV but which did not have acetabular bone deformity and no risk of outer head dislocation. These two hips were on the same patient, who had previously undergone bilateral transtrochanteric anterior rotational osteotomies. Therefore, in this study, there were seven hips at stage II, 28 hips at stage III, and two hips at stage IV.
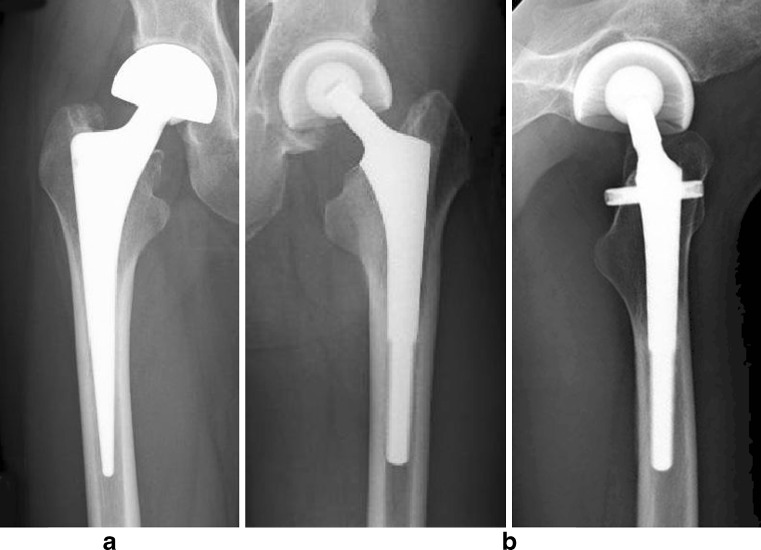
The same surgical technique was performed in all patients. A posterolateral approach was used and the capsule was repaired in order to prevent dislocation. The acetabulum was not reamed, in order to preserve the cartilage. Two types of cementless stems were used: the CLS Spotorno stem (Zimmer, Warsaw, IN, USA), which has a tapered wedge with a rough-blasted microporous surface and no porous coating, in 18 hips from 1995 to 1998, and the Intra -Medullary Cruciate (IMC) stem (Kyocera Medical Corporation, Osaka, Japan), which has a proximal porous coat and transverse locking pin, in 19 hips after 1998 (Fig. 1).
Fig. 1.
Two types of cementless stems were used: a The CLS stem, which has a tapered wedge with a rough-blasted microporous surface and no porous coating, in 18 hips from 1995 to 1998. b the Intra -Medullary Cruciate (IMC) stem, which has a proximal porous coat and transverse locking pin in 19 hips after 1998
Clinical results were evaluated using the criteria published by the Japan Orthopaedic Association (JOA); the hip score before surgery and at the time of the final follow-up were assessed [17]. JOA score ranges from 0 to 100 points, with points assigned as follows: pain 0–40 points; range of motion 0–20 points; walking ability 0–20 points; and daily activity 0–20 points. For cases that required revision, the hip score was evaluated just prior to revision surgery. The cumulative survival rates were evaluated using the Kaplan–Meier method, with conversion to THA or loosening of the prosthesis used as endpoints.
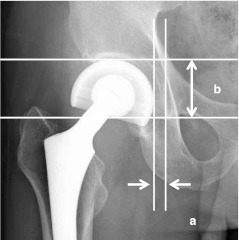
On the acetabular side, proximal migration of the bipolar head was assessed superiorly, medially, and in total on AP radiographs. Superior migration was assessed by measuring the distance between the superior margin of the bipolar head and the vertical line perpendicular to the baseline of the teardrops. Medial migration was assessed by measuring the distance between the medial margin of the bipolar head and the medial plate of the pelvis (Fig. 2). Acetabular side loosening was defined as a change of over two millimetres in the superior or medial direction of the outer head migration at the time of last follow-up. Prosthesis loosening was evaluated using AP radiographs taken immediately after surgery and at the time of the final follow-up. Femoral component fixation was graded as radiographic ingrowth, according to the criteria described by Engh et al. [18]. Loosening was defined as the presence of a radiolucent line around the stem or over five millimetres of subsidence.
Fig. 2.
Proximal migration of the bipolar head on an anteroposterior (AP) radiograph: a Superior migration was assessed by measuring the distance between the superior margin of the bipolar head and the vertical line perpendicular to the baseline of the teardrops. b Medial migration was assessed by measuring the distance between the medial margin of the bipolar head and the medial plate of the pelvis
Statistical analysis was performed using a multiple logistic regression analysis. Risk factors for loosing, such as sex, age and weight at surgery, number of joints affected, and preoperative ONFH stage were examined. A p value < 0.05 was chosen to indicate statistical significance. Component loosening was compared across the two groups of patients (< 40 years of age and ≧ 40 years of age) with a log-rank test.
Results
Clinical results showed an increase in JOA hip score from a preoperative average of 53 ± 14.8 (range:16–83) to 87 ± 10.3 (range 57–97) at the time of the final follow-up (Table 1). Continuous pain during gait (JOA < 20) was present in only two hips (5.4 %). Two hips (5.4 %) dislocated to the point of disassembly.
Table 1.
Average Japan Orthopaedic Association (JOA) hip score increased from a preoperative average of 53 points to 87 points at the time of the final follow-up
| Scoring items | Preoperative score mean ± SD | Score at the last follow-up mean ± SD |
|---|---|---|
| Pain (0–40) | 16 | 37 |
| ROM (0–20) | 16 | 18 |
| Ability to walk (0–20) | 10 | 15 |
| ADL (0–20) | 11 | 17 |
| Total | 53 ± 14.8 | 87 ± 10.3 |
Maintained gait pain (JOA < 20): 2/37 hips (5.4 %)
ROM range of motion, ADL activities of daily living, SD standard deviation
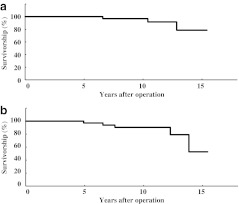
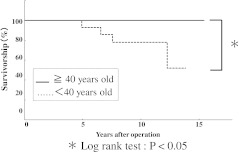
Prosthesis loosening occurred in five hips (13.5 %) on the acetabular side; no loosening was observed around the femoral component. At last follow-up, all cases showed stable or fibrous-stable radiographic fixation according to criteria established by Engh et al. [18]. Revision THA was performed on three hips (8.1 %) during this study. Survival rates with revision THA as the end point were 96.8 % at ten years and 78.6 % at 15 years (Fig. 3a). Survival rates with prosthesis loosening as the end point were 90.4 % at ten years and 52.7 % at 15 years (Fig. 3b). Multiple logistic regression analysis showed a significant difference in preoperative age at surgery and preoperative stage of necrosis on both univariate and multivariate analysis (P < 0.01) (Table 2). Component loosening (which only occurred on the acetabular side) was worse in young patients and in patients with higher stages of necrosis. When patients were divided into two groups, under 40 years of age and over 40 years of age, a significant difference between groups was demonstrated for component loosening (log-rank test P < 0.05) (Fig. 4). Both hips with ARCO stage IV ONFH were disassembled and revised to THA. The revision rate was 3.5 % in patients with stage III and 100 % in patients with stage IV.
Fig. 3.
Kaplan–Meier survivorship analysis curve: a Survival rates with revision total hip arthroplasty (THA) as the end point were 96.8 % at 10 years and 78.6 % at 15 years. b Survival rates with prosthesis loosening as the end point were 90.4 % at 10 years and 52.7 % at 15 years
Table 2.
Multiple logistic regression analysis showed a significant difference in preoperative age at surgery and preoperative stage of necrosis for both univariate and multivariate analyses (P < 0.01)
| Univariable analysis | Multivariable analysis | |||||
|---|---|---|---|---|---|---|
| HR | 95 % CI | P value | HR | 95 % CI | P value | |
| Gender | 1.192 | 0.944–1.440 | P = 0.12 | 1.126 | 0.919–1.334 | P = 0.22 |
| Age | 0.999 | 0.983–0.999 | P = 0.01 | 0.992 | 0.982–1.000 | P < 0.01 |
| Weight | 0.992 | 0.981–1.006 | P = 0.22 | 1.001 | 0.988–1.019 | P = 0.72 |
| Number of joint | 1.182 | 0.892–1.473 | P = 0.22 | 1.099 | 0.868–1.331 | P = 0.39 |
| Necrosis stage | 1.332 | 1.111–1.554 | P < 0.01 | 1.285 | 1.090–1.479 | P < 0.01 |
HR hazard raito, CI confidence interval
Fig. 4.
When patients were divided into two groups, < 40 years of age and ≧ 40 years of age, a significant difference between groups was demonstrated for component loosening (log-rank test P < 0.05)
Discussion
Though corticosteroids are indicated for treating various diseases, there are few reports examining the incidence of steroid-induced ONFH according to the underlying disease. Fukushima et al. investigated a nationwide epidemiological survey in Japan [19] and estimated the number of patients who received medical care in 2004 was 11,400. In the 1,502 patients whose detailed information was available, the potential causative factors of ONFH were largely attributable to systemic steroid administration (51 %), with SLE reported most frequently (31 %). Shigemura et al. [20] investigated the relationship between underlying disease and risk factors for steroid-associated ONFH in a prospective MRI study. They reported that the incidence of ONFH was significantly higher in the SLE group than in the non-SLE group (37 % vs 21 %, P = 0.001). In our study, steroid treatment for SLE also accounted for a high percentage of cases (18 of 37 cases, 48.6 %).
The reason that patients with SLE may be predisposed to ONFH may be related to blood coagulation factors. Several studies indicated that haemostatic abnormalities caused by administration of corticosteroids are related to the development of ONFH. SLE is associated with antiphospholipid antibody syndrome, which is an autoimmune disorder characterised by recurrent thrombotic episodes. Tektonidou et al. [21] reported a case of ONFH developing in a patient with antiphospholipid antibody syndrome who was not being treated with corticosteroids. The appearance of ONFH should suggest SLE as a possible aetiological factor.
ONFH is a disease of the femoral head, for which BHA has been adapted. However, many reports of mid- to long-term results demonstrate unacceptably high rates of pain, migration, osteolysis, and the need for revision THA [6, 8, 11–13]. Ito et al. [13] reported results of BHA performed for ONFH of 48 hips in 35 patients with an average of 11.4 years follow-up, and they reported radiographic failures and groin symptoms present in 20 hips (42 %). However, 21 of these patients (60 %) had a history of steroid administration, seven hips in ARCO stage IV were included, and in five hips, reaming of the acetabular cartilage to the size of the outer prosthetic head was performed. These factors may have contributed to the poor outcomes. Our study showed a significant difference in preoperative age at surgery and preoperative stage of ONFH, demonstrated with both univariate and multivariate analyses (P < 0.01). It is important to note that both factors were important for the longevity of BHA.
One of the most important side effects of long-term steroid therapy is secondary osteoporosis. Bone loss occurs rapidly within the first six months and is greatest in cancellous bone. Patients with steroid-induced osteoporosis may have weak acetabular bone, which will cause migration of the femoral head, especially with no cartilage barrier. Young patients with steroid-induced ONFH tend to undergo long-term steroid therapy. Thus, these patients could be at a higher risk for secondary osteoporosis, and this may shorten the longevity of BHA.
The presence of the remaining cartilage is very important for the clinical results of BHA. Pellegrini et al. [22] investigated the results of BHA for treating degenerative arthritis and reported that over 90 % of cases with mechanical failure had undergone acetabular reaming. They concluded that preservation of acetabular articular cartilage at the time of BHA may provide a barrier that impedes the access of particulate debris to subchondral bone. To prevent varus displacement of the outer head and to improve durability of components, a centering mechanism has been developed for second-generation bipolar artificial femoral head implants, but this may be difficult to achieve in cases with osteoarthritis or acetabular reaming.
Difficulties may be due to the generation of a large amount of debris from wear of the polyethylene insert caused by impingement of the bipolar femoral neck on the edge of the outer head. A large amount of polyethylene wear debris may result in massive osteolysis, migration of the femoral head, and femoral-stem-component loosening during mid- to long-term follow-up. Therefore, the use of BHA has been associated with substantial failure rates. The two cases requiring revision in this study (ARCO stage IV) were dislocated to the point of disassembly, which, as described above, may have been caused by failure of the self-centering mechanism (Fig. 5a, b).
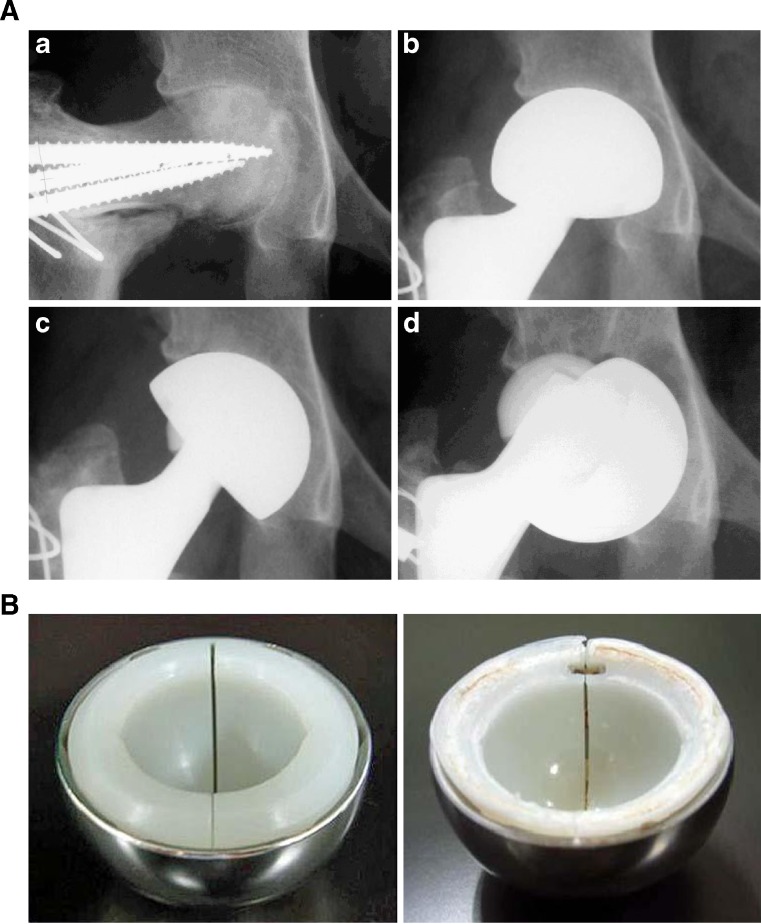
Fig. 5.
a Radiographs of osteonecrosis of the femoral head (ONFH) in a 21-year-old woman with systemic lupus erythematosus (SLE): A Preoperative radiograph demonstrating secondary osteoarthritis after anterior rotational osteotomy [Association Research Circulation Osseous (ARCO) stage IV]. B Radiograph after bipolar hemiarthroplasty. C Radiograph taken at the 3 -year follow-up showing superior acetabular migration and progressive varus displacement of the bipolar cup. D Seven years after surgery, disassembly of the bipolar cup occurred with hip flexion. b New (left) and retrieved (right) bipolar heads. The retrieved bipolar head shows apparent circumferential wear with failure of the self-centering mechanism
In recent years, the literature has increasingly supported BHA [7, 23], and some recent comparison studies concluded that BHA was superior to THA. In a report by Chan et al. [7], 28 patients with bilateral ONFH were treated with a cementless BHA in one hip and cementless THA in the other. Results showed that the hips that received THA had a higher complication rate associated with osteolysis (3.6 %) compared with hips in which BHA was performed (1.8 %). The most likely reason for these successful outcomes was that all patients had intact acetabular cartilage and acetabular reaming was not performed. Tsumura et al. [23] compared results of BHA divided into two groups with and without cartilage and found a statistically significant difference in superior migration, with the group without cartilage showing increased migration. The authors emphasised that BHA is indicated in cases in which the acetabular cartilage remains. Though no acetabular reaming was performed in our study in order to preserve the cartilage, two cases without cartilage (ARCO stage IV) were included. As a result, both cases required revision surgery.
There are other causes responsible for problematic outcomes associated with BHA in younger patients: These patients are more active and have a greater range of motion, which may extend beyond the oscillation angle, resulting in acetabular cartilage degeneration and other mechanical problems, such as rim wear. Moreover, steroid-induced ONFH in young patients directly inhibits osteoblastic bone formation and stimulates increased bone resorption [24, 25]. Kindsfater et al. [10] reported prosthesis survival rates up to eight years in a general group of patients with osteoarthritis, with intermediate-term clinical results of BHA being satisfactory independent of age and not related to underlying diagnosis. In our study, a significant difference in the incidence of loosening was found between patients under 40 years of age and older patients.
Nishii et al. [12] investigated the relationship of femoral endocortical osteolysis with age. The average age of the osteolysis group was 37.1 years and of the nonosteolytic group 45.7 years; there was a statistically significant difference between groups. This suggests that younger patients may have better outcomes with THA because good long-term results have been reported using THA for younger patients with ONFH [26, 27].
In conclusion, BHA, with strict surgical indications may be a good option for treatment of ONFH. Based on the results of this study, THA is recommended for patients with ARCO stage IV ONFH or for patients under 40 years of age.
References
- 1.Sugano N, Atsumi T, Ohzono K, Kubo T, Hotokebuchi T, Takaoka K. The 2001 revised criteria for diagnosis, classification, and staging of idiopathic ONFH of the femoral head. J Orthop Sci. 2002;7:601–605. doi: 10.1007/s007760200108. [DOI] [PubMed] [Google Scholar]
- 2.Bradway JK, Morrey BF. The natural history of the silent hip in birateral atraumatic ONFH. J Arthroplasty. 1993;8:383–387. doi: 10.1016/S0883-5403(06)80036-7. [DOI] [PubMed] [Google Scholar]
- 3.Marker DR, Seyler TM, McGrath MS, Delanois RE, Ulrich SD, Mont MA. Treatment of early stage ONFH of the femoral head. J Bone Joint Surg Am. 2008;90:175–187. doi: 10.2106/JBJS.H.00671. [DOI] [PubMed] [Google Scholar]
- 4.Yamamoto T, Ikemura S, Iwamoto Y, Sugioka Y. The repair process of ONFH after a transtrochanteric rotational osteotomy. Clin Orthop Relat Res. 2010;468:3186–3191. doi: 10.1007/s11999-010-1384-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ito H, Tanino H, Yamanaka Y, Nakamura T, Takahashi D, Minami A, Matsuno T. Long-term results of conventional varus half-wedge proximal femoral osteotomy for the treatment of ONFH of the femoral head. J Bone Joint Surg Br. 2012;94:308–314. doi: 10.1302/0301-620X.94B3.27814. [DOI] [PubMed] [Google Scholar]
- 6.Cabanera ME. Bipolar versus total hip arthroplasty for avascular necrosis of the femoral head. A comparison. Clin Orthop Relat Res. 1990;261:59–62. [PubMed] [Google Scholar]
- 7.Chan Y-S, Shih C-H. Bipolar versus total hip arthroplasty for hip ONFH in the same patient. Clin Orthop Relat Res. 2000;379:169–177. doi: 10.1097/00003086-200010000-00020. [DOI] [PubMed] [Google Scholar]
- 8.Lee SB, Sugano N, Nakata K, Matsui M, Ohzono K. Comparison between bipolar hemiarthropalsty and THA for ONFH of the femoral head. Clin Orthop Relat Res. 2004;424:161–165. doi: 10.1097/01.blo.0000128217.18356.87. [DOI] [PubMed] [Google Scholar]
- 9.Muraki M, Sudo A, Hasegawa H, Fukuda A, Uchida A. Long -term results of bipolar hemiarthroplasty for osteoarthritis of the hip and idiopathic ONFH of the femoral head. J Othop Sci. 2008;13:313–317. doi: 10.1007/s00776-008-1238-2. [DOI] [PubMed] [Google Scholar]
- 10.Kindsfater KA, Spitzer AI, Schaffer JL, Scott RD. Bipolar hemiarthroplasty for primary osteoarthritis of the hip: a review of 41 cases with 8 to 10 years of follow-up. Orthopedics. 1998;21:425–431. doi: 10.3928/0147-7447-19980401-07. [DOI] [PubMed] [Google Scholar]
- 11.Lachiewicz PF, Desman SM. The bipolar endoprosthesis in avascular necrosis of the femoral head. J Arthroplasty. 1988;3:131–138. doi: 10.1016/S0883-5403(88)80078-0. [DOI] [PubMed] [Google Scholar]
- 12.Nishi T, Sugano N, Masuhara K, Takaoak K. Bipolar cup design may lead to osteolysis around the uncemented femoral component. Clin Orthop Relat Res. 1995;316:112–120. [PubMed] [Google Scholar]
- 13.Ito H, Matsuno T, Kaneda K. Bipolar hemiarthroplasty for ONFH of the femoral head. A7- to 18-year followup. Clin Orthop Relat Res. 2000;374:201–211. doi: 10.1097/00003086-200005000-00019. [DOI] [PubMed] [Google Scholar]
- 14.Ortiguera CJ, Pulliam IT, Cabanela ME. Total hip arthorplasty for ONFH: matched-pair analysis of 188 hips with long-term follow-up. J arthroplasty. 1999;14:21–28. doi: 10.1016/S0883-5403(99)90197-3. [DOI] [PubMed] [Google Scholar]
- 15.Hartley WT, McAuley JP, Culpepper WJ, Engh CA, Jr, Engh CA., Sr ONFH of the femoral head treated with cementless total hip arthroplasty. J Bone Joint Surg Am. 2000;82:1408–1413. doi: 10.2106/00004623-200010000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Mont MA, Seyler TM, Plate JF, Delanois RE, Parvizi J. Uncemented total hip arthroplasty in young adults with ONFH of the femoral head: a comparative study. J Bone Joint Surg Am. 2006;88(Suppl 3):104–109. doi: 10.2106/JBJS.F.00451. [DOI] [PubMed] [Google Scholar]
- 17.Takatori Y, Ito K, Sofue M, Hirota Y, Itoman M, Matsumoto T, Hamada Y, Shindo H, Yamada H, Yasunaga Y, et al. Analysis of interobserver reliability for radiographic staging of coxarthrosis and indexes of acetabular dysplasia: a preliminary study. J Orthop Sci. 2010;15:14–19. doi: 10.1007/s00776-009-1412-1. [DOI] [PubMed] [Google Scholar]
- 18.Engh CA, Hooten JP, Zettl-Schaffer KF. Porous-coated total hip replacement. Clin Orthop Relat Res. 1994;298:89–96. [PubMed] [Google Scholar]
- 19.Fukushima W, Fujioka M, Kubo T, Tamakoshi A, Nagai M, Hirota Y. Nationwide epidemiologic survey of idiopathic ONFH of the head. Clin Orthop Relat Res. 2010;468:2715–2724. doi: 10.1007/s11999-010-1292-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shigemura T, Nakamura J, Kishida S, Harada Y, Ohtori S, Kamikawa K, Ochiai N, Takahashi K. Incidence of ONFH associated with corticosteroid therapy among different underlying disease: prospective MRI study. Rheumatology. 2011;50:2023–2028. doi: 10.1093/rheumatology/ker277. [DOI] [PubMed] [Google Scholar]
- 21.Tektonidou MG, Malagari K, Vlachoyiannopoulos PG, Kelekis DA, Moutsopoulos HM. Asymptomstic avscular necrosis in patients with primary antiphospholipid syndrome in the absence of corticosteroid use: a prospective study by magnetic imaging. Arthritis Rheum. 2003;48:732–736. doi: 10.1002/art.10835. [DOI] [PubMed] [Google Scholar]
- 22.Pellegrini VD, Jr, Heiges BA, Bixler B, Lehman EB, Davis CM., 3rd Minimum ten-year results of primary bipolar hip arthroplasty for degenerative arthritis of the hip. J Bone Joint Surg Am. 2006;88:1817–1825. doi: 10.2106/JBJS.01879.pp. [DOI] [PubMed] [Google Scholar]
- 23.Tsumura H, Torisu T, Kaku N, Higashi T. Five- to fifteen-year clinical results and the radiographic evaluation of acetabular changes after bipolar hip arthroplasty for femoral head ONFH. J Arthroplasty. 2005;20:892–897. doi: 10.1016/j.arth.2004.11.010. [DOI] [PubMed] [Google Scholar]
- 24.Clowes JA, Peel N, Eastell R. Glucocorticoid-induced osteoporosis. Rheumatology. 2001;13:326–332. doi: 10.1097/00002281-200107000-00015. [DOI] [PubMed] [Google Scholar]
- 25.Schorlemmer S, Gohl C, Iwabu S, Ignatius A, Claes L, Augat P. Glucocorticoid treatment of ovarietomized sheep affects mineral density, structure, and mechanical properties of cancellous bone. J Bone Miner Res. 2003;18:2010–2015. doi: 10.1359/jbmr.2003.18.11.2010. [DOI] [PubMed] [Google Scholar]
- 26.Koch PP, Tannast M, Fujita H, Sibenrock K, Ganz R. Minimum ten year results of total hip arthroplasty with the acetabular reinforcement ring in avascular ONFH. Int Orthop. 2008;32:173–179. doi: 10.1007/s00264-006-0303-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kim YH, Choi Y, Kim JS. Cementless total hip arthroplasty with ceramic-on-ceramic bearing in patients younger than 45 years with femoral-head ONFH. Int Orthop. 2010;34:1123–1127. doi: 10.1007/s00264-009-0878-y. [DOI] [PMC free article] [PubMed] [Google Scholar]