Abstract
Purpose
ADVANCE® Medial-Pivot (MP) (Wright Medical Technology, Arlington, TN, USA) total knee arthroplasty (TKA) was developed to replicate normal tibiofemoral knee joint kinematics, allowing medial-pivot knee motion. The design concept of the prosthesis is unique; therefore, the influence on the patellofemoral knee joint remains unclear at present. The purpose of this study was to determine the in vivo patellofemoral kinematics with ADVANCE® MP TKA and compare them with the pre-operative conditions.
Methods
ADVANCE® MP TKA was performed in ten subjects with osteoarthritis (OA). At before and one month after surgery, lateral radiographs with weight-bearing at maximum extension, 30, 60 and 90° were taken, and patella flexion angle (PF), tibiopatellar angle (TP) and estimated patellofemoral contact point (PC) were evaluated, according to a previously reported method.
Results
In PF and TP, there was no statistically significant change between pre-operative and postoperative values. Pre-operative PC reached its peak at 90°; however, its peak was at 60° at one month after surgery. Postoperative PC at maximum extension was significantly higher compared to before surgery.
Conclusions
The results in this study indicated that ADVANCE® MP TKA changed patellofemoral joint kinematics compared to before surgery. Early postoperative evaluation is the limitation of this study; however, we consider that the results in this study might be one of the keys to resolving the kinematic features of this prosthesis, helping clinicians to comprehend this prosthesis.
Introduction
Total knee arthroplasty (TKA) is a well-established procedure that generally results in a high level of patient satisfaction. However, joint kinematics after TKA are quite different from normal kinematics, including paradoxical anterior motion of the femur. In many cases, poor TKA kinematics and abnormal forces may play a key role in wear, malalignment or accelerated failure associated with design flows [1, 2]. Hence, to comprehend the kinematics of the artificial knee joints is important in sophisticated TKA.
Although the patellofemoral joint is a major cause of poor function in the prosthetic knee [3, 4], patellofemoral joint kinematics are not so well understood compared to tibiofemoral joint kinematics. ADVANCE® Medial-Pivot (MP) TKA (Wright Medical Technology, Arlington, TN, USA) was developed to replicate the medial pivoting behaviour observed in normal knees and has been found to exhibit excellent anterior-posterior stability. This implant has a single radius of femoral curvature and a high level of conformity in the medial compartment about which it rotates. It does not roll back as in the post and cam mechanism of posterior stabilised (PS) arthroplasty. This prosthesis is more bone conserving and has been reported to improve biomechanics of the patellofemoral joint [5].
Several studies have revealed the tibiofemoral kinematics of this prosthesis and reported its favourable performance in patients; however, its patellofemoral joint kinematics remain unknown at present [6–8]. Thus, the aim of this study was to determine the in vivo patellofemoral kinematics with ADVANCE MP TKA and compare the results with the pre-operative condition, while discussing possible effects on patients.
Materials and methods
The study was approved by the Institutional Review Board, and informed consent was obtained from all patients. From May to November 2010, ADVANCE® MP TKA was performed in ten subjects with varus deformity diagnosed with osteoarthritis (OA). Patients with valgus deformity, severe bony defects and rheumatoid arthritis were excluded from this study. TKA was implanted in both groups by the same experienced surgeon (K.I.) using a conventional manual technique, as mentioned below. Briefly, knees were exposed with a medial parapatellar arthrotomy and bony resection was performed using the measured resection technique. The posterior cruciate ligament (PCL) was sacrificed at the beginning of the procedure. The rotational alignment of the femoral prosthesis was set at 3° of external rotation in relation to the posterior condylar axis, according to each patient. The proximal tibial osteotomy was performed perpendicular to the long axis in the coronal plane with 3° posterior slope in the sagittal plane. A tibial bony cut was made at 10 mm below the highest point of the articular cartilage on the lateral tibial plateau. No lateral retinacular release was performed and all patellae were unresurfaced with removal of the surrounding osteophyte. All surgeries were deemed clinically successful without any ligamentous laxity, postoperative surgical stiffness or pain up to one year after surgery.
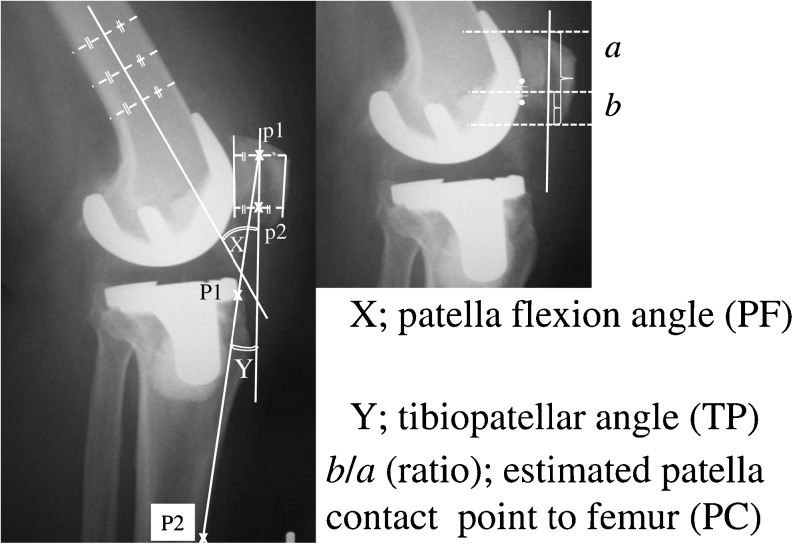
Before and one month after operation, each patient was asked to perform deep bending from full extension to maximum knee flexion. During this motion, lateral radiographs with weight-bearing (320 mA, 0.03 s exposure at 80–100 kV, depending on soft tissue thickness) at maximum extension, 30, 60 and 90° were taken. The flexion angle was measured on the X-ray images and was defined as the angle made by the longitudinal axes of the femur and tibial long bones [9]. Thereafter, patella flexion angle (PF), tibiopatellar angle (TP) and estimated patellofemoral contact point (PC) were evaluated, according to a previously reported method [10, 11] (Fig. 1). The measurements were performed at least three times in each patient by two independent authors blinded to clinical information using commercially available imaging software systems (SYNAPSE, FUJIFILM, Tokyo, Japan) and the averages were used in this study.
Fig. 1.
Detailed explanation of the radiographic measurements. P1 the most anterior point on the tibial plateau, P2 the most anterior and distally available point of the tibia, p1 midpoint at proximal portion of the patella, p2 midpoint at distal portion of the patella, a patella length, b distance from apex of the patella to the contact point, patella axis line connecting points p1 and p2, X patella flexion angle (PF), Y tibiopatellar angle (TP), b/a estimated patellofemoral contact point (PC)
The TP was defined as the angle between the longitudinal axis of the tibia and patella [10, 11] (angle Y in Fig. 1). The most anterior point on the tibial plateau and the most anterior and most distally available point of the tibia were defined as points P1, and P2, respectively. The longitudinal axis of the tibia was assumed to be parallel to the line connecting points P1 and P2. The patella axis was also defined as follows: First we determined four points of the patella to characterise the shape of the patella body (anterior and proximal, anterior and distal, posterior and proximal and posterior and distal). Thereafter, each midpoint at the proximal portion and distal portion of the patella were determined as p1 and p2, respectively. Finally, the patella axis was defined by connecting points p1 and p2.
PF was defined as the angle between the longitudinal axis of the femur and patella (angle X in Fig. 1).
PC was determined by finding the closest point between the most anterior portions of the femoral component and the most posterior osseous portion of the patella. The location of the most posterior point of the patella along the patella axis was assumed to agree with the PC. In extension and pre-operative conditions, it is relatively easy to determine the PC because the unresurfaced patellae allows us to visualise the entire bone easily. In deeper flexion, the patella slides between the femoral condyles, which overlap the patella and femoral component. In these cases, the centroid of the overlapping area was found, and its location along the patella axis was assumed to agree with the PC. The PC was expressed as a ratio, which was determined by measuring the distance from the apex of the patella to the contact point (b in Fig. 1) normalised with respect to the patella length (a in Fig. 1).
Statistical analysis
Results were analysed statistically using a statistical software package (Stat Mate III, ATMS Co., Ltd., Tokyo, Japan). The differences between pre-operative and postoperative values were analysed using the paired Student’s t test. Differences of p < 0.05 were considered statistically significant.
Results
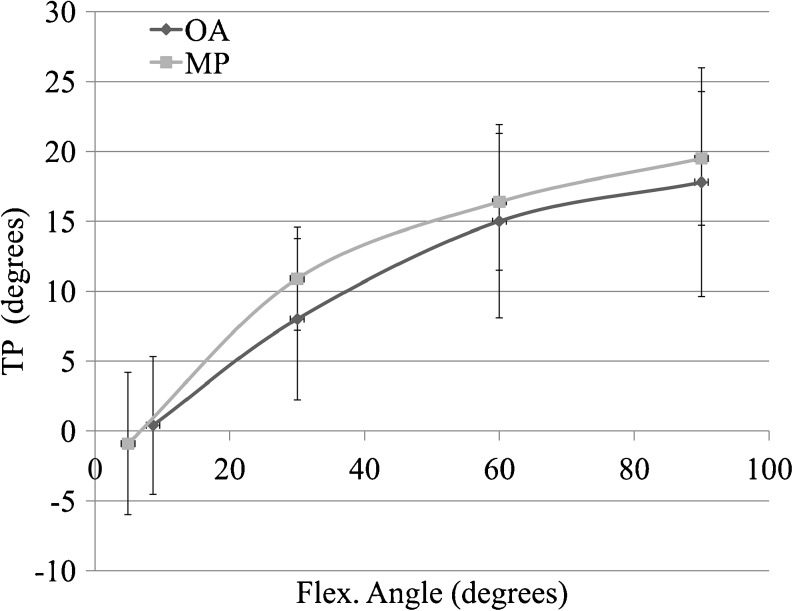
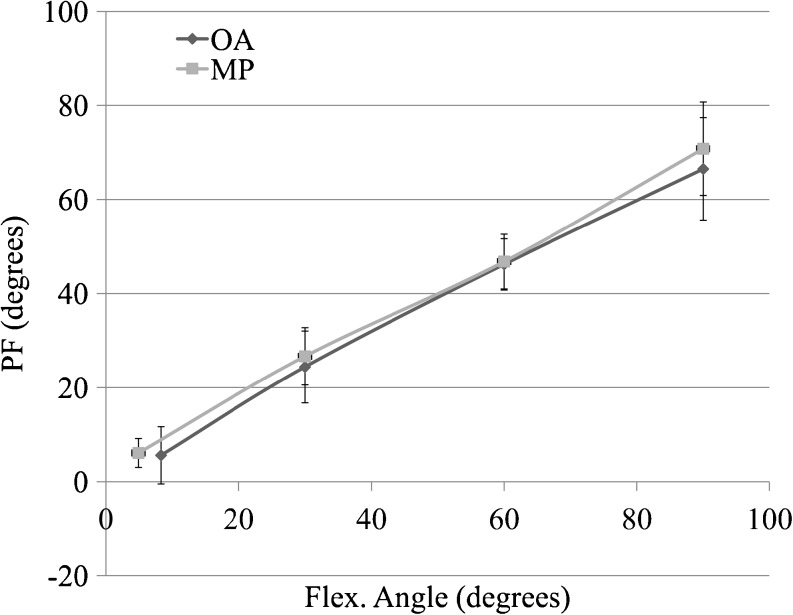
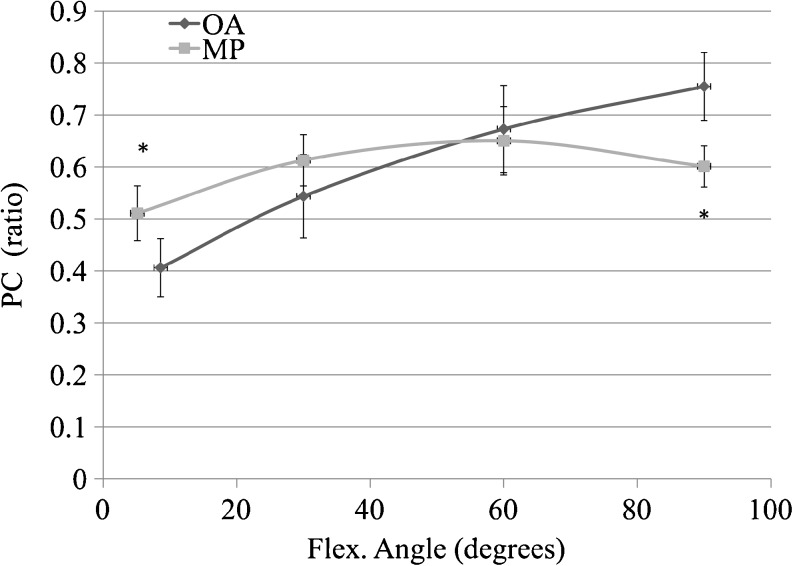
The average pre-operative maximum extension and flexion angles were −8.6 ± 7.4° and 117.8 ± 12.0°, respectively. The average postoperative maximum extension and flexion angles were −4.9 ± 5.3° and 102.2 ± 9.3°, respectively. TP at maximum extension, 30°, 60° and 90° of flexion before and after surgery were 0.4 ± 4.9°, 8.0 ± 5.8°, 15.0 ± 6.9° and 17.8 ± 8.2° and −0.9 ± 5.1°, 10.9 ± 3.7°, 16.4 ± 4.9° and 19.5 ± 4.8°, respectively. TP results (Fig. 2) showed a similar pattern of 90° in both groups, and the differences between the angles before and after surgery at each flexion angle showed no statistically significant difference. PF at maximum extension, 30°, 60° and 90° of flexion before and after surgery were 5.6 ± 6.1°, 24.4 ± 7.6°, 46.2 ± 5.5° and 66.5 ± 10.9° and 6.1 ± 3.1°, 26.7 ± 6.1°, 46.8 ± 5.8° and 70.8 ± 9.9°, respectively. PF (Fig. 3) also showed an almost similar pattern between pre- and postoperative values and the differences between the angles before and after surgery at each flexion angle showed no statistically significant difference. The results of PC (Fig. 4) at maximum extension, 30°, 60° and 90° of flexion before and after surgery were 0.41 ± 0.06, 0.54 ± 0.08, 0.67 ± 0.08 and 0.75 ± 0.07 and 0.51 ± 0.05, 0.61 ± 0.05, 0.65 ± 0.07 and 0.60 ± 0.04, respectively. PC translated proximally on the patella with increasing flexion. The range of this translation was smaller before surgery than after surgery. Pre-operative PC reached its peak at 90°; however, its peak was 60° at 1 month after surgery. Postoperative PC at maximum extension was significantly higher compared to before surgery (p < 0.05). Postoperative PC at 90° was significantly lower compared to before surgery (p < 0.05).
Fig. 2.
Pre- and postoperative tibiopatellar angle. Tibiopatellar angle (TP) results showed a similar pattern of 90° in both groups. OA pre-operative data, MP postoperative data
Fig. 3.
Pre- and postoperative patella flexion angle. Patella flexion angle (PF) results also showed an almost similar pattern between pre- and postoperative values. OA pre-operative data, MP postoperative data
Fig. 4.
Pre- and postoperative estimated patellofemoral contact point. Preoperative PC reached its peak at 90°; however, its peak was 60° after surgery. Postoperative PC at maximum extension was significantly higher, and postoperative PC at 90° was significantly lower compared to before surgery (*p < 0.05). OA pre-operative data, MP postoperative data
Discussion
This study is the first report to examine radiographic patellofemoral joint kinematics in ADVANCE® MP TKA. The results demonstrated that this prosthesis showed characteristic patellofemoral kinematics, especially in PC, and differed from those of previous reports on PS and cruciate-retaining design [10, 11].
There are some limitations of this study. Firstly, the evaluation in this study was performed in the early postoperative period, only one month after surgery. The timing of the evaluation will change the effects of the surrounding tissues, thus leading to different results, especially maximum flexion angles. Secondly, the factors affecting the patellofemoral joint are multifactorial, including rotation of the tibia, joint line elevation etc.; therefore, the influences of such factors remain unknown in this study [12, 13]. In this study, the surgical methods such as rotation references were consistent through the experiment; therefore, we consider that the influences of such factors are negligible in this study. In addition, controversy exists as to whether the PCL should be retained or sacrificed in ADVANCE® MP TKA [14–17]. Some authors recommend complete resection of the PCL for adequate flexion or function in MP knee [17], indicating knee motion led by MP insert was mismatched with the knee motion due to the PCL. Thus, the condition of the PCL might change the kinematics, also in the patellofemoral joint. Finally, kinematic effects on long-term survival and wear were not analysed and beyond the scope of this report.
The result at maximum extension was compared to previous reports that showed patellofemoral kinematics with PCL-retaining (CR) and PS designs [10]. Leszko et al. have suggested that one of the reasons for possible changes in patellofemoral interaction was the more posterior contact point of the tibiofemoral joint at full extension for implanted knees than for natural knees [10]. It has also been reported that most of the superior migration of the contact point occurred during early knee flexion in the healthy patella [10, 18, 19]. In this study, we investigated pre-operative osteoarthritic knees and found the same tendency of the PC compared to the healthy patella as previously reported [10, 18, 19].
The postoperative results of PC are quite different from other reports, with this report showing its peak at over 90° [10, 11]. Leszko et al. reported that patella contact point locations seemed to remain unchanged in classic CR, PS and high-flexion TKA [10]. This report and the results in this study indicated that ADVANCE® MP moves quite differently from CR and PS TKA. We supposed that one of the main reasons is femorotibial kinematics [10, 20]. D’Lima et al. pointed out that greater leverage for the extensor mechanism is maintained by preventing anterior translation and shortening of the quadriceps lever/arm in the MP prosthesis [21]. It is also said that patients could feel stability via anterior-posterior stability by the MP prosthesis [17]. Meanwhile, it has been reported that the lateral condyle showed anterior movement in the early stage, changing thereafter to posterior movement in ADVANCE® TKA [7]. We supposed that this motion pattern might possibly cause an increase in patellofemoral contact pressure in the early stage. Generally, it has been reported that a bicondylar rollback motion pattern such as that exhibited in the normal knee is desirable for deep knee bending [22]. For example, Johal et al. reported that the medial condyle moved posteriorly 8.4 mm at full flexion, and the lateral condyle moved posteriorly 21.1 mm at 120° of flexion in their motion analysis with normal weight-bearing knees [22]. For prosthetic knees, Becher et al. also pointed out that femoral rollback reduces patellofemoral pressure and superior patellofemoral kinematics [23]. It was also reported that the posterior location of the contact points at a higher angle increases the quadriceps moment arm that should reduce quadriceps and patellofemoral forces and aid implant survival [24, 25]. In ADVANCE® MP TKA, high conformity insert contributes to reproducing the medial-pivot motion and the patients’ subjective feelings of stability; however, we supposed that the design concept that does not allow posterior femoral rollback may influence the radiographic result in this study. Further studies are needed to investigate the correlation with femorotibial kinematics, or compare with other prosthesis, such as the PS design.
In conclusion, this study showed radiographic patellofemoral joint kinematics in ADVANCE® MP TKA for the first time. The results in this study indicated that ADVANCE® MP TKA changes patellofemoral joint kinematics compared to before surgery. Whether this change in kinematics is favourable for patients receiving TKA remains unknown in this study. Comprehensive evaluations including objective and subjective scoring and survival of the prosthesis are mandatory for assessing the design concept of all prostheses. Early postoperative evaluation is the limitation of this study; however, we consider our results might be pivotal in resolving the kinematic features of this prosthesis, thus leading to improvement of the prosthesis design for all patients.
Acknowledgment
We thank Ms. Janina Tubby for English rewriting.
References
- 1.Hofmann GO, Hagena FW. Pathomechanics of the femoropatellar joint following total knee arthroplasty. Clin Orthop Relat Res. 1987;224:251–259. [PubMed] [Google Scholar]
- 2.Matsuda S, Ishinishi T, White SE, Whiteside LA. Patellofemoral joint after total knee arthroplasty. Effect on contact area and contact stress. J Arthroplasty. 1997;12:790–797. doi: 10.1016/S0883-5403(97)90010-3. [DOI] [PubMed] [Google Scholar]
- 3.Chew JT, Stewart NJ, Hanssen AD, Luo ZP, Rand JA, An KN. Differences in patellar tracking and knee kinematics among three different total knee designs. Clin Orthop Relat Res. 1997;345:87–98. doi: 10.1097/00003086-199712000-00013. [DOI] [PubMed] [Google Scholar]
- 4.Dalury DF, Dennis DA. Extensor mechanism problems following total knee replacement. J Knee Surg. 2003;16:118–122. [PubMed] [Google Scholar]
- 5.Anderson MJ, Becker DL, Kieckbusch T. Patellofemoral complications after posterior-stabilized total knee arthroplasty: a comparison of 2 different implant designs. J Arthroplasty. 2002;17:422–426. doi: 10.1054/arth.2002.32173. [DOI] [PubMed] [Google Scholar]
- 6.Barnes CL, Sharma A, Blaha JD, Nambu SN, Carroll ME. Kneeling is safe for patients implanted with medial-pivot total knee arthroplasty designs. J Arthroplasty. 2011;26:549–554. doi: 10.1016/j.arth.2010.04.027. [DOI] [PubMed] [Google Scholar]
- 7.Miyazaki Y, Nakamura T, Kogame K, Saito M, Yamamoto K, Suguro T. Analysis of the kinematics of total knee prostheses with a medial pivot design. J Arthroplasty. 2011;26:1038–1044. doi: 10.1016/j.arth.2010.08.015. [DOI] [PubMed] [Google Scholar]
- 8.Omori G, Onda N, Shimura M, Hayashi T, Sato T, Koga Y. The effect of geometry of the tibial polyethylene insert on the tibiofemoral contact kinematics in Advance Medial Pivot total knee arthroplasty. J Orthop Sci. 2009;14:754–760. doi: 10.1007/s00776-009-1402-3. [DOI] [PubMed] [Google Scholar]
- 9.Dennis DA, Komistek RD, Stiehl JB, Walker SA, Dennis KN. Range of motion after total knee arthroplasty: the effect of implant design and weight-bearing conditions. J Arthroplasty. 1998;13:748–752. doi: 10.1016/S0883-5403(98)90025-0. [DOI] [PubMed] [Google Scholar]
- 10.Leszko F, Sharma A, Komistek RD, Mahfouz MR, Cates HE, Scuderi GR. Comparison of in vivo patellofemoral kinematics for subjects having high-flexion total knee arthroplasty implant with patients having normal knees. J Arthroplasty. 2010;25:398–404. doi: 10.1016/j.arth.2008.12.007. [DOI] [PubMed] [Google Scholar]
- 11.Stiehl JB, Komistek RD, Dennis DA, Keblish PA. Kinematics of the patellofemoral joint in total knee arthroplasty. J Arthroplasty. 2001;16:706–714. doi: 10.1054/arth.2001.24443. [DOI] [PubMed] [Google Scholar]
- 12.König C, Sharenkov A, Matziolis G, Taylor WR, Perka C, Duda GN, Heller MO. Joint line elevation in revision TKA leads to increased patellofemoral contact forces. J Orthop Res. 2010;28:1–5. doi: 10.1002/jor.20952. [DOI] [PubMed] [Google Scholar]
- 13.Miller MC, Berger RA, Petrella AJ, Karmas A, Rubash HE. Optimizing femoral component rotation in total knee arthroplasty. Clin Orthop Relat Res. 2001;392:38–45. doi: 10.1097/00003086-200111000-00005. [DOI] [PubMed] [Google Scholar]
- 14.Bae DK, Song SJ, Cho SD. Clinical outcome of total knee arthroplasty with medial pivot prosthesis A comparative study between the cruciate retaining and sacrificing. J Arthroplasty. 2011;26:693–698. doi: 10.1016/j.arth.2010.04.022. [DOI] [PubMed] [Google Scholar]
- 15.Karachalios T, Roidis N, Giotikas D, Bargiotas K, Varitimidis S, Malizos KN. A mid-term clinical outcome study of the Advance Medial Pivot knee arthroplasty. Knee. 2009;16:484–488. doi: 10.1016/j.knee.2009.03.002. [DOI] [PubMed] [Google Scholar]
- 16.Shakespeare D, Ledger M, Kinzel V. Flexion after total knee replacement. A comparison between the Medial Pivot knee and a posterior stabilised implant. Knee. 2006;13:371–373. doi: 10.1016/j.knee.2006.05.007. [DOI] [PubMed] [Google Scholar]
- 17.Pritchett JW. Patients prefer a bicruciate-retaining or the medial pivot total knee prosthesis. J Arthroplasty. 2011;26:224–228. doi: 10.1016/j.arth.2010.02.012. [DOI] [PubMed] [Google Scholar]
- 18.Hsu HC, Luo ZP, Rand JA, An KN. Influence of lateral release on patellar tracking and patellofemoral contact characteristics after total knee arthroplasty. J Arthroplasty. 1997;12:74–83. doi: 10.1016/S0883-5403(97)90051-6. [DOI] [PubMed] [Google Scholar]
- 19.Komistek RD, Dennis DA, Mabe JA, Walker SA. An in vivo determination of patellofemoral contact positions. Clin Biomech (Bristol, Avon) 2000;15:29–36. doi: 10.1016/S0268-0033(98)00061-8. [DOI] [PubMed] [Google Scholar]
- 20.Stiehl JB. A clinical overview patellofemoral joint and application to total knee arthroplasty. J Biomech. 2005;38:209–214. doi: 10.1016/j.jbiomech.2004.02.026. [DOI] [PubMed] [Google Scholar]
- 21.D’Lima DD, Poole C, Chadha H, Hermida JC, Mahar A, Colwell CW., Jr Quadriceps moment arm and quadriceps forces after total knee arthroplasty. Clin Orthop Relat Res. 2001;392:213–220. doi: 10.1097/00003086-200111000-00026. [DOI] [PubMed] [Google Scholar]
- 22.Johal P, Williams A, Wragg P, Hunt D, Gedroyc W. Tibio-femoral movement in the living knee. A study of weight bearing and non-weight bearing knee kinematics using ‘interventional’ MRI. J Biomech. 2005;38:269–276. doi: 10.1016/j.jbiomech.2004.02.008. [DOI] [PubMed] [Google Scholar]
- 23.Becher C, Heyse TJ, Kron N, Ostermeier S, Hurschler C, Schofer MD, Fuchs-Winkelmann S, Tibesku CO. Posterior stabilized TKA reduce patellofemoral contact pressure compared with cruciate retaining TKA in vitro. Knee Surg Sports Traumatol Arthrosc. 2009;17:1159–1165. doi: 10.1007/s00167-009-0768-2. [DOI] [PubMed] [Google Scholar]
- 24.Browne C, Hermida JC, Bergula A, Colwell CW, Jr, D’Lima DD. Patellofemoral forces after total knee arthroplasty: effect of extensor moment arm. Knee. 2005;12:81–88. doi: 10.1016/j.knee.2004.05.006. [DOI] [PubMed] [Google Scholar]
- 25.Churchill DL, Incavo SJ, Johnson CC, Beynnon BD. The influence of femoral rollback on patellofemoral contact loads in total knee arthroplasty. J Arthroplasty. 2001;16:909–918. doi: 10.1054/arth.2001.24445. [DOI] [PubMed] [Google Scholar]