Abstract
Purpose
A rupture of the Achilles tendon may heal in continuity, resulting in a lengthened Achilles tendon. The elongated structure must be shortened to restore effective push off. We report the results of a longitudinal study using Z-shortening of ruptured Achilles tendons that healed in continuity but were elongated.
Methods
Nine patients underwent surgery for elongation of a healed Achilles tendon rupture. All participants were prospectively followed up for two to five years, and final review was performed at 32 ± 14 months from operation. Clinical and functional assessment (anthropometric measurements, isometric strength, postoperative total rupture score) was performed.
Results
All patients were able to walk on tiptoes, and no patient used a heel lift or walked with a visible limp. No patient developed clinically evident deep-vein thrombosis or sustained a rerupture. Two patients were managed conservatively following a superficial surgical wound infection. At final review, maximum calf circumference remained significantly decreased in the operated leg. The operated limb was significantly weaker than the nonoperated one.
Conclusions
Managing a healed Achilles tendon rupture using Z-shortening is safe and effective, providing good recovery and early weight bearing and active ankle mobilisation. Such patients should be warned that they are at risk for postoperative complications and that their ankle–plantar flexion strength is likely to be permanently reduced.
Introduction
Achilles tendon ruptures are common [1] but may be missed in up to 20 % of patients at initial presentation [2]. Patients may present with weakness on push off, pes planus, and toe clawing [3]. Ruptures may heal in continuity, resulting in a lengthened tendon [4]. The elongated tendon may have to be shortened or reconstructed to allow restoration of push off. Z-shortening has been reported for operative shortening of the elongated Achilles tendon following healed rupture [5]. We describe a modification of this technique for a chronic rupture of the Achilles tendon that healed in continuity and resulted in an elongated, non-functional gastroc-soleus [6].
We performed a Z-shortening in nine patients in whom the Achilles tendon had healed in continuity but was elongated. We therefore evaluated long-term results of this single-centre, single-surgeon study using as outcome measures the postoperative Achilles Tendon Total Rupture Scores (ATRS), maximum calf circumference, isometric plantar flexion strength and complications.
Patients and methods
Ethics
All the procedures described were performed after local Ethical Committee approval had been granted.
Patients
All operations were performed in the period 2001–2006. A total of 11 patients were secondary or tertiary referrals from other health-care professionals. We were able to track down nine of the original cohort of 11 patients, and this article focuses on patients for whom we obtained complete data. These nine patients (two women, aged 41 and 53 years; and seven men, mean age 50.4 ± 8.1 years; range 40–62 years) underwent Z-shortening of a lengthened Achilles tendon following rupture and healing in continuity (five after conservative management, three following percutaneus management, one open surgery). Between eight and 19 (mean 13.8) months elapsed before the index operation.
Diagnosis
When questioned by the senior author, all patients reported a sudden sharp pain in the calf or at the posterior aspect of the ankle. Subsequently, routine daily tasks such as walking up hill or climbing stairs became difficult. At presentation to the senior author, no patient had a palpable gap, and they were all able to perform active plantar flexion but were not able to stand on tiptoes with the knee extended. Single-leg toe raises were possible with a variable degree of flexion of the ipsilateral knee, and all patients kept the foot of the affected limb in slight external rotation when walking and with a nonpropulsive gait. In all patients, calf muscles of the affected limb were wasted. Eight patients had clawing of the lesser toes and an apparent higher medial arch.
Regardless of appearance at MRI or ultrasound scan, and although the calf squeeze test did produce some motion in the ipsilateral ankle [7, 8], the knee flexion test showed elongation of the gastroc-soleus–Achilles tendon complex [9] (Fig. 1). In the knee-flexion test, the patient lies prone with knees flexed to 90°. The ankle on the affected side assumes a more dorsiflexed position compared with the normal side. This is due to the absence of the normal slight tension under which the tendon connects the gastroc-soleus complex to the calcaneum. The effects of gravity make the foot dorsiflex on the ankle. All patients had undergone a trial of up to three months using a heel lift of 1–1.5 cm but declared themselves dissatisfied and wished to undergo surgery.
Fig. 1.
Typical magnetic resonance imaging (MRI) appearance: the size of the Achilles tendon is increased, and there appears to be continuity
Operative technique
With the patient prone, a calf tourniquet is applied and inflated to 250 mmHg after exsanguination. Skin preparation and sterile drapes are used. Following preoperative skin marking, a medial, gently curvilinear incision is made. In the patient who had undergone open repair of an acute Achilles tendon tear, the scar of the previous surgery was used. The tendon appears macroscopically intact, having healed in continuity, although it is elongated and thicker and rounder than a normal Achilles tendon (Fig. 2). Macroscopically, it may be possible to detect healthy areas, whereas scar tissue lacks fibre continuity. Once the distal and proximal borders of the normal tendon are established, the tendon is mobilised from the flexor hallucis longus fascia. Kager’s triangle is greatly reduced, and often the Achilles tendon lies directly on the flexor hallucis longus fascia. A longitudinal split is made through the length of the healed scar area, extending from normal tendon proximally through the healed area into the normal tendon distally (Fig. 3). The opposing halves of the tendon are released on opposing sides in a z-shape. With the ankle held in full plantarflexion, the opposing strands of the shortened z are resected, leaving enough tissue to adequately approximate opposing tendon ends with the ankle in full plantarflexion (Fig. 4). A longitudinal running suture using no. 1 Maxon (Tyco Healthcare, Norwalk, CT, USA) is then used to secure both halves of the tendon. The approximated transverse halves are then sutured using a modified Kessler suture, further increasing the strength of the repair (Fig. 5). Using tissue forceps, the tendon is turned over, and the undersurface of the incision is sutured again using the locking, running Maxon suture. The final knot is tied on the undersurface of the tendon so as not to irritate the overlying skin. Care is taken to ensure that the sural nerve is not damaged. The wound is closed in layers with a subcuticular suture; wound edges are covered with Steristrips (3M Health Care, St. Paul, MN, USA), and a Mepore (Molnlycke Health Care, Gothenburg, Sweden) dressing is applied. Patients are immobilised in a below-knee synthetic cast in full equinus, leaving the metatarsal heads free.
Fig. 5.

Z-shortening is secured using strong absorbable sutures along the entirety of its course
Fig. 2.
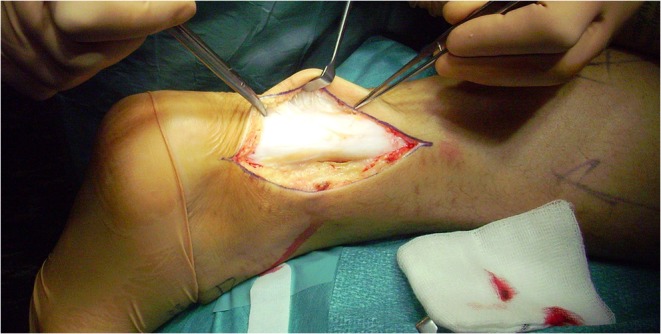
Intraoperative appearance: The anteroposterior diameter of the tendon is increased. The tendon appears in continuity, with peritendinous adherences to the superficial tissues
Fig. 3.

After drawing the direction of the Z-shortening cuts, the relevant amount of tendon is excised from the proximal and distal transverse branches of the Z
Fig. 4.

If necessary, the tendon can be debulked
Postoperative management
No venous thromboembolism prophylaxis was implemented in our patients. Patients are allowed to weight bear on the metatarsal heads, as comfort allows, using elbow crutches [10]. It would be unusual for a patient to weight bear fully at this stage. They are encouraged to perform active flexion and extension of the hallux and toes and to perform isometric exercises of the calf muscles and toes. After two weeks, the plaster is bivalved, the back shell is removed, and physiotherapy is commenced with the front shell in situ, thus preventing ankle dorsiflexion and focusing on proprioception, plantar flexion, inversion and eversion [10, 11]. During this period of rehabilitation, the patient is permitted to weight bear as comfort allows with the front shell in situ, although full weight bearing rarely occurs on account of balance difficulties, and patients usually continue to require the assistance of a single elbow crutch at this stage. The front shell may be removed after six weeks. We do not use a heel lift after cast removal, and patients normally regain a plantigrade ankle within two or three weeks [10, 11].
Follow-up
Patients were assessed during the sixth postoperative week, after the cast had been removed, and during the third and sixth postoperative month. They were then followed up at three-month intervals unless clinical needs required more frequent appointments. All patients were able to perform at least ten heel raises unaided on the operated leg and had returned to work and/or leisure activities by two years after the operation. Patients were routinely discharged 24 months after the operation. They were prompted to contact the operating surgeon should any problems arise at any time after the operation. They underwent a final assessment for the purposes of this project at a mean of 32.4 ± 14.1 months from operation.
Achilles Tendon Total Rupture Score
The ATRS [12] was used to evaluate postoperative symptoms and physical activity after treatment.
Anthropometric measurements
Maximum calf circumference was measured in both the affected and the contralateral leg using a commercially available steel tape measurer.
Functional assessment
Patients were asked to perform ten single-leg heel raises on the affected leg and were judged as either being able or as being unable to do so.
Classification of results
Surgical outcome was rated using the 4-point scale by Boyden et al. [13], which is routinely used and had been validated in our setting [10, 14]. A patient with an excellent result had no pain, no limitation of recreational or daily activities, no footwear restrictions, and was thoroughly satisfied with the surgery. A patient with a good result had mild occasional pain, limitation of recreational but not daily activities, no footwear restrictions, and was satisfied, with only minor reservations. A patient with a fair result had mild to moderate pain, limitation of recreational and daily activities, moderate footwear restrictions (unable to tolerate fashionable shoes, with or without an insert), and was satisfied, with major reservations. A patient with a poor result had moderate to severe pain, limitation of recreational and daily activities, severe footwear restrictions (brace or modified shoes only), and was dissatisfied or had rerupture.
Isometric gastroc-soleus strength
Isometric plantarflexion strength of the gastroc-soleus complex was determined bilaterally with the ankle in the neutral (0°) position by using a custom-made apparatus [15] consisting of a foot plate, the angle of which could be varied and locked into a given position. An analogue to digital converter (ADC-10; PICO Technology, Cambridge, UK) connected the strain gauge on the foot plate to a voltmeter (Picoscope; PICO Technology). In its turn, the voltmeter was connected to a computer. Voltage changes were then converted into Newtons to measure strength. The apparatus was calibrated by suspending known weights from 2.5 kg to 37.5 kg before and after each patient was tested, giving a linear response. Each patient supported their lower limb in the leg rest, with their heel placed firmly at the top of the foot plate and with the plantar aspect of their foot resting at ease. The patient was then asked to exert maximal isometric force on to the foot plate for three to five seconds. The maximum result was noted. The amplifier was used each time to return the voltmeter to 0. Each patient performed two maximal attempts, and the average was used for further analysis [15]. For technical reasons, we were able to collect strength data from 25 of our 32 patients.
Statistics
Data were entered in a commercially available database. Descriptive statistics were calculated. Comparisons between operated and normal limb were performed using the McNemar test to analyse binary data and the Wilcoxon test on the difference in scores for continuous data. Significance was set at the 0.05 level. The paired-samples t test was used to compare isometric gastroc-soleus strength in the ruptured side with the nonruptured side.
Source of funding
No funding source was received to perform the study.
Results
All patients were discharged from routine clinical care by two years following the index procedure. Although most patients were satisfied with the procedure, only two were classified as having an excellent result, and six of our nine patients achieved a good result. The other patient experienced a fair result (Table 1).
Table 1.
Clinical results (N = 9)
| Postoperative evaluation | |
|---|---|
| Clinical | |
| Pain | |
| None | 6 |
| Mild, occasional 2 | 2 |
| Moderate 2 | 2 |
| Severe 0 | 0 |
| Activity limitations | |
| None 6 | 6 |
| Limited recreational but not daily living activities 2 | 2 |
| Limited recreational and daily living activities 1 | 1 |
| Footwear restrictions | |
| None, mild (most shoes tolerated) 9 | 9 |
| Moderate (unable to tolerate fashionable shoes, with or without insert) 0 | 0 |
| Severe (only modified shoes tolerated or brace) 0 | 0 |
| Satisfaction | |
| Satisfied 7 | 7 |
| Satisfied with minor reservations 2 | 2 |
| Satisfied with major reservations 0 | 0 |
| Dissatisfied 0 | 0 |
| Overall results | |
| Excellent 2 | 2 |
| Good 6 | 6 |
| Fair 1 | 1 |
| Poor 0 | 0 |
Complications
Two patients had a superficial infection of the surgical wound and were managed conservatively with systemic antibiotics and local dressings. All healed within three months of the index procedure without need for additional operations. One patient developed a hypertrophic scar in the area of the Achilles tendon surgical wound. No patient developed a clinically evident deep-vein thrombosis or sustained a rerupture. All were able to walk on tiptoes, and no patient used a heel lift. Two patients, although not walking with a visible limp, still retained external rotation of the affected limb.
Anthropometric measurements
Maximum calf circumference was significantly decreased in the operated leg by the time of latest follow-up [37.7 ± 4.0 cm (side with rupture) vs. 43.2 ± 3.6 cm (uninjured side); P = 0.05)] (Table 2).
Table 2.
Patients and results
| Patient number | Sex | Age at operation | ATRS | Isometric strength operated side | Isometric strength nonoperated side | Functional assessment (single-leg heel lifts) | Calf circumference operated side | Calf circumference nonoperated side | Work at latest FU | Leisure at latest FU | Activities at the time of rupture |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 43 | 78 | 278 | 319 | 10 | 31.5 | 37.8 | Office worker | Gym work | Jogging |
| 2 | M | 56 | 81 | 191 | 239 | 10 | 44.1 | 50.2 | Accountant | Gardening | Dancing |
| 3 | M | 40 | 83 | 219.9 | 288.5 | 10 | 35.2 | 42 | Roofer | Gym work | Falling from a height |
| 4 | F | 41 | 92 | 185 | 261.5 | 60 | 32.8 | 39.2 | Housewife | Power walking | Pushing a car |
| 5 | M | 45 | 79 | 236.9 | 285.7 | 10 | 39.9 | 44.3 | Office worker | Gym work, walking | Accident at home |
| 6 | M | 56 | 81 | 339.1 | 391.6 | 10 | 41 | 46.2 | Teacher | Cycling | Accident at work |
| 7 | F | 53 | 86 | 291.7 | 332 | 10 | 39.2 | 44.2 | Pensioner | Gardening | Running to catch a bus |
| 8 | M | 51 | 92 | 199.3 | 290.1 | 60 | 38.7 | 42.4 | Sales representative | Cycling | Accident at home |
| 9 | M | 62 | 82 | 227 | 283.8 | 10 | 37.1 | 42.5 | Accountant | Walking | Falling from a height |
Functional assessment
Patients were able to perform at least ten single-leg heel lifts on the affected leg by discharge, and two patients were able to perform at least 60 single-leg heel lifts on the affected leg. All patients had returned to their preinjury working occupation. (Table 2).
ATRS
The ATRS score at final follow-up was 83.8 ± 5.2. (Table 2).
Isometric gastroc-soleus strength
The duplicate measurements showed a high intraobserver reliability (r = 0.90; P = 0.012). T test paired sampled statistics showed that the operated limb had a lower peak torque than the nonoperated leg (240.9 N ± 51.9 N vs. 299.0 N ± 44.2 N; P = 0.05), but the patients did not perceive this decrease in strength as interfering with their daily or leisure activities. (Table 2).
Discussion
We evaluated postoperative ATRS, maximum calf circumference, isometric plantar flexion strength of the gastroc-soleus complex, and complications in a series of nine patients who underwent Z-shortening for a rupture of the Achilles tendon that had healed in continuity [6]. Surgery for these lesions is challenging because of greater muscle atrophy at time of surgery and adherences between skin and tendon that can be frequently present around the tendon.
Wound breakdown is a common complication in Achilles tendon reconstruction surgery, and superficial infection rate is up to 9 % [14]. Z-shortening of the Achilles tendon has been performed through a longitudinal medial incision. Sural nerve injury is another complication. At the level of the tendon’s insertion, the sural nerve is 18.8 mm lateral to the tendon; but, as it progresses proximally, the nerve gradually traverses medially, crossing the lateral border of the tendon 9.8 cm proximal to the calcaneum [16]. In our study, we did not experience any sural nerve complication.
Our technique is useful in patients in whom a rupture of the Achilles tendon has healed in continuity and the Achilles tendon is lengthened. The shape of the cut allows the healing surface of the tendon to be maximised. The approximation of the tendon ends is wide without leaving defects. The shape of the cut also minimises interposed scar tissue between tendon ends and consequently reduces the risk of further elongation. However, we recently showed that in Achilles tendon ruptures, the areas proximal and distal to the rupture itself exhibit profound biochemical and gene-expression changes and cannot be considered normal [17].
We allow early weight bearing following surgery: this not detrimental to the outcome of repair after rupture and shortens the time needed for rehabilitation [10, 18]. Full weight bearing following repair is optimal for tendon healing [19], as shown in well-conducted randomised studies [10, 19]. To suture Z-shortening cuts, we use absorbable material, so we impart initial strength to the repair itself, and, as healing progresses and the suture material degrades, progressively greater loads are transmitted to the tendon itself, allowing appropriate physiological healing [20]. Also, using absorbable material, we avoid the presence of a permanent foreign body, which could act as a focus of infection.
We tested the strength of the gastroc-soleus complex, and although the strength deficit was relatively low and patients reported no subjective loss of strength, it appears that there is permanent loss of plantar flexion of the gastroc-soleus complex. All patients were operated on by a fully trained orthopaedic surgeon with a special interest in such injuries, and postoperative management was uniform throughout the study. We are aware that the evidence given for assessing postsurgical outcomes and for establishing causation is not as strong as that which would be produced by a randomised controlled trial. However, the condition reported in this study is uncommon, and a randomised controlled trial would probably be long and costly, necessitating large numbers of patients.
We were able to follow up nine of the 11 patients originally operated upon with this technique. Nevertheless, we are confident that the sample reported is representative of the entire population. We noticed clawing of the toes in a remarkable percentage of patients. It is likely that this may be a consequence of the overactivity of the long toe flexors to compensate for the lack of activity of the gastroc-soleus complex. We are not sure of the clinical relevance of this finding, although it is possible that prolonged overactivity of these muscles may produce permanent toe deformity.
In conclusion, this technique allows close approximation of normal tendon tissue, optimises repair strength, minimises further scar formation, subsequent potential for scar elongation, and further plantarflexion weakness. It affords good recovery in patients with a rupture of the Achilles tendon healed in continuity. However, the patients should be warned about postoperative complications, e.g. wasting of the calf is not likely to recover and ankle plantar flexion strength can remain permanently reduced.
Acknowledgments
Competing interests
None
References
- 1.Jozsa L, Kvist M, Balint BJ, Reffy A, Jarvinen M, Lehto M, Barzo M. The role of recreational sport activity in Achilles tendon rupture. A clinical, pathoanatomical, and sociological study of 292 cases. Am J Sports Med. 1989;17:338–43. doi: 10.1177/036354658901700305. [DOI] [PubMed] [Google Scholar]
- 2.Maffulli N. Clinical tests in sports medicine: more on Achilles tendon. Br J Sports Med. 1996;30:250. doi: 10.1136/bjsm.30.3.250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Platt H. Observations of some tendon ruptures. Br Med J. 1931;1:811. doi: 10.1136/bmj.1.3670.811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maffulli N, Ajis A, Longo UG, Denaro V. Chronic rupture of tendo Achillis. Foot Ankle Clin. 2007;12:583–96. doi: 10.1016/j.fcl.2007.07.007. [DOI] [PubMed] [Google Scholar]
- 5.Cannon LB, Hackney RG. Operative shortening of the elongated defunctioned tendoachillies following previous rupture. J R Nav Med Serv. 2003;89:139–41. [PubMed] [Google Scholar]
- 6.Carmont MR, Maffulli N. Z shortening of healed Achilles tendon rupture: a technical note. Foot Ankle Int. 2009;30:704–7. doi: 10.3113/FAI.2009.0704. [DOI] [PubMed] [Google Scholar]
- 7.Maffulli N. The clinical diagnosis of subcutaneous tear of the Achilles tendon. A prospective study in 174 patients. Am J Sports Med. 1998;26:266–70. doi: 10.1177/03635465980260021801. [DOI] [PubMed] [Google Scholar]
- 8.Simmonds FA. The diagnosis of the ruptured Achilles tendon. Practitioner. 1957;179:56–8. [PubMed] [Google Scholar]
- 9.Matles AL. Rupture of the tendo Achilles. Another diagnostic sign. Bull Hosp Joint Dis. 1975;36:48–51. [PubMed] [Google Scholar]
- 10.Maffulli N, Tallon C, Wong J, Lim KP, Bleakney R. Early weightbearing and ankle mobilization after open repair of acute midsubstance tears of the achilles tendon. Am J Sports Med. 2003;31:692–700. doi: 10.1177/03635465030310051001. [DOI] [PubMed] [Google Scholar]
- 11.Maffulli N, Tallon C, Wong J, Peng Lim K, Bleakney R. No adverse effect of early weight bearing following open repair of acute tears of the Achilles tendon. J Sports Med Phys Fitness. 2003;43:367–79. [PubMed] [Google Scholar]
- 12.Nilsson-Helander K, Thomee R, Gravare-Silbernagel K, Thomee P, Faxen E, Eriksson BI, Karlsson J. The Achilles tendon Total Rupture Score (ATRS): development and validation. Am J Sports Med. 2007;35:421–6. doi: 10.1177/0363546506294856. [DOI] [PubMed] [Google Scholar]
- 13.Boyden EM, Kitaoka HB, Cahalan TD, An KN. Late versus early repair of Achilles tendon rupture. Clinical and biomechanical evaluation. Clin Orthop Relat Res. 1995;317:150–8. [PubMed] [Google Scholar]
- 14.Pintore E, Barra V, Pintore R, Maffulli N. Peroneus brevis tendon transfer in neglected tears of the Achilles tendon. J Trauma. 2001;50:71–8. doi: 10.1097/00005373-200101000-00013. [DOI] [PubMed] [Google Scholar]
- 15.Bleakney RR, Tallon C, Wong JK, Lim KP, Maffulli N. Long-term ultrasonographic features of the Achilles tendon after rupture. Clin J Sport Med. 2002;12:273–8. doi: 10.1097/00042752-200209000-00003. [DOI] [PubMed] [Google Scholar]
- 16.Webb J, Moorjani N, Radford M. Anatomy of the sural nerve and its relation to the Achilles tendon. Foot Ankle Int. 2000;21:475–7. doi: 10.1177/107110070002100604. [DOI] [PubMed] [Google Scholar]
- 17.Karousou E, Ronga M, Vigetti D, Passi A, Maffulli N. Collagens, proteoglycans, MMP-2, MMP-9 and TIMPs in human achilles tendon rupture. Clin Orthop Relat Res. 2008;466:1577–82. doi: 10.1007/s11999-008-0255-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hamilton B, Remedios D, Loosemore M, Maffulli N. Achilles tendon rupture in an elite athlete following multiple injection therapies. J Sci Med Sport. 2008;11:566–8. doi: 10.1016/j.jsams.2007.03.008. [DOI] [PubMed] [Google Scholar]
- 19.Thordarson D. Immediate full weight-bearing mobilization was better than immobilization after operative repair of a ruptured achilles tendon. J Bone Joint Surg Am. 2006;8:1894. doi: 10.2106/JBJS.8808.ebo2. [DOI] [PubMed] [Google Scholar]
- 20.Sharma P, Maffulli N. Tendon injury and tendinopathy: healing and repair. J Bone Joint Surg Am. 2005;87:187–202. doi: 10.2106/JBJS.D.01850. [DOI] [PubMed] [Google Scholar]



