Abstract
Purpose
Kienböck’s disease is an unusual pathology with unknown aetiology within the pediatric population. Several treatment options have been described in the literature; however, there are neither large series nor homogeneous studies that have clarified which treatment is best. The aim of this study was to describe five cases in which definitive distal radius epiphysiodesis was performed as an alternative method to the classic distal radius shortening osteotomy in skeletally immature patients with Kienböck’s disease.
Methods
The clinical charts and radiographs of four patients (five wrists) diagnosed as having Kienböck’s disease and treated by definitive distal radius epiphysiodesis were reviewed.
Results
All patients were symptomatically free with full range of motion at 4.25 months (range, three to six months) after surgery. In all cases, shortening of the distal radius was achieved (p = 0.032).
Conclusions
This new technique is a simple, effective, and minimally invasive procedure with low morbidity and good clinical and radiological outcomes.
Introduction
Kienböck’s disease has an unusual pathology with unknown aetiology within the pediatric population. This entity is called infantile lunatomalacia in children under 13 years of age and juvenile lunatomalacia in older patients [1]. Several treatment options have been described in the literature; however, there are neither large series nor homogeneous studies that have clarified which treatment is best [1–9]. Nonsurgical treatment should be considered for children under 15 years of age as the first approach [1]. However, when either conservative treatment fails or the disease is in a more advanced stage, surgery should be performed; distal radius shortening or closed-wedge osteotomy are the most commonly used procedures [1]. Radius overgrowth after these procedures has been described, but a clear relationship to the final outcome has not been identified [10, 11]. In addition to certain technical issues encountered when performing an osteotomy, osteosynthetic implants are required and a future decision must be made on the need and/or timing of removal.
The aim of this study was to describe five cases in which definitive distal radius epiphysiodesis was performed as an alternative method to the classic distal radius shortening osteotomy in skeletally immature patients with Kienböck’s disease. To the best of our knowledge, this is the first report of this technique used for this purpose.
Methods
The clinical charts of four patients diagnosed as having Kienböck’s disease who were treated by definitive distal radius epiphysiodesis were reviewed. There were four patients (two males and two females) with five lunates affected. The mean pre-operative symptomatic period was eight months (range, five–20 months), and the mean age at surgery was 13 years (range, 12–14 years). There were two cases in stage III (Table 1).
Table 1.
Demographic data of the study patients who underwent distal radius definitive epiphysiodesis for treatment of Kienböck’s disease
| PATIENT | GENDER | AGE (y) | SIDE | SYMPTOMS (m) | STAGE | FOLLOW-UP (m) | Ischemia time (min) |
|---|---|---|---|---|---|---|---|
| 1 | Male | 12y,8 m | Right | 5 | IIIB | 26 | 52 |
| 2L | Male | 13y,10 m | Left | 5 | I | 25 | 45 |
| 2R | Male | 13y,10 m | Right | 5 | I | 25 | 55 |
| 3 | Female | 12y,4 m | Left | 20 | I | 121 | 53 |
| 4 | Female | 12y,5 m | Left | 5 | IIIA | 43 | 50 |
L:left ; R: right ; y: years; m: months; min : minutes
All patients complained of pain during active and passive palmar flexion and dorsiflexion that was associated with loss of power handling when performing prehensile functions. There was also tenderness over the lunate and radiolunate interval. Plain radiography and magnetic resonance imaging (MRI) (Fig. 1a, b and c) were used to diagnose all patients who were first treated with early immobilization for three to six months and showed no improvement of symptoms. Surgery was then performed, with a mean follow-up time of 48 months (range, 25–121 months).
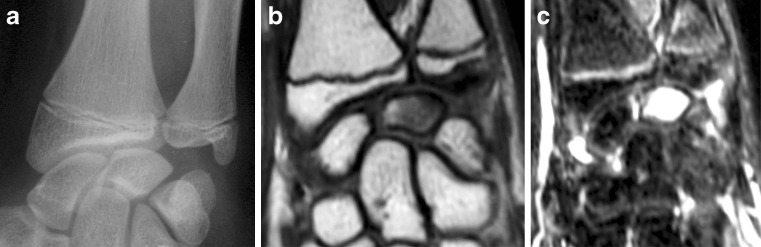
Fig. 1.
A 13-year-10-month-old boy with a five-month history of left wrist pain underwent distal radius definitive epiphysiodesis due to stage I Kienböck’s disease after conservative treatment failure. a Preoperative posteroanterior plain X-ray image of the left carpal bones. Nonobvious bone abnormalities are shown. There is no carpal collapse. b Low-intensity T1-weighted coronal view of the lunate bone. There is no carpal collapse and no lunate fracture. c High-intensity T2-weighted coronal view of the lunate bone
Definitive epiphysiodesis was performed through a radial longitudinal incision over the radial styloid process, taking care to not damage the sensitive radial cutaneous branch and localizing the brachioradialis insertion. The periosteum was sectioned, which allowed vision of the physeal zone where a wire for a cannulated drill (Fig. 2a) was inserted. Definitive epiphysiodesis was performed by drilling the physis under C-arm guidance (Fig. 2b, c) and augmented with the use of a curette (Fig. 2d). A contrast dye was used to confirm adequate cartilage disruption (Fig. 2e, f). Soft tissues were closed by layers. After surgery, the patients needed only a sterile dressing and did not require any type of immobilization. A postoperative plain X-ray image was also taken (Fig. 2g). An upper limb tourniquet was used to prevent bleeding, and the average ischemia time was 51 minutes.
Fig. 2.
Description of the surgical procedure performed in a 12-year-4-month-old girl with stage I Kienböck’s disease. Shown is the left wrist. a Shown is the wire placement in the distal radius physis after open longitudinal approach over radius styloid. b Posteroanterior view of the left wrist. Drilling of the distal radius physis under C-arm guidance. c Lateral view of the left wrist showing drilling of the central distal radius physis. d Posteroanterior view of the left wrist showing curettage of the residual growing cartilage from the distal radius physis. e Posteroanterior view of the left wrist. Injection of contrast dye to confirm disruption of the distal radius physis. f Lateral view of the left wrist. Injection of contrast dye to confirm central disruption of the distal radius physis. g Immediate postoperative posteroanterior plain X-ray image of the left wrist where the epiphysiodesis procedure was performed
Postoperative rehabilitation consisted of early mobilization, renewal of daily activities in four weeks, and full activities in eight weeks. In all cases, postoperative X-ray images were taken to confirm definitive epiphysiodesis (Fig. 3), and a minimum of 1 MRI follow-up was performed in each wrist. In addition, radiological assessments were performed for all patients; the pre-operative and postoperative carpal height ratio, radio-scaphoid angle, Ståhls angle, and ulnar variance were measured on plain radiographs. Clinical assessments were performed postoperatively and the Disabilities of the Arm, Shoulder, and Hand (DASH) scores were also recorded. Normal values were considered to be a range of motion of 85° of flexion, 85° of extension, 15° of abduction, and 45° of adduction [8]. Postoperative surgical complications, such as damage to the cutaneous radial nerve branch, epiphysiodesis failure, skin complications, hematomas, and reflex sympathetic dystrophy syndrome were recorded. Epiphysiodesis failure was defined as a failure to achieve shortening of the distal radius and was determined by assessing whether failure to decrease ulnar variance (failure to achieve neutral or positive variance) occurred.
Fig. 3.

Posteroanterior view of the right wrist in a 12-year-8-month-old boy who was treated with distal radius definitive epiphysiodesis. At the 26-month follow-up, fusion was observed
Statistical analysis
Study participants' characteristics will be described and pre- and post-surgical radiological measurements of patients with Kienböck's disease will be compared by non-parametric Wilcoxon test. All significance tests will be 2-tailed and differences will be considered to be significant at p-value < 0.05.
Results
Patient 1 was free of symptoms five months after surgery and demonstrated normal range of motion. Patient 2 was asymptomatic three months after surgery in both wrists, but showed regression of radiological changes on MRI within the left; however, range of motion was normal at the four-month follow-up in both wrists. In both wrists a good clinical result was achieved. Patient 3 presented with diffuse pain over the lunate, and pain with active movements which were completely resolved three months after surgery and showed normal MR images and complete range of motion. After ten years of follow-up (eight years after growth was completed), she began to show mild symptoms compatible with distal radioulnar joint (DRUJ) instability. The patient is a manual worker, and the symptoms don’t limit her work. Her work may be the source of these symptoms as a significant amount of time has passed since the surgery was performed, so we think these symptoms may not be associated to our procedure.
Patient 4 was asymptomatic and demonstrated full range of motion at the six-month follow-up. In general, all patients were symptomatically free and had full range of motion at a mean of 4.25 months (range, three to six months) after surgery.
In those patients who were stage IIIA and IIIB, progression of the Stahl index was observed, whereas in those who had stage I disease, no progression or even improvement was observed (Table 2); however, the differences were not statistically significant. No radius overgrowth was found. There were no surgical complications recorded.
Table 2.
Pre- and postsurgical radiological measurements of the study patients with Kienböck’s disease
| PATIENT | Carpal Height Ratio | p-value | Radioscaphoid Angle | p-value | Ståhl Index | p-value | Ulnar variance (mm) | p-value | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PRE | POST | 0.245 | PRE | POST | 0.492 | PRE | POST | 0.892 | PRE | POST | 0.032 | |
| 1 | 0.41 | 0.33 | 33 | 33 | 0.31 | 0.29 | -10 | -3 | ||||
| 2L | 0.51 | 0.5 | 50 | 49 | 0.59 | 0.6 | -1 | 1 | ||||
| 2R | 0.49 | 0.48 | 45 | 47 | 0.56 | 0.57 | -1 | 1 | ||||
| 3 | 0.48 | 0.51 | 45 | 43 | 0.57 | 0.61 | 0 | 5 | ||||
| 4 | 0.42 | 0.4 | 50 | 49 | 0.37 | 0.32 | -5 | -1 | ||||
Results with p-values ≤0.05 were considered to be statistically significant
mm: millimeters
In all cases, shortening of the distal radius was achieved (decrease in ulnar variance), which was the primary aim of the surgery using this technique (p < 0.05). In all patients, a successful epiphysiodesis was performed.
Discussion
Several techniques have been described for the treatment of Kienböck’s disease within the pediatric population. De Smet [3] reported a 12-year-old girl with Kienböck’s disease who was treated conservatively, which resulted in a mobile and pain-free wrist; however, there was no sign of radiological improvement at the 25-month follow-up. Herzberg et al. [12] conservatively treated a 14-year-old gymnast and achieved complete clinical and radiological recovery at the 45-month follow-up. Irisarri el al [1]. reviewed nine patients with “juvenile lunatomalacia”; all were treated first with immobilization. Three were lost to final follow-up, three achieved excellent results with conservative treatment, and the remaining patients were treated surgically through a radial shortening osteotomy and showed good radiological and clinical outcomes at the five-year follow-up. Yasuda et al. [9] performed a temporary fixation of the scaphotrapezoidal joint in an asymptomatic 12-year-old girl with stage IIIB Kienböck’s disease. Radiological signs of revascularization were observed at the 16-month follow-up. Shigematsu et al. [8] reported a temporary fixation of the scaphotrapeziotrapezoid joint in an 11-year-old girl with stage IIIA Kienböck’s disease. Signs of revascularization and no pain were observed at four months postsurgery.
There are only a few reported cases in the literature, and they have used nonhomogeneous approaches and shown inconsistent results. In our short series, three cases achieved complete clinical recovery (stage I). Patient 3 began with symptoms of DRUJ instability ten years after surgery. The symptoms were subtle compared with those of contralateral DRUJ, and the patient had a DASH score of 61. Lunate morphology was completely recovered. In patient 4, there was disease progression, with the symptoms reappearing two years after surgery. Pain killers were used for optimal pain control.
We report a new surgical technique, distal radius epiphysiodesis, for treatment of skeletally immature patients affected by Kienböck’s disease in which a neutral or negative ulnar variance and failure of conservative treatment were observed. Our technique is based on achieving radial shortening with the subsequent diminution of compressive forces acting in the lunate. This technique is an alternative to the classic radial shortening osteotomy previously described. Our technique has some advantages such as: it’s a well known technique used for other diseases; no radial overgrowth (this complication is observed with the radial shortening osteotomy); technically is easier than an osteotomy; early recovery and allows a progressive shortening of the radius with regards to the ulna that theoretically permits a better adaptation of the DRUJ. However, this technique needs a closer follow-up. More studies with larger numbers of patients are needed, but we found our technique to be a simple, effective, and minimally invasive procedure with low morbidity and good clinical and radiological results.
Acknowledgments
Conflict of interest statement
All named authors hereby declare that they have no conflicts of interest to disclose.
References
- 1.Irisarri C, Kalb K, Ribak S. Infantile and juvenile lunatomalacia. J Hand Surg Eur. 2010;35:544–548. doi: 10.1177/1753193410364913. [DOI] [PubMed] [Google Scholar]
- 2.Ando Y, Yasuda M, Kazuki K. Temporary scaphotrapezoidal joint fixation for adolescent Kienbock’s disease. J Hand Surg Am. 2009;34:14–19. doi: 10.1016/j.jhsa.2008.09.019. [DOI] [PubMed] [Google Scholar]
- 3.Smet L. Kienbock’s disease in a 12-year-old girl. Acta Orthop Belg. 2003;69:361–362. [PubMed] [Google Scholar]
- 4.Greene WB. Kienbock disease in a child who has cerebral palsy. A case report. J Bone Joint Surg Am. 1996;78:1568–1573. doi: 10.2106/00004623-199610000-00016. [DOI] [PubMed] [Google Scholar]
- 5.Hosking OR. Kienbock’s disease in an 8-year-old boy. Aust N Z J Surg. 1989;59:92–93. doi: 10.1111/j.1445-2197.1989.tb01472.x. [DOI] [PubMed] [Google Scholar]
- 6.Kahn SJ, Sherry DD. Kienbock’s disease–avascular necrosis of the carpal lunate bone–in a 7-year-old girl with dermatomyositis. Clin Pediatr (Phila) 1994;33:752–754. doi: 10.1177/000992289403301210. [DOI] [PubMed] [Google Scholar]
- 7.Rasmussen F, Schantz K. Lunatomalacia in a child. Acta Orthop Scand. 1987;58:82–84. doi: 10.3109/17453678709146349. [DOI] [PubMed] [Google Scholar]
- 8.Shigematsu K, Yajima H, Kobata Treatment of Kienbock disease in an 11-year-old girl with temporary fixation of the scaphotrapeziotrapezoidal joint. Scand J Plast Reconstr Surg Hand Surg. 2005;39:60–63. doi: 10.1080/02844310410017988. [DOI] [PubMed] [Google Scholar]
- 9.Yasuda M, Okuda H, Egi T. Temporary scapho-trapezoidal joint fixation for Kienbock’s disease in a 12-year-old girl: a case report. J Hand Surg Am. 1998;23:411–414. doi: 10.1016/S0363-5023(05)80458-7. [DOI] [PubMed] [Google Scholar]
- 10.Herdem M, Ozkan C, Bayram H. Overgrowth after radial shortening for Kienbock’s disease in a teenager: case report. J Hand Surg Am. 2006;31:1322–1325. doi: 10.1016/j.jhsa.2006.07.014. [DOI] [PubMed] [Google Scholar]
- 11.Matsuhashi T, Iwasaki N, Oizumi N. Radial overgrowth after radial shortening osteotomies for skeletally immature patients with Kienbock’s disease. J Hand Surg Am. 2009;34:1242–1247. doi: 10.1016/j.jhsa.2009.04.028. [DOI] [PubMed] [Google Scholar]
- 12.Herzberg G, Mercier S, Charbonnier JP. Kienbock’s disease in a 14-year-old gymnast: a case report. J Hand Surg Am. 2006;31:264–268. doi: 10.1016/j.jhsa.2005.09.016. [DOI] [PubMed] [Google Scholar]