Abstract
Purpose
The aim of our study was to investigate trends over time in the mortality of elderly patients after femoral neck fractures treated with bipolar hemiarthroplasty.
Methods
Altogether 487 cases of femoral neck fracture treated with bipolar hemiarthroplasty were observed during a 20-year period. Mortality rates were calculated for five years postoperatively. To account for the age distribution of the study population standardised mortality ratios (SMR) with respect to the age-specific mortality of the German population were determined and compared. Additional changes of the SMRs over time and the influence of the time delay before surgery on long-term mortality were evaluated.
Results
Femoral neck fractures treated with bipolar hemiendoprosthesis have a significant impact on mortality. Postoperative mortality is increased in patients of all age groups, but the effect diminishes in higher age groups. The influence on mortality was significantly greater for men than for women. The SMR has decreased from 3.52 before 1995 to 1.2 after 2006. Since 2006 there is no longer an increase in mortality after surgical treatment of a femoral neck fracture compared to general German population of the same age.
Conclusion
Femoral neck fractures treated with bipolar hemiendoprosthesis result in a significantly increased mortality, however in our population this impact has significantly decreased over time. The effect on mortality is less in women and higher age groups than in men and younger patients. No influence of the time between accident and surgery on mortality could be detected.
Introduction
Worldwide about 1.7 million mainly older people sustain a hip fracture every year [1]. In Germany the incidence of femoral neck fractures in patients older than 65 years was 966 of 100,000 persons per year in 2001 [2]. Considering a general increase in life expectancy, these injuries will become more frequent and a tripling of hip fractures is expected within the next 50 years [1].
Femoral neck fractures in elderly patients are usually treated surgically. Available procedures can be differentiated between those with or without preservation of the femoral head. Hip joint-preserving surgical procedures often do not allow early weight bearing and high revision rates are reported [3–5]. Therefore especially in geriatric patients the preferred therapy option is hip arthroplasty, while in younger patients a hip-preserving procedure is preferred [6]. However, the ideal surgical treatment and the implications of a delayed treatment of elderly patients with displaced femoral neck fracture are still controversial [4, 7–12].
As a result of femoral neck fractures patients do not only have a significantly increased risk of permanent physical disability and social dependency, but these injuries also are associated with significant mortality [13, 14]. The one-year mortality rates reported in literature range from 11 to 36 % [1, 15–17]. Although the implantation of bipolar hemiendoprosthesis in geriatric patients is currently the procedure of choice, data on long-term mortality are sparse [10, 18, 19].
The aim of our study was to determine the influence of femoral neck fracture treated with bipolar hemiarthroplasty on mortality and to compare these mortality rates over a time frame of 20 years.
In this analysis the times of survival of all patients treated with bipolar hemiarthroplasty for a displaced femoral neck fracture treated at our institution between 1989 and 2003 have been collected and standardised mortality ratios (SMR) have been determined. Additionally, the SMR ratios and the influence of delay before surgery have been examined. The SMR during different observation periods was analysed to determine changes in relative mortality risk over time.
Patients and methods
Altogether 487 cases of traumatic displaced femoral neck fractures treated by bipolar hemiarthroplasty between 1989 and 2003 at the authors’ institution were collected retrospectively and included in this study. According to the German Society of Gerontology and Geriatrics a geriatric patient was defined as being older than 70 years of age or suffering geriatric multimorbidity. Patients with pathological fractures and bipolar hemiarthroplasty due to failed internal fixation were excluded. All participating surgeons were experienced in arthroplasty. Demographic data including patients’ gender, age, and the date of accident, hospital admission and surgery were collected. At the end of the follow-up evaluation in December 2009 the dates of death of all deceased patients were requested from the responsible registry offices. To evaluate the influence of femoral neck fractures and bipolar hemiarthroplasty on mortality in comparison to a general population, standardised mortality ratios with respect to the age-specific mortality of the German population were calculated. The SMR is defined as the ratio of the number of observed deaths in the study population to the expected number of deaths that occur under the age-specific mortality pattern of a reference population. Thus, the measure reflects the mortality risk attributed to femoral neck fractures. An SMR of 1 implies that the number of deaths observed in the study population is exactly the same as the number of expected deaths in a population without femoral neck fractures, implying that this injury would not have an influence on mortality. An SMR above 1 (below 1) indicates higher (lower) mortality than expected in a general population. For example, an SMR of 1.45 means that the observed mortality for patients with femoral neck fractures is 45 % higher or 1.45 times as high as the mortality expected in a general population with the same age distribution.
In order to compare different SMRs via relative SMRs a Poisson regression was used. Age, gender and the observation period were selected as covariates. For example, the relative SMR for gender is the ratio of the observed deaths for women to the observed deaths for men, weighted with the ratio of the expected deaths for men to women. Thus a relative SMR of 1.13 means that the mortality for women compared to men is 1.13 times as high in a population with femoral neck fractures as the mortality for women compared to men in an healthy population with the same age distribution.
Average measures are displayed with range and their standard deviations and SMRs with 95 % confidence intervals (CI).
Results
The average age of the 396 female and 91 male patients was 81.5 (48–99; ± 8.1) years at the time of accident. Female patients had an average age of 82.1 (50–99; ± 7.7) years and were significantly (p = 0.004) older than males with an average age of 79.0 (48–95; ± 9.6) years. The median time between accident and the surgical treatment was one day. At the end of our follow-up evaluation 409 patients had died.
For all calculations living patients were treated as right censored data. The median survival time after injury was 34.9 (CI 28.2 – 44.2) months. Averaging 89 (CI 88 - 89) years of age, female patients reached higher ages than males who averaged 85 (CI 82 - 86) years. Mortality during the first year after surgery was 27.7 %. This figure decreased to 14.6 % within the second, 8.4 % in the third, 5.5 % in the fourth and 4.9 % within the fifth year.
Calculating the overall standardised mortality ratio (SMR), we found an SMR of 1.85 (CI 1.68–2.04), which means that a femoral neck fracture treated with bipolar hemiarthroplasty increases the mortality 1.85 times. Additionally, a sex-related difference in mortality rates could be shown. The mortality after femoral neck fracture and bipolar hemiarthroplasty was 1.73 times (CI 1.56–1.93) higher than expected in women and 2.56 (CI 2.05–3.18) higher than expected in men (Table 1). Following the relative SMR for gender, the chance of death after implantation of a bipolar hemiarthroplasty earlier than expected, was 1.42 (CI 1.10–1.83) times greater for men than for women.
Table 1.
Observed and expected death with resulting standardised mortality ratio (SMR) and gender differences
| Group | Observed deaths | Expected deaths | SMR | Lower 95% confidence limit | Upper 95 % confidence limit |
|---|---|---|---|---|---|
| Overall | 409 | 221,15 | 1,85 | 1,68 | 2,04 |
| Female | 329 | 189,85 | 1,73 | 1,56 | 1,93 |
| Male | 80 | 31,3 | 2,56 | 2,05 | 3,18 |
The observed mortality differs significantly from the expected in all age groups (Table 2). Comparing the SMR for different patient ages at the time of accident revealed a decreasing influence with increasing age, as shown by the SMR converging to 1 in older patient groups. The least difference was observed in patients older than 89 years of age (SMR 1.34, CI 1.12–1.61). In patients over 89 years of age the mortality was increased significantly less after hemiarthroplasty compared to younger patients (Table 3).
Table 2.
Observed and expected death with resulting standardised mortality ratio (SMR) for different age classes
| Age class | Observed deaths | Expected deaths | SMR | Lower 95%confidence limit | Upper 95%confidence limit |
|---|---|---|---|---|---|
| < 70 | 10 | 0.63 | 15.77 | 8.5 | 29.3 |
| 70–74 | 13 | 6.07 | 2.14 | 1.2 | 3.7 |
| 75–79 | 31 | 20.00 | 1.55 | 1.24 | 2.51 |
| 80–84 | 93 | 41.70 | 2.23 | 1.82 | 2.73 |
| 85–89 | 147 | 70.33 | 2.09 | 1.78 | 2.46 |
| > 89 | 115 | 85.82 | 1.34 | 1.12 | 1.61 |
Table 3.
Relative standardised mortality ratios (SMR) with patients older than 89 years of age as a reference adjusted for gender and observation period
| Age class | Relative SMR | Lower 95% confidence limit | Upper 95% confidence limit | P-value |
|---|---|---|---|---|
| < 70 | 9.16 | 4.71 | 17.79 | < 0.001 |
| 70–74 | 1.37 | 0.76 | 2.46 | 0.290 |
| 75–79 | 1.10 | 0.73 | 1.64 | 0.656 |
| 80–84 | 1.39 | 1.06 | 1.84 | 0.023 |
| 85–89 | 1.39 | 1.09 | 1.79 | 0.009 |
| > 89 | Reference |
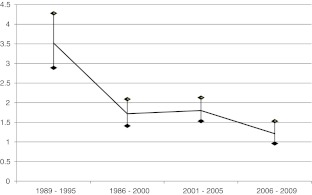
When analysing the effects over the observation period of 20 years, a significant decrease in mortality over time is apparent. The highest SMR (3.52; CI 2.89–4.28) was observed during the period from 1989 to 1995. The SMR in patients treated from 1996 to 2000 was 1.72 (CI 1.41–2.09) and from 2001 to 2005 it was 1.80 (CI 1.53–2.13). The SMR for the period between 2006 and 2009 was 1.21 (CI 0.96–1.53) and did not differ significantly from that of the general population (Fig. 1).
Fig. 1.
Standardised mortality ratio (SMR) with 95 % confidence interval in the different observation periods
Concerning the time between accident and surgery in the different observation periods, the proportion of early operative treatments increased significantly over the observation period. During the period from 1989 to 1995 only 9 % of the patients were treated on the day of hospital admission, whereas this figure increased to 31 % in the period 1996–2000, and to 69 % in 2001–2005. However, comparing the SMR of patients treated within 48 hours after injury with patients treated later we did not find significant differences.
Discussion
Displaced fractures of the femoral neck are frequent and serious injuries especially in geriatric patients. As a result of the increasing life expectancy and growing population of elderly people, this represents an increasing issue. In addition to efforts to provide adequate treatment yielding good functional outcome for the individual patient, economic considerations on the treatment options also need to be taken into consideration.
The high average patient age (81 years) and high proportion of female patients (82 %) in our study is similar to other series [9, 13, 17, 18, 20].
The overall SMR showed that the mortality in the study population is 1.85 times as high as in a population of the same age without femoral neck fractures. Even though such an analysis cannot rule out all confounding variables the observed effect is probably attributable to the femoral neck fracture treated by bipolar hemiarthroplasty. Represented by the smaller difference between observed and expected mortality, women seem to be affected less than men.
So far randomised trials have not shown significant differences in mortality rates between different surgical procedures for hip fractures. However, superior results in pain, patient satisfaction, quality of life and need for revision surgery are reported after primary arthroplasty [3, 4, 8, 21]. Disadvantages on the other hand are prolonged operating time, increased blood loss and higher infection rates [3]. Apart from total hip arthroplasty, bipolar hemiarthroplasty is an option for displaced femoral neck fractures. While total hip replacement provides comparable results in the medium-term, the functional long-term results are superior to bipolar hemiarthroplasty [4, 22]. Advantages of hemiarthroplasty are the lower surgical stress with less blood loss, and fewer dislocations with similar mid-term functional outcome compared to total hip replacement [4, 23]. The disadvantages of hemiarthroplasty are the loss of function over time and the erosion of the acetabulum that correlates with the physical activity [3, 4, 24–26]. However, a recent survey of American surgeons showed that primary hemiarthroplasty is the treatment of choice for displaced femoral neck fractures in geriatric patients [19].
In addition to the risk of persistent physical limitation up to social dependency [14], a significant mortality after hip fractures is described. During the first year after femoral neck fractures a mortality of 11–36 % is reported [1, 15–17, 27]. With 28.3 % one year mortality rate this study is comparable to the literature mentioned above. The high mortality rate within the first year is well documented, but offers few clues to the mortality during the following years. Even though several studies show a high one-year mortality rate, few studies evaluated mortality of geriatric patients over the course of more than one year [17, 18, 20]. Due to comorbidities and general health issues elderly patients have higher mortality rates even in the absence of injuries and surgical events, hence an analysis focussing on the impact of an event on mortality should present values relative to a comparable population. As yet there are few studies comparing the long-term mortality after implantation of a bipolar hemiarthroplasty in femoral neck fracture with the mortality in a general population [18]. In this study SMRs were used to explore this issue. By this comparative approach the influence of displaced femoral neck fracture treated with bipolar hemiarthroplasties on the mortality of elderly people was evaluated over time.
In a retrospective analysis of 241 cases of bipolar hemiarthroplasty for displaced femoral neck fracture Lim et al. demonstrated a significant correlation between higher patient age and rising mortality [17]. In this study mortality was not compared to a matched population, therefore the actual impact of injury and treatment remains unclear. The data in our study demonstrates a similar increase of mortality with age, although we are unable to show a difference in patients above age 89. The fact that with increasing age, the mortality rates approach those of a general population may be based on the general life expectancy and less measurable impact of injury and surgery on mortality.
The most striking finding of our study is the decease in SMR over time. Whereas from 1989 to 1995 the highest SMR was observed, a significant trend toward lower SMR over time was seen, and during the period from 2006 to 2009 the SMR was not significantly higher than 1. This could be explained by improved care and the observed trend towards early surgical treatment. However this should be interpreted cautiously since one limitation of this study is the fact that within the last observation period no surgical treatment was performed and hence the early postoperative mortality is not represented.
In a retrospective matched-pair cohort study including data from external quality assurance of 2004 to 2006, Smektala et al. found a higher rate of intra- and postoperative complications, and development of pressure ulcers in patients receiving surgical therapy later than 48 hours after admission to hospital. However a correlation between mortality during hospital stay and the time to treatment could not be detected [28]. In contrast to our study, Smektala et al. included femoral neck fractures regardless of the surgical treatment. Furthermore, only the effect on in-hospital mortality was evaluated. Our data does also not display a significant influence of delayed surgery on mortality.
Evaluating the factors influencing mortality after bipolar hemiarthroplasty for femoral neck fractures, Eiskjaer et al. could not show an influence of the timing of surgery on mortality after six or 12 months [9]. In a study on mortality of elderly patients with surgically treated femoral neck fractures, Kopp et al. showed a significantly reduced life expectancy in patients with high age, multiple pre-existing conditions and poor mobility before the accident, nor could an influence of delayed therapy be detected [29]. In contrast, Lim et al. pointed out a raised mortality due to a delay before surgery of more than five days whereas any delay shorter than that did not have an influence on mortality [17].
We could not identify a significant effect of a delayed therapy on postoperative mortality, however the study might be underpowered to draw this conclusion. The significant trend towards earlier treatment of patients with femoral neck fractures in our series over the observation period could possibly be a reason for the lower SMR in the later observation periods. However, due to a low number of patients with a delay of more than three days we could not test for the influence of longer delays.
Conclusion
Femoral neck fractures treated with bipolar hemiendoprosthesis result in a significantly increased mortality; however, in our population this impact decreased over time. In women mortality is less increased than in men. Influence of the time between accident and surgery on mortality could not be detected. The significant decrease in mortality over recent years suggests that bipolar hemiarthroplasty is an increasingly secure treatment option for elderly patients sustaining a femoral neck fracture.
Acknowledgments
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Miyamoto RG, Kaplan KM, Levine BR, Egol KA, Zuckerman JD. Surgical management of hip fractures: an evidence-based review of the literature. I: femoral neck fractures. J Am Acad Orthop Surg. 2008;16(10):596–607. doi: 10.5435/00124635-200810000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Minne HW, Pfeifer M, Wittenberg R, Würtz R (2001) Schenkelhalsfrakturen in Deutschland: Prävention, Therapie, Inzidenz und sozioökonomische Bedeutung. [Hip Fractures in Germany] Dtsch Arztebl 98(26)
- 3.Bhandari M, Devereaux PJ, Swiontkowski MF, Tornetta P, 3rd, Obremskey W, Koval KJ, Nork S, Sprague S, Schemitsch EH, Guyatt GH. Internal fixation compared with arthroplasty for displaced fractures of the femoral neck. A meta-analysis. J Bone Joint Surg Am. 2003;85-A(9):1673–1681. doi: 10.2106/00004623-200309000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Keating JF, Grant A, Masson M, Scott NW, Forbes JF. Randomized comparison of reduction and fixation, bipolar hemiarthroplasty, and total hip arthroplasty. Treatment of displaced intracapsular hip fractures in healthy older patients. J Bone Joint Surg Am. 2006;88(2):249–260. doi: 10.2106/JBJS.E.00215. [DOI] [PubMed] [Google Scholar]
- 5.Johansson T, Bachrach-Lindstrom M, Aspenberg P, Jonsson D, Wahlstrom O. The total costs of a displaced femoral neck fracture: comparison of internal fixation and total hip replacement. A randomised study of 146 hips. Int Orthop. 2006;30(1):1–6. doi: 10.1007/s00264-005-0037-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Macaulay W, Yoon RS, Parsley B, Nellans KW, Teeny SM. Displaced femoral neck fractures: is there a standard of care? Orthopedics. 2007;30(9):748–749. doi: 10.3928/01477447-20070901-08. [DOI] [PubMed] [Google Scholar]
- 7.Bhandari M, Devereaux PJ, Tornetta P, 3rd, Swiontkowski MF, Berry DJ, Haidukewych G, Schemitsch EH, Hanson BP, Koval K, Dirschl D, Leece P, Keel M, Petrisor B, Heetveld M, Guyatt GH. Operative management of displaced femoral neck fractures in elderly patients. An international survey. J Bone Joint Surg Am. 2005;87(9):2122–2130. doi: 10.2106/JBJS.E.00535. [DOI] [PubMed] [Google Scholar]
- 8.Bjorgul K, Reikeras O. Hemiarthroplasty in worst cases is better than internal fixation in best cases of displaced femoral neck fractures: a prospective study of 683 patients treated with hemiarthroplasty or internal fixation. Acta Orthop. 2006;77(3):368–374. doi: 10.1080/17453670610046271. [DOI] [PubMed] [Google Scholar]
- 9.Eiskjaer S, Ostgard SE. Risk factors influencing mortality after bipolar hemiarthroplasty in the treatment of fracture of the femoral neck. Clin Orthop Relat Res. 1991;270:295–300. [PubMed] [Google Scholar]
- 10.Kannan A, Kancherla R, McMahon S, Hawdon G, Soral A, Malhotra R. Arthroplasty options in femoral-neck fracture: answers from the national registries. Int Orthop. 2012;36(1):1–8. doi: 10.1007/s00264-011-1354-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kim JW, Nam KW, Yoo JJ, Kim HJ. The role of preoperative bone scan for determining the treatment method for femoral neck fracture. Int Orthop. 2007;31(1):61–64. doi: 10.1007/s00264-006-0138-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sebestyen A, Boncz I, Sandor J, Nyarady J. Effect of surgical delay on early mortality in patients with femoral neck fracture. Int Orthop. 2008;32(3):375–379. doi: 10.1007/s00264-007-0331-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Balen R, Steyerberg EW, Polder JJ, Ribbers TL, Habbema JD, Cools HJ. Hip fracture in elderly patients: outcomes for function, quality of life, and type of residence. Clin Orthop Relat Res. 2001;390:232–243. doi: 10.1097/00003086-200109000-00027. [DOI] [PubMed] [Google Scholar]
- 14.Schneppendahl J, Betsch M, Petrov V, Bottner F, Thelen S, Grassmann JP, Hakimi M, Windolf J, Wild M. Recovery after hip fractures: influence of bipolar hemiarthroplasty on physical disability and social dependency in the elderly. Hip Int. 2011;21(6):751–756. doi: 10.5301/HIP.2011.8824. [DOI] [PubMed] [Google Scholar]
- 15.Kenzora JE, McCarthy RE, Lowell JD, Sledge CB. Hip fracture mortality. Relation to age, treatment, preoperative illness, time of surgery, and complications. Clin Orthop Relat Res. 1984;186:45–56. [PubMed] [Google Scholar]
- 16.Sexson SB, Lehner JT. Factors affecting hip fracture mortality. J Orthop Trauma. 1987;1(4):298–305. doi: 10.1097/00005131-198701040-00005. [DOI] [PubMed] [Google Scholar]
- 17.Lim YW, Kwon SY, Han SK, Sun DH, Choi SP, Kim YS. Postoperative mortality and factors related to mortality after bipolar hemiarthroplasty in patients with femoral neck fractures. J Arthroplasty. 2009;24(8):1277–1280. doi: 10.1016/j.arth.2009.06.019. [DOI] [PubMed] [Google Scholar]
- 18.Haidukewych GJ, Israel TA, Berry DJ. Long-term survivorship of cemented bipolar hemiarthroplasty for fracture of the femoral neck. Clin Orthop Relat Res. 2002;403:118–126. doi: 10.1097/00003086-200210000-00019. [DOI] [PubMed] [Google Scholar]
- 19.Iorio R, Schwartz B, Macaulay W, Teeney SM, Healy WL, York S. Surgical treatment of displaced femoral neck fractures in the elderly: a survey of the American Association of Hip and Knee Surgeons. J Arthroplasty. 2006;21(8):1124–1133. doi: 10.1016/j.arth.2005.12.008. [DOI] [PubMed] [Google Scholar]
- 20.Kenzora JE, Magaziner J, Hudson J, Hebel JR, Young Y, Hawkes W, Felsenthal G, Zimmerman SI, Provenzano G. Outcome after hemiarthroplasty for femoral neck fractures in the elderly. Clin Orthop Relat Res. 1998;348:51–58. doi: 10.1097/00003086-199803000-00010. [DOI] [PubMed] [Google Scholar]
- 21.Gjertsen JE, Vinje T, Lie SA, Engesaeter LB, Havelin LI, Furnes O, Fevang JM. Patient satisfaction, pain, and quality of life 4 months after displaced femoral neck fractures: a comparison of 663 fractures treated with internal fixation and 906 with bipolar hemiarthroplasty reported to the Norwegian Hip Fracture Register. Acta Orthop. 2008;79(5):594–601. doi: 10.1080/17453670810016597. [DOI] [PubMed] [Google Scholar]
- 22.Schleicher I, Kordelle J, Jurgensen I, Haas H, Melzer C. Femoral neck fractures in the elderly—bipolar hemiarthroplasty in total hip replacement. Unfallchirurg. 2003;106(6):467–471. doi: 10.1007/s00113-003-0597-6. [DOI] [PubMed] [Google Scholar]
- 23.Sierra RJ, Schleck CD, Cabanela ME. Dislocation of bipolar hemiarthroplasty: rate, contributing factors, and outcome. Clin Orthop Relat Res. 2006;442:230–238. doi: 10.1097/01.blo.0000183741.96610.c3. [DOI] [PubMed] [Google Scholar]
- 24.Ravikumar KJ, Marsh G. Internal fixation versus hemiarthroplasty versus total hip arthroplasty for displaced subcapital fractures of femur—13 year results of a prospective randomised study. Injury. 2000;31(10):793–797. doi: 10.1016/S0020-1383(00)00125-X. [DOI] [PubMed] [Google Scholar]
- 25.Baker RP, Squires B, Gargan MF, Bannister GC. Total hip arthroplasty and hemiarthroplasty in mobile, independent patients with a displaced intracapsular fracture of the femoral neck. A randomized, controlled trial. J Bone Joint Surg Am. 2006;88(12):2583–2589. doi: 10.2106/JBJS.E.01373. [DOI] [PubMed] [Google Scholar]
- 26.Dorr LD, Glousman R, Hoy AL, Vanis R, Chandler R. Treatment of femoral neck fractures with total hip replacement versus cemented and noncemented hemiarthroplasty. J Arthroplasty. 1986;1(1):21–28. doi: 10.1016/S0883-5403(86)80006-7. [DOI] [PubMed] [Google Scholar]
- 27.Ions GK, Stevens J. Prediction of survival in patients with femoral neck fractures. J Bone Joint Surg Br. 1987;69(3):384–387. doi: 10.1302/0301-620X.69B3.3584189. [DOI] [PubMed] [Google Scholar]
- 28.Smektala R, Hahn S, Schrader P, Bonnaire F, Schulze Raestrup U, Siebert H, Fischer B, Boy O (2010) Mediale Schenkelhalsfraktur: Einfluss des Versorgungszeitpunkts auf die ErgebnisqualitätErgebnisse der Daten der externen stationären Qualitätssicherung im Rahmen sekundärer Datennutzung [Medial hip neck fracture: influence of pre-operative delay on the quality of outcome. Results of data from the external in-hospital quality assurance within the framework of secondary]. Unfallchirurg 113 (4):287-292. doi:10.1007/s00113-009-1674-2 [DOI] [PubMed]
- 29.Kopp L, Edelmann K, Obruba P, Prochazka B, Blstakova K, Dzupa V. Mortality risk factors in the elderly with proximal femoral fracture treated surgically. Acta Chir Orthop Traumatol Cech. 2009;76(1):41–46. [PubMed] [Google Scholar]