Abstract
Objective
To determine the prevalence of hypertension and diabetes among members of an Ethiopian occupational cohort; and to examine the proportion of adults who were aware of their conditions.
Methods
A total of 2,153 of subjects were included in this cross-sectional study. The World Health Organization STEPwise approach for non-communicable diseases was used to collect socio-demographic data, blood pressure measures and blood samples from participants. Prevalence estimates for hypertension and diabetes were determined separately. The 95% confidence intervals for prevalence estimates were also determined.
Results
The overall prevalence of hypertension was 19.1% (95%CI: 17.1–20.8) and 22% (95%CI: 20.2–23.8) and 14.9% (95%CI: 13.4–16.4) among men and women respectively. The overall prevalence of diabetes was 6.5%(95%CI: 5.4–7.6) and 6.4%(95%CI: 5.0–7.8) and 6.6%(95%CI: 4.8–8.4) among men and women correspondingly. Notably, 15% of hypertensives reported never having had their blood pressure checked prior to the present study examination. Approximately 45% of participants who had their blood pressure checked were never diagnosed with hypertension, but were found to be hypertensive in our study. Approximately 27% of newly diagnosed diabetics (during this study) reported never having a previous blood glucose test. Among those who had their blood glucose assessed prior to this study, 17.4% were found to have diabetes but were never diagnosed.
Conclusion
The high prevalence of hypertension and diabetes reported in our study confirms findings from other Sub Saharan Africa countries, and extends the literature to urban dwelling Ethiopians where non-communicable diseases are emerging as a major public health concern.
INTRODUCTION
In 2008, World Health Organization (WHO) estimated that 13.40 million individuals died of cardiovascular diseases (CVD)1. Hypertension is one of the major risk factors for CVD. Kearney at al. reported that in the year 2000 an estimated 639 million individuals had hypertension in economically developing countries and this number is expected to rise to 1.15 billion by 20252. Uncontrolled hypertension causes pathological changes and promotes the progression of atherosclerosis and subsequent coronary heart disease (CHD), stroke, heart failure, and chronic kidney disease3. Diabetes coexists with hypertension and central obesity at a high frequency4. In 2006, 10.8 million Sub-Saharan Africans were estimated to have diabetes. This number is expected to rise to 18.7 million by 20255. Diabetes leads to vasculature complications, including atherosclerosis, known to contribute to various other disorders including stroke, small and large vesicle disease, and coronary heart disease6. A growing body of epidemiologic evidence suggests that there are a number of modifiable risk factors that lead to increased incidence of diabetes and hypertension in low income countries such as Ethiopia7. These include obesity, change in dietary habits, physical inactivity, socioeconomic changes, and excess alcohol consumption8. Given that the burden of CVD morbidity and mortality is projected to increase in developing countries, it is essential to provide current reliable data on the epidemiology of hypertension and diabetes. However, few sub-Saharan countries have undertaken the task of estimating the prevalence of both hypertension and diabetes on a nationwide scale and assessment of prevalence among various sample populations are sparse9.
In Ethiopia, few studies have evaluated the prevalence of hypertension and diabetes. For instance, a study conducted in 1982 among Ethiopian Bank employees attending a clinic in Addis Ababa found prevalence of 3.8% and 1.2% for hypertension and diabetes respectively10. A more recent study conducted among residents of Addis Ababa found the prevalence of hypertension among adults to be 31.5% among men and 28.9% among women11. Given mounting evidence suggesting increased burden of non-communicable diseases among Sub-Saharan African populations and the scarcity of studies conducted in Ethiopia, we sought to evaluate the prevalence of hypertension and diabetes among members of an epidemiologically and clinically well characterized Ethiopian occupational cohort. We also sought to examine the proportion of individuals with hypertension or diabetes who were aware of their condition. Results from our study will provide objective evidence that may be used to develop specific disease prevention and risk management strategies aimed at ultimately reducing the non-communicable disease burden in an urban African workforce.
METHODS
Study Design and Population
This study was conducted in Addis Ababa, the capital city of Ethiopia, during the months of December 2009 and January 2010. Subjects were permanent employees of the Commercial Bank of Ethiopia and teachers from government and public schools of Addis. Multistage sampling procedures were used to select participants by means of probability proportional to size (PPS) sampling12. A total of 2,153 participants were included in this study. Details of the data collection procedures were previously described13, 14. Briefly, each participant was interviewed by a trained interviewer in accordance with the WHO STEPwise approach of the WHO for non-communicable diseases surveillance in developing countries [25]. The approach had three levels: (1) questionnaire to gather demographic and behavioral information, (2) simple physical measurements, and (3) biochemical tests. Participants were interviewed by trained interviewers using the WHO STEPs structured questionnaire. Some questions were added to supplement the WHO questionnaire and to reflect on the local context.
Blood pressure was digitally measured (Microlife BP A50, Microlife AG, Switzerland) after individuals had been resting for five minutes. Two additional blood pressure measurements were taken with three minutes elapsing between successive measurements. In accordance with WHO recommendation the mean systolic and diastolic BP from the second and third measurements were considered for analyses. Mean arterial pressure was diastolic pressure plus one third of systolic BP. Blood samples were collected after a 12 hours of fasting, using proper sanitation and infection prevention techniques. The collected aliquots of blood were used to determine participants’ fasting blood glucose concentrations and lipid profiles.
All study participants provided informed consent and all research protocols were approved by the Institutional Review Boards of Addis Continental Institute of Public Health, Addis Ababa, Ethiopia and the Human Subjects Division at the University of Washington, USA.
Variable Specification
High blood pressure was defined as having systolic blood pressure (SBP) ≥140mmHg or diastolic blood pressure (DBP) ≥ 90 mmHg or on antihypertensive treatment. Isolated systolic blood pressure (ISH) was defined as having SBP ≥140mmHg and DBP < 90 mmHg. Isolated diastolic hypertension (IDH) was defined as having SBP <140mmHg and DBP ≥ 90 mmHg. Systolic and diastolic hypertension (SDH) was defined as having SBP ≥140mmHg and diastolic blood pressure DBP ≥ 90 mmHg8. Diabetes mellitus was defined using the International Diabetes Federation definition, which is a fasting blood glucose concentration of ≥126mg/dl 15.
Awareness of high blood pressure and diabetes
Participants were asked the following question: “Have you ever had your blood pressure checked?” Those who answered affirmatively were then asked, “Have you ever been told by a doctor or other health professional that your blood pressure level was high?” Those who answered affirmatively were considered aware of having a hypertension. Similar questions and definitions were used for determining participants’ awareness of their diabetes status.
Other covariates were defined as follows: body mass index (BMI), a measure of overall adiposity, was categorized according to WHO criteria (underweight: BMI <18.5 kg/m2; normal: 18.5 –24.9 kg/m2; overweight: 25.0 –29.9 kg/m2; and obese: BMI≥ 30.0 kg/m2). Alcohol consumption was classified as low (< 1 alcoholic beverage a week), moderate (1–21 alcoholic beverages a week), and high to excessive consumption (> 21 alcoholic beverages a week) according to WHO classification.16 Self-reported health status was determined by asking the participant to rate their overall health as excellent, very good, good, fair, or poor. Participants were grouped, a priori, as, those having “good to excellent” and “fair to poor” health, respectively.
Statistical Analysis
Frequency distributions of socio-demographic, behavioral and clinical characteristics of study subjects by gender were examined. Continuous variables were expressed as mean with standard deviation of means (SEM). Categorical variables were expressed as number (percent, %). Chi-Square tests were used to evaluate differences in means for continuous variables. Prevalence estimates for hypertension and diabetes were determined separately. Using previously described methods, 95% confidence intervals (95% CI) for prevalence estimates were determined.17 All reported p values were two tailed, and statistical significance was set at α=0.05. All statistical analyses were performed using IBM SPSS, version 19 (Chicago, IL, USA).
RESULTS
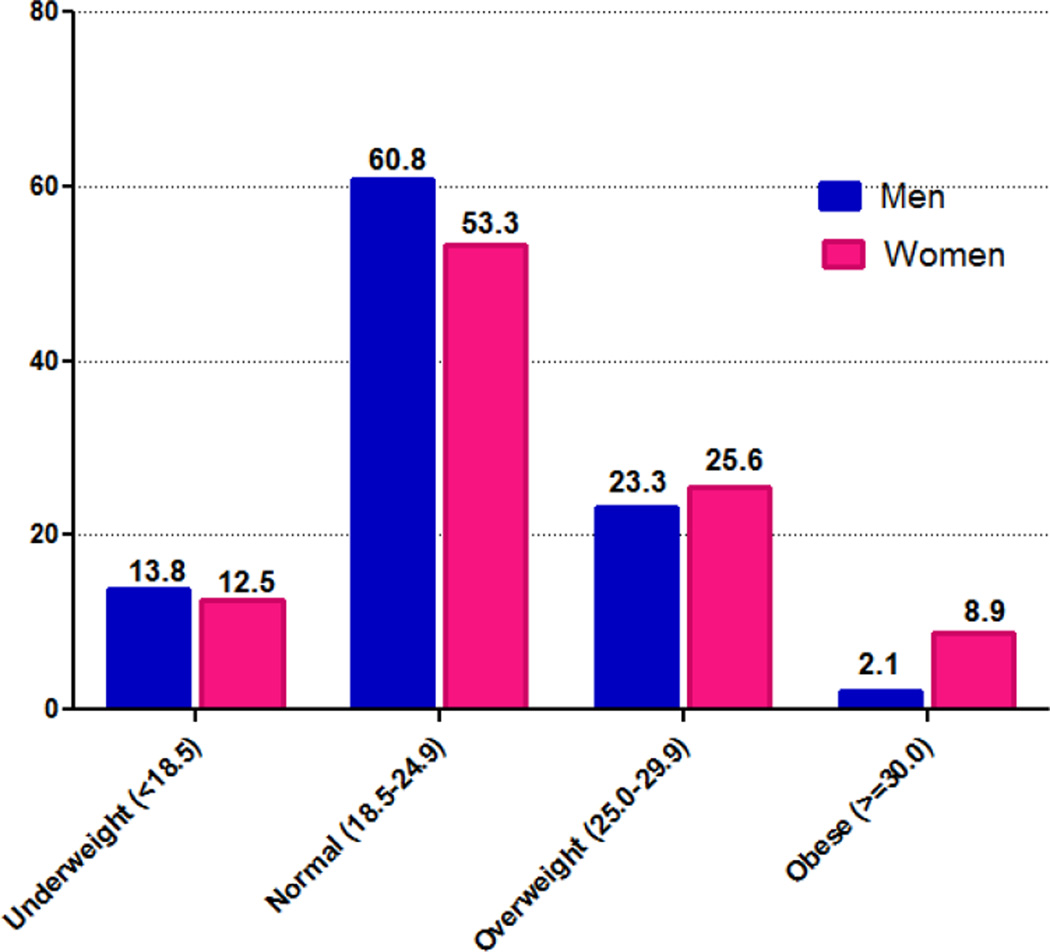
Approximately 80% of participants reported having some college education and 9% reported being current smokers(14.3% men and 0.7% women). Compared with women, men were more likely to report heavy alcohol consumption(11.8% versus 0.4%) and consumption of khat(an evergreen plant with amphetamine-like effects commonly used as a mild stimulant for social recreation and improve work performance in Ethiopia)15, 16 (14% versus 0.8%). Approximately 26% of women were overweight, whilst the corresponding proportion among men was 24%. As shown in Figure 1, the frequency of obesity was more than 4-fold higher among women, as compared with their male counterparts (9.6% vs. 2.2%). Age-group specific mean systolic, diastolic and arterial blood pressures for men and women are presented in Table 2. Overall, mean systolic, diastolic, and arterial blood pressure of men were higher than that of women. For men, mean systolic, diastolic and arterial blood pressures were 124.1mmHg, 79.8mmHg, 94.6mmHg, respectively. The corresponding values for women were 116.0mmHg, 76.0 mmHg, 89.3mmHg. Noted gender differences in mean blood pressure values persisted across all age groups. As expected, mean systolic diastolic and arterial blood pressure values increased with increasing age increased for both men and women.
Figure 1.
Distribution of BMI by gender
Table 2.
Age and gender specific mean systolic, diastolic and mean arterial blood pressures
| Systolic Blood Pressure | Diastolic Blood Pressure | Mean Arterial Blood Pressure | |
|---|---|---|---|
| Mean [SE] (95% CI) | Mean [SE] (95% CI) | Mean [SE] (95% CI) | |
| Men (n= 1298) | |||
| Overall | 124.1[0.4](123.2,125.0) | 79.8[.4](79.02,80.59) | 94.6[0.4](93.8,95.3) |
| Age (years) | |||
| ≤24 | 117.03[0.7] (115.6,118.5) | 73.08[.6] (72.0,74.2) | 87.73[0.6] (86.6,88.8) |
| 25–34 | 119.76[0.6] (118.7,120.8) | 77.6[.4] (76.6,78.4) | 91.66[0.4] (90.8,92.5) |
| 35–44 | 123.06[0.8] (121.4,124.7) | 82.70[1.8] (79.2,86.2) | 96.15[1.3] (93.7,98.6) |
| 45–54 | 133.69[1.3] (131.2,136.2) | 85.91[.7] (84.5,87.4) | 101.84[0.9] (100.1,103.6) |
| ≥55 | 138.70[1.8] (135.2,142.2) | 85.73[1.1] (83.6,87.8) | 103.38[1.2] (101.0,105.8) |
| Women (n=855) | |||
| Overall | 116.0[0.6](114.9,117.1) | 75.96[0.4](75.24,76.65) | 89.30[0.4](88.53,90.09) |
| Age (years) | |||
| ≤24 | 108.93[0.8](107.3,110.6) | 71.64[0.7](70.3,73.0) | 84.07[0.7](82.8,85.4) |
| 25–34 | 109.03[0.7](107.6,110.5) | 72.53[0.5] (71.5,73.5) | 84.70[0.5] (83.7,85.7) |
| 35–44 | 117.91[1.2] (115.5,120.4) | 78.66[0.8] (77.0,80.3) | 91.75[0.9] (90.0,93.6) |
| 45–54 | 126.70[1.2] (124.3,129.0) | 81.45[0.7] (80.0,82.8) | 96.52[0.8] (95.0,98.1) |
| ≥55 | 134.70[2.9] (128.8,140.5) | 82.91[0.4] (80.0,85.8) | 100.17[1.8] (96.6,103.7) |
Age-specific prevalence estimates of hypertension, isolated systolic hypertension, isolated diastolic hypertension and systolic and diastolic hypertension for men and women are summarized in Table 3. Overall, hypertension was more prevalent among men 22% (95% CI: 20.2–23.8) than among women among 14.9% (95% CI: 13.4–16.4). As expected, prevent hypertension was positively associated with age in both men and women. Overall, men had a higher frequency of isolated systolic hypertension, isolated diastolic hypertension and higher systolic and diastolic hypertension compared with their female counterparts.
Table 3.
Prevalence hypertension by gender and age groups
| All N=2153 |
Women (N=855) | Men (N=1,298) | |
|---|---|---|---|
| High Blood Pressure(HBP)* | |||
| Overall | 19.1(17.4–20.8) | 14.9(13.4–16.4) | 22.0 (20.2–23.8) |
| Age (years) | |||
| ≤24 (n=449) | 5.6(3.4–7.7) | 5.0(1.9–8.1) | 6.0(3.0–9.0) |
| 25–34 (n=757) | 9.0(9.6–11.1) | 4.1(1.7–6.5) | 11.7(8.8–14.6) |
| 35–44 (n=351) | 18.5(14.4–22.7) | 16.7(10.5–22.9) | 19.8(14.3–25.3) |
| 45–54 (n=409) | 37.7(32.9–42.49) | 29.0(22.3–35.7) | 44.8(38.1–51.5) |
| ≥55 (n=187) | 53.5(46.2–60.8) | 50.9(37.4–64.4) | 54.5(45.8–63.2) |
| Isolated Systolic Hypertension(ISH)* | |||
| Overall | 4.6(3.7–5.5) | 3.9(3.1–4.7) | 5.1(4.2–6.1) |
| Age (years) | |||
| ≤24 | 1.1(0.1–2.1) | 0.5(0.0–1.5) | 1.6(0.1–3.2) |
| 25–34 | 2.0(1.0–3.0) | 1.5(0.0–2.98) | 2.3(0.9–3.7) |
| 35–44 | 1.7(0.3–3.1) | 2.1(0.0–4.5) | 1.4(0.2–3) |
| 45–54 | 9.3(6.4–12.2) | 8.1(4.1–12.1) | 10.3(6.2–14.4) |
| ≥55 | 18.7(13.24.4) | 18.2(7.8–28.6) | 18.9(12.1–25.7) |
| Isolated Diastolic Hypertension(IDH)* | |||
| Overall | 6.1(5.1–7.1) | 5.4(4.4–6.4) | 6.6(5.5–7.7) |
| Age (years) | |||
| ≤24 | 3.3(1.6–5.0) | 3.5(.9–6.1) | 3.2(1–5.4) |
| 25–34 | 4.9(3.3–6.5) | 2.6(.7–4.5) | 6.2(4–8.4) |
| 35–44 | 9.1(6–12.2) | 9.7(4.8–14.6) | 8.7(4.8–12.6) |
| 45–54 | 7.8(5.1–10.5) | 6.5(2.9–10.1) | 9.0(5.2–12.8) |
| ≥55 | 8.6(4.5–12.7) | 10.9(2.5–19.3) | 7.6(3.0–12.2) |
| Systolic and Diastolic Hypertension(SDH)* | |||
| Overall | 7.2(6.1–8.3) | 4.7(3.8–5.6) | 8.9(7.7–10.1) |
| Age (years) | |||
| ≤24 | 1.1(0.1–2.1) | 1.0(0.0–2.4) | 1.2(0.0–2.6) |
| 25–34 | 2.1(1.1–3.1) | 0.0(0.0–0.0) | 3.3(1.7–4.9) |
| 35–44 | 5.1(2.8–7.5) | 4.2(0.9–7.5) | 5.8(2.6–9.1) |
| 45–54 | 18.3(14.5–22.1) | 11.8(7.1–16.5) | 23.8(18.0–30.0) |
| ≥55 | 22.5(16.4–28.6) | 18.2(7.8–28.6) | 24.2(16.7–31.7) |
HBP: SBP ≥ 140 mmHg or DBP ≥ 90 mmHg or on antihypertensive treatment, ISH: SBP ≥ 140 mmHg and DBP <90 mmHg; IDH: SBP < 140 mmHg and DBP ≥ 90 mmHg; SDH:SBP ≥ 140 mmHg and DBP ≥ 90 mmHg.
A total of 548 participants were found to have diabetes or pre-diabetes (Table 4). Overall, the frequencies of diabetes mellitus and pre-diabetes were largely similar for women (6.6% and 21.8%) and men (6.4% and 21.6%). The prevalence of diabetes (21.8% vs. 13.5%), however, was substantially higher among women aged 45–54 years as compared with their similarly aged male counterparts. Likewise, the prevalence of pre-diabetes was higher among women aged ≥55 years (30.2% vs. 29.1%) as compared with similarly aged men.
Table 4.
Prevlance of diabetes and pre-diabetes by gender and age groups
| All % (95%CI) |
Women % (95%CI) |
Men % (95%CI) |
|
|---|---|---|---|
| Diabetes Mellitus | |||
| Overall | 6.5(5.4–7.6) | 6.6(4.8–8.4) | 6.4(5.0–7.8) |
| Age (years) | |||
| ≤24 (n=377) | 0.8(−0.1–1.7) | 0.6(−0.6–1.8) | 1.0(−0.4–2.4) |
| 25–34 (n=688) | 1.3(0.4–2.2) | 0.4(−0.4–1.2) | 18.0(14.4–21.6) |
| 35–44 (n=324) | 6.2(3.5–8.9) | 3.0(0.0–5.9) | 8.3(4.3–12.3) |
| 45–54 (n=382) | 17.3(13.4–21.2) | 21.8(15.5–28.1) | 13.5(8.8–18.2) |
| ≥55 (n=180) | 15.6(10.2–21.0) | 13.2(3.9–22.5) | 16.5(9.9–23.1) |
| Pre-diabetes | |||
| Overall | 21.6(19.7–23.5) | 21.8(19.4–24.2) | 21.6(19.7–23.5) |
| Age (years) | |||
| ≤24 (n=377) | 21.7(17.5–25.9) | 21.2(14.9–27.5) | 22.2(16.4–27.9) |
| 25–34 (n=688) | 16.4(13.6–19.2) | 15.3(10.7–19.9) | 17.0(13.4–20.5) |
| 35–44 (n=324) | 21.0(16.5–25.5) | 21.9(14.7–29.1) | 20.3(14.5–26.1) |
| 45–54 (n=382) | 27.8(23.2–32.4) | 27.0(20.3–33.7) | 28.4(22.1–34.6) |
| ≥55 (n=180) | 29.4(22.6–36.2) | 30.2(17.6–42.8) | 29.1(21.0–37.1) |
Diabetes Mellitus defined as fasting glucose blood levels ≥ 126 mg/dl (or with normal glucose but under treatment (diet or medical) for diabetes. Pre-diabetes defined as having as fasting blood glucose level between 100 and 125 mg/dl. Fasting is defined as no caloric intake for at least 8 hour
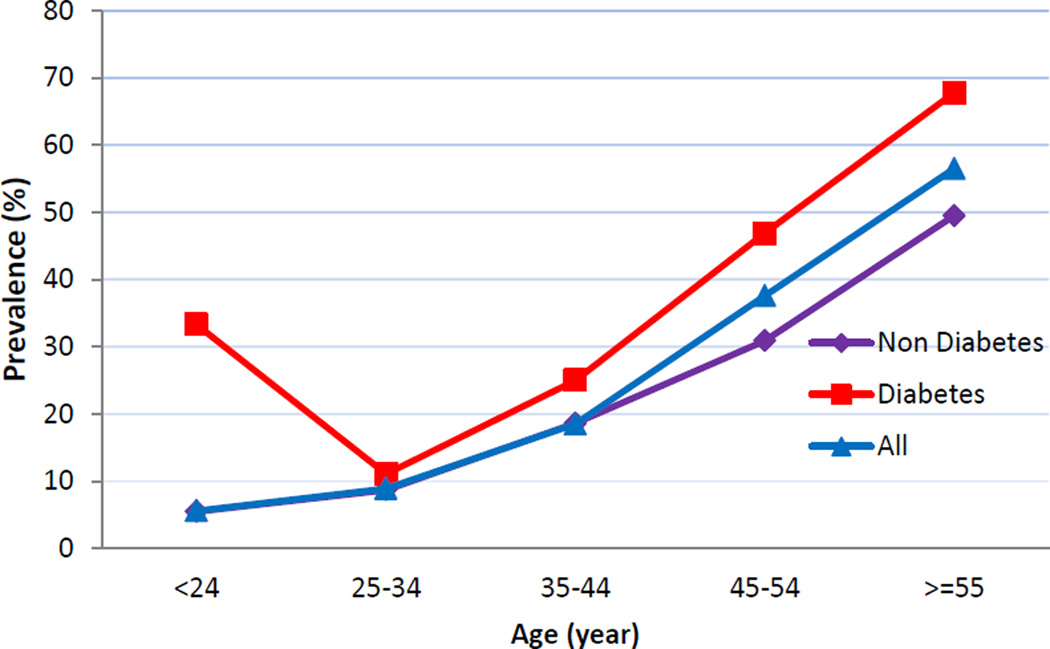
Figure 2 shows prevalence of hypertension by age group and diabetes status. Diabetics have the highest prevalence of hypertension across all age groups. Moreover, the figure illustrates the positive trend of increasing prevalent hypertension with increasing age, irrespective of participants’ diabetes status.
Figure 2.
Prevalence of hypertension by age group and diabetes status
As shown in Table 5, 85% of individuals with hypertension reported having ever checked their blood pressure. Among those who were found to be hypertensive and reported to have had their blood pressure checked by a physician or other health professional, the proportion that was not aware of their condition was 45%. Approximately 2 % of those who reported having checked their blood pressure but did not check their results were found to have hypertension. Among hypertensives, the proportion that was not aware of their hypertension status was 15%.
Table 5.
Relationship of blood pressure and diabetes measurements with participants’ history of health services utilization
| Health services utilization | Hypertension | |
|---|---|---|
| No(N=1,738) | Yes(N=411) | |
| Ever checked blood pressure | n (%) | n (%) |
| No | 538(30.9) | 62(15) |
| Yes | 1,200(69.1) | 349(85.0) |
| Didn’t get diagnosis for hypertension | 1,040(86.7) | 157(45) |
| Diagnosed with hypertension | 1,26(10.5) | 186(53.3) |
| Didn’t check results | 34(2.8) | 6(1.7) |
| Diabetes Mellitus | ||
| Ever checked blood glucose level | No(N=1,400) | Yes(N=126) |
| No | 1,111(79.4) | 34(27.0) |
| Yes | 289(20.6) | 92 (73.0) |
| Didn’t get diagnosis for diabetes | 268(92.7) | 16(17.4) |
| Diagnosed with diabetes | 21(7.3) | 76(82.6) |
Among participants who found to have diabetes mellitus, 73% of them reported having checked their blood glucose level checked by a physician or other health professional. Among those who were found to be diabetics and reported to have had their blood glucose level checked, the proportion that was not aware of their condition was 17%. Among diabetics who reported to have never checked their blood glucose in the past, the proportion that was not aware of their diabetes status was 27%.
DISCUSSION
Prevalence estimates for hypertension and diabetes among members of our occupational cohort of bank employees and teachers are quite a bit higher than reports from an earlier study of Ethiopian bank employees10, 17. Our reported prevalence estimates are consistent with the larger literature documenting positive secular trends in hypertension and diabetes over the past two decades. Additionally, data from our cross-sectional study suggests that a substantial proportion of individuals with hypertension and/or diabetes are unaware of their condition. Our findings underscore the conclusions drawn from the World Health Organization report which emphasize a need for enhanced non-communicable disease surveillance, prevention and health promotion activities in developing countries.
We are aware of only four published studies focused on hypertension prevalence among Ethiopians. In one study conducted in a rural and semi-urban community of Butajira, investigators reported that 8.2% of women and 12.3% of men had prevalent hypertension 18. Pauletto et al, reported exceedingly low prevalence estimates for hypertension in their study of semi-nomadic residents of Arssi (0.4%) and urban residents of Shashamane (3.15%) 19. A recent study conducted among residents of Addis Ababa estimated a prevalence of 31.5% among men and 28.9% among women11. Compared to studies conducted outside Addis Ababa, our prevalence estimates are higher (14.9% in women and 22% in men), but lower than the community based study in Addis Ababa. Despite variations in study design and underlying differences in study population characteristics (e.g., age and gender distributions, community residents, workers, urban, rural residents), available evidence suggests that hypertension is an increasing health problem in Ethiopia.
Of note, hypertension prevalence estimates observed among members of the present Ethiopian occupational cohortare comparable with estimates reported from studies conducted in other Sub-Saharan African countries. For example, in Enugu, Nigeria the hypertension prevalence was found to be 35.4% in semi-urban population and 25.1% in rural communities20. In rural and urban Mozambique the overall prevalence of hypertension was reported to be 33.1% 21. Similarly in Tanzania prevalence of hypertension among men and women was reported to be about 31% 22. Taken together, these data suggest the emergence of hypertension as an important public health problem, and the likely importance of taking a pan-African approach when considering strategies for hypertension prevention and control programs in low income countries.
We are aware of two published reports that evaluated the prevalence of diabetes among Ethiopian adults. The first study conducted among bank employees in Addis Ababa reported a prevalence of diabetes of 0.3% in women and 1.4% in men 10. The second study was conducted among high school students and antenatal care attendees in Gondar, one of the country’s northern cities. The investigators noted prevalence estimates of 0.5% and 2.4% respectively23. Some investigators have provided diabetes prevalence estimates among recent Ethiopian immigrants in Israel. For instance, Rubinstein et al. conducted a study among Ethiopian Jews in 1991 and found a prevalence of diabetes of 0.4% upon their arrival in Israel24, 25. More recently, Cohen et al. in their study of Ethiopian immigrants in Israel, reported the prevalence of diabetes to be 8.9%25. The estimate in our study (6.5%) is lower than the prevalence reported by Cohen, but higher than what was reported by Rubinstein and the two previous studies in Ethiopia24, 25. The results of our study, however, are in general agreement with some reports from other Sub-Saharan countries such Cameroon (6.1%), Mauritania (6.0%) and the Republic of Congo (7.1%)26. Our diabetes prevalence estimates are, however, substantially higher than reports from Contrary to our results, some have reported low prevalence of diabetes mellitus in other Sub-Saharan countries. Mbanya et al. found the prevalence of diabetes to be 0.85% in rural areas and 0.9% in urban areas of Cameroon27. Motala et al. reported a prevalence of 3.9 among its study participants in rural South Africa28. A recent study by Christensen et al. reported a prevalence of 4.2% in both rural and urban areas of Kenya29. Differences in diabetes prevalence estimates across studies maybe due to different diabetic diagnosis methods used and research setting (urban vs. rural).
In our study we found that among those who were found to be hypertensives and diabetics, the proportion that was not aware of their condition was 45% and 17%, respectively. A study by Damasceno et al in Mozambique indicated that only 10.6% of men and 18.4% of women were aware of their hypertension21. A study in Nigeria showed that among the 42% of those screened for hypertension, 70.6% of them were not aware of their condition30. Another study in Ghana reported that 69.9% of participants were previously undiagnosed31. High number of newly diagnosed cases during the study suggests that there is low awareness of these chronic conditions among the study population. Early recognition of participants with hypertension and diabetes should be considered to be of importance, not only for clinical disease management, but also for education and empowerment. Moreover, our study findings showed that 4.5% of participants who ever checked their blood pressure did not check their result. Investigators have speculated measurements of blood pressure and other biological risk factors of CVD can be useful to motivate change as long as the results are presented in a clear and meaningful way8. Strategies that increase an adequately and appropriately trained health work force could be one modality.
To the best of our knowledge this is the first study of hypertension and diabetes among working Ethiopian adults. Our study adds to the limited body of evidence on hypertension and diabetes in Ethiopia. Some limitations should be considered when interpreting our study. Our findings may not be generalizable to rural populations of Ethiopia. Our study participants are all working professionals who are urban residents and fairly well educated. Therefore, their health status may not be representative of the general populations.
Our substantial finding of hypertension and diabetes prevalence, and the rising prevalence projections for Sub-Saharan Africa, suggests that treatment and prevention of these diseases are urgently needed2, 32. Our study indicates that there may be a large number of people who have hypertension or diabetes in Ethiopia, but are not aware of it. When these diseases go undiagnosed they can cause further complications, which is why awareness and promotion of health services utilization are so important.3 The economic impact of these diseases on the work place institutions as well as the health care system should also be assessed. The health care system may not be equipped to handle the increased burden of chronic disease management and control. Our findings underscore the need for disease prevention and health promotion programs to prevent hypertension and diabetes.
Table 1.
Socio-demogrpahic characteristics of the study population
| Characteristic | All N=2,153 |
Women N=855 |
Men N=1,298 |
|---|---|---|---|
| Age (years) | n(%) | n(%) | n(%) |
| ≤24 | 449(20.9) | 200(23.4) | 249(19.2) |
| 25–34 | 757(35.2) | 270(31.6) | 487(37.5) |
| 35–44 | 351(16.3) | 144(16.8) | 207(15.9) |
| 45–54 | 409(19.0) | 186(21.8) | 409(19.0) |
| ≥55 | 187(8.7) | 55(6.4) | 132(10.2) |
| Education | |||
| ≤ High school | 630(29.3) | 353(41.3) | 277(21.3) |
| ≥ College education | 1523(70.7) | 502(58.7) | 1021(78.7) |
| Marital Status | |||
| Single | 1100(51.2) | 351(41.1) | 749(57.9) |
| Married | 909(42.3) | 415(48.7) | 494(38.2) |
| Other | 138(6.4) | 87(10.2) | 51(3.9) |
| Smoking status | |||
| Non smoker | 1862(86.5) | 848(99.2) | 1014(78.1) |
| Current smoker | 192(8.9) | 6(0.7) | 186(14.3) |
| Previous smoker | 99(4.6) | 1(0.1) | 98(7.6) |
| Alcohol consumption | |||
| Non drinker | 1181(54.9) | 616(72.0) | 565(43.5) |
| Moderate | 961(44.6) | 239(28.0) | 722(55.6) |
| Heavy | 11(0.5) | 0(0.0) | 11(0.8) |
| Khat chewing | |||
| No | 1963(91.2) | 847(99.2) | 1116(86) |
| Yes | 189(8.8) | 7(0.8) | 182(14.0) |
| Family size | |||
| 1–2 | 885(41.1) | 273(31.9) | 612(47.1) |
| 3–5 | 1005(46.7) | 462(54.0) | 543(41.8) |
| ≥6 | 263(12.2) | 120(14.0) | 143(11.0) |
| Self-reported health status | |||
| Poor/Fair | 862(40) | 377(44.1) | 485(37.4) |
| Good/Excellent | 1291(60) | 478(55.9) | 813(62.6) |
Acknowledgements
This research was completed while Ms. Lemba D. Nshisso and Ms. Angela Reese were research training fellows with the Multidisciplinary International Research Training (MIRT) Program of the University and Washington, School of Public Health. The MIRT Program is supported by an award from the National Institutes of Health, National Institute on Minority Health and Health Disparities (T37- MD001449). The authors thank Addis Continental Institute of Public Health for providing facilities and logistics support throughout the research process. The authors also thank the Commercial Bank of Ethiopia and Addis Ababa Education Office for granting access to conduct the study and International Clinical Laboratories for completing all laboratory analyses.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest: NIL
References
- 1.WHO. The Global Burden of Disease 2004 Update. Geneva, Switzerland: World Health Organization; 2004. [Google Scholar]
- 2.Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365(9455):217–223. doi: 10.1016/S0140-6736(05)17741-1. [DOI] [PubMed] [Google Scholar]
- 3.Post WS, Hill MN, Dennison CR, Weiss JL, Gerstenblith G, Blumenthal RS. High prevalence of target organ damage in young, African American inner-city men with hypertension. J Clin Hypertens (Greenwich) 2003;5(1):24–30. doi: 10.1111/j.1524-6175.2003.01246.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364(9438):937–952. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 5.Roglic G, Unwin N, Bennett PH, Mathers C, Tuomilehto J, Nag s, et al. The burden of mortality attributable to diabetes: realistic estimates for the year 2000. Diabetes Care. 2005;28(9):2130–2135. doi: 10.2337/diacare.28.9.2130. [DOI] [PubMed] [Google Scholar]
- 6.Labarthe D. Epidemiology and prevention of cardiovascular diseases : a global challenge. Gaithersburg, Md: Aspen Publishers; 1998. [Google Scholar]
- 7.Amuna P, Zotor FB. Epidemiological and nutrition transition in developing countries: impact on human health and development. Proc Nutr Soc. 2008;67(1):82–90. doi: 10.1017/S0029665108006058. [DOI] [PubMed] [Google Scholar]
- 8.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42(6):1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 9.Dalal S, Beunza JJ, Volmink J, Adebamowo C, Bajunirwe F, Njelekela M, et al. Non-communicable diseases in sub-Saharan Africa: what we know now. Int J Epidemiol. 2011;40(4):885–901. doi: 10.1093/ije/dyr050. [DOI] [PubMed] [Google Scholar]
- 10.Teklu B. Chronic disease prevalence in Ethiopian bank employees. Ethiop Med J. 1982;20(2):49–54. [PubMed] [Google Scholar]
- 11.Tesfaye F, Byass P, Wall S. Population based prevalence of high blood pressure among adults in Addis Ababa: uncovering a silent epidemic. BMC Cardiovasc Disord. 2009;9:39. doi: 10.1186/1471-2261-9-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Foreman EK. Survey sampling principles. M. Dekker: New York; 1991. [Google Scholar]
- 13.Wai WS, Dhami RS, Gelaye B, Girma B, Lemma S, Berhane Y, et al. Comparison of measures of adiposity in identifying cardiovascular disease risk among Ethiopian adults. Obesity (Silver Spring) 2011 doi: 10.1038/oby.2011.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tran A, Gelaye B, Girma B, Lemma S, Berhane Y, Bekele T, et al. Prevalence of metabolic syndrome among working adults in Ethiopia. Int J Hypertens. 2011;2011:193719. doi: 10.4061/2011/193719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kalix P. Khat: scientific knowledge and policy issues. Br J Addict. 1987;82(1):47–53. doi: 10.1111/j.1360-0443.1987.tb01436.x. [DOI] [PubMed] [Google Scholar]
- 16.Belew M, Kebede D, Kassaye M, Enquoselassie F. The magnitude of khat use and its association with health, nutrition and socio-economic status. Ethiop Med J. 2000;38(1):11–26. [PubMed] [Google Scholar]
- 17.Teklu B. Hypertension amongst bank employees in urban Ethiopia. Ethiop Med J. 1983;21(4):217–221. [PubMed] [Google Scholar]
- 18.Tesfaye F, Nawi NG, Van Minh H, Byass P, Berhane Y, Bonita R, et al. Association between body mass index and blood pressure across three populations in Africa and Asia. J Hum Hypertens. 2007;21(1):28–37. doi: 10.1038/sj.jhh.1002104. [DOI] [PubMed] [Google Scholar]
- 19.Pauletto P, Caroli M, Pessina AC, Dal Palu C. Hypertension prevalence and age-related changes of blood-pressure in semi-nomadic and urban Oromos of Ethiopia. Eur J Epidemiol. 1994;10(2):159–164. doi: 10.1007/BF01730365. [DOI] [PubMed] [Google Scholar]
- 20.Ulasi II, Ijoma CK, Onodugo OD. A community-based study of hypertension and cardio-metabolic syndrome in semi-urban and rural communities in Nigeria. BMC Health Serv Res. 2010;10:71. doi: 10.1186/1472-6963-10-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Damasceno A, Azevedo A, Silva-Matos C, Prista A, Diogo D, Lunet N. Hypertension prevalence, awareness, treatment, and control in mozambique: urban/rural gap during epidemiological transition. Hypertension. 2009;54(1):77–83. doi: 10.1161/HYPERTENSIONAHA.109.132423. [DOI] [PubMed] [Google Scholar]
- 22.Edwards R, Unwin N, Mugusi F, Whiting D, Rashid S, Kissima J, et al. Hypertension prevalence and care in an urban and rural area of Tanzania. J Hypertens. 2000;18(2):145–152. doi: 10.1097/00004872-200018020-00003. [DOI] [PubMed] [Google Scholar]
- 23.Peters WH. A study of the prevalence of diabetes mellitus in Northern Ethiopia. Dutsch Gesundheitswesen. 1983;38:1283–1289. [Google Scholar]
- 24.Rubinstein A, Graf E, Landau E, Reisin LH, Goldbourt U. Prevalence of diabetes mellitus in Ethiopian immigrants. Isr J Med Sci. 1991;27(5):252–254. [PubMed] [Google Scholar]
- 25.Cohen MP, Stern E, Rusecki Y, Zeidler A. High prevalence of diabetes in young adult Ethiopian immigrants to Israel. Diabetes. 1988;37(6):824–828. doi: 10.2337/diab.37.6.824. [DOI] [PubMed] [Google Scholar]
- 26.WHO. [accessed on September 9, 2011];STEPS Country Reports. Available at: http://www.who.int/chp/steps/reports/en/index.html.
- 27.Mbanya JC, Ngogang J, Salah JN, Minkoulou E, Balkau B. Prevalence of NIDDM and impaired glucose tolerance in a rural and an urban population in Cameroon. Diabetologia. 1997;40(7):824–829. doi: 10.1007/s001250050755. [DOI] [PubMed] [Google Scholar]
- 28.Motala AA, Esterhuizen T, Gouws E, Pirie FJ, Omar MA. Diabetes and other disorders of glycemia in a rural South African community: prevalence and associated risk factors. Diabetes Care. 2008;31(9):1783–1788. doi: 10.2337/dc08-0212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Christensen DL, Friis H, Mwaniki DL, Kilonzo B, Tetens I, Boit MK, et al. Prevalence of glucose intolerance and associated risk factors in rural and urban populations of different ethnic groups in Kenya. Diabetes Res Clin Pract. 2009;84(3):303–310. doi: 10.1016/j.diabres.2009.03.007. [DOI] [PubMed] [Google Scholar]
- 30.Ulasi II, Ijoma CK, Onwubere BJ, Arodiwe E, Onodugo O, Okafor C. High prevalence and low awareness of hypertension in a market population in enugu, Nigeria. Int J Hypertens. 2011;2011:869675. doi: 10.4061/2011/869675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Amoah AG, Owusu SK, Adjei S. Diabetes in Ghana: a community based prevalence study in Greater Accra. Diabetes Res Clin Pract. 2002;56(3):197–205. doi: 10.1016/s0168-8227(01)00374-6. [DOI] [PubMed] [Google Scholar]
- 32.Mbanya JC, Motala AA, Sobngwi E, Assah FK, Enoru ST. Diabetes in sub-Saharan Africa. Lancet. 2010;375(9733):2254–2266. doi: 10.1016/S0140-6736(10)60550-8. [DOI] [PubMed] [Google Scholar]