Abstract
Alcoholic beverages are causally related to esophageal cancer. The genetic polymorphisms of the alcohol-metabolizing enzymes ADH1B rs1229984 and ALDH2 rs671 may modulate individual differences in alcohol-oxidizing capability. A case-control study was conducted to evaluate the genetic effects of these two functional single nucleotide polymorphisms (SNPs) on the development of esophageal cancer. A total of 380 esophageal squamous cell carcinoma cases and 380 controls were recruited. Genotypes were determined by matrix-assisted laser desorption/ionization time-of-flight mass spectrometry. Variant alleles of the functional polymorphism ADH1B rs1229984 SNP were associated with an increased risk of esophageal cancer [adjusted odds ratio (OR)=2.39, 95% confidence interval (CI)=1.42–4.03 for ADH1B rs1229984 GG vs. AA]. There was a borderline-significantly decreased risk between the ALDH2 rs671 genotype and esophageal cancer (adjusted OR=0.47, 95% CI=0.22–1.00 for ALDH2 rs671 AA vs. GG). Stratified analyses indicated that both of these effects were more evident among male, younger subjects and smokers. In conclusion, the functional polymorphisms ADH1B rs1229984 and ALDH2 rs671 may contribute to susceptibility to esophageal cancer, particularly among male, younger subjects and smokers.
Keywords: ADH1B, ALDH2, polymorphisms, esophageal cancer, molecular epidemiology
Introduction
Esophageal cancer is an extremely aggressive cancer, of which China has high-incidence regions (1). Esophageal squamous cell carcinoma (ESCC) is a subtype of esophageal cancer which accounts for >90% of cases (2). Esophageal cancer is known to be associated with environmental carcinogens. Epidemiological studies indicate that use of tobacco and consumption of alcohol are major risk factors for esophageal cancer. However, only a subset of individuals exposed to tobacco and alcohol develop esophageal cancer, suggesting a role of host susceptibility factors in cancer development. The genetic basis of esophageal cancer is complex and appears to involve multiple genes. Some studies have suggested that genetic polymorphisms might explain individual differences in susceptibility to esophageal cancer (3).
Alcohol intake may be causally related to cancer of the oral cavity, pharynx, larynx and esophagus. Ethanol is oxidized to acetaldehyde and then to acetate by alcohol dehydrogenase (ADH) and aldehyde dehydrogenase (ALDH); both of which have genetic polymorphisms. The genetic polymorphisms of alcohol-metabolizing enzymes modulate individual differences in alcohol-oxidizing capability and drinking behavior (4).
In humans, the major enzymes involved in the alcohol-metabolizing pathways are alcohol dehydrogenase 1B (ADH1B) and aldehyde dehydrogenase 2 (ALDH2). Alcohol is first oxidized by ADH to acetaldehyde, which is oxidized to acetate by ALDH. These enzymes are mainly expressed in the liver, but are also present in the gastrointestinal tract (5).
The gene encoding the ADH1B enzyme is located on chromosome 4q22, and the ADH1B gene (encoding for subunit β) is the locus responsible for the majority of the ADH activity on ethanol in the liver (6). It has been predicted that individuals expressing variants of ADH1B in particular could have different rates of alcohol elimination (7). ADH1B is a low Km (Michaelis constant)-class enzyme and exhibits high activity in catalyzing ethanol to acetaldehyde (6). The most frequently reported locus is ADH1B Arg47His (rs1229984). In ADH1B His/His individuals, which are associated with flushing or other reactions to alcohol, the activity of ADH1B has been demonstrated to be decreased by 40-fold (8).
The sequence variant (rs671) on chromosome 12q24.2 was found to be associated with inactive ALDH2. A mutant allele, ALDH2 AA, has a single point mutation (G→A transition in exon 12) at position 1510 of the active ALDH2 GA gene. This results in the substitution of glutamic acid 504 to lysine, and therefore produces inactive ALDH2 (4,9,10).
A recent genome-wide association study identified the variation of ADH1B rs1229984 and ALDH2 rs671 polymorphisms as risk factors for esophageal cancer (11). Another genome-wide association study reported that variations of ADH1B rs1229984 and ALDH2 rs671 coupled with alcohol drinking and smoking synergistically enhanced the risk of esophageal cancer (12).
Due to the biological and pathological significance of ADH1B and ALDH2, functional genetic variations in the ADH1B and ALDH2 genes may contribute to the development of esophageal cancer. We evaluated the association between ADH1B and ALDH2 genotypes and susceptibility to esophageal cancer in a hospital-based case-control study. Genotyping analyses were conducted for the two SNPs with 380 ESCC cases and 380 controls in a Chinese population.
Patients and methods
Ethical approval of the study protocol
This hospital-based case-control study was approved by the Review Board of Jiangsu University (Zhenjiang, China). All subjects provided written informed consent prior to inclusion in the study.
Study subjects
A total of 380 subjects with esophageal cancer were consecutively recruited from the Affiliated People’s Hospital of Jiangsu University and Affiliated Hospital of Jiangsu University (Jiangsu, China) between October 2008 and November 2009. All cases of esophageal cancer were diagnosed as ESCC by pathological means. The exclusion criteria were patients who previously had cancer, any metastasized cancer, radiotherapy or chemotherapy. The controls were patients without cancer who were frequency-matched to the cases with regard to age (±5 years) and gender, and were recruited from the two abovementioned hospitals during the same period. The majority of the control subjects had trauma or infectious diseases.
Each subject was personally questioned by trained interviewers using a pre-tested questionnaire to obtain information on demographic data (e.g., age, gender) and related risk factors (including tobacco smoking and alcohol consumption). Following the interview, 2 ml samples of venous blood were collected from each subject. Individuals who smoked one cigarette per day for >1 year were defined as ‘smokers’. Subjects who consumed ≥3 alcoholic drinks a week for >6 months were considered to be ‘alcohol drinkers’.
Isolation of DNA and genotyping by matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-ToF-MS)
Blood samples were collected from patients using Vacutainers and transferred to tubes lined with ethylenediaminetetraacetic acid (EDTA). Genomic DNA was isolated from whole blood using the QIAamp DNA Blood Mini kit (Qiagen, Berlin, Germany). Genotyping was conducted by MALDI-ToF-MS as previously described (13). SNP genotyping was performed using the MassArray system (Sequenom, San Diego, CA, USA) by MALDI-ToF-MS according to the manufacturer’s instructions. Completed genotyping reactions were spotted onto a 384-well spectro-CHIP system (Sequenom) using a MassArray Nanodispenser (Sequenom) and determined by MALDI-ToF-MS. Genotype calling was performed in real time with MassArray RT software version 3.1 (Sequenom), and analyzed using MassArray Typer software version 4.0 (Sequenom) (Figs. 1 and 2). For quality control, repeated analyses were conducted for 10% of randomly selected samples.
Figure 1.

Genotyping of ADH1B rs1229984 A/G by MALDI-ToF-MS. ADH1B, alcohol dehydrogenase 1B; MALDI-ToF-MS, matrix-assisted laser desorption/ionization time-of-flight mass spectrometry.
Figure 2.
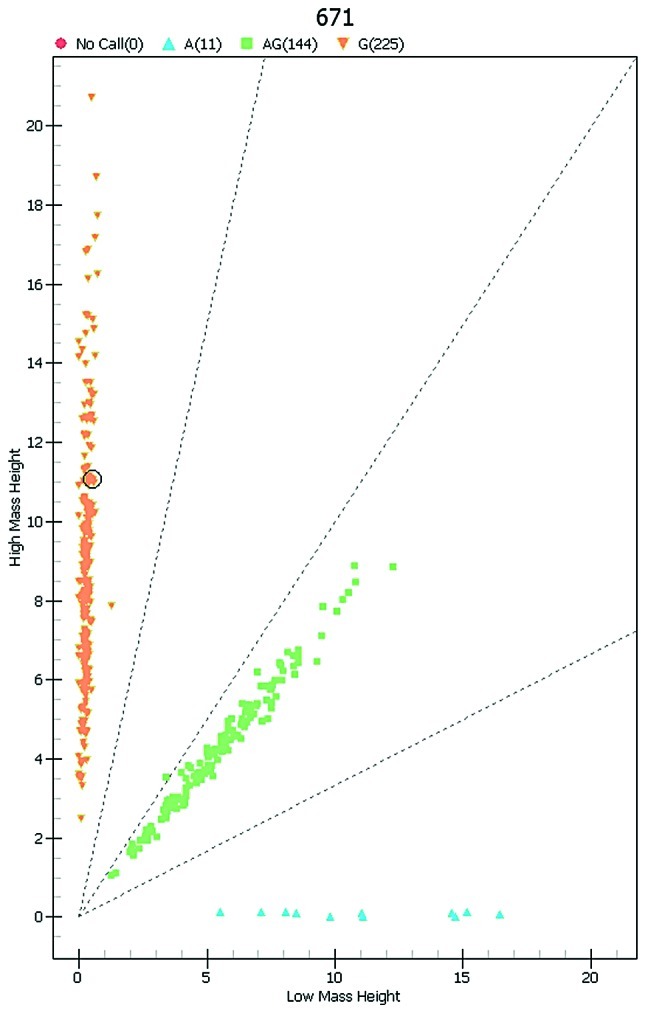
Genotyping of ALDH2 rs671 G/A by MALDI-ToF-MS. ALDH2, aldehyde dehydrogenase 2; MALDI-ToF-MS, matrix-assisted laser desorption/ionization time-of-flight mass spectrometry.
Statistical analyses
Differences in the distributions of demographic characteristics, selected variables and genotypes of ADH1B and ALDH2 variants between cases and controls were evaluated using the χ2 test. Associations between ADH1B and ALDH2 genotypes and the risk of esophageal cancer were estimated by computing the odds ratios (ORs) and their 95% confidence intervals (CIs) using logistic regression analyses for crude ORs and adjusted ORs when adjusting for age, gender, tobacco use and drinking status. The Hardy-Weinberg equilibrium was tested by a goodness-of-fit χ2 test to compare the observed genotype frequencies to the expected among the control subjects. All statistical analyses were conducted using SAS 9.1.3 software (SAS Institute, Cary, NC, USA).
Results
Characteristics of the study population
Among the 380 ESCC cases and the 380 controls with DNA samples, genotyping was successful in 379 (99.7%) cancer cases and 378 (99.5%) controls for ADH1B rs1229984. For ALDH2 rs671, genotyping was successful in 380 (100.0%) cancer cases and 378 (99.5%) controls. Characteristics of cases and controls are summarized in Table I. Cases and controls appeared to be adequately matched with respect to age and gender as suggested by the χ2 tests (p=0.056 and 0.346, respectively). No significant difference was observed with regard to drinking status between cases and controls (p=0.183). However, the prevalence of smoking was higher in the esophageal cancer patients than in the control subjects (p=0.014) (Table I).
Table I.
Distribution of selected demographic variables and risk factors in esophageal cancer cases and control subjects.
| Variable | Cases (n=380)
|
Controls (n=380)
|
p-valuea | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Age (years) | 0.056 | ||||
| <60 | 142 | 37.4 | 117 | 30.8 | |
| ≥60 | 238 | 62.6 | 263 | 69.2 | |
| Gender | 0.346 | ||||
| Male | 269 | 70.8 | 257 | 67.6 | |
| Female | 111 | 29.2 | 123 | 32.4 | |
| Tobacco use | 0.014 | ||||
| Never smoked | 220 | 57.9 | 253 | 66.6 | |
| Have smoked | 160 | 42.1 | 127 | 33.4 | |
| Alcohol use | 0.183 | ||||
| Never consumed | 253 | 66.6 | 270 | 71.1 | |
| Have consumed | 127 | 33.4 | 110 | 28.9 | |
Two-sided χ2 test.
Associations between ADH1B rs1229984 and ALDH2 rs671 polymorphisms and the risk of esophageal cancer
The genotype distributions of ADH1B and ALDH2 in the cases and controls are shown in Table II. The observed genotype frequencies for these two polymorphisms in the controls were all within Hardy-Weinberg equilibrium (p=0.102 and 0.925 for ADH1B and ALDH2, respectively). In the single-locus analyses, the genotype frequencies of ADH1B rs1229984 were 41.7% (AA), 44.3% (AG) and 14.0% (GG) in the patients, and 48.1% (AA), 45.0% (AG) and 6.9% (GG) in the control subjects. The difference was revealed to be significant (p=0.004). Logistic regression analyses revealed that subjects carrying the GG variant homozygote had a significant 2.39-fold (adjusted OR=2.39; 95% CI=1.42–4.03) increased risk of esophageal cancer. However, the genotype frequencies of ALDH2 rs671 were not significantly different between the cases and the controls (p=0.141). Logistic regression analyses revealed that the ALDH2 rs671 AA variant genotype, but not the ALDH2 rs671 GA heterozygote, was associated with a borderline-significantly decreased risk of esophageal cancer (adjusted OR=0.47, 95% CI=0.22–1.00 for rs671 AA and adjusted OR=0.99, 95% CI=0.73–1.34 for rs671 GA, respectively), compared with the rs671 GG wild-type homozygote.
Table II.
Logistic regression analyses of associations between ADH1B and ALDH2 polymorphisms and risk of esophageal cancer.
| Genotype | Casesa (n=380)
|
Controls (n=380)
|
Crude OR (95% CI) | p-value | Adjusted ORb (95% CI) | p-value | ||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | |||||
| ADH1B rs1229984 | ||||||||
| AA | 158 | 41.7 | 182 | 48.1 | 1.00 | 1.00 | ||
| AG | 168 | 44.3 | 170 | 45.0 | 1.14 (0.84–1.54) | 0.400 | 1.14 (0.84–1.54) | 0.399 |
| GG | 53 | 14.0 | 26 | 6.9 | 2.35 (1.40–3.93) | 0.001 | 2.39 (1.42–4.03) | 0.001 |
| AA+AG | 326 | 86.0 | 352 | 93.1 | 1.00 | 1.00 | ||
| GG | 53 | 14.0 | 26 | 6.9 | 2.20 (1.34–3.60) | 0.002 | 2.23 (1.36–3.68) | 0.002 |
| G allele | 36.1 | 29.4 | ||||||
| ALDH2 rs671 | ||||||||
| GG | 225 | 59.2 | 219 | 57.9 | 1.00 | 1.00 | ||
| GA | 144 | 37.9 | 137 | 36.2 | 1.02 (0.76–1.34) | 0.881 | 0.99 (0.73–1.34) | 0.956 |
| AA | 11 | 2.9 | 22 | 5.8 | 0.49 (0.23–1.03) | 0.059 | 0.47 (0.22–1.00) | 0.050 |
| GG+GA | 369 | 97.1 | 356 | 94.2 | 1.00 | 1.00 | ||
| AA | 11 | 2.9 | 22 | 5.8 | 0.48 (0.23–1.01) | 0.053 | 0.47 (0.22–1.00) | 0.048 |
| A allele | 21.8 | 23.9 | ||||||
Genotyping was successful in 379 (99.7%) cancer cases, and 378 (99.5%) controls for ADH1B rs1229984. For ALDH2 rs671, genotyping was successful in 380 (100.0%) cancer cases and 378 (99.5%) controls.
Adjusted for age, gender, smoking and drinking status. CI, confidence interval; OR, odds ratio; ADH1B, alcohol dehydrogenase 1B; ALDH2, aldehyde dehydrogenase 2. Bold type indicates statistical significance (p<0.05).
In the recessive model, the ADH1B rs1229984 GG variant homozygote was associated with a 2.20-fold significantly increased risk of esophageal cancer compared with rs1229984 AA/AG genotypes (adjusted OR=2.20, 95% CI=1.34–3.60). However, for the ALDH2 rs671 G/A polymorphism, the rs671 AA genotype was associated with a significantly decreased risk of esophageal cancer (adjusted OR=0.47, 95% CI=0.22–1.00), compared with rs671 GG/GA genotypes.
Stratification analyses of ADH1B rs1229984 and ALDH2 rs671 polymorphisms and risk of esophageal cancer
Stratification analyses were conducted to evaluate the effects of ADH1B and ALDH2 genotypes on the risk of esophageal cancer according to age, gender, smoking status and alcohol-consumption status (Table III). A significantly increased risk of esophageal cancer associated with the ADH1B rs1229984 GG genotype was evident among males (adjusted OR=2.72, 95% CI=1.50–4.95) aged <60 years (adjusted OR=2.41, 95% CI=1.29–4.48), smokers (adjusted OR=3.24, 95% CI=1.44–7.28), and consumers of alcohol (adjusted OR=3.05, 95% CI=1.35–6.90), compared with the rs1229984 AA/AG genotype. For the ALDH2 rs671 variant, the risk effects of rs671 AA vs. rs671 GG/GA were significant in males (adjusted OR=0.13, 95% CI=0.04–0.47), younger subjects (<60 years) (adjusted OR=0.24, 95% CI=0.06–0.92), and smokers (adjusted OR=0.05, 95% CI=0.01–0.38).
Table III.
Stratified analyses between ADH1B and ALDH2 polymorphisms and risk of esophageal cancer by gender, age, smoking status and alcohol consumption.
| Variable |
ADH1B rs1229984 (case/control)
|
ORa (95% CI)
|
ALDH2 rs671 (case/control)
|
ORa (95% CI)
|
||||
|---|---|---|---|---|---|---|---|---|
| AA+AG | GG | AA+AG | GG | GG+GA | AA | GG+GA | AA | |
| Gender | ||||||||
| Male | 226/238 | 43/17 | 1.00 | 2.72 (1.50–4.95) | 266/237 | 3/18 | 1.00 | 0.13 (0.04–0.47) |
| Female | 100/114 | 10/9 | 1.00 | 1.26 (0.49–3.27) | 103/119 | 8/4 | 1.00 | 2.40 (0.70–8.26) |
| Age (years) | ||||||||
| <60 | 118/109 | 24/8 | 1.00 | 2.41 (1.29–4.48) | 139/107 | 3/10 | 1.00 | 0.24 (0.06–0.92) |
| ≥60 | 208/243 | 29/18 | 1.00 | 1.87 (0.79–4.40) | 230/249 | 8/12 | 1.00 | 0.68 (0.27–1.71) |
| Smoking status | ||||||||
| Never smoked | 195/235 | 24/17 | 1.00 | 1.84 (0.95–3.56) | 210/241 | 10/12 | 1.00 | 1.05 (0.44–2.51) |
| Have smoked | 131/117 | 29/9 | 1.00 | 3.24 (1.44–7.28) | 159/115 | 1/10 | 1.00 | 0.05 (0.01–0.38) |
| Alcohol consumption | ||||||||
| Never consumed | 227/252 | 25/17 | 1.00 | 1.90 (0.99–3.65) | 242/253 | 11/16 | 1.00 | 0.67 (0.30–1.52) |
| Have consumed | 99/100 | 28/9 | 1.00 | 3.05 (1.35–6.90) | 127/103 | 0/6 | 1.00 | Not available |
Adjusted for age, gender, smoking status and alcohol consumption in a logistic regression model. CI, confidence interval; OR, odds ratio. ADH1B, alcohol dehydrogenase 1B; ALDH2, aldehyde dehydrogenase 2. Bold type indicates statistical significance.
Discussion
We investigated the associations of ADH1B and ALDH2 SNPs with risk of esophageal cancer in a high-risk Chinese population. Multivariable logistic analyses revealed that the ADH1B rs1229984 GG genotype was associated with an increased risk, and that the ALDH2 rs671 AA genotype was associated with a significantly decreased risk of esophageal cancer, and that this effect was more evident among males, younger subjects and smokers. We found a significant gene-environment interaction between exposure to smoking and ADH1B and ALDH2 SNPs for the risk of esophageal cancer. Our results suggest a potential role of ADH1B and ALDH2 SNPs on the etiology of esophageal cancer.
Two recent genome-wide association studies identified the variation of ADH1B rs1229984 and ALDH2 rs671 polymorphism as risk factors for esophageal cancer in a Japanese population (11,12). However, in another three genome-wide association studies in larger Chinese populations, the results presented negative or protective efforts of these polymorphisms for esophageal cancer risk (2,3,14). The reason for these inconsistent findings for ADH1B rs1229984 and ALDH2 rs671 polymorphisms is unknown. However, variation in enzyme activity with ethnicity and gender could contribute to differences in influences on neoplasms. The genome instability induced by ethanol- and acetaldehyde-mediated pathways could explain ADH1B and ALDH2 polymorphic effects on alcohol-induced carcinogenesis (15). In the present study, we also found a significant gene-environment interaction between ADH1B rs1229984 and ALDH2 rs671 polymorphisms and smoking habit, suggesting susceptibility to esophageal cancer.
Alcoholic beverages may have carcinogenic effects on humans and are causally related to cancer of the oral cavity, pharynx, larynx and esophagus (10). The genetic polymorphisms of alcohol-metabolizing enzymes modulate individual differences in alcohol-oxidizing capability and drinking behavior (4). Individuals with the ALDH2 GA/AA genotype should have only 6.25% of normal ALDH2 GG protein, and molecules containing one or more ALDH2 A subunits are considered to be inactive (9). How enzyme polymorphisms influence individual cancer susceptibility is a new area of research.
Distribution of the ALDH2 rs671 allele varies with ethnicity. The ALDH2 rs671 allele is prevalent in subjects in East Asia, but has not been found in Caucasians or Africans (16). However, this variant is common in Asians, with 30–40% of the population being heterozygous (ALDH2 GA) and 2.5–5% being homozygous for the null variant (ALDH2 AA) (17). The allele frequency of the ALDH2 rs671 polymorphism in our control population (36.2% for GA and 5.8% for AA) was similar to results observed in Asians. The observed genotype frequency for the ALDH2 rs671 polymorphism in the controls was within Hardy-Weinberg equilibrium (p=0.925), indicating a good representation for our control population.
A recent study found that there was no significant impact of ADH1B rs1229984 and ALDH2 rs671 polymorphisms on the risk of breast cancer. Neither was there a significant gene-environment interaction between alcohol consumption and polymorphisms in ADH1B rs1229984 and ALDH2 rs671 (18). In a recent study in a Chinese Han population, Gao et al found that rs671 A/G and A/A genotypes were protective against the risk of colorectal cancer (19). However another study by Sangrajrang et al did not find any affect of the ALDH2 rs671 polymorphism on the risk of breast cancer (20). Two studies in Asian populations found a significantly higher risk of cancer of the upper aerodigestive tract (UADT), oral cavity or oropharynx and hypopharynx in moderate or heavy drinkers of alcohol carrying the ADH1B *1/*1 (GG) genotype (21,22).
Hashibe et al identified the variation of ADH1B rs1229984 as a risk factor for esophageal cancer in European and Latin American populations (23). Their results were consistent with the results of the present study and another investigation conducted by Tanaka et al in a Japanese population (11). A recent meta-analysis conducted by Guo et al revealed that the ADH1B 47Arg (G) allele was a common genetic variant that increased the risk of cancers of the UADT, while also modulating the susceptibility to UADT cancers coupled with alcohol drinking (24). In another two meta-analyses investigating the ADH1B rs1229984 polymorphism and esophageal cancer, genetic variations of ADH1B His47Arg (A/G) were also found to be susceptible loci for esophageal cancer (25,26). The conclusions were in accordance with our results. For the ADH1B rs1229984 polymorphism, the observed genotype frequencies in the controls were also within Hardy-Weinberg equilibrium (p=0.102).
The present study has several limitations. Firstly, it was a hospital-based case-control study, therefore selection bias may be unavoidable and the subjects may not be representative of the general population. Secondly, the polymorphisms investigated were based on functional considerations, so they may not give a comprehensive view about the genetic variability in ADH1B and ALDH2. Thirdly, the present study involved a relatively small number of subjects in the subgroup analyses. This may have resulted in reduction in the magnitude of the statistical power, with an increase in the potential for random error. Therefore, larger well-designed studies are required to confirm our findings. Finally, we did not obtain detailed information on cancer metastasis and survival, which restricted further analyses on the role of ADH1B and ALDH2 polymorphisms in the progression and prognosis of esophageal cancer.
In conclusion, the present study provided marked evidence that functional polymorphism of ADH1B rs1229984 and ALDH2 rs671 may contribute to the risk of esophageal cancer. However, our results were obtained with a limited sample size and therefore only preliminary conclusions can be drawn. Validations of these findings with further larger studies and more diversely ethnic populations are required.
Acknowledgments
This study was supported in part by National Natural Science Foundation of China (81101889) and Social Development Foundation of Zhenjiang (SH2010017).
Abbreviations:
- ADH
alcohol dehydrogenase
- ALDH
aldehyde dehydrogenase
- SNP
single nucleotide polymorphism
References
- 1.Kapeller P, Barber R, Vermeulen RJ, et al. Visual rating of age-related white matter changes on magnetic resonance imaging: scale comparison, interrater agreement, and correlations with quantitative measurements. Stroke. 2003;34:441–445. doi: 10.1161/01.str.0000049766.26453.e9. [DOI] [PubMed] [Google Scholar]
- 2.Wu C, Hu Z, He Z, et al. Genome-wide association study identifies three new susceptibility loci for esophageal squamous-cell carcinoma in Chinese populations. Nat Genet. 2011;43:679–684. doi: 10.1038/ng.849. [DOI] [PubMed] [Google Scholar]
- 3.Wang LD, Zhou FY, Li XM, et al. Genome-wide association study of esophageal squamous cell carcinoma in Chinese subjects identifies susceptibility loci at PLCE1 and C20orf54. Nat Genet. 2010;42:759–763. doi: 10.1038/ng.648. [DOI] [PubMed] [Google Scholar]
- 4.Bosron WF, Li TK. Genetic polymorphism of human liver alcohol and aldehyde dehydrogenases, and their relationship to alcohol metabolism and alcoholism. Hepatology. 1986;6:502–510. doi: 10.1002/hep.1840060330. [DOI] [PubMed] [Google Scholar]
- 5.Badger TM, Ronis MJ, Seitz HK, et al. Alcohol metabolism: role in toxicity and carcinogenesis. Alcohol Clin Exp Res. 2003;27:336–347. doi: 10.1097/01.ALC.0000052583.87673.37. [DOI] [PubMed] [Google Scholar]
- 6.Kayaalti Z, Soylemezoglu T. Distribution of ADH1B, ALDH2, CYP2E1 *6, and CYP2E1 *7B genotypes in Turkish population. Alcohol. 2010;44:415–423. doi: 10.1016/j.alcohol.2010.06.002. [DOI] [PubMed] [Google Scholar]
- 7.Crabb DW, Matsumoto M, Chang D, You M. Overview of the role of alcohol dehydrogenase and aldehyde dehydrogenase and their variants in the genesis of alcohol-related pathology. Proc Nutr Soc. 2004;63:49–63. doi: 10.1079/pns2003327. [DOI] [PubMed] [Google Scholar]
- 8.Matsuo K, Hiraki A, Hirose K, et al. Impact of the alcohol-dehydrogenase (ADH) 1C and ADH1B polymorphisms on drinking behavior in nonalcoholic Japanese. Hum Mutat. 2007;28:506–510. doi: 10.1002/humu.20477. [DOI] [PubMed] [Google Scholar]
- 9.Crabb DW, Edenberg HJ, Bosron WF, Li TK. Genotypes for aldehyde dehydrogenase deficiency and alcohol sensitivity. The inactive ALDH2(2) allele is dominant. J Clin Invest. 1989;83:314–316. doi: 10.1172/JCI113875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yokoyama A, Omori T. Genetic polymorphisms of alcohol and aldehyde dehydrogenases and risk for esophageal and head and neck cancers. Jpn J Clin Oncol. 2003;33:111–121. doi: 10.1093/jjco/hyg026. [DOI] [PubMed] [Google Scholar]
- 11.Tanaka F, Yamamoto K, Suzuki S, et al. Strong interaction between the effects of alcohol consumption and smoking on oesophageal squamous cell carcinoma among individuals with ADH1B and/or ALDH2 risk alleles. Gut. 2010;59:1457–1464. doi: 10.1136/gut.2009.205724. [DOI] [PubMed] [Google Scholar]
- 12.Cui R, Kamatani Y, Takahashi A, et al. Functional variants in ADH1B and ALDH2 coupled with alcohol and smoking synergistically enhance esophageal cancer risk. Gastroenterology. 2009;137:1768–1775. doi: 10.1053/j.gastro.2009.07.070. [DOI] [PubMed] [Google Scholar]
- 13.Schaeffeler E, Zanger UM, Eichelbaum M, et al. Highly multiplexed genotyping of thiopurine s-methyltransferase variants using MALD-TOF mass spectrometry: reliable genotyping in different ethnic groups. Clin Chem. 2008;54:1637–1647. doi: 10.1373/clinchem.2008.103457. [DOI] [PubMed] [Google Scholar]
- 14.Abnet CC, Freedman ND, Hu N, et al. A shared susceptibility locus in PLCE1 at 10q23 for gastric adenocarcinoma and esophageal squamous cell carcinoma. Nat Genet. 2010;42:764–767. doi: 10.1038/ng.649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Weng H, Weng Z, Lu Y, Nakayama K, Morimoto K. Effects of alcohol-drinking behaviour and ADH1B and ALDH2 polymorphisms on basal DNA damage in human mononuclear cells as determined by the comet assay. Mutat Res. 2010;701:132–136. doi: 10.1016/j.mrgentox.2010.05.013. [DOI] [PubMed] [Google Scholar]
- 16.Goedde HW, Agarwal DP, Fritze G, et al. Distribution of ADH2 and ALDH2 genotypes in different populations. Hum Genet. 1992;88:344–346. doi: 10.1007/BF00197271. [DOI] [PubMed] [Google Scholar]
- 17.Eng MY, Luczak SE, Wall TL. ALDH2, ADH1B, and ADH1C genotypes in Asians: a literature review. Alcohol Res Health. 2007;30:22–27. [PMC free article] [PubMed] [Google Scholar]
- 18.Kawase T, Matsuo K, Hiraki A, et al. Interaction of the effects of alcohol drinking and polymorphisms in alcohol-metabolizing enzymes on the risk of female breast cancer in Japan. J Epidemiol. 2009;19:244–250. doi: 10.2188/jea.JE20081035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gao CM, Takezaki T, Wu JZ, et al. Polymorphisms of alcohol dehydrogenase 2 and aldehyde dehydrogenase 2 and colorectal cancer risk in Chinese males. World J Gastroenterol. 2008;14:5078–5083. doi: 10.3748/wjg.14.5078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sangrajrang S, Sato Y, Sakamoto H, et al. Genetic polymorphisms in folate and alcohol metabolism and breast cancer risk: a case-control study in Thai women. Breast Cancer Res Treat. 2010;123:885–893. doi: 10.1007/s10549-010-0804-4. [DOI] [PubMed] [Google Scholar]
- 21.Asakage T, Yokoyama A, Haneda T, et al. Genetic polymorphisms of alcohol and aldehyde dehydrogenases, and drinking, smoking and diet in Japanese men with oral and pharyngeal squamous cell carcinoma. Carcinogenesis. 2007;28:865–874. doi: 10.1093/carcin/bgl206. [DOI] [PubMed] [Google Scholar]
- 22.Hiraki A, Matsuo K, Wakai K, et al. Gene-gene and gene-environment interactions between alcohol drinking habit and polymorphisms in alcohol-metabolizing enzyme genes and the risk of head and neck cancer in Japan. Cancer Sci. 2007;98:1087–1091. doi: 10.1111/j.1349-7006.2007.00505.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hashibe M, McKay JD, Curado MP, et al. Multiple ADH genes are associated with upper aerodigestive cancers. Nat Genet. 2008;40:707–709. doi: 10.1038/ng.151. [DOI] [PubMed] [Google Scholar]
- 24.Guo H, Zhang G, Mai R. Alcohol dehydrogenase-1b Arg47His polymorphism and upper aerodigestive tract cancer risk: a meta-analysis including 24,252 subjects. Alcohol Clin Exp Res. 2011 Sep 6; doi: 10.1111/j.1530-0277.2011.01621.x. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 25.Smith M, Zhou M, Whitlock G, et al. Esophageal cancer and body mass index: results from a prospective study of 220,000 men in China and a meta-analysis of published studies. Int J Cancer. 2008;122:1604–1610. doi: 10.1002/ijc.23198. [DOI] [PubMed] [Google Scholar]
- 26.Zhang GH, Mai RQ, Huang B. Meta-analysis of ADH1B and ALDH2 polymorphisms and esophageal cancer risk in China. World J Gastroenterol. 2010;16:6020–6025. doi: 10.3748/wjg.v16.i47.6020. [DOI] [PMC free article] [PubMed] [Google Scholar]


