Abstract
Portal vein thrombosis (PVT) is one of the most common complications occurring during the natural course of liver cirrhosis. Even though PVT is often asymptomatic, the worsening of liver function, an unexpected episode of gastrointestinal bleeding or ascitic decompensation may be landmarks of PVT development. Beyond these clinical manifestations, it is debated whether PVT really has an impact on liver cirrhosis natural history or rather represents only one of its consequences. Probably PVT development should not only be considered as a matter of impaired blood flow or pro-coagulation tendency. On one hand, PVT seems a consequence of the worsening in portal vein outflow due to the increased hepatic resistance in cirrhotic livers. On the other hand, vascular microthrombosis secondary to necroinflammation may cause liver ischemia and infarction, with loss of hepatic tissue (parenchymal extinction) which is replaced by fibrotic tissue. Therefore, PVT might also be considered as the overt manifestation of the liver fibrosing process evolution and anticoagulant therapy may thus have microscopic indirect effects also on the progression of liver disease. At present, a connection between PVT development and the progression of liver fibrosis/cirrhosis has not yet been demonstrated. Nevertheless, it is not clear if PVT development may worsen cirrhotic patients’ outcome by itself. Some authors tried to assess liver transplant benefit in PVT cirrhotic patients but data are contrasting. In this review, we will try to answer these questions, providing a critical analysis of data reported in literature.
Keywords: Portal vein thrombosis, Liver cirrhosis, Liver fibrosis, Microthrombi, Survival
INTRODUCTION
Portal vein thrombosis (PVT) is a well-known complication occurring during the course of liver cirrhosis, frequently in the advanced stages. It has been demonstrated that the alteration of blood flow within the portal vein plays an important role in PVT development, together with inherited or acquired pro-thrombotic disorders. Over the past few years, PVT diagnosis has been constantly increasing due to the amelioration of diagnostic imaging, with partial PVT being now more easily recognizable (Figure 1).
Figure 1.
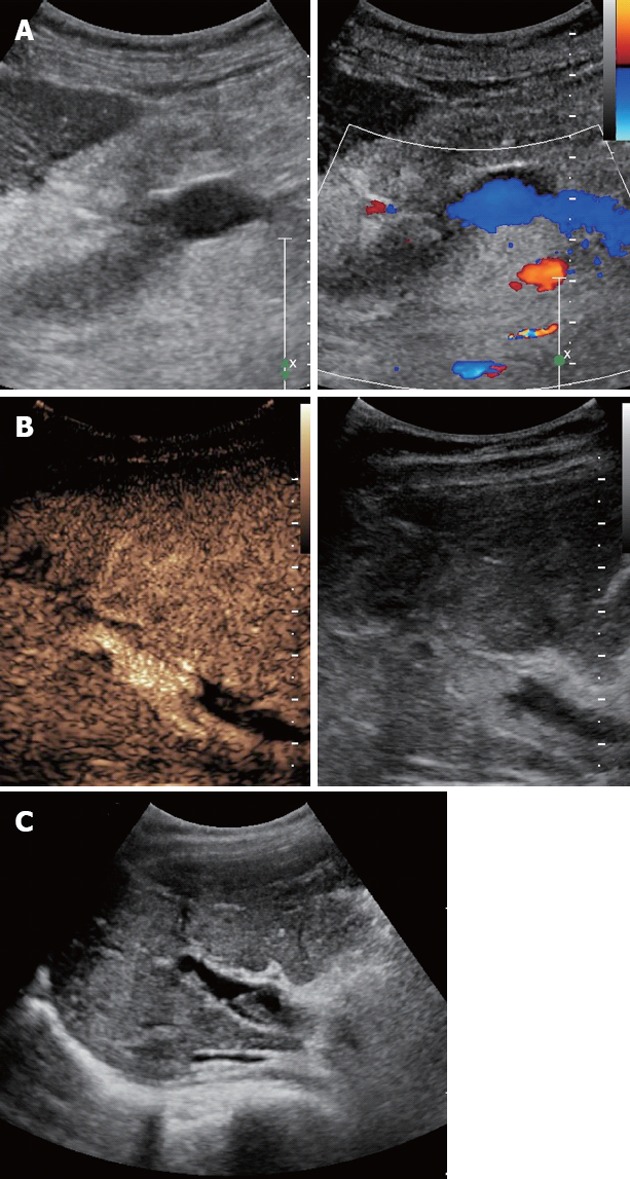
Portal vein thrombosis. A: Complete thrombosis of the portal vein trunk with patent splenic vein (B-Mode and Color Doppler imaging); B: Partial thrombosis of portal vein right branch at B-Mode and contrast-enhanced ultrasound imaging; C: Partial thrombosis of portal vein right branch at B-Mode imaging.
When PVT occurs in a cirrhotic patient, it is always considered a harmful event, because the increase of portal pressure and impaired liver vascularization may lead to gastrointestinal bleeding, worsening of liver function, and ascitic decompensation.
PVT is a matter of concern, especially regarding its treatment. Since PVT occurrence often represents a precipitating event during the course of cirrhotic disease, at the moment of the diagnosis every clinician will try to resolve the obstruction. However, it is unclear whether it could be beneficial or not to treat asymptomatic patients, and which treatment could have the best risk/benefit ratio in cirrhotics. Although anticoagulants seem to be the most used treatment in the last few years, there is at present no consensus regarding the dose and duration of treatment[1].
Some cardinal questions regarding PVT still remain unanswered: as PVT occurs often in the advanced stages of liver disease, what is the connection between PVT development and the progression of liver fibrosis/cirrhosis? Does PVT really have an impact on liver cirrhosis natural history or is PVT only one of its consequences?
In this review we will try to answer to these questions, on the basis of the evidence reported in literature. We intend to point out the question if there really is a connection between PVT development, which often occurs in the advanced stages of liver disease, and histological progression of fibrosis.
PREVALENCE AND CAUSES
Among all cases of PVT, cirrhosis is the underlying cause in 22%-28%[2,3]. Studies based on ultrasonography have reported a prevalence of 10%-25%, excluding neoplastic thrombosis[4-7]. The prevalence of PVT increases with the severity of cirrhosis, being approximately 1% in patients with compensated cirrhosis[8] and rising to 8%-25% in candidates for liver transplantation (LT)[5]; evidence for hepatic vein thrombosis was found in 70% of livers explanted at a stage of advanced cirrhosis[9]. This large variability is due to the fact that PVT is often asymptomatic, therefore its frequency may be underestimated. Indeed, in the majority of patients with cirrhosis, PVT is diagnosed as an incidental finding, often during routine ultrasound evaluation. However, when an episode of decompensation such as the development of ascites or gastrointestinal bleeding occurs, the presence of PVT should always be suspected and investigated[10,11]. At the time of evaluation for LT[12], at LT[13] or at surgical porto-systemic shunting[14], the model for end-stage liver disease (MELD) and Child-Pugh scores seems to be higher in patients with PVT than in those without.
At the origin of PVT development, there is always one or more of the following reasons, which are included in the “Virchow triad”: an impaired portal blood outflow (liver architectural changes of liver cirrhosis increase the resistances to flow), a tendency to hypercoagulability, or vascular damage, together with the development of hepatocellular carcinoma[15-17]. In cirrhotic patients, some of these factors may have a greater impact on PVT development (Table 1). Zocco et al[18] showed that portal flow velocity is the most important predictive factor for PVT development, especially when portal flow velocity is lower than 15 cm/s at Doppler ultrasound evaluation. It has been reported that when cirrhotic patients develop a hepatocellular carcinoma, PVT incidence rises to 10%-40%[19]. However, although the evidence of a pro-thrombotic condition is not frequent in cirrhotic patients, it should not be a priori excluded.
Table 1.
Risk factors most frequently involved in portal vein thrombosis. Development in cirrhotic patients, according to the Virchow triad, with the addition of vascular invasion
| Circulatory stasis | Procoagulant status | Vascular injury | Vascular invasion |
| Cirrhosis | Inherited: | Trauma | Hepatocellular carcinoma |
| Factor V Leiden mutation | Surgery (e.g., splenectomy colectomy, gastrectomy cholecystectomy | Cholangiocarcinoma | |
| Factor II (prothrombin) mutation | Liver transplantation | ||
| Protein C deficiency | Invasive procedures (TIPS placement, fine needle aspiration, radiofrequency) | ||
| Protein S deficiency antithrombin deficiency | Chemical irritation (alcoholization) | ||
| Acquired: | Infections | ||
| Myeloproliferative disorder antiphospholipid syndrome | Focal inflammatory lesions (e.g., diverticulitis, appendicitis, pancreatitis, duodenal ulcer, cholecystitis, tuberculous) | ||
| Hyperhomocysteinemia | |||
| Malignancy (any abdominal organ) | |||
| Pregnancy/puerperium | |||
| Oral contraceptives | |||
| Sepsis |
TIPS: Transjugular intrahepatic portosystemic shunt.
In a recent study including 136 consecutive cirrhotic outpatients (24.2% diagnosed with PVT), a significant increase of factor VIII and D-dimer was observed in those with advanced liver cirrhosis. High levels of factor VIII have already been reported in cirrhotic patients and it is now well known that they represent an intrinsic feature of the disease (plasmatic levels of factor VIII beyond the 66th percentile - 129 IU/dL - are reported to have a 6-fold greater risk of PVT development[20]), while the increase in D-dimer is rather considered to be a non-specific finding[21]. However, the only conclusion the author could provide was that low values of D-dimer had high sensitivity and specificity in excluding PVT[22]. Among the other inherited pro-thrombotic disorders, prothrombin gene G20210A mutation seems to be the most frequent in cirrhotics with PVT[23-27], while the role of anticardiolipin antibodies is still a matter of concern, due to a high susceptibility to infections and to the presence of liver damage[28-33]. Recently, it has also been reported the presence of the JAK2 V617F gene mutation in about 17%-35% of PVT patients without a known underlying disease[34-36]; however, even if it could be a marker of a myeloproliferative disorder before it becomes clinically evident, the prevalence among cirrhotic PVT patients is actually unknown.
PVT DEVELOPMENT AND THE PROGRESSION OF LIVER FIBROSIS/CIRRHOSIS
Is there a link between the progression of liver disease throughout the development of liver cirrhosis and portal vein thrombosis? The answer may be “yes”. Different factors appear to be involved in chronic liver injury; among them, the coagulation system appears to be particularly involved. Animal models of cirrhosis confirmed that mice carrying the factor V Leiden mutation exhibit more severe fibrosis than wild-type littermates[37,38]. In other clinical studies, factor V Leiden mutation was reported to be associated with a 3.28-fold increased risk of rapid fibrosis progression in patients with hepatitis C[39]. A similar tendency has been demonstrated in patients with protein C deficiency, increased factor VIII expression and hyperhomocysteinemia[40]. The main link between hypercoagulability and fibrosis progression is still being investigated, but it is more likely due to a reaction to liver tissue ischemic damage. It has been postulated that micro-infarcts resulting from thrombosis of the hepatic and portal vein branches may cause ischemia and cell death, with consequent parenchymal collapse manifesting with areas of parenchymal extinction[41,42]. These areas are then replaced by fibrous tissue producing cirrhosis[37]. Liver injury is able to activate the perisinusoidal hepatic stellate cells, which can transdifferentiate into myofibroblasts, showing pro-inflammatory and pro-fibrogenic activity[38,43]. A similar mechanism of intrahepatic thrombosis of portal vein branches has been recognized at the origin of nodular regenerative hyperplasia development, which could be confused with liver cirrhosis[44].
Indeed, the t-PA-plasmin system is involved in activation of transforming growth factor-beta (TGF-β), a pro-fibrogenic cytokine, which is essential in the pathogenesis of liver cirrhosis. Wanless et al[41,42] demonstrated that microthrombi are frequently present within hepatic vessels of patients with liver cirrhosis and other studies showed a correlation between inherited thrombophilic conditions and severity and progression of liver disease. Moreover, hepatitis C virus infected haemophilic patients seem to have a slower disease progression, supporting the hypothesis that a hypercoagulant state may heavily worsen the natural history of liver disease[45].
Even if the exact mechanism is still unknown, a primary role of parenchymal extinction and of stellate cells activation in triggering this process has been postulated. Indeed, vascular microthrombosis secondary to necroinflammation, may cause liver ischemia and infarction, with loss of hepatic tissue (parenchymal extinction) which is replaced by fibrotic tissue. Cirrhosis will therefore result from the confluence of these microfibrotic areas. Alternatively, thrombin may induce fibrogenesis by itself, both activating specific receptors on stellate cells, or indirectly, stimulating release of platelet-derived growth factors by platelets and promoting post-translational activation of TGF-β[37,39,40,46]. The first of these is a direct mechanism; G-protein coupled protease activated receptor (PAR)-1, PAR-3 and PAR-4 are associated to thrombin signaling[47-50]. Thrombin exerts a chemotactic effect on monocytes and a mitogenic stimulus for smooth muscle cells, fibroblasts and hepatic stellate cells[51], which express members of the PAR family via PAR-1[52-54]. Therefore both an increased generation of thrombin, due to the activation of the coagulation system, and the lack of an adequate inhibition of thrombin generation, as in patients carrying the factor V Leiden mutation or PC deficiency, may contribute to liver fibrogenesis. Elevated levels of factor VIII may also activate PAR-1 signaling[55].
The role of FXa/PAR-2 signaling in hepatic fibrosis is less well characterized, however, there is now evidence for its role in several fibrotic diseases through fibroblast activation including α-smooth muscle actin production, monocyte chemoattractant protein-1 and interleukin-6 secretion, and TGF-β expression[51]. Moreover, FXa signaling via PAR-1 remains the most important although this may vary in different tissues[56].
In conclusion, stellate cells activation and parenchymal extinction play a pivotal role in determining liver fibrosis evolution, with a recognized trigger in the coagulation system[33]. In this perspective, PVT development should not only be considered as a matter of impaired blood flow or pro-coagulation tendency, but also as the overt manifestation of the liver fibrosing process.
HOW MUCH DOES PVT IMPACT ON THE NATURAL HISTORY OF LIVER CIRRHOSIS?
Impact on complications
In the past years, cirrhotic patients developing PVT where considered at high risk of mortality for gastrointestinal bleeding, especially in case of complete occlusion. The risk of variceal bleeding is nearly 80-120 times higher in cirrhotics with PVT than in those without liver disease (19%-40%)[17,19,57]. Therefore an episode of unexpected variceal hemorrhage can be linked with a high probability to acute PVT development, as well as refractory ascites in a patient previously responsive to the diuretic treatment[58]. In addition, when the thrombus extends to the superior mesenteric vein, the risk of intestinal infarction is high[59].
PVT has been found to be an independent predictor for failure to control active variceal bleeding and prevent variceal re-bleeding, irrespective of the use of endoscopic hemostasis or surgical shunting as treatment modalities[60,61]. There are some doubts about a supposed favoring role of the endoscopic therapy of esophageal varices in PVT development; probably, varices represent by themselves a marker of portal hypertension, which might be a risk factor for PVT independently of the procedure[59].
Recent data highlight that the prevention of PVT development is a useful tool to avoid the occurrence of decompensation in cirrhotic patients. Zecchini et al[62] randomized 51 cirrhotics with advanced liver disease (Child B7-C10) to receive enoxaparin 4000 IU/d (26 patients) or placebo (25 patients) for 12 mo; PVT occurred in 5 patients in the placebo group (2 complete, 3 partial) and in none in the treatment group. Treated patients experienced fewer episodes of decompensation.
Impact on survival
The natural history of cirrhosis in patients with PVT is largely unknown. In the past, patients with PVT were considered to be at increased risk of mortality related to bleeding complications, but the improvement in gastrointestinal bleeding management has changed this perspective[23].
Ferreira et al[63] reported data about prognosis of non-tumoral PVT in 40 consecutive cirrhotic patents (median follow-up 6.5 mo). Fifty-eight percent of patients survived at the end of follow-up and PVT was associated with increased risk of mortality at 3 years (but not at 1 year) compared to controls, and this effect was evident only in patients with Child Pugh score lower than 10 (Child Pugh A and B patients).
Englesbe et al[64] recently performed a retrospective study to evaluate the survival of cirrhotic PVT patients including a small sample of 148 cirrhotic patients presenting with occlusive PVT followed-up at the University of Michigan during a large period (1995-2007). In this study, which has the limitation of retrospective studies, only patients undergoing pre-transplant screening were included, and there was no certain data regarding the presence of pro-thrombotic disorders, administration of anticoagulants and thrombosis grading. The authors reported 54.7% of deaths in patients with PVT versus 37.2% in patients without PVT. Interestingly, from the time of the initial evaluation, PVT patients had a risk of mortality similar to that of patients with a MELD score of 26, even if their MELD score at the time of LT evaluation was of 12. This risk increased over the time, reaching that of patients who presented for listing with a MELD score of 31. PVT was also showed to influence short-term survival after LT too. Differently from other previous studies, this by Englesbe et al[64] took into account MELD score.
On this basis, Englesbe et al[64] postulated that, if patients with PVT have significantly worse waiting list survival and an increased mortality, they should consequently have an augmented access to LT. However, the most used allocation system, based on the classification of waiting list patients according to the MELD score, may not represent the real priority of PVT patients as well, since they could maintain a good liver function for long times. Moreover, the assignation of MELD extra points, such as in case of hepatocellular carcinoma, has not yet been introduced in PVT patients. Therefore, Englesbe et al[64] tried to assess the real LT benefit for patients with PVT analyzing data on adult liver transplant candidates wait-listed between September 2001 and December 2007 from the Scientific Registry of Transplant Recipients. Candidates with PVT had similar survival rates on the waiting list compared to those without PVT, but they had a significantly inferior post-LT survival. Therefore, even if a low MELD score may reflect better clinical conditions for liver candidates, with obvious benefits in terms of peri- and post-LT outcomes, especially in presence of PVT that seems by itself to complicate the LT procedure, it seems disadvantageous to allow an early access to LT for cirrhotic patients with PVT. Specifically, the threshold for transplant benefit among patients without PVT was MELD score > 11 compared to MELD score > 13 for patients with PVT. The authors concluded that clinicians should carefully consider the risks of LT in clinically stable patients with PVT. Another recent interesting but small study confirmed this evidence[65]. In this study PVT was related to a decreased post-LT survival only in patients with a low MELD score, while no difference in outcome between PVT and non-PVT patients were found for MELD scores > 15. Notably, there was no difference in PVT extension between the groups with high and low MELD scores. Indeed, the impact of PVT on patients’ survival seems to be dependent by its extension; Doenecke et al[65] reported 90% 1 year post-LT survival for PVT grade 1/2 patients, compared to 57% for PVT grade 3/4. Except for a slightly higher transfusion requirement for PVT patients, intraoperative parameters as well as the duration of in-hospital stay and the incidence of post-operative liver dysfunction or failure did not differ significantly between high and low MELD PVT groups. In the study by Englesbe et al[12] the presence of occlusive PVT at the time of LT was associated with an increased 30 d risk of mortality. Therefore, the increased risk of post-LT mortality in PVT patients seems not only a matter of MELD score[65].
Taking together all these considerations, the outcome of PVT patients undergoing LT still seems to be controversial, almost similar to that of non-PVT patients or rather worse. Even if some authors conclude that no increased risk of mortality was observed for PVT patients while on waiting list and that there was no transplant benefit with an early LT, these considerations should be more cautious. Certainly, PVT grading could be a useful tool to identify those patients with a higher risk of mortality or complications. The observation that PVT patients are not at increased risk of mortality may be a too hazardous generalization of a more complex problem, and the prioritization of these patients should be evaluated on a single case basis.
CONCLUSION
Interesting perspectives may be opened by the connection between hypercoagulation, intrahepatic microthrombosis and progression of liver fibrosis. In particular, stellate cell activation and parenchymal extinction seem to play together a pivotal role in determining liver fibrosis evolution, with a recognized trigger in the coagulation system[33]. From this point of view, PVT development should not only be considered as a matter of impaired blood flow or pro-coagulation tendency, but also as the overt manifestation of liver fibrosing process evolution. Moreover, fibrogenesis itself could be controlled by targeting thrombin generation or its downstream signaling. It has been shown that administration of PAR-1 antagonist, thrombin inhibitor SSR182289, dipyridamole, rivaroxaban (a FXa inhibitor), vitamin K or low molecular weight heparin was able to reduce hepatic fibrosis in animal models[41,52,66-69]. Unfortunately, to date, data about the use of anticoagulants as anti-fibrotic therapy are scarce in humans but they are subject of many ongoing clinical trials.
As regards the second question of this review we can conclude that PVT represents an important event in the natural history of liver cirrhosis. We agree with Tripodi et al[55] that liver cirrhosis, slowing-down the physiologic flow of blood in the portal venous system, might favor PVT development but also that PVT development might have an impact on liver function by decreasing portal perfusion. This looping interaction confirms the strict connection between PVT and liver disease. First, PVT could not be merely considered as a problem to solve but, rather, as the alarm-bell that liver disease is evolving. In this perspective PVT prevention could be very important in order to control disease evolution and reduce episodes of decompensation as demonstrated by a recent study by Zecchini et al[62].
Second, the impact of PVT development on liver disease progression opens a new debate on the assignation of MELD extra points, such as in the case of hepatocellular carcinoma, in PVT patients on a waiting list for liver transplantation. This point of view is supported by the evidence that PVT cirrhotic patients have a high mortality risk compared to non-PVT ones from the time of evaluation for LT, which could be comparable to that of a MELD score as high as 26-31[64]. On the other hand, it seems that transplant benefit and the post-LT survival of PVT patients might not be advantageous in those with a low risk of liver disease-related mortality (low MELD scores)[12]. In our opinion, this problem should be seen from another perspective; the severity of liver disease may have a heavy impact on patients’ survival despite the presence of PVT, which, in turn, should not represent a good reason to prioritize all patients on waiting list, especially those with a low MELD score. However, the presence of major complications, such as chronic hepatic encephalopathy, refractory ascites, recurrent variceal bleeding, with either major or minor bleeding episodes with scarce response to the endoscopic or medical therapy, could represent reasons for the prioritization on waiting list for patients with PVT. Probably, PVT extension should also be considered since it has been reported to impact on post-LT survival[65]. Even if we are far away from the solution of this debate, we would like to remark that in those countries (e.g., Italy, United States) where the access to LT is determined by the risk of mortality on the waiting list, it is essential to determine how PVT could increase the risk of mortality of cirrhotics awaiting for LT. In this age characterized by organ shortage, liver graft loss should be avoided, thus maximizing the benefit of LT.
Footnotes
Peer reviewers: Erwin Biecker, MD, PhD, Department of Gastroenterology and Hepatology, Helios Klinikum Siegburg, 53343 Siegburg, Germany; Marco Senzolo, MD, PhD, Gastroenterology Unit, Department of Surgical and Gastroenterological Sciences, University-Hospital of Padua, Via Giustiniani 2, 35136 Padua, Italy
S- Editor Lv S L- Editor O’Neill M E- Editor Li JY
References
- 1.Ponziani FR, Zocco MA, Tortora A, Gasbarrini A. Is there a role for anticoagulants in portal vein thrombosis management in cirrhotic patients? Expert Opin Pharmacother. 2010;11:1479–1487. doi: 10.1517/14656561003749264. [DOI] [PubMed] [Google Scholar]
- 2.Janssen HL, Wijnhoud A, Haagsma EB, van Uum SH, van Nieuwkerk CM, Adang RP, Chamuleau RA, van Hattum J, Vleggaar FP, Hansen BE, et al. Extrahepatic portal vein thrombosis: aetiology and determinants of survival. Gut. 2001;49:720–724. doi: 10.1136/gut.49.5.720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ogren M, Bergqvist D, Björck M, Acosta S, Eriksson H, Sternby NH. Portal vein thrombosis: prevalence, patient characteristics and lifetime risk: a population study based on 23,796 consecutive autopsies. World J Gastroenterol. 2006;12:2115–2119. doi: 10.3748/wjg.v12.i13.2115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Amitrano L, Brancaccio V, Guardascione MA, Margaglione M, Iannaccone L, D’Andrea G, Marmo R, Ames PR, Balzano A. Inherited coagulation disorders in cirrhotic patients with portal vein thrombosis. Hepatology. 2000;31:345–348. doi: 10.1002/hep.510310213. [DOI] [PubMed] [Google Scholar]
- 5.Francoz C, Belghiti J, Vilgrain V, Sommacale D, Paradis V, Condat B, Denninger MH, Sauvanet A, Valla D, Durand F. Splanchnic vein thrombosis in candidates for liver transplantation: usefulness of screening and anticoagulation. Gut. 2005;54:691–697. doi: 10.1136/gut.2004.042796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fimognari FL, De Santis A, Piccheri C, Moscatelli R, Gigliotti F, Vestri A, Attili A, Violi F. Evaluation of D-dimer and factor VIII in cirrhotic patients with asymptomatic portal venous thrombosis. J Lab Clin Med. 2005;146:238–243. doi: 10.1016/j.lab.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 7.Gaiani S, Bolondi L, Li Bassi S, Zironi G, Siringo S, Barbara L. Prevalence of spontaneous hepatofugal portal flow in liver cirrhosis. Clinical and endoscopic correlation in 228 patients. Gastroenterology. 1991;100:160–167. doi: 10.1016/0016-5085(91)90596-d. [DOI] [PubMed] [Google Scholar]
- 8.Okuda K, Ohnishi K, Kimura K, Matsutani S, Sumida M, Goto N, Musha H, Takashi M, Suzuki N, Shinagawa T. Incidence of portal vein thrombosis in liver cirrhosis. An angiographic study in 708 patients. Gastroenterology. 1985;89:279–286. doi: 10.1016/0016-5085(85)90327-0. [DOI] [PubMed] [Google Scholar]
- 9.Primignani M. Portal vein thrombosis, revisited. Dig Liver Dis. 2010;42:163–170. doi: 10.1016/j.dld.2009.08.003. [DOI] [PubMed] [Google Scholar]
- 10.De Gaetano AM, Lafortune M, Patriquin H, De Franco A, Aubin B, Paradis K. Cavernous transformation of the portal vein: patterns of intrahepatic and splanchnic collateral circulation detected with Doppler sonography. AJR Am J Roentgenol. 1995;165:1151–1155. doi: 10.2214/ajr.165.5.7572494. [DOI] [PubMed] [Google Scholar]
- 11.Bayraktar Y, Harmanci O. Etiology and consequences of thrombosis in abdominal vessels. World J Gastroenterol. 2006;12:1165–1174. doi: 10.3748/wjg.v12.i8.1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Englesbe MJ, Kubus J, Muhammad W, Sonnenday CJ, Welling T, Punch JD, Lynch RJ, Marrero JA, Pelletier SJ. Portal vein thrombosis and survival in patients with cirrhosis. Liver Transpl. 2010;16:83–90. doi: 10.1002/lt.21941. [DOI] [PubMed] [Google Scholar]
- 13.Yerdel MA, Gunson B, Mirza D, Karayalçin K, Olliff S, Buckels J, Mayer D, McMaster P, Pirenne J. Portal vein thrombosis in adults undergoing liver transplantation: risk factors, screening, management, and outcome. Transplantation. 2000;69:1873–1881. doi: 10.1097/00007890-200005150-00023. [DOI] [PubMed] [Google Scholar]
- 14.Orloff MJ, Orloff MS, Orloff SL, Girard B. Portal vein thrombosis in cirrhosis with variceal hemorrhage. J Gastrointest Surg. 1997;1:123–130, discussion 130-131. doi: 10.1016/s1091-255x(97)80099-6. [DOI] [PubMed] [Google Scholar]
- 15.Lebrec D, Bataille C, Bercoff E, Valla D. Hemodynamic changes in patients with portal venous obstruction. Hepatology. 1983;3:550–553. doi: 10.1002/hep.1840030412. [DOI] [PubMed] [Google Scholar]
- 16.Ohnishi K, Okuda K, Ohtsuki T, Nakayama T, Hiyama Y, Iwama S, Goto N, Nakajima Y, Musha N, Nakashima T. Formation of hilar collaterals or cavernous transformation after portal vein obstruction by hepatocellular carcinoma. Observations in ten patients. Gastroenterology. 1984;87:1150–1153. [PubMed] [Google Scholar]
- 17.Ponziani FR, Zocco MA, Campanale C, Rinninella E, Tortora A, Di Maurizio L, Bombardieri G, De Cristofaro R, De Gaetano AM, Landolfi R, et al. Portal vein thrombosis: insight into physiopathology, diagnosis, and treatment. World J Gastroenterol. 2010;16:143–155. doi: 10.3748/wjg.v16.i2.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zocco MA, Di Stasio E, De Cristofaro R, Novi M, Ainora ME, Ponziani F, Riccardi L, Lancellotti S, Santoliquido A, Flore R, et al. Thrombotic risk factors in patients with liver cirrhosis: correlation with MELD scoring system and portal vein thrombosis development. J Hepatol. 2009;51:682–689. doi: 10.1016/j.jhep.2009.03.013. [DOI] [PubMed] [Google Scholar]
- 19.Hoekstra J, Janssen HL. Vascular liver disorders (II): portal vein thrombosis. Neth J Med. 2009;67:46–53. [PubMed] [Google Scholar]
- 20.Martinelli I, Primignani M, Aghemo A, Reati R, Bucciarelli P, Fabris F, Battaglioli T, Dell’Era A, Mannucci PM. High levels of factor VIII and risk of extra-hepatic portal vein obstruction. J Hepatol. 2009;50:916–922. doi: 10.1016/j.jhep.2008.12.020. [DOI] [PubMed] [Google Scholar]
- 21.Violi F, Ferro D, Saliola M, Quintarelli C, Alessandri C. Evaluation of D-dimer in patients with liver cirrhosis. Thromb Haemost. 1989;62:1149–1150. [PubMed] [Google Scholar]
- 22.Xu Z, Westrick RJ, Shen YC, Eitzman DT. Pulmonary fibrosis is increased in mice carrying the factor V Leiden mutation following bleomycin injury. Thromb Haemost. 2001;85:441–444. [PubMed] [Google Scholar]
- 23.Amitrano L, Guardascione MA, Brancaccio V, Margaglione M, Manguso F, Iannaccone L, Grandone E, Balzano A. Risk factors and clinical presentation of portal vein thrombosis in patients with liver cirrhosis. J Hepatol. 2004;40:736–741. doi: 10.1016/j.jhep.2004.01.001. [DOI] [PubMed] [Google Scholar]
- 24.Amitrano L, Brancaccio V, Guardascione MA, Margaglione M, Sacco M, Martino R, De Nucci C, Mosca S, Iannaccone L, Ames PR, et al. Portal vein thrombosis after variceal endoscopic sclerotherapy in cirrhotic patients: role of genetic thrombophilia. Endoscopy. 2002;34:535–538. doi: 10.1055/s-2002-33210. [DOI] [PubMed] [Google Scholar]
- 25.Erkan O, Bozdayi AM, Disibeyaz S, Oguz D, Ozcan M, Bahar K, Karayalcin S, Ozden A, Bozkaya H, Yurdaydin C, et al. Thrombophilic gene mutations in cirrhotic patients with portal vein thrombosis. Eur J Gastroenterol Hepatol. 2005;17:339–343. doi: 10.1097/00042737-200503000-00013. [DOI] [PubMed] [Google Scholar]
- 26.Walker AP. Portal vein thrombosis: what is the role of genetics? Eur J Gastroenterol Hepatol. 2005;17:705–707. doi: 10.1097/01.meg.0000170927.60979.1d. [DOI] [PubMed] [Google Scholar]
- 27.Kocher G, Himmelmann A. Portal vein thrombosis (PVT): a study of 20 non-cirrhotic cases. Swiss Med Wkly. 2005;135:372–376. doi: 10.4414/smw.2005.11035. [DOI] [PubMed] [Google Scholar]
- 28.Rosendaal FR. Venous thrombosis: a multicausal disease. Lancet. 1999;353:1167–1173. doi: 10.1016/s0140-6736(98)10266-0. [DOI] [PubMed] [Google Scholar]
- 29.Mangia A, Margaglione M, Cascavilla I, Gentile R, Cappucci G, Facciorusso D, Grandone E, Di Minno G, Rizzetto M, Andriulli A. Anticardiolipin antibodies in patients with liver disease. Am J Gastroenterol. 1999;94:2983–2987. doi: 10.1111/j.1572-0241.1999.01447.x. [DOI] [PubMed] [Google Scholar]
- 30.Wahl DG, Guillemin F, de Maistre E, Perret-Guillaume C, Lecompte T, Thibaut G. Meta-analysis of the risk of venous thrombosis in individuals with antiphospholipid antibodies without underlying autoimmune disease or previous thrombosis. Lupus. 1998;7:15–22. doi: 10.1191/096120398678919688. [DOI] [PubMed] [Google Scholar]
- 31.Liappis AP, Roberts AD, Schwartz AM, Simon GL. Thrombosis and infection: a case of transient anti-cardiolipin antibody associated with pylephlebitis. Am J Med Sci. 2003;325:365–368. doi: 10.1097/00000441-200306000-00008. [DOI] [PubMed] [Google Scholar]
- 32.Gervais A, Czernichow B, Grunebaum L, Wiesel ML, Auperin A, Rivalland D, Gabanyi J, Goldstein L, Cazenave JP, Doffoël M. [Serum cardiolipin antibodies in patients with alcoholic cirrhosis] Gastroenterol Clin Biol. 1996;20:736–742. [PubMed] [Google Scholar]
- 33.Ponziani FR, De Stefano V, Gasbarrini A. Viral cirrhosis: an overview of haemostatic alterations and clinical consequences. Mediterr J Hematol Infect Dis. 2009;1:e2009033. doi: 10.4084/MJHID.2009.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Colaizzo D, Amitrano L, Tiscia GL, Scenna G, Grandone E, Guardascione MA, Brancaccio V, Margaglione M. The JAK2 V617F mutation frequently occurs in patients with portal and mesenteric venous thrombosis. J Thromb Haemost. 2007;5:55–61. doi: 10.1111/j.1538-7836.2006.02277.x. [DOI] [PubMed] [Google Scholar]
- 35.Primignani M, Barosi G, Bergamaschi G, Gianelli U, Fabris F, Reati R, Dell’Era A, Bucciarelli P, Mannucci PM. Role of the JAK2 mutation in the diagnosis of chronic myeloproliferative disorders in splanchnic vein thrombosis. Hepatology. 2006;44:1528–1534. doi: 10.1002/hep.21435. [DOI] [PubMed] [Google Scholar]
- 36.De Stefano V, Fiorini A, Rossi E, Za T, Farina G, Chiusolo P, Sica S, Leone G. Incidence of the JAK2 V617F mutation among patients with splanchnic or cerebral venous thrombosis and without overt chronic myeloproliferative disorders. J Thromb Haemost. 2007;5:708–714. doi: 10.1111/j.1538-7836.2007.02424.x. [DOI] [PubMed] [Google Scholar]
- 37.Anstee QM, Goldin RD, Wright M, Martinelli A, Cox R, Thursz MR. Coagulation status modulates murine hepatic fibrogenesis: implications for the development of novel therapies. J Thromb Haemost. 2008;6:1336–1343. doi: 10.1111/j.1538-7836.2008.03015.x. [DOI] [PubMed] [Google Scholar]
- 38.Mann J, Mann DA. Transcriptional regulation of hepatic stellate cells. Adv Drug Deliv Rev. 2009;61:497–512. doi: 10.1016/j.addr.2009.03.011. [DOI] [PubMed] [Google Scholar]
- 39.Wright M, Goldin R, Hellier S, Knapp S, Frodsham A, Hennig B, Hill A, Apple R, Cheng S, Thomas H, et al. Factor V Leiden polymorphism and the rate of fibrosis development in chronic hepatitis C virus infection. Gut. 2003;52:1206–1210. doi: 10.1136/gut.52.8.1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Poujol-Robert A, Rosmorduc O, Serfaty L, Coulet F, Poupon R, Robert A. Genetic and acquired thrombotic factors in chronic hepatitis C. Am J Gastroenterol. 2004;99:527–531. doi: 10.1111/j.1572-0241.2004.04092.x. [DOI] [PubMed] [Google Scholar]
- 41.Wanless IR, Liu JJ, Butany J. Role of thrombosis in the pathogenesis of congestive hepatic fibrosis (cardiac cirrhosis) Hepatology. 1995;21:1232–1237. [PubMed] [Google Scholar]
- 42.Wanless IR, Wong F, Blendis LM, Greig P, Heathcote EJ, Levy G. Hepatic and portal vein thrombosis in cirrhosis: possible role in development of parenchymal extinction and portal hypertension. Hepatology. 1995;21:1238–1247. [PubMed] [Google Scholar]
- 43.Mann DA, Marra F. Fibrogenic signalling in hepatic stellate cells. J Hepatol. 2010;52:949–950. doi: 10.1016/j.jhep.2010.02.005. [DOI] [PubMed] [Google Scholar]
- 44.Hartleb M, Gutkowski K, Milkiewicz P. Nodular regenerative hyperplasia: evolving concepts on underdiagnosed cause of portal hypertension. World J Gastroenterol. 2011;17:1400–1409. doi: 10.3748/wjg.v17.i11.1400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yee TT, Griffioen A, Sabin CA, Dusheiko G, Lee CA. The natural history of HCV in a cohort of haemophilic patients infected between 1961 and 1985. Gut. 2000;47:845–851. doi: 10.1136/gut.47.6.845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Poujol-Robert A, Boëlle PY, Poupon R, Robert A. Factor V Leiden as a risk factor for cirrhosis in chronic hepatitis C. Hepatology. 2004;39:1174–1175. doi: 10.1002/hep.20166. [DOI] [PubMed] [Google Scholar]
- 47.Di Cera E. Thrombin interactions. Chest. 2003;124:11S–17S. doi: 10.1378/chest.124.3_suppl.11s. [DOI] [PubMed] [Google Scholar]
- 48.Borensztajn K, Stiekema J, Nijmeijer S, Reitsma PH, Peppelenbosch MP, Spek CA. Factor Xa stimulates proinflammatory and profibrotic responses in fibroblasts via protease-activated receptor-2 activation. Am J Pathol. 2008;172:309–320. doi: 10.2353/ajpath.2008.070347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Riewald M, Kravchenko VV, Petrovan RJ, O’Brien PJ, Brass LF, Ulevitch RJ, Ruf W. Gene induction by coagulation factor Xa is mediated by activation of protease-activated receptor 1. Blood. 2001;97:3109–3116. doi: 10.1182/blood.v97.10.3109. [DOI] [PubMed] [Google Scholar]
- 50.Riewald M, Ruf W. Mechanistic coupling of protease signaling and initiation of coagulation by tissue factor. Proc Natl Acad Sci USA. 2001;98:7742–7747. doi: 10.1073/pnas.141126698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jenkins RG, Su X, Su G, Scotton CJ, Camerer E, Laurent GJ, Davis GE, Chambers RC, Matthay MA, Sheppard D. Ligation of protease-activated receptor 1 enhances alpha(v)beta6 integrin-dependent TGF-beta activation and promotes acute lung injury. J Clin Invest. 2006;116:1606–1614. doi: 10.1172/JCI27183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fiorucci S, Antonelli E, Distrutti E, Severino B, Fiorentina R, Baldoni M, Caliendo G, Santagada V, Morelli A, Cirino G. PAR1 antagonism protects against experimental liver fibrosis. Role of proteinase receptors in stellate cell activation. Hepatology. 2004;39:365–375. doi: 10.1002/hep.20054. [DOI] [PubMed] [Google Scholar]
- 53.Marra F, DeFranco R, Grappone C, Milani S, Pinzani M, Pellegrini G, Laffi G, Gentilini P. Expression of the thrombin receptor in human liver: up-regulation during acute and chronic injury. Hepatology. 1998;27:462–471. doi: 10.1002/hep.510270221. [DOI] [PubMed] [Google Scholar]
- 54.Gaça MD, Zhou X, Benyon RC. Regulation of hepatic stellate cell proliferation and collagen synthesis by proteinase-activated receptors. J Hepatol. 2002;36:362–369. doi: 10.1016/s0168-8278(01)00285-9. [DOI] [PubMed] [Google Scholar]
- 55.Tripodi A, Anstee QM, Sogaard KK, Primignani M, Valla DC. Hypercoagulability in cirrhosis: causes and consequences. J Thromb Haemost. 2011;9:1713–1723. doi: 10.1111/j.1538-7836.2011.04429.x. [DOI] [PubMed] [Google Scholar]
- 56.Scotton CJ, Krupiczojc MA, Königshoff M, Mercer PF, Lee YC, Kaminski N, Morser J, Post JM, Maher TM, Nicholson AG, et al. Increased local expression of coagulation factor X contributes to the fibrotic response in human and murine lung injury. J Clin Invest. 2009;119:2550–2563. doi: 10.1172/JCI33288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sogaard KK, Astrup LB, Vilstrup H, Gronbaek H. Portal vein thrombosis; risk factors, clinical presentation and treatment. BMC Gastroenterol. 2007;7:34. doi: 10.1186/1471-230X-7-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gabr MA, Bessa SS, El-Zamarani EA. Portal vein thrombosis in Egyptian patients with liver cirrhosis: Role of methylenetetrahydrofolate reductase C677T gene mutation. Hepatol Res. 2010;40:486–493. doi: 10.1111/j.1872-034X.2010.00628.x. [DOI] [PubMed] [Google Scholar]
- 59.DeLeve LD, Valla DC, Garcia-Tsao G. Vascular disorders of the liver. Hepatology. 2009;49:1729–1764. doi: 10.1002/hep.22772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sarfeh IJ. Portal vein thrombosis associated with cirrhosis: clinical importance. Arch Surg. 1979;114:902–905. doi: 10.1001/archsurg.1979.01370320034006. [DOI] [PubMed] [Google Scholar]
- 61.D'Amico G, De Franchis R. Upper digestive bleeding in cirrhosis. Post-therapeutic outcome and prognostic indicators. Hepatology. 2003;38:599–612. doi: 10.1053/jhep.2003.50385. [DOI] [PubMed] [Google Scholar]
- 62.Zecchini RFA, Bernabucci V, Lei B, Vukotic R, De Maria N, Schepis F, Marietta M, Fornaciari G, Schianchi S, Villa E. Anticoagulant therapy is safe and effective n preventing portal vein thrombosis (PVT) in advanced cirrhotic patients: a prospective randomized controlled study. J Hepatol. 2010;52:S460. [Google Scholar]
- 63.Ferreira CNRT, Alexandrino P, Ramalho F, Velosa JF. Portal vein thrombosis in cirrhotic patients is associated with advanced liver disease and predicts poor long term prognosis. Hepatology. 2010;52:1072A. [Google Scholar]
- 64.Englesbe MJ, Schaubel DE, Cai S, Guidinger MK, Merion RM. Portal vein thrombosis and liver transplant survival benefit. Liver Transpl. 2010;16:999–1005. doi: 10.1002/lt.22105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Doenecke A, Tsui TY, Zuelke C, Scherer MN, Schnitzbauer AA, Schlitt HJ, Obed A. Pre-existent portal vein thrombosis in liver transplantation: influence of pre-operative disease severity. Clin Transplant. 2010;24:48–55. doi: 10.1111/j.1399-0012.2009.00977.x. [DOI] [PubMed] [Google Scholar]
- 66.Abdel-Salam OM, Baiuomy AR, Ameen A, Hassan NS. A study of unfractionated and low molecular weight heparins in a model of cholestatic liver injury in the rat. Pharmacol Res. 2005;51:59–67. doi: 10.1016/j.phrs.2004.04.009. [DOI] [PubMed] [Google Scholar]
- 67.Abe W, Ikejima K, Lang T, Okumura K, Enomoto N, Kitamura T, Takei Y, Sato N. Low molecular weight heparin prevents hepatic fibrogenesis caused by carbon tetrachloride in the rat. J Hepatol. 2007;46:286–294. doi: 10.1016/j.jhep.2006.08.023. [DOI] [PubMed] [Google Scholar]
- 68.Duplantier JG, Dubuisson L, Senant N, Freyburger G, Laurendeau I, Herbert JM, Desmoulière A, Rosenbaum J. A role for thrombin in liver fibrosis. Gut. 2004;53:1682–1687. doi: 10.1136/gut.2003.032136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wanless IR, Belgiorno J, Huet PM. Hepatic sinusoidal fibrosis induced by cholesterol and stilbestrol in the rabbit: 1. Morphology and inhibition of fibrogenesis by dipyridamole. Hepatology. 1996;24:855–864. doi: 10.1002/hep.510240417. [DOI] [PubMed] [Google Scholar]


