Abstract
AIM: To investigate the symptom presentation and quality of life in obese Chinese patients with gastroesophageal reflux disease (GERD).
METHODS: Data from patients diagnosed with GERD according to the Montreal definition, were collected between January 2009 to March 2010. The enrolled patients were assigned to the normal [body mass index (BMI) < 25 kg/m2], overweight (25-30 kg/m2), and obese (BMI > 30 kg/m2) groups. General demographic data, endoscopic findings, and quality of life of the three groups of patients were analyzed and compared.
RESULTS: Among the 173 enrolled patients, 102, 56 and 15 patients were classified in the normal, overweight, and obese, respectively. There was significantly more erosive esophagitis (73.3% vs 64.3% vs 39.2%, P = 0.002), hiatal hernia (60% vs 33.9% vs 16.7%, P = 0.001), and males (73.3% vs 73.2% vs 32.4%, P = 0.001) in the obese cases. The severity and frequency of heartburn, not acid regurgitation, was positively correlated with BMI, with a significant association in men, but not in women. Obese patients were prone to have low quality of life scores, with obese women having the lowest scores for mental health.
CONCLUSION: In patients with GERD, obese men had the most severe endoscopic and clinical presentation. Obese women had the poorest mental health.
Keywords: Gastroesophageal reflux disease, Gender, Heartburn, Life’s quality, Obesity
INTRODUCTION
Gastroesophageal reflux disease (GERD) is a chronic disease that tends to relapse and develop complications. According to previous studies, the risk factors in patients with GERD include age[1,2], obesity[3,4], hiatal hernia[5,6], and an unfavorable lifestyle, such as alcohol drinking and cigarette smoking. Obesity, defined by a body mass index (BMI) over 30 kg/m2, constitutes a public health problem in most industrialized countries, and impairs health-related quality of life[7]. At present, there are few studies on the assessment of quality of life on obese patients with GERD. There might exist a difference in the presentation of symptoms and quality of life between obese and normal weight patients. The aim of the study was to investigate symptom presentation and quality of life in GERD patients with normal or high BMI among a Chinese population in Taiwan.
MATERIALS AND METHODS
Data from consecutive adult patients, older than 18 years, in our hospital, diagnosed with GERD according to the Montreal definition, were collected from January 2009 to March 2010. The Montreal definition of GERD is a condition which develops when the reflux of stomach contents causes troublesome symptoms and/or complications[8]. Exclusion criteria were as follows: (1) GERD combined with other structural gastrointestinal disorders, such as peptic ulcer disease, esophageal or gastric malignancy; (2) prior gastric and esophageal surgery; (3) use of chronic antacid medication, such as proton pump inhibitors or H2-receptor antagonists, for more than 2 mo prior to enrollment; and (4) pregnancy. This study was conducted with the approval of the Clinical Research Ethics Committee of Taichung Veterans General Hospital.
General data of enrolled patients, including age, gender, BMI, and symptom duration, were recorded. All patients underwent an open-access transoral upper gastrointestinal endoscopy, and details of esophagocardiac mucosal break or hiatal hernia in each case were collected.
The patients were stratified into three groups according to BMI: a normal weight group (BMI < 25 kg/m2), an overweight group (BMI 25-30 kg/m2), and an obese group (BMI > 30 kg/m2). All patients were asked to complete the modified Chinese GERD questionnaire (GERDQ) and the short-form 36 (SF-36) questionnaire (Chinese version).
The modified Chinese GERDQ included with the severity and frequency of symptoms of regurgitation and heartburn, graded on a 3-point Likert scale. Mild, moderate and advanced severity were defined, respectively, as symptoms that can easily be ignored, symptoms that can be easily tolerated, and symptoms sufficient to cause interference with normal activities. Low, middle, and high frequency were classified, respectively, as at least once per month, at least once weekly, and at least once daily[9].
The SF-36 questionnaire measures generic quality of life, which allows comparisons between different disease states. It measures health status in eight domains: physical functioning, role limitations-physical, bodily pain, general health, vitality, social functioning, role limitations-emotional, and mental health. Two summary scores are also calculated from subject responses: the physical health (PH) score and the mental health (MH) score. Scores on the SF-36 range from 0 to 100 on each dimension and on the summary scales, with higher scores indicating better quality of life[10,11].
Data are expressed as mean and standard deviation for each of the measured parameters. Gender and endoscopic findings, including hiatal hernia and erosive esophagitis, are expressed as a percentage of the total patient number. A P value < 0.05 was considered statistically significant. Statistical comparisons were made using Pearson’s χ2 test to compare the effects of gender and endoscopic findings; analysis of variance was used to analyze age, symptom duration, and of questionnaire scores.
RESULTS
A total of 173 consecutive patients were enrolled between January 2009 and March 2010, with 102 (58.9%), 56 (32.4%), and 15 patients (8.7%) assigned to the normal weight, overweight, and obese groups, respectively. As shown in Table 1, there were significantly more women in the normal weight group (67.6%), but significantly more men in the overweight (73.2%) and obese (73.3%) groups. A longer mean duration of GERD symptoms was noted in patients with increased BMI (normal weight group 2.17 mo, overweight group 2.64 mo, obese group 3.15 mo, P = 0.406), although the differences were not significant. The mean age of the cases in these three groups were similar.
Table 1.
Basic characteristics of the three groups of patients with gastroesophageal reflux disease
| Variable | Normal weight (n = 102) | Overweight (n = 56) | Obese (n = 15) | P value | |||
| n (%) | mean ± SD | n (%) | mean ± SD | n (%) | mean ± SD | ||
| Age (yr) | 44.32 ± 15.14 | 50.77 ± 15.88 | 41.47 ± 12.24 | 0.4232 | |||
| Gender | 0.0011 | ||||||
| Male | 33 (32.4) | 41 (73.2) | 11 (73.3) | ||||
| Female | 69 (67.6) | 15 (26.8) | 4 (26.7) | ||||
| Symptom duration (mo) | 2.17 ± 3.16 | 2.64 ± 3.69 | 3.15 ± 4.30 | 0.4062 | |||
| NERD | 62 (60.8) | 20 (35.7) | 4 (26.7) | 0.0021 | |||
| EE | 40 (39.2) | 36 (64.3) | 11 (73.3) | ||||
| Hiatal hernia | 17 (16.7) | 19 (33.9) | 9 (60.0) | 0.0011 | |||
| ECJ ulcer | 7 (6.9) | 5 (8.9) | 2 (13.3) | 0.6661 | |||
Pearson’s Chi-square test;
Analysis of variance. ECJ: Esophagocardiac junction; EE: Erosive esophagitis; NERD: Non-erosive reflux disease.
The endoscopic findings among the three groups are also summarized in Table 1. The more obese patients had a significantly greater rate of erosive esophagitis (73.3% in the obese group, 64.4% in the overweight group, 39.2% in the normal weight group, P = 0.002), and hiatal hernia (60% in the obese group, 33.9% in the overweight group, 16.7% in the normal weight group, P = 0.001). Furthermore, there was a trend for the rate of esophagocardiac ulcer to be increased in obese patients (13.3% in the obese group, 8.9% in the overweight group, 6.9% in the normal weight group, P = 0.666).
The severity and frequency of heartburn and acid regurgitation, measured by the modified Chinese GERDQ, among the three groups are presented in Table 2. There was significantly greater severity and higher frequency of heartburn in obese patients than in those with normal BMI. In contrast, the severity and frequency of acid regurgitation wer similar among these groups.
Table 2.
Basic characteristic of the three groups of male and female patients with gastroesophageal reflux disease
| Variable | Normal weight (n = 102) | Overweight (n = 56) | Obesity (n = 15) | P value | |||
| n (%) | mean ± SD | n (%) | mean ± SD | n (%) | mean ± SD | ||
| Male | 33 (38.8) | 41 (48.3) | 11(12.9) | ||||
| Mean age (yr) | 51.88 ± 16.93 | 52.54 ± 16.96 | 39.64 ± 11.09 | 0.1052 | |||
| NERD | 20 (60.6) | 10 (24.4) | 4 (36.4) | 0.0071 | |||
| EE | 13 (39.4) | 31 (75.6) | 7 (63.6) | ||||
| Hiatal hernia | 10 (30.3) | 14 (34.1) | 7 (63.6) | 0.1261 | |||
| ECJ ulcer | 5 (15.2) | 5 (12.2) | 2 (18.2) | 0.8591 | |||
| Female | 69 (78.4) | 15 (17.1) | 4 (4.5) | ||||
| Age (yr) | 40.71 ± 12.84 | 45.93 ± 11.59 | 46.50 ± 15.59 | 0.2482 | |||
| NERD | 42 (60.9) | 10 (66.7) | 0 | 0.0451 | |||
| EE | 27 (39.1) | 5 (33.3) | 4 (100) | ||||
| Hiatal hernia | 7 (10.1) | 5 (33.3) | 2 (50.0) | 0.0141 | |||
| ECJ ulcer | 2 (2.9) | 0 | 0 | 0.7541 | |||
Pearson’s χ2 test;
Analysis of variance. ECJ: Esophagocardiac junction; EE: Erosive esophagitis; NERD: Non-erosive reflux disease.
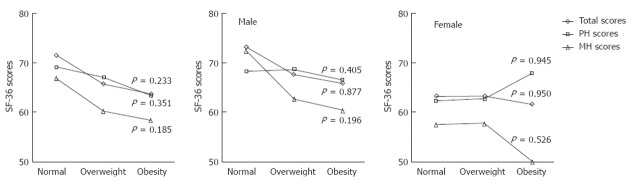
The total scores, PH scores and MH scores, measured by the SF-36 questionnaire, are shown in Figure 1. The patients in the obese group tended to have lower scores (mean total score 63.64, PH score 63.44, MH score 58.32), than those in the overweight group (mean total score 65.69, PH score 66.90, MH score 60.20) and in the normal group (mean total score 71.47, PH score 69.02, MH score 66.87), but there was no significant difference among these groups (P = 0.351).
Figure 1.
Characteristics of short-form 36 questionnaire scores in obese patients with gastroesophageal reflux disease. SF-36: Short-form 36; PH: Physical health; MH: Mental health.
Comparing the endoscopic findings by gender, as shown in Table 2, men were more prone to have erosive esophagitis in the overweight (75.6%) and obese (63.6%) groups. In contrast, women had similar rates of erosive eosphagitis, in the normal weight group (39.1%) or the overweight group (33.3%), though all four obese women had erosive esophagitis. The occurrence of hiatal hernia had a significantly positive correlation with obesity in women (P = 0.014), but not in men (P = 0.126).
The severity and frequency of heartburn and acid regurgitation among the three groups of men and women are shown separately in Figure 2. In general, the male cases had more serious symptoms, and there was significantly greater severity and frequency of heartburn in obese males (P = 0.001). In contrast, there were no differences in severity and frequency of heartburn and acid regurgitation among female patients in all groups
Figure 2.
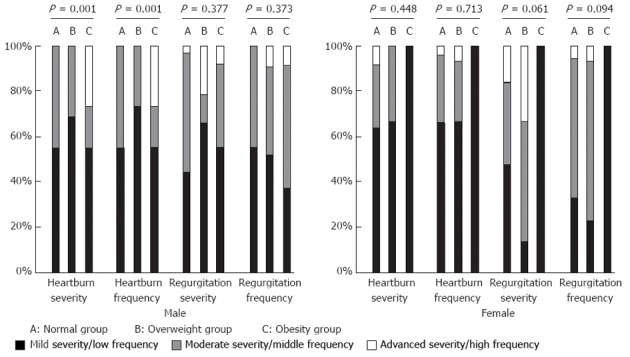
Rates of clinical presentation of symptoms in obese patients with gastroesophageal reflux disease.
The scores of the SF-36 questionnaire in male and female patients are also summarized in Figure 1. The men in the obese group had the lowest scores (mean total score 65.97, PH score 66.33, MH score 60.33), followed by those in the overweight group (mean total score 67.59, PH score 68.61, MH score 62.63) and those in the normal weight group (mean total score 73.27, PH score 68.09, MH score 72.82). In contrast, there were no differences in women’s scores among the obese group (mean total score 61.67, PH score 68.02, MH score 49.32), the overweight group (mean total score 63.40, PH score 62.91, MH score 67.81) and the normal weight group (mean total score 63.06, PH score 62.52, MH score 57.59).
DISCUSSION
GERD is a chronic disease which has an impact on the everyday lives of affected individuals, and obesity is found to be a significant risk factor in the development of severe forms of GERD. Changes in gastroesophageal anatomy and physiology caused by obesity may explain the association. Thus, obese patients may experience extrinsic gastric compression by surrounding adipose tissue, and has been associated with significantly increased intra-abdominal pressure[12], impaired gastric emptying[13], decreased lower esophageal sphincter pressure, and increased frequency of transient sphincter relaxation[14,15], leading to increased esophageal acid exposure time[5] .
Obesity is also considered an independent risk factor for the presence of a hiatal hernia[6], which has a role in initiating and promoting GERD. In patients with a hiatal hernia, esophagitis or abnormal low distal esophageal pH were more common than in those without a hiatal hernia[5]. However, after controlling for the presence of hiatal hernia, obesity still remained an independent risk factor for severe esophagitis[3].
In our study, obese patients with GERD had a significantly higher rate of erosive esophagitis and hiatal hernia, but the mean age and GERD symptom duration of these cases were not different. Furthermore, obese men had a more significant association with erosive esophagitis than obese women, but the association of hiatal hernia and obesity was significant only in female patients. Thus, both obesity and hiatal hernia were contributing factors to GERD, but there existed a complicated pathogenesis.
A German study reported that neither the frequency nor the duration of symptoms, including heartburn and acid regurgitation, differed significantly between obese patients and normal body mass cases[16]. Another study reported a positive association between frequency of reflux symptoms and BMI[17]. In addition, an increase in reflux symptoms has been shown to occur in individuals who gain weight, contributing to the epidemiological evidence for a possible dose-response relationship between BMI and increasing GERD symptoms[4].
There were many previous studies discussing the impact of different genders on GERD. One famous study examined a large population-based cohort and found that obese women had an increased risk for GERD symptoms compared with obese men, and the risk was highest in premenopausal women and postmenopausal women receiving estrogen therapy[18]. Other population-based case-control endoscopic studies found a strong and dose-dependent association between BMI and reflux esophagitis, particularly in women rather than men, and hypothesized that this might be caused by increased estrogen activity in overweight and obese females[19,20].
However, several other studies found that the increased risk of acid-related esophageal disease among overweight and obese persons was neither confounded nor modified by gender. For example, a large cross-sectional study found that increased BMI was associated with reflux symptoms, but the relationship differed for different ethnic groups, with a much greater association in whites, but no relationship in the Asian population in either men or women[21]. A recent systematic review either found no association between gender and GERD symptoms[22]. Thus, the estrogen hypothesis does not explain the gender- or race-related differences in GERD.
Our study documented that both the severity and frequency of heartburn had a positive correlation with BMI, but the symptom of acid regurgitation did not. The relationship was present in male patients, but not in females. A Spanish study in severely obese patients found higher rates of heartburn (46.4%) than acid regurgitation (22.5%), and the frequency of symptoms was higher in men than in women[23], which was similar to our results. The possible explanation of the gender predilection of GERD symptoms in males is that abdominal obesity is characteristic of male pattern obesity, and abdominal obesity is known to be a key factor in both the symptoms and perhaps even the complications of GERD.
The results of our study also found reduced overall quality of life scores, measured by the SF-36 questionnaire, in obese patients with GERD, and the association was observed in male patients, but not in females. Increasing overweight has been associated with a deterioration in quality of life, and the risk of suffering from any longstanding illness is associated with an increased BMI[6]. Obese women perceived markedly more psychosocial problems due to their obesity than men[24]. In our patients, obese women had the lowest MH scores (60.33) among all groups in our study.
There were some limitations in our study. Firstly, the lifestyle characteristics in our study were only limited to the patients’ current status, and the past history of each case, such as cigarette smoking and alcohol consumption, was not recorded. Secondly, comorbidity in these patients that tend to influence the severity of GERD, such as chronic heart failure or chronic obstructive pulmonary disease, were not considered, and this might have led to inaccurate outcomes. Thirdly, we only collected the BMI of each patient, but abdominal girth, an indicator of abdominal obesity, might be more correlated with GERD. In addition, a long-term record of BMI would also be necessary to ensure adequate analysis of the relationship of obesity with GERD. Lastly, our study’s design was hospital-based and included only a small number of cases. Further research in representative samples of the general population are needed to confirm these results.
In conclusion, in the present study, obese GERD patients were more likely to have higher rates of erosive esophagitis and hiatal hernia, more severe and frequent heartburn symptoms, and a poorer quality of life. Obesity in men was associated with the most severe endoscopic and clinical presentations, but obesity in women had the greatest influence on mental health.
COMMENTS
Background
Gastroesophageal reflux disease (GERD) is a chronic disease that tends to relapse and develop complications. Obesity constitutes a public health problem in most industrialized countries, and impairs health-related quality of life. At present, there are few studies on the assessment of quality of life performed on obese patients with GERD.
Research frontiers
Body mass index is one risk factor for GERD. The aim of the study was to investigate symptom presentation and quality of life in male and female obese patients with GERD among a Chinese population.
Innovations and breakthroughs
Obese GERD patients had higher rates of erosive esophagitis and hiatal hernia, more severe and frequent heartburn, and poorer quality of life. Obese men had the most severe endoscopic and clinical presentation, while obese women had the poorest mental health.
Applications
The presentations and impact of GERD were apparent in obese patients, but different between men and women. Obese women had the worst quality of life.
Peer review
This is a good descriptive study in which authors investigate the symptom presentation and quality of life in the obese patients with GERD among a Chinese population. The results are interesting and suggest that the obese men owned the most severe endoscopic and clinical presentation, but obese women had the worst mental health.
Footnotes
Peer reviewer: Dr. Wojciech Blonski, MD, PhD, Gastroenterology Unit, University of Pennsylvania, 3400 Spruce St, Philadelphia, PA 19104, United States
S- Editor Gou SX L- Editor Cant MR E- Editor Li JY
References
- 1.Mold JW, Reed LE, Davis AB, Allen ML, Decktor DL, Robinson M. Prevalence of gastroesophageal reflux in elderly patients in a primary care setting. Am J Gastroenterol. 1991;86:965–970. [PubMed] [Google Scholar]
- 2.Lee SW, Chang CM, Chang CS, Kao AW, Chou MC. Comparison of presentation and impact on quality of life of gastroesophageal reflux disease between young and old adults in a Chinese population. World J Gastroenterol. 2011;17:4614–4618. doi: 10.3748/wjg.v17.i41.4614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.El-Serag HB, Johanson JF. Risk factors for the severity of erosive esophagitis in Helicobacter pylori-negative patients with gastroesophageal reflux disease. Scand J Gastroenterol. 2002;37:899–904. doi: 10.1080/003655202760230847. [DOI] [PubMed] [Google Scholar]
- 4.El-Serag H. The association between obesity and GERD: a review of the epidemiological evidence. Dig Dis Sci. 2008;53:2307–2312. doi: 10.1007/s10620-008-0413-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Iovino P, Angrisani L, Galloro G, Consalvo D, Tremolaterra F, Pascariello A, Ciacci C. Proximal stomach function in obesity with normal or abnormal oesophageal acid exposure. Neurogastroenterol Motil. 2006;18:425–432. doi: 10.1111/j.1365-2982.2006.00768.x. [DOI] [PubMed] [Google Scholar]
- 6.Wilson LJ, Ma W, Hirschowitz BI. Association of obesity with hiatal hernia and esophagitis. Am J Gastroenterol. 1999;94:2840–2844. doi: 10.1111/j.1572-0241.1999.01426.x. [DOI] [PubMed] [Google Scholar]
- 7.Doll HA, Petersen SE, Stewart-Brown SL. Obesity and physical and emotional well-being: associations between body mass index, chronic illness, and the physical and mental components of the SF-36 questionnaire. Obes Res. 2000;8:160–170. doi: 10.1038/oby.2000.17. [DOI] [PubMed] [Google Scholar]
- 8.Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R. The Montreal definition and classification of gastroesophageal reflux disease: a global, evidence-based consensus paper. Z Gastroenterol. 2007;45:1125–1140. doi: 10.1055/s-2007-963633. [DOI] [PubMed] [Google Scholar]
- 9.Wong WM, Lam KF, Lai KC, Hui WM, Hu WH, Lam CL, Wong NY, Xia HH, Huang JQ, Chan AO, et al. A validated symptoms questionnaire (Chinese GERDQ) for the diagnosis of gastro-oesophageal reflux disease in the Chinese population. Aliment Pharmacol Ther. 2003;17:1407–1413. doi: 10.1046/j.1365-2036.2003.01576.x. [DOI] [PubMed] [Google Scholar]
- 10.Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 11.Revicki DA, Wood M, Maton PN, Sorensen S. The impact of gastroesophageal reflux disease on health-related quality of life. Am J Med. 1998;104:252–258. doi: 10.1016/s0002-9343(97)00354-9. [DOI] [PubMed] [Google Scholar]
- 12.Barak N, Ehrenpreis ED, Harrison JR, Sitrin MD. Gastro-oesophageal reflux disease in obesity: pathophysiological and therapeutic considerations. Obes Rev. 2002;3:9–15. doi: 10.1046/j.1467-789x.2002.00049.x. [DOI] [PubMed] [Google Scholar]
- 13.Maddox A, Horowitz M, Wishart J, Collins P. Gastric and oesophageal emptying in obesity. Scand J Gastroenterol. 1989;24:593–598. doi: 10.3109/00365528909093095. [DOI] [PubMed] [Google Scholar]
- 14.O'Brien TF. Lower esophageal sphincter pressure (LESP) and esophageal function in obese humans. J Clin Gastroenterol. 1980;2:145–148. [PubMed] [Google Scholar]
- 15.Orlando RC. Overview of the mechanisms of gastroesophageal reflux. Am J Med. 2001;111 Suppl 8A:174S–177S. doi: 10.1016/s0002-9343(01)00828-2. [DOI] [PubMed] [Google Scholar]
- 16.Madisch A, Weihs C, Schlaud M, Heimann D, Meyer H, Hotz J. The Body-Mass-Index (BMI) has no impact on the frequency of typical reflux symptoms -- results of a nationwide telephone-based informing campaign in Germany. Zentralbl Chir. 2002;127:1064–1067. doi: 10.1055/s-2002-36464. [DOI] [PubMed] [Google Scholar]
- 17.Locke GR, Talley NJ, Fett SL, Zinsmeister AR, Melton LJ. Risk factors associated with symptoms of gastroesophageal reflux. Am J Med. 1999;106:642–649. doi: 10.1016/s0002-9343(99)00121-7. [DOI] [PubMed] [Google Scholar]
- 18.Nilsson M, Johnsen R, Ye W, Hveem K, Lagergren J. Obesity and estrogen as risk factors for gastroesophageal reflux symptoms. JAMA. 2003;290:66–72. doi: 10.1001/jama.290.1.66. [DOI] [PubMed] [Google Scholar]
- 19.Stene-Larsen G, Weberg R, Frøyshov Larsen I, Bjørtuft O, Hoel B, Berstad A. Relationship of overweight to hiatus hernia and reflux oesophagitis. Scand J Gastroenterol. 1988;23:427–432. doi: 10.3109/00365528809093890. [DOI] [PubMed] [Google Scholar]
- 20.Nilsson M, Lundegårdh G, Carling L, Ye W, Lagergren J. Body mass and reflux oesophagitis: an oestrogen-dependent association? Scand J Gastroenterol. 2002;37:626–630. doi: 10.1080/00365520212502. [DOI] [PubMed] [Google Scholar]
- 21.Corley DA, Kubo A, Zhao W. Abdominal obesity, ethnicity and gastro-oesophageal reflux symptoms. Gut. 2007;56:756–762. doi: 10.1136/gut.2006.109413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dent J, El-Serag HB, Wallander MA, Johansson S. Epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut. 2005;54:710–717. doi: 10.1136/gut.2004.051821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ortiz V, Ponce M, Fernández A, Martínez B, Ponce JL, Garrigues V, Ponce J. Value of heartburn for diagnosing gastroesophageal reflux disease in severely obese patients. Obesity (Silver Spring) 2006;14:696–700. doi: 10.1038/oby.2006.79. [DOI] [PubMed] [Google Scholar]
- 24.Sullivan M, Karlsson J, Sjöström L, Backman L, Bengtsson C, Bouchard C, Dahlgren S, Jonsson E, Larsson B, Lindstedt S. Swedish obese subjects (SOS)--an intervention study of obesity. Baseline evaluation of health and psychosocial functioning in the first 1743 subjects examined. Int J Obes Relat Metab Disord. 1993;17:503–512. [PubMed] [Google Scholar]