Abstract
Ulcerative jejunoileitis is an uncommon clinical syndrome consisting of abdominal pain, weight loss associated with diarrhea, and multiple inflammatory ulcerations and strictures of the small bowel. Ulcerative jejunoileitis can complicate established celiac disease or develop in patients de novo. Increased levels of tumor necrosis factor-alpha (TNF-α) in the small intestine of patients with untreated celiac disease are associated with a role in the immune pathogenesis of this disorder. No specific therapy has been shown to change the course of ulcerative jejunoileitis. We report a case of severe ulcerative jejunoileitis previously unresponsive to traditional therapies, including high dose corticosteroids and cyclosporine. The patient had a dramatic resolution of symptoms and a complete normalization of endoscopic findings after anti-TNF-α monoclonal antibody, infliximab (Remicade®).
Keywords: Ulcerative jejunoileitis, Biologic therapy, Tumor necrosis factor-alpha, Infliximab
INTRODUCTION
Ulcerative jejunoileitis, also termed chronic nongranulomatous enteritis or idiopathic chronic ulcerative jejunoileitis, is a clinical syndrome consisting of abdominal pain, diarrhea, and multiple inflammatory ulcerations of the small bowel, especially the jejunum[1]. Ulcerative jejunoileitis can complicate established celiac disease or occur in patients de novo[1,2]. It is uncommon and largely a diagnosis of exclusion.
CASE REPORT
A 62-year-old man presented in May 2009 with a 20-year history of intermittent abdominal pain, diarrhea, weight loss, and gastrointestinal bleeding. In 2008, he was admitted at another institution with abdominal pain, and found to have a perforated jejunum with an interloop abscess requiring small bowel resection. There was no evidence of granulomas or histologic Crohn’s disease in the resected specimen, and no history of diverticulum at the site of perforation. He was hospitalized several times with pain, bleeding, and intussusception in the postoperative period. He had been started on 25 mg prednisone per day preoperatively because of possible Crohn’s disease and continued on this medication.
Physical examination revealed a chronically ill, tremulous man. His prednisone was increased to 40 mg/d, but the patient continued to have abdominal pain and bloody bowel movements. Enteroscopy showed circumferential ulceration and a stricture of the distal esophagus with a clot, severe duodenal ulceration, a stricture and a 4-cm ulcer cavity at the jejunal anastomosis as well as more distal ulceration (Figure 1A and B). Computerized tomography (CT) of the abdomen demonstrated a long segment of inflamed jejunum and mesenteric adenopathy. Serum gastrin level was normal. Despite parenteral nutrition, 60 mg/d of prednisone and 8 mg/kg per day of oral cyclosporine, the patient continued to have refractory diarrhea and bleeding. Repeat endoscopies demonstrated deep anastomotic and multiple distal ulcerations.
Figure 1.
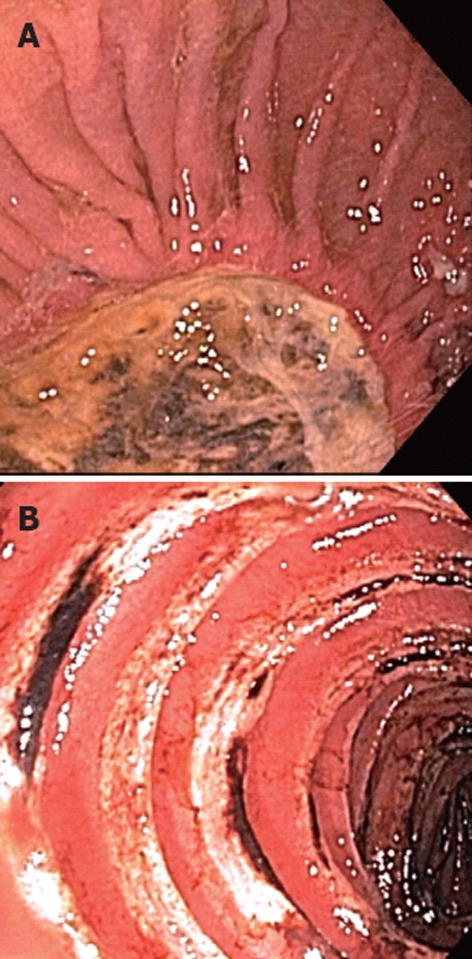
Enteroscopic appearance of the lesions. A: A 4-cm chronic cavity consistent with chronic perforation at the jejunal anastomosis; B: More distal jejunal ulcerations.
Because of relapsing bleeding and steroid-dependence, infliximab was initiated at 5 mg/kg dose at 0, 2 and 6 wk, followed by every eight-week intervals in conjuction with cyclosporine and prednisone. One month after initial infusion, he was admitted with rebleeding from the anastomotic ulcer (Figure 2). Angiography was negative for active bleeding. An exploratory laparotomy was performed with distal duodenal and proximal jejunal resection and revealed a chronic 5 cm jejunal ulcer at the jejunojejunostomy site associated with microperforation and an inflammatory mass with matted lymph nodes. Full thickness biopsies of the jejunum demonstrated multiple ulcerations but no features of Crohn’s, celiac disease, ischemia, lymphoma, vasculitis, neoplasm, or infectious etiology (Figure 3A-C). After the surgery, prednisone was tapered and discontinued 6 mo postoperatively.
Figure 2.
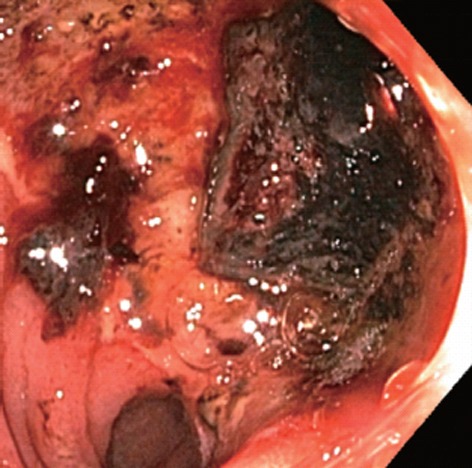
Endoscopy showing bleeding from an anastomotic ulcer.
Figure 3.
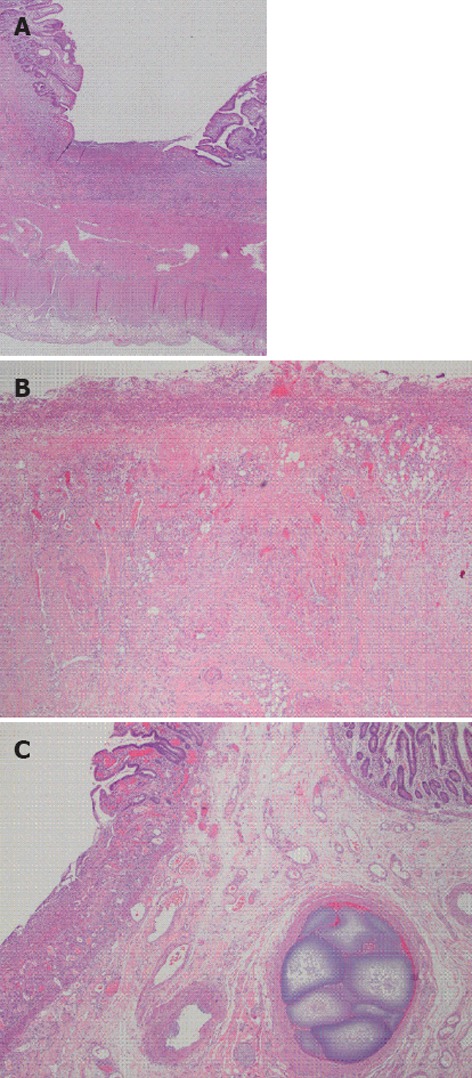
Surgically resected jejunum. A: Full thickness small bowel section showing ulcerated small intestinal mucosa; B: Ulcer bed showing acute and chronic inflammation, granulation tissue and overlying fibrinopurulent exudate, no granulomas are seen; C: Intravascular embolization material in submucosal blood vessel.
To date (30 mo), the patient is stable on every eight week infliximab infusion. His PPI has been discontinued, and there is no evidence of ulceration, enteritis, or lymphoma on follow-up enteroscopy (Figure 4A and B), colonoscopy, or abdominal CT.
Figure 4.
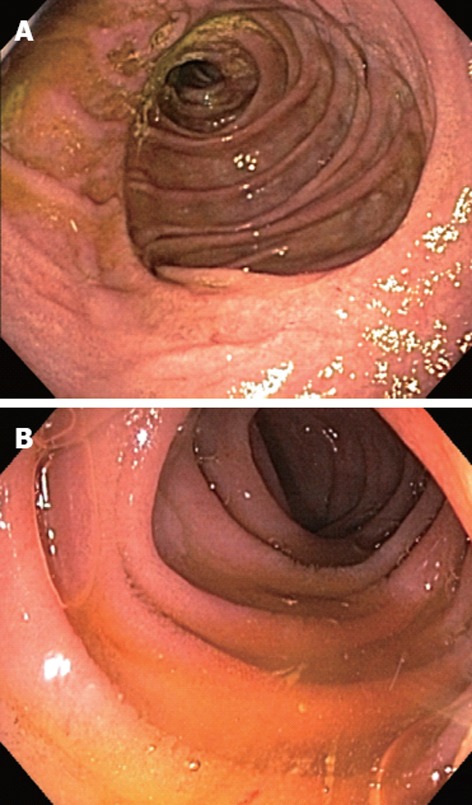
Complete improvement on endoscopic findings after infliximab therapy. A: Jejunojejunostomy; B: Distal jejunum.
DISCUSSION
Although pathophysiology of ulcerative jejunoileitis is poorly understood, it may be related to mucosal infiltration by activated T-cells. A molecular analysis of mucosal T-cell populations has previously shown that monoclonal T-cells exist in ulcers and normal mucosa, suggesting a fundamental role of T-cells in ulcer pathogenesis[3]. Another study demonstrated that the cytotoxic capability of T-cells is responsible for the development of the ulcers with preference for mucosa-associated lymphoid tissue localization[4]. Tumor necrosis factor alpha (TNF-α) plays a pivotal role in Crohn’s disease[5]. Increased levels of interleukin-6 and TNF-α in the lamina propria and epithelium of patients with untreated celiac disease also support their role in the development of the mucosal damage observed in celiac disease[6]. Infliximab therapy results in a reduction in the activated T lymphocytes that accumulate within the lamina propria in Crohn’s disease, and neutralization of TNF is effective in induction and maintenance of remission in Crohn’s disease[7]. Case reports using infliximab in patients with refractory celiac disease have shown improvement in symptoms, and duodenal histology[8,9]. One additional case of ulcerative jejunoileitis complicating refractory celiac disease has been published, demonstrating improvement in fecal output and small bowel histology[10]. However, a complete recovery was not achieved and parenteral nutritional support continued. Seven months later, the patient developed a stenosis of the distal ileum and surgical resection demonstrated enteropathy-associated T-cell lymphoma.
In contrast, we have demonstrated that infliximab plays a key role in the management of ulcerative jejunoileitis and should be considered a treatment option for patients with this disorder.
Footnotes
Peer reviewer: Dr. Lisheng Zhang, Beckman Research Institute, City of Hope/National Medical Center, Duarte, CA 91010, United States
S- Editor Gou SX L- Editor A E- Editor Li JY
References
- 1.Biagi F, Lorenzini P, Corazza GR. Literature review on the clinical relationship between ulcerative jejunoileitis, coeliac disease, and enteropathy-associated T-cell. Scand J Gastroenterol. 2000;35:785–790. doi: 10.1080/003655200750023129. [DOI] [PubMed] [Google Scholar]
- 2.O’Mahony S, Howdle PD, Losowsky MS. Review article: management of patients with non-responsive coeliac disease. Aliment Pharmacol Ther. 1996;10:671–680. doi: 10.1046/j.1365-2036.1996.66237000.x. [DOI] [PubMed] [Google Scholar]
- 3.Ashton-Key M, Diss TC, Pan L, Du MQ, Isaacson PG. Molecular analysis of T-cell clonality in ulcerative jejunitis and enteropathy-associated T-cell lymphoma. Am J Pathol. 1997;151:493–498. [PMC free article] [PubMed] [Google Scholar]
- 4.de Bruin PC, Kummer JA, van der Valk P, van Heerde P, Kluin PM, Willemze R, Ossenkoppele GJ, Radaszkiewicz T, Meijer CJ. Granzyme B-expressing peripheral T-cell lymphomas: neoplastic equivalents of activated cytotoxic T cells with preference for mucosa-associated lymphoid tissue localization. Blood. 1994;84:3785–3791. [PubMed] [Google Scholar]
- 5.Plevy SE, Landers CJ, Prehn J, Carramanzana NM, Deem RL, Shealy D, Targan SR. A role for TNF-alpha and mucosal T helper-1 cytokines in the pathogenesis of Crohn’s disease. J Immunol. 1997;159:6276–6282. [PubMed] [Google Scholar]
- 6.Przemioslo RT, Kontakou M, Nobili V, Ciclitira PJ. Raised pro-inflammatory cytokines interleukin 6 and tumour necrosis factor alpha in coeliac disease mucosa detected by immunohistochemistry. Gut. 1994;35:1398–1403. doi: 10.1136/gut.35.10.1398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.van Dullemen HM, van Deventer SJ, Hommes DW, Bijl HA, Jansen J, Tytgat GN, Woody J. Treatment of Crohn’s disease with anti-tumor necrosis factor chimeric monoclonal antibody (cA2) Gastroenterology. 1995;109:129–135. doi: 10.1016/0016-5085(95)90277-5. [DOI] [PubMed] [Google Scholar]
- 8.Gillett HR, Arnott ID, McIntyre M, Campbell S, Dahele A, Priest M, Jackson R, Ghosh S. Successful infliximab treatment for steroid-refractory celiac disease: a case report. Gastroenterology. 2002;122:800–805. doi: 10.1053/gast.2002.31874. [DOI] [PubMed] [Google Scholar]
- 9.Turner SM, Moorghen M, Probert CS. Refractory coeliac disease: remission with infliximab and immunomodulators. Eur J Gastroenterol Hepatol. 2005;17:667–669. doi: 10.1097/00042737-200506000-00012. [DOI] [PubMed] [Google Scholar]
- 10.Gaia S, Bruno M, Marzano A, Novero D, Astegiano M, Actis GC, Rizzetto M. A case of ulcerative jejunoileitis treated with anti tumor necrosis factor-alpha antibodies. Panminerva Med. 2005;47:269–272. [PubMed] [Google Scholar]


