Abstract
Background
In HCM, myocardial abnormalities are commonly heterogeneous. Two patterns of LGE have been reported: a bright “confluent” and an intermediate intensity abnormality termed “diffuse,” each representing different degrees of myocardial scarring. We used MRI to study the relation between intramural cardiac function and the extent of fibrosis in HCM. The aim of this study was to determine whether excess collagen or myocardial scarring, as determined by late gadolinium enhancement (LGE) MRI, are the primary mechanisms leading to heterogeneous regional contractile function in patients with hypertrophic cardiomyopathy (HCM).
Methods and Results
Intramural left ventricular (LV) strain, transmural LV function, and regions of myocardial fibrosis/scarring were imaged in 22 patients with HCM using displacement encoding with stimulated echoes (DENSE), cine MRI and LGE. DENSE systolic strain maps were qualitatively and quantitatively compared with LGE images. Intramural systolic strain by DENSE was significantly depressed within areas of confluent and diffuse LGE but also in the core of the most hypertrophic non-enhanced segment (all p<0.001 vs. non-hypertrophied segments). DENSE demonstrated an unexpected inner rim of largely preserved contractile function and a non-contracting outer wall within hypertrophic segments in 91% of patients.
Conclusions
LGE predicted some but not all of the heterogeneity of intramural contractile abnormalities. This indicates that myocardial scarring or excess interstitial collagen deposition does not fully explain the observed contractile heterogeneity in HCM. Thus, myofibril disarray or other non-fibrotic processes affect systolic function in a large number of patients with HCM.
Keywords: hypertrophic cardiomyopathy, magnetic resonance imaging, DENSE, displacement encoding with stimulated echoes, myocardial function, strain, late gadolinium enhancement
Hypertrophic cardiomyopathy (HCM) is a genetic disease characterized by left ventricular (LV) hypertrophy1, 2 due to hyperplasia and hypertrophy of myocytes and hyperplasia of several other cell types. Myofiber disarray and interstitial fibrosis occur commonly 3, 4. Hypertrophy and fibrosis are associated with LV systolic and diastolic dysfunction, heart failure, arrhythmias, morbidity, and mortality 5–8. Myocardial ischemia, infarction and fibrosis occur in HCM despite widely-patent epicardial coronary artery vessels 9, 10,6. MRI late gadolinium enhancement (LGE) has revealed two types of abnormalities which may be related to infarction or fibrosis. Confluent LGE appears in most respects comparable to the type of bright gadolinium enhancement seen in the myocardial infarctions of patients with ischemic heart disease 11. Diffuse LGE likely represents less severe myocardial fibrosis or milder degrees of excess collagen deposition. It has also been postulated that the interstitial fibrosis may be a secondary and reversible phenotype 5, 12.
Extrapolations from transmural measurements of myocardial strain have led some investigators to postulate that patients with HCM may have preserved endocardial strain 13, 14 while others suggest there should be reduced endocardial strain 15, 16. A study by Tseng et al. 4 shows that myocardial fiber disarray is related to reduced myocardial strain. However, this study does not address the presence or absence of myocardial fibrosis within the hypokinetic regions. A more recent echocardiographic study by Popovic et al. 17 reports that non-fibrotic myocardial segments exhibit increased strain compared to segments with fibrosis. This finding suggests that perhaps some function is preserved in non-fibrotic hypertrophic segments. However, this could also reflect partial volume effects since average midwall strain measurements were studied in a 12 segment model.
High resolution imaging of intramural strain might provide insight into the relative contribution of myocardial fiber disarray and myocardial fibrosis as distinct mechanisms causing regional LV dysfunction. DENSE 18, 19 (Displacement Encoding with Stimulated Echoes) MRI can quantify short axis regional systolic function at high spatial resolution. DENSE allows direct measurement of intramural myocardial strain expressed in terms of circumferential shortening (CS) and radial thickening (RT) - a significant advance over transmural measures of regional function such as absolute systolic change in wall thickness (in mm) or percent wall thickening.
This study aimed to determine whether excess collagen or myocardial scarring, as determined by gadolinium enhanced MRI, are the primary mechanisms leading to heterogeneous regional contractile function in patients with HCM. We hypothesized that if intramural contractile function in HCM is heterogeneous due to excess collagen deposition or myocardial scarring, then hypokinesis will be localized primarily in areas with LGE. However, if extensive hypokinesis is observed outside the areas of LGE, then excess collagen or myocardial scarring is unlikely to be the only mechanism leading to heterogeneous regional contractile function in patients with HCM. Finally, it is possible that severely hypertrophic myocardium has diffusely abnormal function regardless of regional fibrosis. This possibility is sometimes referred to as “muscle bound”. We also hypothesized that high resolution intramyocardial DENSE strain maps would be able to image these functional abnormalities. Such imaging should be able to resolve these three possibilities.
An unexpected finding of this work was the presence of largely preserved inner wall strain in hypertrophic segments with overall low transmural strain. While an endocardial ring of preserved contractility in HCM has been postulated to exist, 17 no direct visualization has been provided to date. Therefore, additional analysis of this pattern of intramural strain was performed since it was not predicted by geometric models of myocardial hypertrophy.
Methods
Study Population
Twenty-two patients with HCM were studied under research protocol 09-H-N237 approved by the National Heart Lung and Blood Institute’s review board. The diagnosis of HCM was established by echocardiography (>15 mm LV wall thickness in the absence of another cause for the increased cardiac mass). Patients with a history of alcohol septal ablation or cardiac surgery were excluded. Only patients who underwent both DENSE and LGE imaging were included. LV outflow tract gradients at rest were obtained by cardiac catheterization.
MRI Studies
Subjects were scanned in a 1.5 T MRI scanner using a cardiac phased array coil. LV systolic function and mass were imaged with cine MRI along contiguous short axis slices (typically with 1.4×1.4 mm/pixel and 8 mm slice thickness). Intramural circumferential shortening (CS) and radial thickening (RT) measurements were made with DENSE with a volumetric preparation. Displacement was mapped for every pixel of the end-systolic image allowing systolic strain (CS and RT) maps to be computed. End-systole was determined from the cine MRI. LGE imaging was performed with an inversion recovery method 20 after a dose of 0.2 mmol/kg gadopentetate dimeglumine (typical resolution of 1.4×1.4 mm/pixel, slice thickness of 8 mm) with the inversion time optimized to null normal myocardium.
Data analysis
LV ejection fraction and total myocardial mass were measured using computer assisted planimetry. The signal intensity was quantified in confluent and diffuse lesions21, from normal myocardium and the LV blood pool. In short, confluent lesions were defined as qualitatively having bright signal similar to that found in non-viable myocardium in patients with CAD. Diffuse lesions were defined as qualitatively having signal brighter than that of nulled myocardium and signal less bright than that of confluent lesions. The “most hypertrophic non-enhancing segment” was defined as the thickest segment (as seen on end-diastolic cine images) without LGE. To mitigate potential through-plane motion misregistration issues between DENSE and LGE, the adjacent slices to the one containing the “most hypertrophic non-enhancing segment” were examined for absence of LGE. Remote myocardium was defined as myocardium diametrically opposite to the hypertrophic segments. Following endocardial and epicardial segmentation, DENSE displacement maps were automatically processed to produce circumferential shortening (CS) and radial thickening (RT) strain maps 22. CS and RT maps were scaled using a standardized color scale that displayed quantitative regional function on a pixel-by-pixel basis. Region of Interest (ROI) analysis was performed to measure CS and RT within confluent, diffuse and most hypertrophic non-enhanced areas. Only one slice per patient was analyzed in order to preserve the independence of the samples. Apical slices were excluded from data analysis to avoid partial volume effects 23.
Statistical Analysis
Continuous measurements are expressed as mean ± standard deviation (SD) for descriptive purposes. Standard error of the mean (SEM) was used in figures where the primary purpose was to depict differences between two average values. Comparisons used a paired t-test with Bonferroni correction for multiple comparisons (p-values are presented unadjusted and the appropriate level of significance is used within each group of comparisons).
Results
Demographics
Six patients (Table 1) had severe symptoms related to LV outflow obstruction while others had mild or no symptoms. Four were asymptomatic, seven presented with shortness of breath (SOB), three with chest pain (CP) and eight with a combination of SOB and CP. The average pulmonary capillary wedge pressure (PCWP) was 12±5 mmHg but 6 patients had significantly elevated PCWP. The maximum wall thickness averaged 25±5 mm. Median value of LV mass was 185 grams (range: 76 to 567) and the ejection fraction averaged 66±6%. Median value of LGE was 5.8% of the left ventricle (range:1.8 to 41.5). Nineteen of the patients had asymmetric septal hypertrophy (ASH), two with severe concentric hypertrophy (CON) and one with hypertrophy localized to the mid-ventricle (MID). Of the 22 individuals evaluated, only 4 had identified mutations after an unbiased screening of the Beta-Myosin head (exons 1–23) (Table 1). Patient numbers 1 and 20 are related and have the R403Q mutation. Patient number 5 has the K847E mutation. Patient number 15 has a Val95Ala mutation in Alpha-tropomyosin. On the basis of the unbiased screening, it can be concluded that the other patients are very unlikely to have mutations in the Beta- Myosin head.
Table 1.
Demographics, clinical and hemodynamic findings
| Patient | Age | Gender | NYHA | Symptoms | HCM Pattern |
SAM | LVOT Gradient |
PCWP | Mutation | EP inducible | Arrhythmias, other findings |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 35 | F | 3 | CP, SOB | ASH | No | 14 | 19 | BMHC, R403Q | No | SVT, AF |
| 2 | 48 | M | 1 | None | CON | Yes | 4 | 10 | NA | NA | 1st deg AVB, SVT |
| 3 | 51 | F | 2 | SOB | ASH | No | 6 | 16 | NA | No | VT |
| 4 | 50 | M | 3 | CP, SOB | ASH | No | 0 | 12 | NA | NA | SVT, VT |
| 5 | 49 | F | 2 | CP | ASH | No | 22 | 10 | BMHC, K847E | NA | PAT |
| 6 | 66 | F | 2 | CP, SOB | ASH | Yes | 12 | 4 | NA | NA | VT, Provocable LVOT obstruction |
| 7 | 32 | F | 2 | SOB | ASH | No | 6 | 8 | NA | NA | |
| 8 | 41 | M | 1 | SOB | ASH | No | 0 | 9 | NA | No | VT |
| 9 | 49 | F | 3 | CP, SOB | ASH | No | 5 | 14 | NA | NA | AF, incomplete LBBB, VT |
| 10 | 23 | M | 1 | None | ASH | No | 8 | 8 | NA | NA | Brief run NSVT during EP testing, Negative holter |
| 11 | 27 | F | 1 | SOB | ASH | Yes | 12 | 9 | NA | No | Negative holter |
| 12 | 26 | M | 2 | CP, SOB | ASH | No | 0 | 7 | NA | No | Negative holter |
| 13 | 32 | M | 1 | None | MID | No | 20 | 8 | NA | NA | Provocable LVOT obstruction |
| 14 | 15 | M | 1 | None | ASH | No | 0 | 11 | NA | No | Provocable RVOT obstruction |
| 15 | 33 | F | 3 | SOB | ASH | No | 0 | 26 | a trop, Val95Ala | NA | |
| 16 | 35 | M | 2 | CP, SOB | ASH | Yes | 10 | NA | NA | VT | AT, VT |
| 17 | 24 | F | 2 | CP | ASH | Yes | 104 | 10 | NA | NA | Provocable LVOT obstruction |
| 18 | 44 | M | 3 | CP, SOB | ASH | No | 0 | 10 | NA | No | VT |
| 19 | 34 | F | 2 | SOB | ASH | Yes | 6 | 20 | NA | NA | |
| 20 | 49 | F | 3 | CP, SOB | ASH | No | 2 | 19 | BMHC, R403Q | NA | |
| 21 | 52 | M | 2 | SOB | CON | No | 0 | 10 | NA | No | TIA, Paroxysmal AF, NSVT |
| 22 | 19 | M | 1 | CP | ASH | No | NA | NA | NA | NA | Near syncope while driving, Negative holter |
NYHA = New York Heart Association classification; M = male; F = female; CP = Chest Pain; SOB = Shortness of Breath; HCM = Hypertrophic Cardiomyopathy; SAM = Systolic Anterior Motion of the mitral valve; LVOT = Left Ventricular Outflow Tract; RVOT = right ventricular outflow tract; EP = Electrophysiology; NA = not available; AF = atrial fibrillation; AVB = atrioventricular block; PAT = paroxysmal atrial tachycardia; VT = ventricular tachycardia; NSVT = non-sustained VT; TIA = transient ischemic attack
DENSE Detects Patterns of Intramural Contractile Function associated with LGE
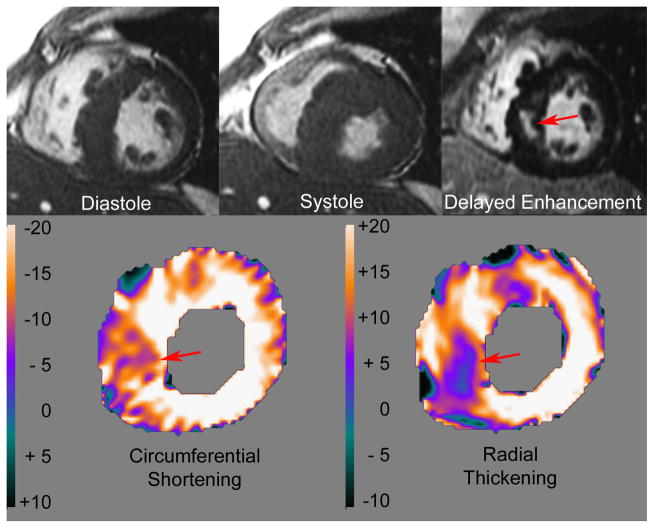
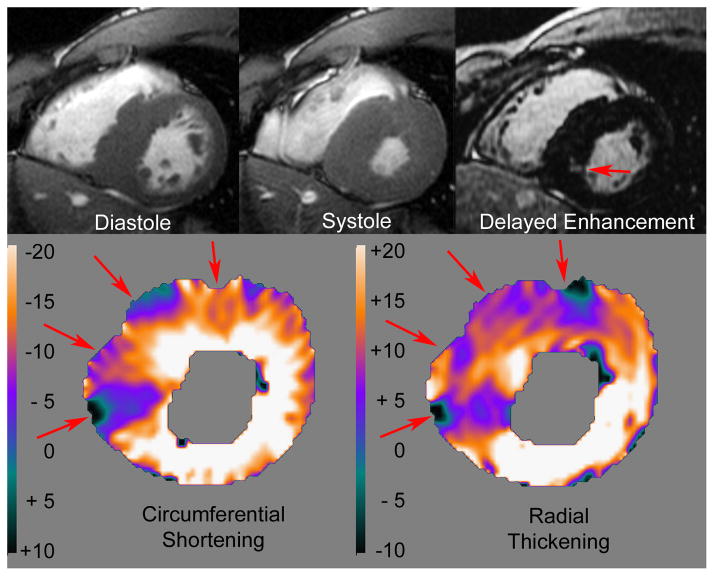
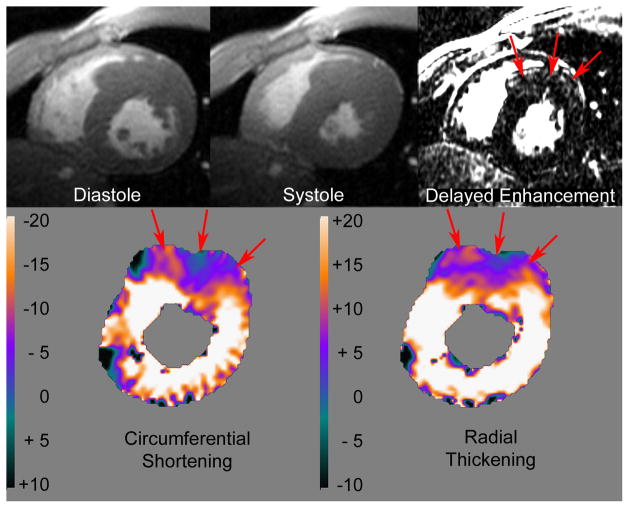
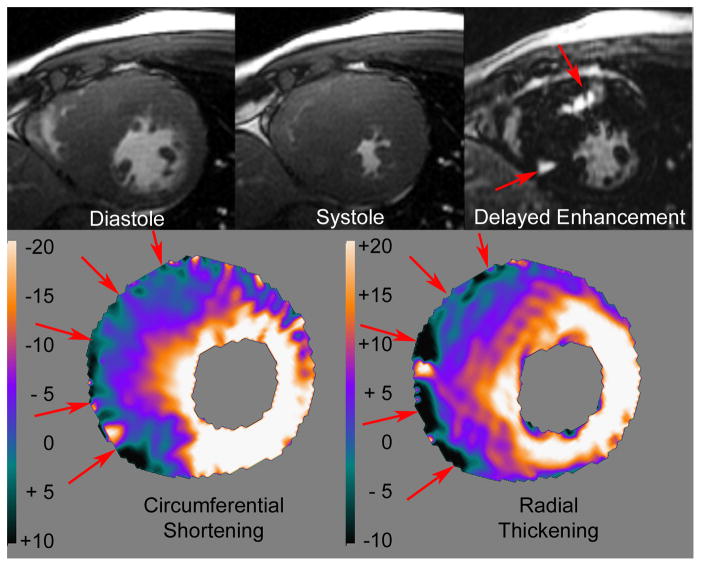
DENSE strain maps and LGE images can directly show that LGE is not a prerequisite for the presence of intramural functional abnormalities. DENSE functional abnormalities that are either more extensive than LGE imaging predicts or that are present in the absence of LGE can directly disprove the primary hypotheses. Figures 1–4 summarize the relationship between LGE and intramural cardiac function as depicted by DENSE CS and RT color strain maps. The color scale represents intramural percent circumferential shortening and percent radial thickening respectively. Normal CS and RT are generally mapped white to bright orange. Dark orange and purple hues represent mild and severe strain abnormalities. The transition from blue to green represents zero systolic strain. Green to black represents dyskinetic strain (i.e. systolic circumferential stretching or systolic radial thinning). Figures 1–4 also show diastolic and systolic frames from cine MRI (first and second images on the top row respectively) as well as LGE (third image on the top row).
Figure 1.
Patient with confluent late gadolinium enhancement in the inferior septum which colocalizes with a severe focal abnormality in radial DENSE (see Results for details).
Figure 4.
Patient with extensive systolic intramural strain abnormality despite minimal late gadolinium gadolinium enhancement (see Results for details).
An example that supports the concept that myocardium with confluent LGE does not contract normally in HCM is shown in Figure 1. This patient has a confluent abnormality of LGE in the inferior septum which corresponds to a severe focal abnormality in systolic strain as represented by the blue and purple patches corresponding to less than 10% circumferential shortening and radial thickening. Note that the signal intensity on the LGE is similar to what is typically observed in patients with myocardial infarction due to coronary artery disease (i.e. the myocardial enhanced zone and the left ventricular blood pool present with similar signal intensity) except that the abnormality is not located in the subendocardium.
Diffusely enhancing myocardium also does not contract in HCM (Figure 2). In this example, a diffuse pattern of LGE, which corresponds to a severe intramural strain abnormality on color-coded DENSE, can be seen in the anterior wall and anteroseptum. The myocardial signal intensity in the late gadolinium enhanced zone is much lower than in cases with confluent LGE. The DENSE CS and RT maps show normal strain (orange to white) in the septum, inferior and lateral walls as well as in the inner 1/3 of the anterior and anteroseptal segments. Thus, there is a substantial amount of myocardium in all segments with normal strain and a zone of very low strain in the outer half of the segment with diffuse gadolinium enhancement. Cine MRI showed normal systolic endocardial excursion and ejection fraction in this patient but could not assess intramural function.
Figure 2.
The diffuse pattern of late gadolinium enhancement seen in the anterior septum matches the contractile abnormality seen with DENSE (see Results for details).
Intramural functional abnormalities can be more extensive than predicted by the extent of LGE. Figure 3 shows a patient with more severe septal hypertrophy but a similar sized abnormality of confluent LGE to the one seen in Figure 1. Despite severely depressed strain in the two thirds of the septum near the right ventricle, DENSE maps of intramural strain again showed a nearly circumferential inner ring of largely normal contraction. The amount of myocardium with normal strain (orange-white) is comparable in all segments around this short axis slice despite large functional abnormalities in the remainder of the septum. Systolic strain in this patient is more heterogeneous than LGE would predict. Cine MRI shows global systolic function (corresponding to an EF of 64%) that almost obliterates the mid left ventricular cavity.
Figure 3.
Patient where the systolic strain deficit extends well beyond the two clearly defined confluent lesions on the late gadolinium enhanced images (see Results for details).
Intramural functional abnormalities in HCM also exist in the absence of significant LGE. Figure 4 shows an example where the DENSE maps of intramural strain show two large distinct contractile abnormalities (purple to blue/black patches) separated by a zone of nearly normally contracting myocardium in the mid-septum. In this patient, there is only a small region of confluent LGE within the inferoseptum. Cine MRI showed hyperdynamic global systolic function in this patient.
The examples shown in Figures 2–4 indicate that reduced contractile function is not necessarily associated with LGE. In most of the patients (17 out of 22) the LGE was not localized to the inner third of the heart consistent with viable myocardium in the regions where strain appeared normal in most of these patients (Table 1).
Heterogeneous Intramural Function Irrespective of Pattern or Presence of Enhancement
Intramural function by DENSE was not only depressed within areas of both confluent and diffuse LGE but also at the core of the most hypertrophic non-enhanced segment (Figure 5). Specifically, CS was significantly reduced within the confluent late gadolinium enhanced regions compared to a normal remote non-enhanced non-hypertrophic region (6.1±1.6 vs. 20.4±1.8% CS respectively, p<0.001). Diffuse late gadolinium enhanced regions exhibited disproportionally reduced intramural CS compared to a normal remote non-enhanced non-hypertrophic region (7.5±0.9 vs. 18.4.8±2.1% CS respectively, p<0.001). Interestingly, the most hypertrophic non-enhanced segment also had significantly reduced intramural strain when compared to a normal remote non-enhanced non-hypertrophic region (9.3±1.5 vs. 19.1±2.2% CS respectively, p<0.001). Radial thickening DENSE data showed similar results (confluent enhancement 7.6±1.3 vs. normal 29.5±1.3%, p<0.001; diffuse enhancement 9.1±0.9 vs. normal 23.4±1.9%, p<0.001; most hypertrophic non-enhanced 9.5±1.2 vs. normal 28.3±1.4%, p<0.001).
Figure 5.
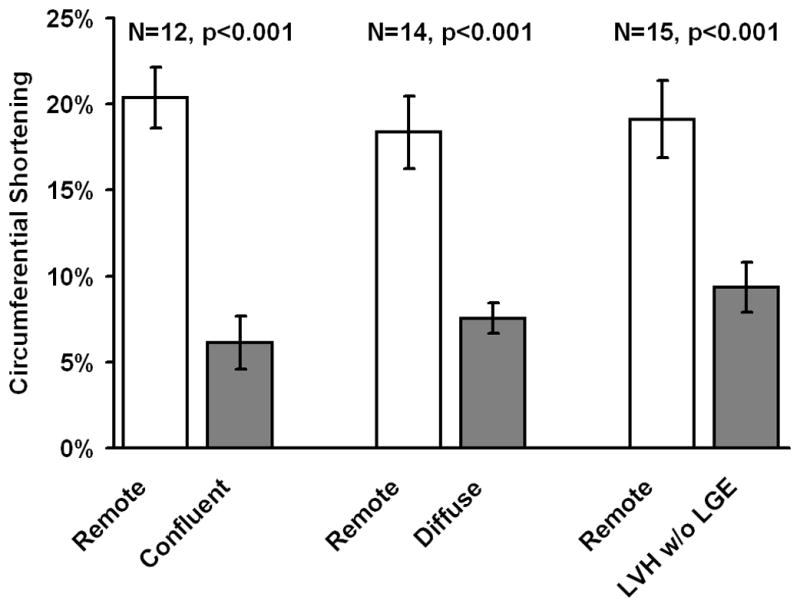
Abnormal systolic strain is seen not only in areas of confluent and diffuse late gadolinium enhancement but also in the most hypertrophic non-enhanced segment. Intramural function is reduced irrespective of type or presence of late gadolinium enhancement pattern in hypertrophic segments indicating that myocardial scarring and interstitial fibrosis cannot predict the entire spectrum of functional abnormalities.
On late gadolinium enhanced images, the signal intensity was significantly different for confluent and diffusely enhancing versus normal myocardium (Figure 6, both p<0.001). The signal intensity in the most hypertrophic non-enhancing myocardium was not significantly different than normal myocardium, an important control measurement that indicates the qualitative characterization of amount of gadolinium in these regions was not simply due to the way the images were displayed.
Figure 6.
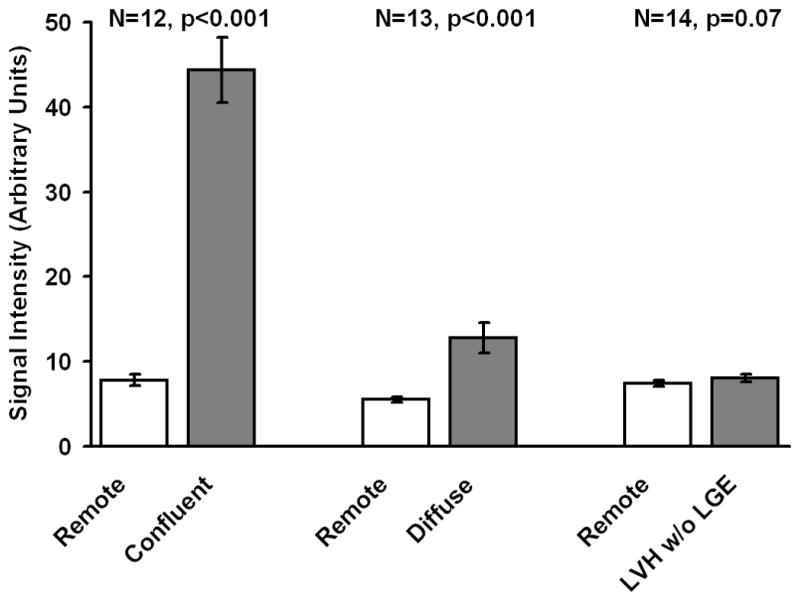
Signal intensities in late gadolinium enhancement images varied depending on presence and type of late gadolinium enhancement. Confluent and diffuse patterns had significantly higher signal intensity than normal myocardium. The signal intensity in the most hypertrophic non-enhancing segment was not significantly different from that of normal myocardium.
Preserved Absolute Wall Thickening and Inner wall Contractile Function
DENSE intramural contractile function demonstrated a complete circumferential inner rim of largely normal contracting myocardium in 77% of the patients (17 out of 22). This group of patients had on average a normal ejection fraction (66.8%±4.3). Predominantly transmural hypokinesis in the hypertrophic zone was observed in 2 out of 22 patients. These two patients had reduced ejection fractions (<55%). The remaining 3 out of 22 patients presented with a mixture of both patterns of intramural contractile function within the hypertrophic zones (ejection fraction 67.7%±5.8). Thus, 91% of patients had a complete or significant amount of myocardium with normal strain in the inner layers of the left ventricle.
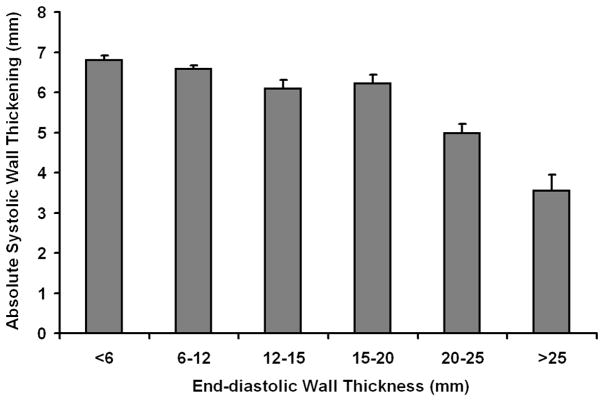
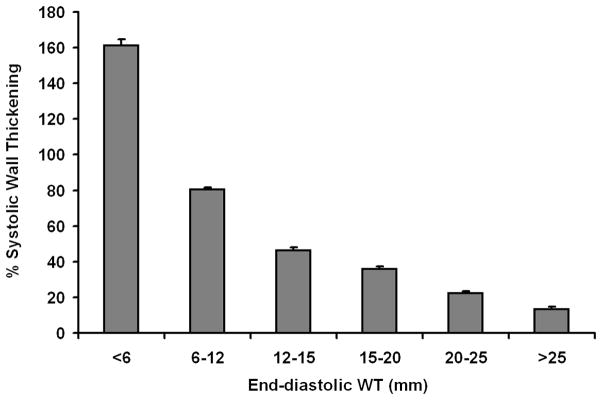
Absolute systolic wall thickening by CINE MRI was overall preserved in these HCM patients (Figure 7A). In particular, absolute systolic wall thickening averaged more than 6 mm even with an end-diastolic wall thickness of 20 mm. Even the most hypertrophic segments (end-diastolic thickness greater than 25 mm) exhibited normal absolute systolic wall thickening defined as >3 mm 24. On average, more than 5 mm of absolute systolic wall thickening was observed by CINE MRI for both hypertrophic and non-hypertrophic segments independent of the extent of LGE. These findings of overall preserved absolute systolic wall thickening are concordant with the observed preserved ejection fractions (Table 2). Conversely, a normal ejection fraction or significant regional wall thickening did not preclude large patches of severely depressed intramural systolic function.
Figure 7.
Left panel 7A: Irrespective of segmental end-diastolic thickness, the myocardium exhibits on average more than 3 mm absolute systolic change in wall thickness. Note that excluding the most hypertrophic segments, absolute systolic change in wall thickness is on average more than 6 mm. In normal subjects, >3 mm represents normal absolute systolic change in wall thickness. Right panel 7B: With increasing end-diastolic thickness the myocardium exhibits reduced percent systolic wall thickening, which is a measure of transmural systolic strain. This seems paradoxical given that these patients have preserved ejection fractions and fairly extensive left ventricular hypertrophy.
(Sample size per category was <6:572, 6–12:1272, 12–15:327, 15–20:449, 20–25:306, >25:134)
Table 2.
CMR findings
| Patient | Max WTh (mm) | LGE (% of LV) | LGE patterns | Strain patterns | LVEF (%) | LV Mass (g) |
|---|---|---|---|---|---|---|
| 1 | 17 | 13.0 | Confluent | Both | 65 | 107 |
| 2 | 28 | 5.1 | Confluent | Endo | 63 | 567 |
| 3 | 25 | 8.1 | Diffuse | Endo | 67 | 179 |
| 4 | 23 | 9.9 | Diffuse | Trans | 55 | 240 |
| 5 | 24 | 3.8 | Diffuse | Endo | 73 | 111 |
| 6 | 22 | 4.3 | Diffuse | Endo | 67 | 129 |
| 7 | 25 | 10.5 | Both | Both | 64 | 107 |
| 8 | 21 | 12.3 | Both | Endo | 61 | 192 |
| 9 | 20 | 5.8 | Confluent | Both | 74 | 136 |
| 10 | 28 | 2.2 | Diffuse | Endo | 68 | 190 |
| 11 | 28 | 5.8 | Diffuse | Endo | 72 | 161 |
| 12 | 33 | 14.6 | Confluent | Endo | 64 | 219 |
| 13 | 27 | 11.1 | Diffuse | Endo | 59 | 207 |
| 14 | 28 | 2.2 | Diffuse | Endo | 65 | 267 |
| 15 | 22 | 4.6 | Confluent | Endo | 73 | 144 |
| 16 | 34 | 5.5 | Both | Endo | 73 | 367 |
| 17 | 33 | 3.5 | Diffuse | Endo | 66 | 263 |
| 18 | 25 | 17.9 | Both | Endo | 68 | 135 |
| 19 | 25 | 3.5 | Confluent | Endo | 65 | 213 |
| 20 | 17 | 12.5 | Confluent | Endo | 62 | 76 |
| 21 | 24 | 41.5 | Confluent | Trans | 53 | 224 |
| 22 | 21 | 1.8 | Diffuse | Endo | 70 | 167 |
LV = Left Ventricle; Max WTh = Maximum Wall Thickening; LGE = Late Gadolinium Enhancement; LVEF = Left Ventricular Ejection Fraction, Endo=endocardial, Trans=transmural.
On average, percent systolic wall thickening (Figure 7B) was inversely related to end-diastolic wall thickness suggesting that transmural contractile function in the most hypertrophic myocardial segments is very low.
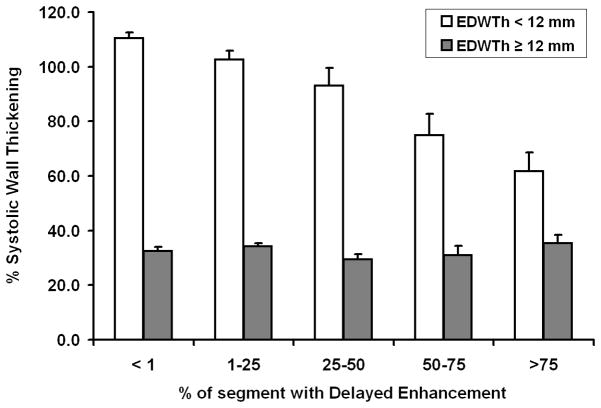
In non-hypertrophic segments (Figure 8, EDWth < 12 mm), percent wall thickening was inversely related to increasing extent of segment LGE. In hypertrophic segments (Figure 8, EDWth >=12 mm), percent wall thickening was low irrespective of extent of LGE.
Figure 8.
Gadolinium delayed enhancement does not fully explain the observed functional abnormalities. For segments with end-diastolic wall thickness (EDWTh) < 12mm percent wall thickening was inversely proportional to the extent of delayed enhancement. However, for segments with EDWTh ≥ 12mm, transmural percent wall thickening was depressed irrespective of the extent of gadolinium delayed enhancement.
Discussion
The DENSE systolic strain maps show heterogeneous myocardial function in HCM which requires a heterogeneous mechanism rather than a diffuse or global process. LGE predicts some but not all of the heterogeneity of intramural contractile abnormalities. Since LGE is a highly sensitive method 11, 25, myocardial scar and excess collagen deposition cannot explain the spectrum of heterogeneous intramural function encountered in HCM. Myofiber disarray is one mechanism that could impair function without showing abnormalities on late enhancement images4. The frequently observed pattern of an inner ring of normal intramural strain provides a mechanism that can explain preserved global left ventricular function despite severe strain abnormalities in the remainder of that segment. That observation could not be predicted by “uniform models” or assumptions about cardiac contraction. There are several factors that lead to heterogeneity of intramural function in patients with HCM and most of these mechanisms cannot be visualized with transmural or low resolution methods. Thus, the ability to spatially register high resolution strain maps with LGE images allows interrogation of the relationships between function and myocardial scar/collagen at an unprecedented level.
Histopathological studies have identified more than one kind of intramural heterogeneity in HCM that could relate to contractile abnormalities. Sarcomeric disarray is highly heterogeneous 26, 27 and not even confined within hypertrophic segments 26. Sarcomeric hypertrophy occurs in the endocardium and the mid-wall 28, 29. Diffuse interstitial fibrosis and myocardial scarring are common in HCM 28, 30, 31. Moreover, a high fraction of young patients with HCM but no coronary artery disease have patchy signs of acute-subacute ischemia postmortem 31.
At a clinical level, HCM is characterized by many types of heterogeneous abnormalities. Resting myocardial blood flow is heterogeneous despite metabolic demands similar to that of normal myocardium 32 and is related to LGE 10. Multi-focal patterns of LGE have also been identified in asymptomatic and mildly symptomatic HCM patients 23. These patterns, which may represent infarction, fibrosis, or excess collagen deposition 33, 34, were later correlated with progressive dilation of the ventricle and risk of sudden death 21.
Characterization of intramural left ventricular strain based on simple geometrical models does not apply in HCM since the assumption of a homogeneously contracting medium is not valid. Based on such models, there is a largely linear endocardial to epicardial gradient of circumferential strain and HCM 35. Pioneering myocardial tagging studies may have masked the intramural strain heterogeneity due to the coarse spatial resolution (tag spacing of 7mm) 35. Other MRI tagging studies in patients with HCM have previously reported abnormal contractile function in the left ventricle. Both radial displacement 36 and circumferential shortening are reduced in the septum 37. Similar results were also obtained for total systolic strain recently with methods that allow full cardiac cycle interrogations 38 whereas diastolic strain was reduced in all segments.
Late gadolinium enhancement is not as closely linked to the full range of contractile abnormalities detected in HCM whereas in coronary artery disease regional function varies inversely with the transmural extent of gadolinium delayed enhancement 20. In patients with HCM, the extent of delayed enhancement is inversely related to systolic segmental percent wall thickening 23. While the current study also found an inverse relationship between percent wall thickening and the extent of LGE, this only applied to the less severely hypertrophic segments (Figure 8). In the thickest regions of the heart, transmural systolic contraction was independent of the extent of LGE (Figure 8). While not addressed by this dataset, myocardial edema or inflammation may also explain the discrepancy between regional contractile function and LGE 39, 40.
The DENSE MRI acquisition has many advantages in producing cardiac strain measurements. DENSE has been used to measure post-infarct recovery of function 41. Myocardial tagging 42, harmonic phase image processing 43 and DENSE have yield comparable strain measurements 43–46 and have been recently shown to rely on the same physics for mapping motion 47. As implemented in this study, DENSE provided approximately 250 measurements of intramural contractile function per short axis slice -- an order of magnitude more measurements than conventional tagged MRI. Therefore, fitting the strain measurements to a predetermined model of the heart 48 was not necessary -- a significant advantage for the irregularly shaped heart in patients with HCM. Since a volumetric preparation is used to sensitize the image to motion, the method intrinsically avoids through-plane motion artifacts.
Regional wall motion assessment by cine MRI and echocardiography can potentially be misleading depending on whether one chooses to report percent wall thickening (i.e. transmural strain) or absolute systolic change in wall thickness (in mm). Percent wall thickening is inversely proportional to end diastolic wall thickness yet the average amount of wall thickening in mm remains normal or hypercontractile in the same hearts. However, the greatest hazard of interpreting percent wall thickening data is the extrapolation to infer the mechanisms leading to abnormalities in regional contractile function in HCM. High-resolution images of intramural systolic function can properly address this issue. The fact that LGE and intramural strain show abnormalities with different spatial distributions suggests that the information may be complementary. Larger studies will need to be performed to determine the prognostic significance of these findings.
Limitations
The current data do not address right ventricular involvement specifically since it was not possible to delineate the RV-LV border within the septum. Multi-slice analysis with appropriate statistical methods to correct for data dependence could have provided insight into intra-subject heterogeneity. However, single slice analysis was favored both for simplicity sake and for preserving the statistical significance lever, which degrades by testing multiple hypotheses (e.g. through the use of the Bonferroni correction). LGE images were acquired during diastole while DENSE images during systole. Despite all efforts to properly place the relevant regions of interest, some partial volume averaging may have influenced the results. Further histopathological studies are needed to shed light on how abnormalities by DENSE may indicate diffuse, interstitial fibrosis in visually-negative LGE regions.
Conclusions
In conclusion, just as high resolution LGE images allowed intramural assessments of myocardial infarction and fibrosis, high-resolution DENSE strain maps provide the most detailed view of intramural function obtained to date in patients with HCM. These results show that LGE as a measure of myocardial fibrosis does not fully explain the observed contractile heterogeneity in these patients. Direct visualization of an inner rim of preserved strain in the endocardium and mid-wall along with otherwise hypokinetic regions is a contractile pattern unique to HCM that has not been previously visualized with other methods.
Acknowledgments
Sources of Funding
This study was supported by the Intramural Research Program of the National Heart, Lung and Blood Institute at the National Institutes of Health.
Footnotes
Disclosures
None.
References
- 1.Hansen MW, Merchant N. Mri of hypertrophic cardiomyopathy: Part 2, differential diagnosis, risk stratification, and posttreatment mri appearances. AJR Am J Roentgenol. 2007;189:1344–1352. doi: 10.2214/AJR.07.2287. [DOI] [PubMed] [Google Scholar]
- 2.Hansen MW, Merchant N. Mri of hypertrophic cardiomyopathy: Part i, mri appearances. AJR Am J Roentgenol. 2007;189:1335–1343. doi: 10.2214/AJR.07.2286. [DOI] [PubMed] [Google Scholar]
- 3.Shirani J, Pick R, Roberts WC, Maron BJ. Morphology and significance of the left ventricular collagen network in young patients with hypertrophic cardiomyopathy and sudden cardiac death. J Am Coll Cardiol. 2000;35:36–44. doi: 10.1016/s0735-1097(99)00492-1. [DOI] [PubMed] [Google Scholar]
- 4.Tseng WY, Dou J, Reese TG, Wedeen VJ. Imaging myocardial fiber disarray and intramural strain hypokinesis in hypertrophic cardiomyopathy with mri. J Magn Reson Imaging. 2006;23:1–8. doi: 10.1002/jmri.20473. [DOI] [PubMed] [Google Scholar]
- 5.Weber KT. Targeting pathological remodeling: Concepts of cardioprotection and reparation. Circulation. 2000;102:1342–1345. doi: 10.1161/01.cir.102.12.1342. [DOI] [PubMed] [Google Scholar]
- 6.Kitamura M, Shimizu M, Ino H, Okeie K, Yamaguchi M, Funjno N, Mabuchi H, Nakanishi I. Collagen remodeling and cardiac dysfunction in patients with hypertrophic cardiomyopathy: The significance of type iii and vi collagens. Clin Cardiol. 2001;24:325–329. doi: 10.1002/clc.4960240413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Spirito P, Bellone P, Harris KM, Bernabo P, Bruzzi P, Maron BJ. Magnitude of left ventricular hypertrophy and risk of sudden death in hypertrophic cardiomyopathy. N Engl J Med. 2000;342:1778–1785. doi: 10.1056/NEJM200006153422403. [DOI] [PubMed] [Google Scholar]
- 8.Dumont CA, Monserrat L, Soler R, Rodriguez E, Fernandez X, Peteiro J, Bouzas B, Pinon P, Castro-Beiras A. [clinical significance of late gadolinium enhancement on cardiovascular magnetic resonance in patients with hypertrophic cardiomyopathy] Rev Esp Cardiol. 2007;60:15–23. [PubMed] [Google Scholar]
- 9.Soler R, Rodriguez E, Monserrat L, Mendez C, Martinez C. Magnetic resonance imaging of delayed enhancement in hypertrophic cardiomyopathy: Relationship with left ventricular perfusion and contractile function. J Comput Assist Tomogr. 2006;30:412–420. doi: 10.1097/00004728-200605000-00011. [DOI] [PubMed] [Google Scholar]
- 10.Knaapen P, van Dockum WG, Gotte MJ, Broeze KA, Kuijer JP, Zwanenburg JJ, Marcus JT, Kok WE, van Rossum AC, Lammertsma AA, Visser FC. Regional heterogeneity of resting perfusion in hypertrophic cardiomyopathy is related to delayed contrast enhancement but not to systolic function: A pet and mri study. J Nucl Cardiol. 2006;13:660–667. doi: 10.1016/j.nuclcard.2006.05.018. [DOI] [PubMed] [Google Scholar]
- 11.Kim RJ, Wu E, Rafael A, Chen EL, Parker MA, Simonetti O, Klocke FJ, Bonow RO, Judd RM. The use of contrast-enhanced magnetic resonance imaging to identify reversible myocardial dysfunction. N Engl J Med. 2000;343:1445–1453. doi: 10.1056/NEJM200011163432003. [DOI] [PubMed] [Google Scholar]
- 12.Lim DS, Lutucuta S, Bachireddy P, Youker K, Evans A, Entman M, Roberts R, Marian AJ. Angiotensin ii blockade reverses myocardial fibrosis in a transgenic mouse model of human hypertrophic cardiomyopathy. Circulation. 2001;103:789–791. doi: 10.1161/01.cir.103.6.789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carasso S, Rakowski H. Myocardial fibrosis and regional function in hypertrophic cardiomyopathy: May the force be with you. J Am Soc Echocardiogr. 2008;21:1306–1308. doi: 10.1016/j.echo.2008.10.009. [DOI] [PubMed] [Google Scholar]
- 14.Carasso S, Yang H, Woo A, Vannan MA, Jamorski M, Wigle ED, Rakowski H. Systolic myocardial mechanics in hypertrophic cardiomyopathy: Novel concepts and implications for clinical status. J Am Soc Echocardiogr. 2008;21:675–683. doi: 10.1016/j.echo.2007.10.021. [DOI] [PubMed] [Google Scholar]
- 15.Nagueh SF, McFalls J, Meyer D, Hill R, Zoghbi WA, Tam JW, Quinones MA, Roberts R, Marian AJ. Tissue doppler imaging predicts the development of hypertrophic cardiomyopathy in subjects with subclinical disease. Circulation. 2003;108:395–398. doi: 10.1161/01.CIR.0000084500.72232.8D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ashrafian H, Redwood C, Blair E, Watkins H. Hypertrophic cardiomyopathy:A paradigm for myocardial energy depletion. Trends Genet. 2003;19:263–268. doi: 10.1016/S0168-9525(03)00081-7. [DOI] [PubMed] [Google Scholar]
- 17.Popovic ZB, Kwon DH, Mishra M, Buakhamsri A, Greenberg NL, Thamilarasan M, Flamm SD, Thomas JD, Lever HM, Desai MY. Association between regional ventricular function and myocardial fibrosis in hypertrophic cardiomyopathy assessed by speckle tracking echocardiography and delayed hyperenhancement magnetic resonance imaging. J Am Soc Echocardiogr. 2008;21:1299–1305. doi: 10.1016/j.echo.2008.09.011. [DOI] [PubMed] [Google Scholar]
- 18.Aletras AH, Ding S, Balaban RS, Wen H. Dense: Displacement encoding with stimulated echoes in cardiac functional mri. J Magn Reson. 1999;137:247–252. doi: 10.1006/jmre.1998.1676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aletras AH, Wen H. Mixed echo train acquisition displacement encoding with stimulated echoes: An optimized dense method for in vivo functional imaging of the human heart. Magn Reson Med. 2001;46:523–534. doi: 10.1002/mrm.1223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim RJ, Fieno DS, Parrish TB, Harris K, Chen EL, Simonetti O, Bundy J, Finn JP, Klocke FJ, Judd RM. Relationship of mri delayed contrast enhancement to irreversible injury, infarct age, and contractile function. Circulation. 1999;100:1992–2002. doi: 10.1161/01.cir.100.19.1992. [DOI] [PubMed] [Google Scholar]
- 21.Moon JC, McKenna WJ, McCrohon JA, Elliott PM, Smith GC, Pennell DJ. Toward clinical risk assessment in hypertrophic cardiomyopathy with gadolinium cardiovascular magnetic resonance. J Am Coll Cardiol. 2003;41:1561–1567. doi: 10.1016/s0735-1097(03)00189-x. [DOI] [PubMed] [Google Scholar]
- 22.Aletras AH, Arai AE. Meta-dense complex acquisition for reduced intravoxel dephasing. J Magn Reson. 2004;169:246–249. doi: 10.1016/j.jmr.2004.05.008. [DOI] [PubMed] [Google Scholar]
- 23.Choudhury L, Mahrholdt H, Wagner A, Choi KM, Elliott MD, Klocke FJ, Bonow RO, Judd RM, Kim RJ. Myocardial scarring in asymptomatic or mildly symptomatic patients with hypertrophic cardiomyopathy. J Am Coll Cardiol. 2002;40:2156–2164. doi: 10.1016/s0735-1097(02)02602-5. [DOI] [PubMed] [Google Scholar]
- 24.Kwong RY, Schussheim AE, Rekhraj S, Aletras AH, Geller N, Davis J, Christian TF, Balaban RS, Arai AE. Detecting acute coronary syndrome in the emergency department with cardiac magnetic resonance imaging. Circulation. 2003;107:531–537. doi: 10.1161/01.cir.0000047527.11221.29. [DOI] [PubMed] [Google Scholar]
- 25.Ricciardi MJ, Wu E, Davidson CJ, Choi KM, Klocke FJ, Bonow RO, Judd RM, Kim RJ. Visualization of discrete microinfarction after percutaneous coronary intervention associated with mild creatine kinase-mb elevation. Circulation. 2001;103:2780–2783. doi: 10.1161/hc2301.092121. [DOI] [PubMed] [Google Scholar]
- 26.Maron BJ, Roberts WC. Quantitative analysis of cardiac muscle cell disorganization in the ventricular septum of patients with hypertrophic cardiomyopathy. Circulation. 1979;59:689–706. doi: 10.1161/01.cir.59.4.689. [DOI] [PubMed] [Google Scholar]
- 27.Kuribayashi T, Roberts WC. Myocardial disarray at junction of ventricular septum and left and right ventricular free walls in hypertrophic cardiomyopathy. Am J Cardiol. 1992;70:1333–1340. doi: 10.1016/0002-9149(92)90771-p. [DOI] [PubMed] [Google Scholar]
- 28.Unverferth DV, Baker PB, Pearce LI, Lautman J, Roberts WC. Regional myocyte hypertrophy and increased interstitial myocardial fibrosis in hypertrophic cardiomyopathy. Am J Cardiol. 1987;59:932–936. doi: 10.1016/0002-9149(87)91128-3. [DOI] [PubMed] [Google Scholar]
- 29.Hoshino T, Fujiwara H, Kawai C, Hamashima Y. Myocardial fiber diameter and regional distribution in the ventricular wall of normal adult hearts, hypertensive hearts and hearts with hypertrophic cardiomyopathy. Circulation. 1983;67:1109–1116. doi: 10.1161/01.cir.67.5.1109. [DOI] [PubMed] [Google Scholar]
- 30.Factor SM, Butany J, Sole MJ, Wigle ED, Williams WC, Rojkind M. Pathologic fibrosis and matrix connective tissue in the subaortic myocardium of patients with hypertrophic cardiomyopathy. J Am Coll Cardiol. 1991;17:1343–1351. doi: 10.1016/s0735-1097(10)80145-7. [DOI] [PubMed] [Google Scholar]
- 31.Basso C, Thiene G, Corrado D, Buja G, Melacini P, Nava A. Hypertrophic cardiomyopathy and sudden death in the young: Pathologic evidence of myocardial ischemia. Hum Pathol. 2000;31:988–998. doi: 10.1053/hupa.2000.16659. [DOI] [PubMed] [Google Scholar]
- 32.Nienaber CA, Gambhir SS, Mody FV, Ratib O, Huang SC, Phelps ME, Schelbert HR. Regional myocardial blood flow and glucose utilization in symptomatic patients with hypertrophic cardiomyopathy. Circulation. 1993;87:1580–1590. doi: 10.1161/01.cir.87.5.1580. [DOI] [PubMed] [Google Scholar]
- 33.Tanaka M, Fujiwara H, Onodera T, Wu DJ, Hamashima Y, Kawai C. Quantitative analysis of myocardial fibrosis in normals, hypertensive hearts, and hypertrophic cardiomyopathy. Br Heart J. 1986;55:575–581. doi: 10.1136/hrt.55.6.575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lombardi R, Betocchi S, Losi MA, Tocchetti CG, Aversa M, Miranda M, D’Alessandro G, Cacace A, Ciampi Q, Chiariello M. Myocardial collagen turnover in hypertrophic cardiomyopathy. Circulation. 2003;108:1455–1460. doi: 10.1161/01.CIR.0000090687.97972.10. [DOI] [PubMed] [Google Scholar]
- 35.Kramer CM, Reichek N, Ferrari VA, Theobald T, Dawson J, Axel L. Regional heterogeneity of function in hypertrophic cardiomyopathy. Circulation. 1994;90:186–194. doi: 10.1161/01.cir.90.1.186. [DOI] [PubMed] [Google Scholar]
- 36.Maier SE, Fischer SE, McKinnon GC, Hess OM, Krayenbuehl HP, Boesiger P. Evaluation of left ventricular segmental wall motion in hypertrophic cardiomyopathy with myocardial tagging. Circulation. 1992;86:1919–1928. doi: 10.1161/01.cir.86.6.1919. [DOI] [PubMed] [Google Scholar]
- 37.Young AA, Kramer CM, Ferrari VA, Axel L, Reichek N. Three-dimensional left ventricular deformation in hypertrophic cardiomyopathy. Circulation. 1994;90:854–867. doi: 10.1161/01.cir.90.2.854. [DOI] [PubMed] [Google Scholar]
- 38.Ennis DB, Epstein FH, Kellman P, Fananapazir L, McVeigh ER, Arai AE. Assessment of regional systolic and diastolic dysfunction in familial hypertrophic cardiomyopathy using mr tagging. Magn Reson Med. 2003;50:638–642. doi: 10.1002/mrm.10543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Knaapen P, van Dockum WG, Bondarenko O, Kok WE, Gotte MJ, Boellaard R, Beek AM, Visser CA, van Rossum AC, Lammertsma AA, Visser FC. Delayed contrast enhancement and perfusable tissue index in hypertrophic cardiomyopathy: Comparison between cardiac mri and pet. J Nucl Med. 2005;46:923–929. [PubMed] [Google Scholar]
- 40.Abdel-Aty H, Cocker M, Strohm O, Filipchuk N, Friedrich MG. Abnormalities in t2-weighted cardiovascular magnetic resonance images of hypertrophic cardiomyopathy: Regional distribution and relation to late gadolinium enhancement and severity of hypertrophy. J Magn Reson Imaging. 2008;28:242–245. doi: 10.1002/jmri.21381. [DOI] [PubMed] [Google Scholar]
- 41.Aletras AH, Tilak GS, Natanzon A, Hsu LY, Gonzalez FM, Hoyt RF, Jr, Arai AE. Retrospective determination of the area at risk for reperfused acute myocardial infarction with t2-weighted cardiac magnetic resonance imaging: Histopathological and displacement encoding with stimulated echoes (dense) functional validations. Circulation. 2006;113:1865–1870. doi: 10.1161/CIRCULATIONAHA.105.576025. [DOI] [PubMed] [Google Scholar]
- 42.Axel L, Dougherty L. Mr imaging of motion with spatial modulation of magnetization. Radiology. 1989;171:841–845. doi: 10.1148/radiology.171.3.2717762. [DOI] [PubMed] [Google Scholar]
- 43.Osman NF, Kerwin WS, McVeigh ER, Prince JL. Cardiac motion tracking using cine harmonic phase (harp) magnetic resonance imaging. Magn Reson Med. 1999;42:1048–1060. doi: 10.1002/(sici)1522-2594(199912)42:6<1048::aid-mrm9>3.0.co;2-m. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gilson WD, Yang Z, French BA, Epstein FH. Complementary displacement-encoded mri for contrast-enhanced infarct detection and quantification of myocardial function in mice. Magn Reson Med. 2004;51:744–752. doi: 10.1002/mrm.20003. [DOI] [PubMed] [Google Scholar]
- 45.Kim D, Gilson WD, Kramer CM, Epstein FH. Myocardial tissue tracking with two-dimensional cine displacement-encoded mr imaging: Development and initial evaluation. Radiology. 2004;230:862–871. doi: 10.1148/radiol.2303021213. [DOI] [PubMed] [Google Scholar]
- 46.Gilson WD, Yang Z, French BA, Epstein FH. Measurement of myocardial mechanics in mice before and after infarction using multislice displacement-encoded mri with 3d motion encoding. Am J Physiol Heart Circ Physiol. 2005;288:H1491–1497. doi: 10.1152/ajpheart.00632.2004. [DOI] [PubMed] [Google Scholar]
- 47.Kuijer JP, Hofman MB, Zwanenburg JJ, Marcus JT, van Rossum AC, Heethaar RM. Dense and harp: Two views on the same technique of phase-based strain imaging. J Magn Reson Imaging. 2006;24:1432–1438. doi: 10.1002/jmri.20749. [DOI] [PubMed] [Google Scholar]
- 48.Guttman MAZEA, McVeigh E. Analysis of cardiac function from mr images. IEEE Comput Graph Appl. 1997;17:30–38. doi: 10.1109/38.576854. [DOI] [PMC free article] [PubMed] [Google Scholar]