Abstract
BACKGROUND
The 2008 Surviving Sepsis Campaign guidelines state that intravenous antibiotic therapy should be started within the first hour of recognition of septic shock. Currently, there are no published studies looking at antibiotic timing in pediatric sepsis patients.
OBJECTIVES
The purpose of this study is to determine if sepsis patients admitted to a Pediatric Intensive Care Unit (PICU) are administered antibiotics in the appropriate time frame according to the Surviving Sepsis Guidelines.
METHODS
A retrospective chart review was conducted during a six-month time frame. For the purpose of this pilot study the onset of severe sepsis was defined as the time of a physician order for a vasopressor. Antibiotic appropriateness was based on culture results, drug dosing, and route. Length of PICU stay, overall hospital days, and mortality data were collected. Descriptive statistics on patient demographics, and the prescribing and time of administration of both antibiotics and vasopressors are included.
RESULTS
Fifty-four patients were identified, 4 of which were admitted twice during the study period. Fifty admissions did not meet criteria for analysis, with a final sample size of 8 patients identified. All patients were male with an average age of 7.6 years, average weight of 33.4 kg, and zero mortality rate. Eighty-eight percent of the patients were administered appropriate antibiotics. The average time from vasopressor order to the administration of antibiotics was 7 hours and 40 minutes.
CONCLUSIONS
The time delay in administering antibiotics to our pediatric sepsis patients likely involved physicians, nurses, and pharmacists. System improvements are needed to decrease the time delay in providing antibiotics to this patient population. Although our sample size was small, the mortality rate found in this study is lower than what has been reported in adults with sepsis.
Keywords: antibiotics, critical care, pediatrics, sepsis
INTRODUCTION
The International Pediatric Sepsis Consensus Conference in 2005 established definitions for sepsis in the pediatric population.1 The progression to septic shock includes the systemic inflammatory response syndrome (SIRS), sepsis, severe sepsis and septic shock. SIRS is defined as core temperature >38.5°C or <36°C or leukocyte count elevated or depressed for age plus either tachycardia (or bradycardia if less than 1 year of age), or tachypnea (or mechanical ventilation).1 Sepsis is defined as SIRS in the presence of proven or suspected infection.1 Severe sepsis is sepsis plus cardiovascular dysfunction, acute respiratory distress syndrome, or two or more other organ dysfunctions.1 Septic shock is sepsis plus cardiovascular dysfunction.1
It is estimated that severe sepsis affects 42,400 pediatric patients and is responsible for 4,400 deaths each year.2 Severe sepsis accounts for approximately $40,000 of hospital costs and an average length of stay of 31 days per patient. The estimated national cost is 1.97 billion dollars annually.2 The Surviving Sepsis Campaign/International Guidelines for Management of Severe Sepsis and Septic Shock published in 2008 state that “intravenous antibiotic therapy should be started as early as possible and within the first hour of recognition of septic shock.”3
The purpose of this study was to determine if patients with severe sepsis or septic shock in a Pediatric Intensive Care Unit (PICU) were administered antibiotics in the appropriate time frame according to the 2008 Surviving Sepsis Guidelines. Secondary objectives included determination of the appropriateness of initial antibiotic therapy based on culture results, characterization of the relationship between antibiotic timing, PICU length of stay, and overall hospital length of stay, and characterization of the relationship between antibiotic timing and patient mortality.
MATERIALS AND METHODS
A retrospective chart review was conducted of all patients admitted to the PICU between August 1, 2007, and January 31, 2008. For the purpose of this pilot study, the onset of severe sepsis was defined as the time of the physician order for a vasopressor. Although first-line treatment for sepsis includes fluid boluses, vasopressor requirement indicates fluid-refractory sepsis and cardiovascular dysfunction, which can be considered severe sepsis or septic shock.1 Inclusion criteria were those patients diagnosed with the International Statistical Classification of Diseases and Related Health Problems (ICD-9) codes of sepsis.4
Patients with positive fungal cultures, no vasopressor order, vasopressor therapy for reasons other than sepsis (i.e., cardiac surgery), care withdrawn prior to antibiotic administration, incomplete documentation of antibiotic data, and/or those who received antibiotics more than two hours prior to vasopressors were excluded.
Demographic data were collected and included age, sex, weight, date and time of admission to and discharge from both the PICU and the hospital. Each vasopressor ordered, accompanied by the date and time of the physician order and administration of the drug, were recorded. Vasopressors included dopamine, dobutamine, epinephrine, norepinephrine, phenylephrine, and vasopressin. Information related to antibiotic therapy consisted of medication name, route, dose, interval, and date and time of order and of administration. Outside hospital and transport medical records were searched for documentation of antibiotic administration. Antibiotic appropriateness was based on culture results including organism, susceptibility, and culture site, as well as drug dosing and route. Appropriate route of administration was defined as the intravenous route. If the patient had negative cultures, antibiotic choice was deemed appropriate if it included broad spectrum coverage. Culture data from 48 hours before and after each vasopressor order included date and time of culture, site of culture, organism identified, and susceptibilities. Length of PICU stay, overall hospital days, and mortality data was also collected. Institutional Review Board approval was granted and informed consent was deemed unnecessary.
RESULTS
Fifty-four patients with a diagnosis of sepsis based on the included ICD-9 codes were identified. Four of the patients were admitted twice for sepsis during the study period, but only one of these multiple admissions was included. Fifty patient admissions were excluded for the reasons noted in Figure 1. Eight patients met all inclusion and exclusion criteria and were included in the analysis.
Figure 1.
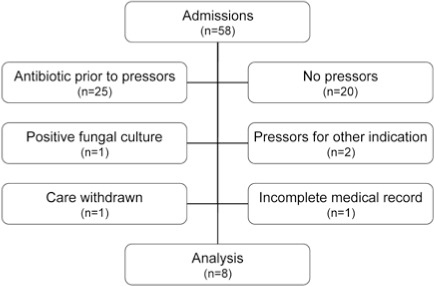
Study patients.
The average age and weight for the 8 patients was 7.6 years (range, 5.0 months to 18.3 years) and 33.4 kilograms (range, 6.3 to 73.0 kg). All patients were male. Antibiotic choices based on culture results were appropriate in 7 of the 8 patients (88%). The inappropriate antibiotic was in a patient who was receiving clindamycin at home, and upon presented to the hospital clindamycin was continued as intravenous therapy. The antibiotic was later changed to broad spectrum coverage with piperacillin/tazobactam.
Five of the eight (63%) patients had positive cultures. One had a positive stool culture for Salmonella enteritidis. Two patients had positive sputum cultures; one for methicillin sensitive Staphylococcus aureus, and one for Pseudomonas aeruginosa in a patient with documented colonization with this organism. Two patients were identified with positive blood cultures for Serratia marcescens and vancomycin sensitive Enterococcus faecalis.
The elapsed time between study points is reviewed in Table. The mean time from onset of sepsis (the original vasopressor order) to antibiotic administration was 7 hours 40 minutes. The mean time from vasopressor order to administration was 49 minutes. The mean difference between vasopressor and antibiotic order time was 1 hour 15 minutes. Although the order for a vasopressor was written 24 minutes before the antibiotic order in one patient, the vasopressor was administered prior to the antibiotic. The mean time from the antibiotic order to its administration was 3 hours 24 minutes. Within that process, the time from antibiotic order to pharmacist verification and production of a label was 33 minutes. None of the patients received antibiotics within 1 hour of vasopressor order (Figure 2).
Table.
Timing of Orders and Administration of Vasopressor and Antibiotics
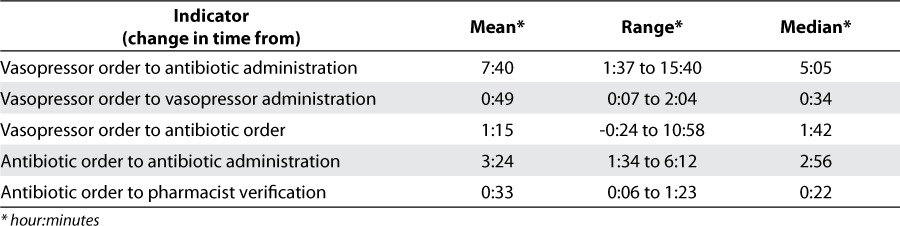
Figure 2.
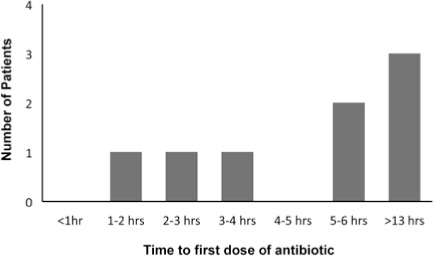
Time to first antibiotic dose administration.
None of the patients died. The mean PICU length of stay was 16 days (range, 1 to 46 days) and mean hospital length of stay was 19 days (range, 2 to 46 days).
DISCUSSION
Although there are no published studies investigating the effect of antibiotic timing in pediatric patients with documented sepsis on outcome, adult data have shown that each hour that antibiotic administration is delayed is associated with an increase in mortality.5 In 2006, Kumar and colleagues conducted a retrospective study of 2,731 adult cases of septic shock.5 The authors demonstrated a link to timing of administration of antibiotics and mortality. If appropriate antibiotics were given within 30 minutes of the onset of hypotension the survival rate was 82.7%; 79.9% if within the first hour; 42.0% if within the first 6 hours, and for each additional hour thereafter, the average decrease in survival was 7.6%.5 If therapy was initiated 36 hours after the onset of hypotension, the odds ratio of death was almost 100%.5 It is interesting to note that 5 patients (63%) in our preliminary study received antibiotics more than 5 hours after the onset of sepsis, but none died. This is inconsistent with the adult published data.
Our study was designed to determine if the mortality and length of PICU/hospital stay would be decreased in patients who received antibiotics within one hour of onset of sepsis. Because none of our patients received antibiotics within the first hour a comparison could not be made.
Our findings are influenced by a combination of the low mortality rate that is normally seen in pediatric patients and our inclusion criteria that resulted in a small sample size. In a 2001 study of almost 4,000 severe sepsis patients, Angus and colleagues found an increasing trend with mortality rate and age. The mortality rate for children was 10% and increased with age to a rate of 20% by age 50 and 38% by 85 years of age or greater.6 We employed a stringent definition for the onset of sepsis (initiation of a vasopressor). This was done to ensure targeting of those patients who were in severe sepsis or septic shock representing the patients with more severe disease. Another limitation of our study resides in the facts that the actual time from the onset of sepsis to recognition and intervention is not known. Based on our definitions, the data may not be reflective of the entire PICU sepsis population.
Our results do show some information about processes in antibiotic administration for pediatric sepsis patients. Appropriate empiric antibiotics were chosen for the majority of patients initially, even based on culture data that was not available at the time of decision making. The time between administration of vasopressors from when the order was written occurs in less time than the administration of antibiotics. There was a delay in physician ordering of antibiotics in this population. There is also a delay in antibiotic administration, which is multifactorial and involves both pharmacy and nursing staff. Our data shows that the delay in pharmacist verification was on average around 30 minutes; the other 3 hours is as yet unexplained. A time study would need to be performed to determine the specific factors associated with the delay in administration of antibiotics.
Based on the preliminary results, we believe that system improvements are needed to insure that antibiotics are given in a timely manner to patients with sepsis. The PICU is serviced by a 24-hour satellite pharmacy located in close proximity to the unit. Once a physician enters an order in the computerized order entry system, it is verified by a pharmacist and a prescription label is produced. After proper preparation and pharmacist check, it is delivered to the unit by hand, or through a pneumatic tube system. Less than one month prior to the beginning of this study, our institution implemented a new electronic computerized practitioner order entry system (CPOE), and time delays may partly be due to unfamiliarity with the new system despite training. To improve this process, plans include changes to both the ordering and the medication administration process. Creation of a pediatric sepsis order set with broad spectrum antibiotics would decrease the time delay in administration of antibiotics as has been shown in adult sepsis patients.7 The antibiotic orders would be designated automatically as STAT in the CPOE system. After pharmacist review of the medication order, select antibiotics stocked in the automated dispensing cabinet would be available to decrease delivery time of antibiotics. Education of physicians, pharmacists, and nurses regarding these improvements and sepsis guidelines would allow for a decrease in time for the entire process.8
CONCLUSIONS
Currently there is room for improvement in the ordering and administration of antibiotics in pediatric sepsis patients to meet the recommendations in the 2008 Surviving Sepsis Guidelines. Our time delay in antibiotic administration is multifactorial and likely involves physician, nurses, and pharmacists. System improvement initiatives are needed to decrease the time delay in providing antibiotics to this patient population. Although our sample size is very small, the mortality rate in this study is lower than what was has been reported in adult patients. Further studies are needed to truly elucidate the pediatric mortality rates in these patients with regards to antibiotic timing in sepsis.
ACKNOWLEDGMENTS
This study was presented at the Pediatric Pharmacy Advocacy Group Neonatal and Pediatric Critical Care Conference in Little Rock, Arkansas in 2008. The authors would like to acknowledge Dr. Danielle Lavallee, Dr. Van Doren Hsu, and Dr. Thomas Dowling for their assistance with this project.
ABBREVIATIONS
- CPOE
computerized practitioner order entry
- PICU
pediatric intensive care unit
- SIRS
systemic inflammatory response syndrome
Footnotes
* hour:minutes
DISCLOSURE The authors declare no conflicts or financial interest in any product or service mentioned in the manuscript, including grants, equipment, medications, employment, gifts, and honoraria. Dr. LaRochelle had full access to data and takes responsibility for the integrity of the data and the accuracy of the data analysis.
REFERENCES
- 1.Goldstein B, Giroir B, Randolph A., the members of the International Consensus Conference on Pediatric Sepsis. International pediatric sepsis consensus conference: Definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med. 2005;6:2–8. doi: 10.1097/01.PCC.0000149131.72248.E6. [DOI] [PubMed] [Google Scholar]
- 2.Watson R, Carcillo J, Linde-Zwirble W. The epidemiology of severe sepsis in children in the United States. Am J Respir Crit Care Med. 2003;167:695–701. doi: 10.1164/rccm.200207-682OC. et al. [DOI] [PubMed] [Google Scholar]
- 3.Dellinger RP, Levy M, Carlet J. Surviving Sepsis Campaign: International guidelines for management of severe sepsis and septic shock. Crit Care Med. 2008;36:296–327. doi: 10.1097/01.CCM.0000298158.12101.41. et al. [DOI] [PubMed] [Google Scholar]
- 4.EICD. Electronic ICD Codes [Internet] Hyattsville, MD: Yaki Technologies; c2004. Available at: http://www.eicd.com. Accessed February 10, 2008. [Google Scholar]
- 5.Kumar A, Roberts D, Wood KA. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med. 2006;34:1589–1596. doi: 10.1097/01.CCM.0000217961.75225.E9. et al. [DOI] [PubMed] [Google Scholar]
- 6.Angus D, Linde-Zwirble W, Lidicker J. Epidemiology of severe sepsis in the United States: Analysis of incidence, outcome and associated costs of care. Crit Care Med. 2001;29:1303–1310. doi: 10.1097/00003246-200107000-00002. et al. [DOI] [PubMed] [Google Scholar]
- 7.Micek S, Roubinian N, Heuring T. Before-after study of a standardized hospital order set for the management of septic shock. Crit Care Med. 2006;34:2707–2713. doi: 10.1097/01.CCM.0000241151.25426.D7. et al. [DOI] [PubMed] [Google Scholar]
- 8.Corey A, Snyder S. Antibiotics in thirty minutes or less for febrile neutropenic patients: A quality control measure in a new hospital. J Pediatr Oncol Nurs. 2008;25:208–212. doi: 10.1177/1043454208319971. [DOI] [PubMed] [Google Scholar]


