Abstract
Background
Geriatric rehabilitation reimbursement increasingly requires documented deficits on standardized measures. Tandem stance performance can characterize balance, but protocols are not standardized.
Objective
The purpose of this study was to explore the impact of: (1) initial support to stabilize in position and (2) maximum hold time on tandem stance tests of balance in older adults.
Design
A cross-sectional secondary analysis of observational cohort data was conducted.
Methods
One hundred seventeen community-dwelling older adults (71% female, 12% black) were assigned to 1 of 3 groups based on the need for initial support to perform tandem stance: (1) unable even with support, (2) able only with support, and (3) able without support. The able without support group was further stratified on hold time in seconds: (1) <10 (low), (2) 10 to 29, (medium), and (3) 30 (high). Groups were compared on primary outcomes (gait speed, Timed “Up & Go” Test performance, and balance confidence) using analysis of variance.
Results
Twelve participants were unable to perform tandem stance, 14 performed tandem stance only with support, and 91 performed tandem stance without support. Compared with the able without support group, the able with support group had statistically or clinically worse performance and balance confidence. No significant differences were found between the able with support group and the unable even with support group on these same measures. Extending the hold time to 30 seconds in a protocol without initial support eliminated ceiling effects for 16% of the study sample.
Limitations
Small comparison groups, use of a secondary analysis, and lack of generalizability of results were limitations of the study.
Conclusions
Requiring initial support to stabilize in tandem stance appears to reflect meaningful deficits in balance-related mobility measures, so failing to consider support may inflate balance estimates and confound hold time comparisons. Additionally, 10-second maximum hold times limit discrimination of balance in adults with a higher level of function. For community-dwelling older adults, we recommend timing for at least 30 seconds and documenting initial support for consideration when interpreting performance.
Reimbursement in geriatric rehabilitation increasingly requires documented deficits on standardized tests of balance and mobility.1,2 In acute care hospital and home health settings, requirements for time, equipment, or open floor space may limit the feasibility of some balance tests. Simple tests that can reveal deficits and predict functional outcomes, including falls, may be preferred in these venues.1,3 Although not a replacement for a more comprehensive functional assessment, tandem stance tests and other brief balance tests traditionally classified as “static” can supplement assessment when screening for deficits.4–6 However, can relative performance on tandem stance tests distinguish among older adults based on meaningful differences in everyday balance-related mobility skills such as walking, and do we sacrifice interpretative power when the “rules” of the test are not standardized?
Holding a heel-to-toe or “tandem” position tests lateral postural stability by narrowing the base of support, and impaired lateral stability is thought to be a key factor in falls among older adults.7–9 In addition to stand-alone administration,5 tandem stance is 1 of 3 positions comprising the Short Physical Performance Battery (SPPB) balance scale10 and is included in the Berg Balance Scale,11 the Clinical Gait and Balance Scale,12 and the Frailty and Injuries: Cooperative Studies of Intervention Techniques (FICSIT)–4 scale.13 Although the rules of SPPB tandem stance administration are well defined and available to clinicians and researchers,14 not all tandem stance tests are so clearly protocolized, challenging replication in clinical or research settings. Among protocols that are described,11,12,15–18 key features may be omitted, and consistency across protocols is rare. Even positioning of the feet can vary: some protocols require the heel and toe to touch in tandem stance,10,16,17 whereas others allow space between the feet.11 Another point of variation is the provision of support to attain the tandem position before timing is begun. Some protocols specify that no support be allowed,18 whereas others allow assistance ranging from light support at one arm10 to holding furniture until steady in position.4,19 In rare cases, the need for assistance is taken into consideration by lowering the score obtained.11
Although rarely factored into the performance score, the need for support could have interpretive value. Jonsson et al15 analyzed ground reaction forces and ankle muscle activity during 30-second tandem stance in active young and older adults who were healthy. Two phases were identified in both age groups: (1) a dynamic “postural adjusting” phase (3–4 seconds), when balance is most challenged, and (2) a static phase thought to represent the “muscle strength and endurance component” of tandem stance. The authors concluded that the ability to attain the position and hold it for the first few seconds is a better measure of balance than total hold time.
An emphasis on this initial “dynamic” component of the tandem stance task—attaining and stabilizing in the position with or without support—highlights the importance of postural strategies previously described as postural preparations, accompaniments or anticipatory adjustments, and responses.20,21 In voluntary stepping, mediolateral anticipatory adjustments shift the body's center of mass toward the weight-bearing limb, even before the contralateral foot is lifted off of the floor, thus preventing a lateral fall.9 From a broader perspective, the transition from self-selected bipedal stance into a dynamic unilateral position en route to full tandem stance would utilize both feedforward and feedback control mechanisms such as those long supported in the postural control literature.22–26 The implications of providing upper-limb support on these postural strategies should not be overlooked, as reaching for support is indeed its own strategy, termed a “postural preparation.”20 We question the validity of comparing tandem stance hold times across individuals who did and did not require initial support to attain the position. Even when considering only individual performance as part of clinical decision making, providing upper-limb support could inflate the hold time and lead to inaccurate characterization of ability, including failure to recognize subtle deficits.
Ultimately, balance performance when measured as tandem stance hold time is limited by the maximum or “cap” for a given protocol. This cap varies from 5 to 60 seconds, but is commonly 10 or 30 seconds.10,11,13,15,27,28 Although one report suggests increased fall risk in those who cannot hold the tandem stance position for 10 seconds,13 other preliminary work suggests a higher cut-point in adults with diabetic peripheral neuropathy,19 and large epidemiologic studies have extended hold times to capture higher-level function in older adults.28 Just as clinical observation of balance function across individuals reveals a continuum of ability, fall risk may be better represented as a gradient along a range of scores than as a single dichotomous cutoff.29 With limited time for screening, testing tandem stance for only 10 seconds is appealing, but do some individuals with “ceiling” performance actually have deficits that warrant further evaluation for rehabilitation services? Among community-dwelling older adults, capping maximum hold time at 10 seconds likely dilutes the ability of tandem stance to reveal more subtle but potentially still meaningful deficits.
The primary aim of this secondary analysis was to explore the functional relevance of the need for support to attain a tandem stance position by determining whether this requirement for support can discriminate among older adults based on meaningful differences in gait speed, Timed “Up & Go” Test (TUG)30 performance, and balance confidence. We hypothesized that older adults who can hold tandem stance only after being assisted into position will have worse scores on these clinical measures compared with those who need no such support. A secondary aim was to examine whether older adults when grouped by tandem stance hold time (using the common clinical caps of 10 and 30 seconds as cut-points) differ on these same functional measures of balance and mobility. We anticipated finding only small differences between hold time groups on these functional measures, supporting interpretation of tandem stance performance on a gradient scale and use of maximum hold times longer than 10 seconds.
Method
Study Design
This was a cross-sectional secondary analysis of an observational cohort study designed to develop and refine measures of balance and mobility in community-dwelling older adults.
Setting
Baseline data were collected at the University of Pittsburgh Claude D. Pepper Older Americans Independence Center from December 2006 to August 2007. Study procedures were approved by the University of Pittsburgh Institutional Review Board. Participants provided written informed consent.
Participants
A cohort of 120 adults aged 65 years and older was recruited from the Pittsburgh Pepper Center's Research Registry of community-dwelling older adults who consent to be contacted for participation in mobility studies. Efforts were made to enroll a cohort diverse in mobility. Participants could use any ambulatory assistive device, but had to rise from a chair and walk household distances without physical assistance. Exclusion criteria were unstable medical conditions (angina), progressive or persistent neuromuscular conditions (Parkinson disease), and pain restricting movement.
Participation was offered to 216 older adults by telephone. Seventy-six older adults were not interested in participating and 20 were ineligible; the remaining 120 were enrolled in the study.
Tandem Stance Protocols
10-second tandem stance test with support (10TSTS).
This protocol followed published SPPB instructions for tandem stance.14 The tester stood to one side of the participant, providing support at one arm if needed until the participant felt stable in tandem stance, with one foot directly in front of and touching the other foot. Participants self-selected the forward foot. Per SPPB protocol, support provided was the minimum needed to prevent loss of balance and was not recorded on the data collection form or otherwise factored into the score. Timing began as support was released and continued for 10 seconds or until participants moved out of tandem or contacted external support. Those who did not feel stable to begin timing were categorized as unable to attempt the test, considered a “floor effect.” Holding the tandem stance position for the full 10 seconds was classified as ceiling performance. Multiple attempts were not allowed. Instructions were given to position the arms, bend at the knees, or move the body as needed to maintain balance.14
30-second tandem stance test without support (30TST).
This test was administered as part of our own 30-second standing balance test protocol. The 30TST protocol differed from the 10TSTS protocol in only 2 features: (1) no support was allowed to attain tandem stance (participants who were unable to stabilize in tandem stance without support were classified as “unable to attempt”), and (2) maximum hold time was extended to 30 seconds. Other procedures followed published SPPB instructions. Timing began when the participant's feet appeared stable in tandem stance and ended after 30 seconds (ceiling performance), or when the participant moved either foot or made contact with any objects.
For both the 10TSTS and the 30TST protocols, hold times were recorded only for participants who were able to hold the tandem stance position for at least 1 second after any support was released.
General Measures
Demographics.
Information collected included age, sex, and race.
Body mass index (BMI).
Previously shown to contribute to performance on mobility tests in this and other cohorts,31,32 BMI was included as a potential confounder. It was calculated in kilograms per square meter from measurements of weight (in kilograms) and height (in centimeters) obtained using a Tanita BWB-800 scale and HR-200 wall-mounted height rod (Perspective Enterprises, Portage, Michigan) while wearing indoor clothing without shoes.
Performance-Based Measures of Mobility and Balance
Gait speed.
Gait speed (in meters per second) was measured using a 6-m GaitMat II instrumented walkway (EQ Inc, Chalfont, Pennsylvania). The GaitMat II is an automated gait analysis system using the opening and closing of pressure-sensitive switches to generate footprints on a computer screen as participants walk on the walkway. Reliability and validity are established.33,34 Gait speed was measured over the central 4 m, allowing 1 m on either side for acceleration and deceleration. Assistive devices were allowed if used for household ambulation. Two practice passes were followed by 4 passes at self-selected walking speed for data collection. Gait speed was recorded as the distance traversed divided by the time between the first and last steps (eg, switch closure). Mean gait speed was calculated by averaging the 4 trials. Found to be the strongest independent predictor of self-reported physical function among community-dwelling older adults,35 gait speed is increasingly recognized as an essential vital sign representing overall health and function in older adults,36,37 with relevant cut-points for predicting hospitalization, declines in health and lower-extremity function, and even survival.38–40 Usual gait speed for this age group is 1.2 to 1.3 m/s,41,42 and speeds above 1.0 m/s are consistent with longer life expectancy and low risk for future disability.38,40 Alternatively, speeds below 1.0 m/s are considered “mildly abnormal,” and those below 0.6 m/s are considered “seriously abnormal”37,43 and predict hospitalization.3
TUG.
Participants were asked to rise from a standard-height chair (44.45 cm [17.5 in] high) with armrests, walk 3 m, turn around without stopping, walk back to the chair, and sit down.30 Assistive devices used for household ambulation were allowed. Time to complete the task at a comfortable and safe pace was averaged over 2 trials. Balance is supported as one of the factors influencing TUG performance in older adults.44 Scores of less than 10 seconds are consistent with independence in activities of daily living (ADL) in people aged 79 years and older.30 A meta-analysis of TUG times in older adults who were healthy showed mean (95% confidence interval [CI]) reference values of 9.4 seconds (8.9–9.9) for individuals aged 60 years and older, 9.2 seconds (8.2–10.2) for those aged 70 to 79 years, and 11.3 seconds (10.0–12.7) for those aged 80 to 99 years.45 These reference values are consistent with findings in a group of community-dwelling older women, all of whom completed the TUG in under 12 seconds.46
Single-leg stance.
As part of our 30-second standing balance battery, participants balanced for up to 30 seconds while standing on the right leg without external support. The position was demonstrated with the left foot lifted behind the body, knee bent to 90 degrees, and hip neutral. The tester stood next to the participant, but no support was provided. Instructions were given to position the arms, bend the right knee, or move the body as needed to maintain balance, but the left foot could not touch down. Those participants who were unable to get into position without initial support were classified as unable to perform. Timing began when the participant appeared stable and ended after 30 seconds, or when external contact was made for support, including touching the left foot to the floor. Only one attempt was allowed, and hold time was recorded only if stable in single-leg stance for at least 1 second.
Self-Report Measures of Balance and Mobility
Activities-specific Balance Confidence Scale (ABC).47–49
Participants reported confidence that they will not fall or lose their balance with performance of 16 mobility-related activities. A response of 0% indicates no confidence, and a response of 100% indicates complete confidence. The total score is the average of scores for all 16 items. Reliability and validity have been established.47,48 Scores of 80% are consistent with a high level of physical functioning, and scores below 50% reflect low functioning, such as the need for home care services.48 Substantial decline in ABC score over 1 year has been reported as 10% in a secondary analysis from this parent cohort.50
Falls history.
Participants were asked about any falls in the previous year. A fall was defined as unintentionally coming to rest at a lower position.49,51 One-week test-retest reliability (kappa) was established as .89 for falling in the previous year in a subsample of 43 participants from our cohort (S. Perera, unpublished data).
To minimize order bias, the order of administration of all measures (both performance-based and self-report) varied by participant, except for sections of the same measure. For example, the 30TST was always attempted before the single-leg stance test, as both were part of our own 30-second standing balance protocol. In contrast, the 2 tandem stance protocols (30TST and 10TSTS) were not part of the same measure, so administration order varied and could be as much as 4 hours apart. To control for the impact of heel height on balance and walking, participants were asked to wear comfortable walking shoes. Times were recorded to the nearest hundredth of a second.
Data Analysis
We used SAS version 9.2 (SAS Institute Inc, Cary, North Carolina) for all analyses. Study participants were characterized using descriptive statistics.
Stratification based on need for initial support to stabilize in tandem stance.
Participants were categorized into 1 of the following 3 groups based on the need for initial support to stabilize in tandem stance as determined by comparing performance on the 10TSTS and the 30TST:
Unable even with support: Unable to hold tandem stance for at least 1 second, even if supported until stable in the position, so unable to perform tandem stance in either the 10TSTS protocol or the 30TST protocol.
Able only with support: Holds tandem stance only if supported until stable in the position, so able to perform the 10TSTS protocol, but not the 30TST protocol.
Able without support: Holds tandem stance after stabilizing in the position without any external support. Able to perform both the 10TSTS and 30TST protocols.
Stratification based on tandem stance hold time for those who could stabilize without support.
Participants who were able to perform tandem stance without initial support were further categorized into 1 of 3 groups based on their tandem stance hold times for the 30TST protocol. Because meaningful cut-points are not widely accepted for tandem stance, we established the following groups based on successful completion using the common maximal hold times of 10 and 30 seconds:
Low: Held tandem stance position less than 10 seconds.
Medium: Held tandem stance position between 10 and 29 seconds.
High: Achieved maximum hold time (30 seconds), considered a ceiling effect.
We are not the first to define achievement of the hold time cap as a complete attempt when establishing groups for comparison,13 and these same cut-points (10 and 30 seconds) have been used to explore age effects of similar tests.52 Thus, a 10-second cap such as used in the SPPB10 would distinguish only those in the low hold group, while extending to a 30-second maximum would further distinguish the medium hold group from the high hold group, who would still be limited by the tester-imposed ceiling.
We performed analysis of variance and Kruskal-Wallis tests with each established performance or self-report outcome measure or potential confounder as the response variable and each of the 3 tandem stance support performance groups (unable even with support, able only with support, and able without support) and the three 30TST hold time groups (low, medium, and high) as the primary factor of interest. We used the Fisher least significant difference and the Wilcoxon rank sum test to perform post hoc pair-wise comparisons among the 3 groups. Furthermore, 95% CIs were calculated around each group mean. Between-group comparisons for the 3 primary outcome measures (gait speed, TUG, ABC) were repeated with adjustment for age.
Role of the Funding Source
This work was funded by the Pittsburgh Claude D. Pepper Older Americans Independence Center (OAIC-NIA P30 AG024827; principal investigator: Dr Studenski), the National Institutes on Aging and American Federation of Aging Research Paul Beeson Career Development Award (K23 AG026766; principal investigator: Dr Brach), and a Training in Aging Research for MD Investigators Award (K07AG023641; principal investigator: Dr Studenski).
Results
Participants
Of 120 enrolled participants, 117 had complete data available for both tests of tandem stance. Table 1 presents the characteristics of the study sample. Briefly, the study sample was 72% female and 12% black and had a mean age of 78.2 years (SD=5.9, range=64–92). Gait speed averaged 1.07 m/s (SD=0.26), and the mean TUG completion time was 10.58 seconds (SD=3.86). The 3 participants with missing data were among those with higher functioning in the cohort based on gait speed and SPPB scores.
Table 1.
Description of the Study Sample (n=117)a
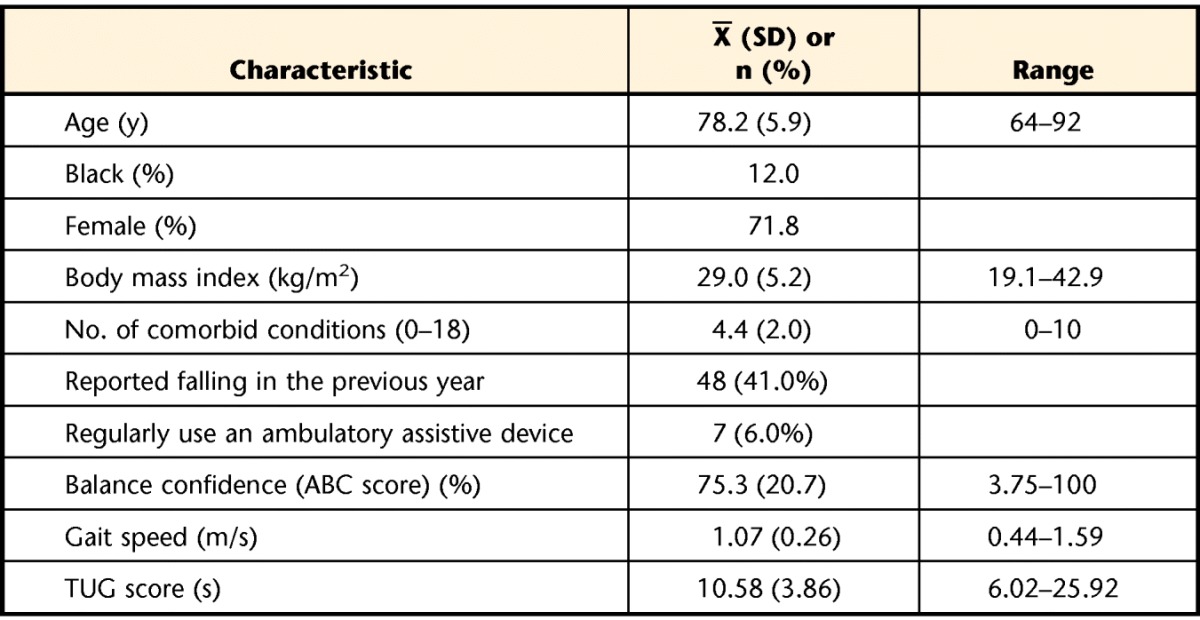
ABC=Activities-specific Balance Confidence Scale, TUG=Timed “Up & Go” Test.
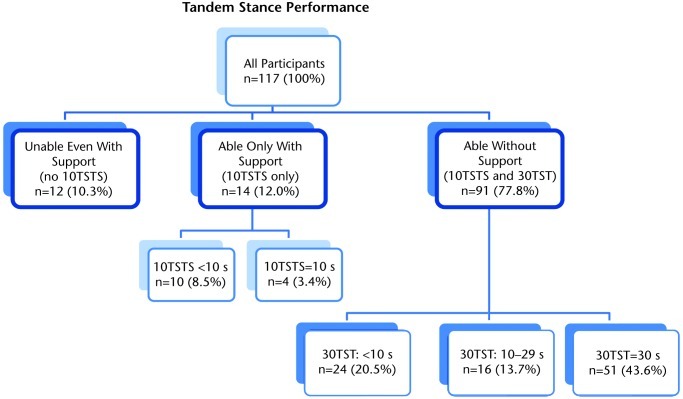
The Figure illustrates performance of the study sample on the 2 different tandem stance protocols (10TSTS and 30TST). Based on the need for external support to stabilize in tandem stance, all 117 participants were assigned to 1 of the 3 categories described in the “Method” section:
Figure.
Descriptive results for tandem stance performance with participants categorized based on ability to perform tandem stance with or without initial support to stabilize in position. All percentages indicate the percentage of the total sample (n=117). 10TSTS=10-second tandem stance test with support, 30TST=30-second tandem stance test without support. Unable even with support=unable to hold tandem stance for 1 second, even if supported until stable in position; unable to perform either the 10TSTS protocol or the 30TST protocol. Able only with support=holds tandem stance only if supported until stable in the position; able to perform the 10TSTS, but not the 30TST protocol. Able without support=holds tandem stance after stabilizing in position without initial support; able to perform both the 10TSTS and 30TST protocols. Support=light physical assistance provided at one arm while moving feet into tandem stance position and attempting to stabilize.
Unable even with support.
Twelve participants were unable to hold tandem stance for at least 1 second even if supported while stabilizing and thus were unable to perform either the 10TSTS protocol or the 30TST protocol.
Able only with support.
Fourteen participants were able to perform tandem stance only with initial support and thus could hold the tandem stance position for at least 1 second on the 10TSTS protocol, but could not perform the 30TST protocol. Nine (64%) of these individuals who were unable to perform the 30TST protocol were able to hold tandem stance for at least 3 seconds when initially supported (10TSTS), and 4 (29%) held tandem stance for the full 10 seconds. Thus, these 4 older adults performed at the ceiling level on the 10TSTS, but at the floor level on the 30TST.
Able without support.
Ninety-one people could perform tandem stance without any initial support to stabilize. Seventy-five (82%) of these individuals held tandem stance for the full 10 seconds when initial support was allowed (10TSTS), and 67 (74%) also were able to hold tandem stance for at least 10 seconds without initial support (30TST). As expected, no participant who was unable to perform tandem stance on the 10TSTS protocol (initial support provided) was able to perform the 30TST protocol (no initial support provided).
Impact of Initial Support to Stabilize in Tandem Stance
Results of the comparison of balance and mobility outcome measures across tandem stance support groups are presented in Table 2. Statistically significant and clinically meaningful differences were found between participants who needed initial support (able only with support group) and those who did not (able without support group) on all 3 primary outcomes. Compared with the able without support group, the able only with support group had slower gait speeds and TUG times and lower balance confidence. In contrast, means on these same measures for the able only with support group did not differ statistically or clinically from those of lowest tandem ability who could not perform even with support. On examination of descriptive measures, the unable even with support group was found to be significantly older than either of the other 2 groups; however, adjusting for age as a potential confounder did not change the results for the 3 primary outcomes in either statistical or clinical significance. Differences in falls over the previous year did not reach statistical significance between any 2 groups, so these analyses were not adjusted.
Table 2.
Comparison of Mobility-Related Results Across Tandem Stance Performance Groups Established Based on Need for Initial Supporta
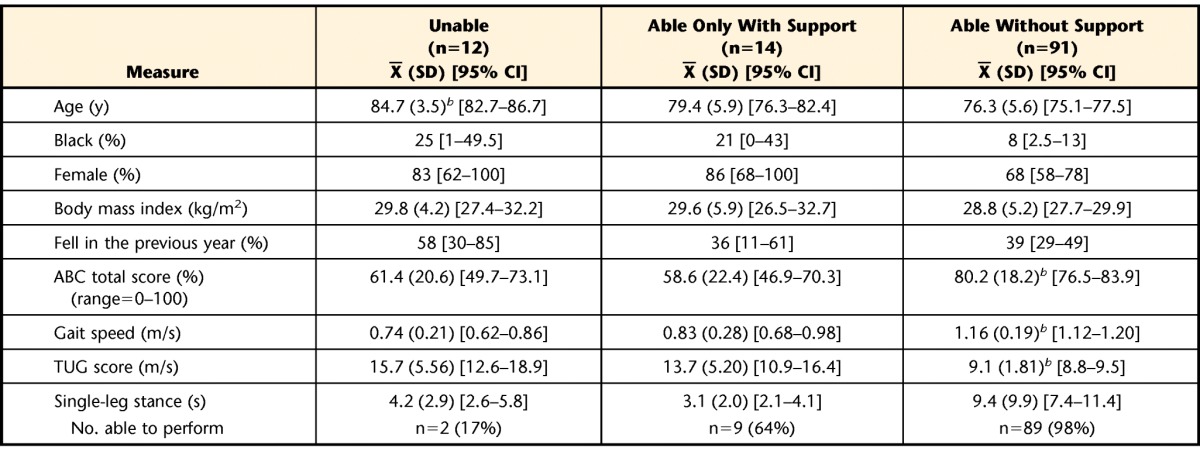
95% CI=95% confidence interval, ABC=Activities-specific Balance Confidence Scale, TUG=Timed “Up & Go” Test.
b Significantly different at the .05 level from the means of the other 2 groups.
Impact of Maximum Hold Time for Those Who Could Stabilize Without Support
Those in the highest-performing group (able without support) were further categorized based on tandem stance hold times for the 30TST protocol as described in the “Method” section. Table 3 summarizes results of a comparison among the 3 hold time groups (low, medium, and high) on measures of mobility and balance described previously. Only the results for comparison of balance confidence appear statistically significant and clinically meaningful, with 11% lower confidence for the low hold group compared with the high hold group. Although a difference of less than 1 second in TUG performance reached statistical significance, the 95% CIs around these means overlapped, and their clinical significance is unclear. Of those participants who could perform tandem stance without initial support, the medium hold group was older than the high hold group (mean=79 versus 75 years, respectively), but adjusting for age did not change the statistical or clinical interpretation of comparisons for the 3 primary outcome measures. Of note, 10 (19.6%) of the 51 participants who achieved high hold time without support to attain the position were over the age of 80 years.
Table 3.
Comparison of Mobility-Related Results Across Tandem Stance Hold Time Groups Established Based on 30TST Hold Times in the Able Without Support Groupa
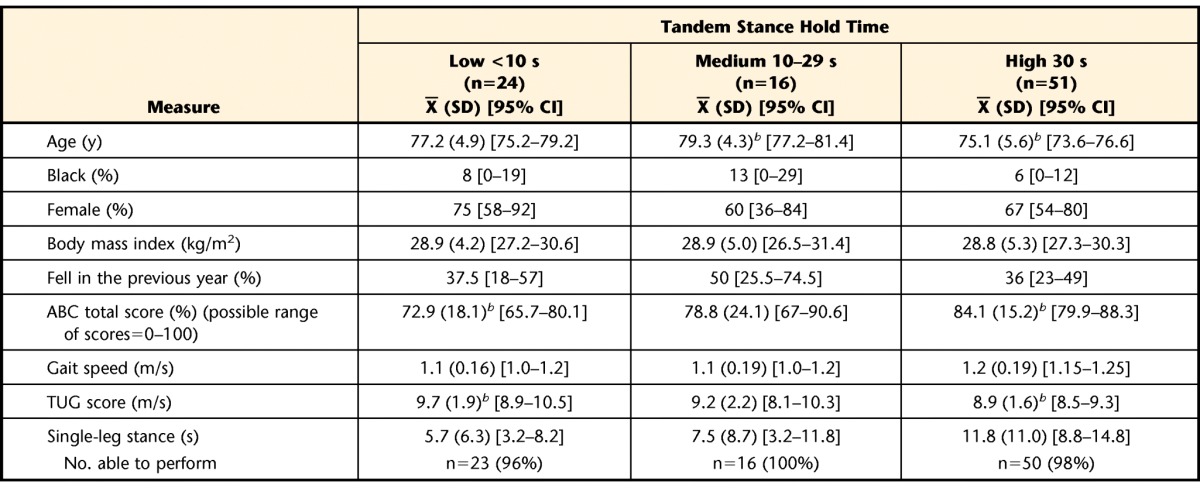
30TST=30-second tandem stance test without support, 95% CI=95% confidence interval, ABC=Activities-specific Balance Confidence Scale, TUG=Timed “Up & Go” Test.
b These 2 groups were significantly different from one another at the .05 level.
Floor and ceiling performance on the 2 different tandem protocols are compared in Table 4. Floor performance was defined as unable to perform or unable to hold the tandem stance position for at least 1 second after release of any initial support. Ceiling performance was defined as holding the tandem stance position for the maximum time (either 10 or 30 seconds). With no initial support provided and an extended maximum hold time, more participants performed at the floor level on the 30TST protocol than on the 10TSTS protocol. However, the reduction in ceiling performance was relatively greater, so that discriminating scores (scores falling between floor and ceiling) were obtained in an additional 13% of the sample with the 30TST protocol. To further isolate the impact of extending maximum hold time to 30 seconds, we compared the percentage of discriminating scores achieved with each cut-point (10 or 30 seconds) by this protocol alone (30TST). A 10-second cutoff provided discriminating scores for 21 individuals (18%), and extending the maximum hold time to 30 seconds provided discriminating scores for an additional 19 people (additional 16%).
Table 4.
Comparison of Floor and Ceiling Effects by Tandem Stance Protocola
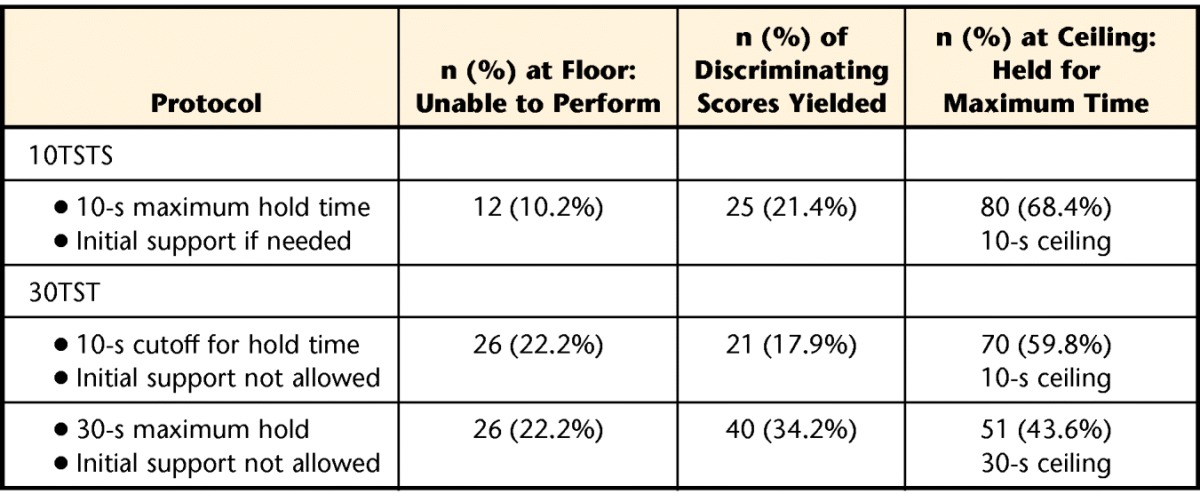
10TSTS=10-second tandem stance test with support, 30TST=30-second tandem stance test without support.
Discussion
When allowing initial support to stabilize in tests of tandem stance, interpret hold times with caution. The comparisons between a group of community-dwelling older adults who could stabilize in tandem stance without support and those who could stabilize only with initial support reported here suggest that the need for such support signals a meaningful distinction in balance-related mobility. When support is provided as needed but not considered during interpretation, some of those who require initial support achieve a ceiling in performance on a 10-second test. Without further testing, they may be incorrectly classified as having balance function no different from those who achieve a ceiling in performance without initial support. Inaccurate assumptions then may be made that those who need initial support but hold the tandem stance position for around 10 seconds have top balance function, low fall risk, and little need for rehabilitative services. We recognize that this was the case for only a small minority (<4%) of our study sample. However, if grouped only by hold time (<10 seconds) without attention to assistance, the others in the able only with support group (Tab. 2) would be classified as similar to the low hold time subgroup of the able without support group (Tab. 3); yet these groups appear distinct based on a clinical comparison of mean gait speed, TUG, and ABC scores. For both of these reasons, we recommend considering the need for initial support along with total tandem stance hold time. Additionally, based on results shown in Tables 3 and 4, when testing balance in older adults who can stabilize without initial support, a maximum of at least 30 seconds is recommended.
Consideration of clinical relevance expands upon the statistical interpretation of differences when comparing means for the intermediate performing (able only with support) and highest performing (able without support) tandem stance support groups (Tab. 2). Means for the able only with support group were both statistically and clinically worse than those for the able without support group for gait speed (0.83 versus 1.16 m/s), TUG (13.7 versus 9.1 second), and balance confidence (58.6% versus 80.2%). Therefore, needing initial support to stabilize in tandem stance appears to be clinically meaningful, distinguishing 2 groups of individuals who differ on balance-related mobility measures.
Our results for primary outcomes do not support meaningful differences between the 2 groups who could not perform the 30TST (unable even with support and able only with support; Tab. 2). Comparisons of group means were not statistically significant, and the 95% CIs around potentially clinically relevant means overlap. Although single-leg stance hold times did not differ between the 2 groups (mean=3.1 seconds for both groups), it should be noted that only 25% of those who were unable to perform tandem stance could stand unsupported on one leg to be included in this mean compared with 65% of those who could perform tandem stance with support. Clearly, both groups have some degree of balance and mobility dysfunction, and although any differences between them may be subtle, it is possible that the transition from unable to perform tandem stance to able to perform tandem stance with support reflects more than simply a continuum of balance ability. These 2 groups also may differ in underlying contributors to their balance impairment, specifically the relative deficits in physiologic systems (eg, vision, strength, peripheral sensation) known to differentially influence postural stability.7,53–56 Limited impairment-based measures are available for exploration of contributors in this cohort, which is beyond the scope of our aims.
Results outlined in Tables 3 and 4 support extending maximum hold times for tandem stance tests from 10 seconds to at least 30 second to better distinguish community-dwelling older adults of higher ability. The lower limit of the CI (upper limit for the TUG) for means on primary measures suggests that even within the medium and high hold time groups, there are individuals with clinically meaningful balance and mobility deficits. After comparing 95% CIs, the only statistically and clinically meaningful difference in primary outcomes between any 2 groups is higher balance confidence (84.1% versus 72.9%) among those who could hold the tandem stance position more than 30 seconds compared with those who could not hold tandem stance for 10 seconds. An even longer hold time may further distinguish the 44% of the study sample who performed at the 30-second ceiling even without initial support (Tab. 4). Although extending hold times is an approach published in the epidemiologic literature,28 an alternative to discriminating balance in older adults with highest functioning is to progress to a more challenging test. Our results (Tab. 3) support those of Rossiter-Fornoff and colleagues, who found one-leg standing further discriminated among those with ceiling performance on tandem stance tests.13 Unfortunately, concerns over standardization of protocols extend to single-leg stance. After reviewing the one-leg standing test, Michikawa and colleagues57 concluded that a uniformly standardized protocol could not be identified and that variation in methods confounded the reporting of reference values.
Our findings also support those of Jonsson and colleagues,15 who identified 2 phases of the tandem stance task. They suggested that the ability to get into position and hold it for the first few seconds (postural adjusting phase) is a better measure of balance than total hold time (muscle strength and endurance component). Our findings in a more functionally diverse older cohort support the significance of the postural adjusting phase. In our cohort, the need for initial support to perform tandem stance categorized older adults into groups with clinically and statistically significant differences in key self-report and performance-based measures. These data begin to suggest that the ability to achieve a stable tandem position for at least 1 second without support may, in itself, be a useful test of balance.
In a more recent article, Shubert and colleagues4 dichotomized results of a tandem stance test performed with initial support. Data from nearly 200 elderly people with high functioning (70% walked ≥1.0 m/s, 99% were independent in ADL, and only 16% were dependent in more than one instrumental ADL task) were bimodal in distribution, with most participants holding the tandem stance position for either 10 (ceiling) or only 1 to 2 seconds. We suggest that those individuals who held tandem stance for only 1 or 2 seconds may represent a group who could not have attained tandem stance without support. Allowing initial support without documenting for later consideration whether such support was necessary may limit clinical utility of tandem stance by measuring only the second phase of the task: the ability to maintain the posture once stable.
The influence of support given to attain the tandem stance position is likely much more complicated than merely having additional mechanical support. Studies suggest that sensory feedback from even the lightest touch provided at the arm is likely to alter postural control. Postural synergies typically observed when rising up onto the toes change when upper-limb support is allowed,58 and balance is known to be influenced by both “haptic cues” from fingertip contact59–61 and proprioceptive input from light contact, or interpersonal support similar to holding hands.62–65 Furthermore, recent evidence suggests that the established link between lower-limb muscle strength and balance66–68 may be explained by related proprioceptive input.69 Although investigators interested only in the ability to hold a challenge position might argue that initial support is irrelevant, we wonder whether the additional sensory cues could alter postural responses even after the support is released. Because participants in our study were not given support unless it was needed, we cannot perform within-subject analyses of the able without support group to explore the influence of the type of upper-limb support we provided on hold times. Standing off to one side of the participant, we provided lateral support, shown to be more stabilizing than other support in other directions during tandem stance.70
We believe that both phases of the tandem stance task reflect functional balance requirements for mobility, although each phase provides very different information. Clinically screening postural preparations, anticipatory postural adjustments, and postural responses by moving into a challenge position would seem just as relevant to everyday mobility as holding that position, especially a position that cannot be attained without help and thus is unlikely to be held in daily life. Our results suggest that the need for support to move into the tandem stance position has clinical meaning and should be considered part of the test, in which case continuing to classify tandem standing testing as “static” would be inaccurate.
Studies have shown standing balance task performance to relate to age,27,52,71–73 and although we found participants who could not perform tandem stance even if support was provided to be the oldest of all groups (Tab. 2), age did not distinguish those who could perform only with initial support from those who could perform without it. Additionally, age did not vary across hold time groups in the able to perform without support group (Tab. 3) as expected, as the medium hold group was oldest. This finding could be a function of our sample, which included some “exceptional” older adults (including 10 over the age of 80 years who performed at the ceiling on the 30TSTS), but it also could be a function of comparing only those who could attain the tandem stance position without support. Note that we are not suggesting that the need for support identifies fallers, one of the most multifactorial issues in aging. Instead, we seek to identify performance deficits that may signal a need for physical therapy intervention.
Limitations of this study should be addressed. First, as a secondary cross-sectional analysis of an observational, prospective study designed for other aims, power was not established a priori for the tandem stance groups as ultimately defined. Small cell sizes for 2 of the 3 groups limited the strength of our between-group comparisons. Additionally, because there is no established standard, we defined being able to hold tandem stance as requiring at least 1 second in the position after any support is released. This definition was based on consideration of reaction time to stop a timer while simultaneously guarding someone who is losing balance; we agreed that times of less than 1 second represent failure to stabilize in tandem stance. Still, a 1-second minimum has been used by at least one other group of authors.13 Similarly, although based on commonly used caps, the cut-points of 10 and 30 seconds used in our hold time comparisons are not well established. Unfortunately, similar comparisons of hold times could not be made for those individuals in the able only with support group, as hold time for the only test they could perform (10TSTS) was capped at 10 seconds. This is another disadvantage of a secondary analysis. Finally, our sample of community-dwelling older adults from a university-based research registry for balance and mobility studies may be different from those encountered in a clinic setting.
In summary, we make the following recommendations for tandem stance testing: (1) when providing initial support to stabilize, document this support along with the hold time to allow appropriate comparisons to be made both within and across individuals, and (2) when testing individuals who can stabilize without initial support, a maximum hold time of 30 seconds or longer may be preferred to a 10-second cap. The first recommendation may better characterize people with lower balance and mobility function, and the latter recommendation may uncover subtle but potentially meaningful deficits in individuals with higher functioning. Finally, continued evidence that a test typically categorized as “static” has a “dynamic” component that may be even more translatable to daily mobility may prompt future change in categorization of these low-burden tests. Further research is warranted into the relative value of the dynamic and static phases of tandem stance when interpreting everyday significance in older adults with widely ranging balance. Our findings support viewing hold times along a continuum and drawing comparisons between individuals only if the same rules are followed in assuming the tandem stance position.
The Bottom Line
What do we already know about this topic?
Tandem stance performance can characterize balance in older adults; however, the protocols do not standardize specifics such as hold times and the provision of initial support. Given that light touch is known to alter postural control, and given that the tandem stance test appears to have 2 phases, further examination of these key protocol features is warranted.
What new information does this study offer?
Based on the results of this study, requiring initial support to attain tandem stance appears to reflect meaningful deficits in balance-related mobility, so getting into the tandem stance position should be part of the test. For community dwellers who are able to attain tandem stance without support, extending the hold time cap to at least 30 seconds further discriminates performance.
If you're a patient, what might these findings mean for you?
When you have your balance assessed, it is important to follow all directions closely. Your clinician is evaluating not only your ability to hold a position, but also your ability to get into the position without help.
Footnotes
Dr Hile, Dr Brach, Dr Perera, and Dr Studenski provided concept/idea/research design. Dr Hile, Dr Brach, Dr Perera, Dr VanSwearingen, and Dr Studenski provided writing. Dr Hile, Dr Brach, Dr Wert, and Dr Studenski provided data collection. Dr Brach, Dr Perera, and Dr Studenski provided data analysis. Dr Hile and Dr Brach provided project management. Dr Brach and Dr Studenski provided fund procurement and study participants. Dr Studenski provided facilities/equipment. Dr Brach, Dr Perera, Dr Wert, and Dr VanSwearingen provided consultation (including review of manuscript before submission).
This cross-sectional analysis and the larger cohort study from which it was derived were approved by the University of Pittsburgh Institutional Review Board.
Preliminary results were presented as a Geriatrics Section poster at the Combined Section Meeting of the American Physical Therapy Association; February 17–20, 2010; San Diego, California.
This work was funded by the Pittsburgh Claude D. Pepper Older Americans Independence Center (OAIC-NIA P30 AG024827; principal investigator: Dr Studenski), the National Institutes on Aging and American Federation of Aging Research Paul Beeson Career Development Award (K23 AG026766; principal investigator: Dr Brach), and a Training in Aging Research for MD Investigators Award (K07AG023641; principal investigator: Dr Studenski). Funding from all sources provided salary support for the investigators and other research staff, remunerated participants for time and travel, purchased equipment, and paid for management and analyses of data.
References
- 1. Anemaet WK, Krulish LH. Fall Risk Assessments in home care: OASIS-C expectations. Home Health Care Manag Pract. 2011;23:125–138 [Google Scholar]
- 2. Kornetti D. Therapy Documentation Toolkit: Balance Module. Gaithersburg, MD: DecisionHealth; 2011 [Google Scholar]
- 3. Studenski S, Perera S, Wallace D, et al. Physical performance measures in the clinical setting. J Am Geriatr Soc. 2003;51:314–322 [DOI] [PubMed] [Google Scholar]
- 4. Shubert TE, Schrodt LA, Mercer VS, et al. Are scores on balance screening tests associated with mobility in older adults? J Geriatr Phys Ther. 2006;29:35–39 [PubMed] [Google Scholar]
- 5. Stel VS, Smit JH, Pluijm SM, Lips P. Balance and mobility performance as treatable risk factors for recurrent falling in older persons. J Clin Epidemiol. 2003;56:659–668 [DOI] [PubMed] [Google Scholar]
- 6. Spirduso WW, Francis KL, MacRae PG. Balance and posture: evaluating the multiple dimensions of balance. In: Spirduso WW, Francis KL, MacRae PG. Physical Dimensions of Aging. Champaign, IL: Human Kinetics; 2005:144 [Google Scholar]
- 7. Lord SR, Rogers MW, Howland A, Fitzpatrick R. Lateral stability, sensorimotor function and falls in older people. J Am Geriatr Soc. 1999;47:1077–1081 [DOI] [PubMed] [Google Scholar]
- 8. Maki BE, Holliday PJ, Topper AK. A prospective study of postural balance and risk of falling in an ambulatory and independent elderly population. J Gerontol. 1994;49:M72–M84 [DOI] [PubMed] [Google Scholar]
- 9. Rogers MW, Mille ML. Lateral stability and falls in older people. Exerc Sport Sci Rev. 2003;31:182–187 [DOI] [PubMed] [Google Scholar]
- 10. Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–M94 [DOI] [PubMed] [Google Scholar]
- 11. Berg K, Wood-Dauphinée S, Williams JI, et al. Measuring balance in the elderly: preliminary development of an instrument. Physiother Can. 1989;41:304–311 [Google Scholar]
- 12. Thomas M, Jankovic J, Suteerawattananon M, et al. Clinical Gait and Balance Scale (GABS): validation and utilization. J Neurol Sci. 2004;217:89–99 [DOI] [PubMed] [Google Scholar]
- 13. Rossiter-Fornoff JE, Wolf SL, Wolfson LI, Buchner DM. A cross-sectional validation study of the FICSIT common data base static balance measures. Frailty and Injuries: Cooperative Studies of Intervention Techniques. J Gerontol A Biol Sci Med Sci. 1995;50:M291–M297 [DOI] [PubMed] [Google Scholar]
- 14. National Institute on Aging Assessing physical performance in the older patient. Available at: http://www.grc.nia.nih.gov/branches/ledb/sppb/. Updated February 13, 2012 Accessed April 13, 2012
- 15. Jonsson E, Seiger A, Hirschfeld H. Postural steadiness and weight distribution during tandem stance in healthy young and elderly adults. Clin Biomech (Bristol, Avon). 2005;20:202–208 [DOI] [PubMed] [Google Scholar]
- 16. Rooks DS, Kiel DP, Parsons C, Hayes WC. Self-paced resistance training and walking exercise in community-dwelling older adults: effects on neuromotor performance. J Gerontol A Biol Sci Med Sci. 1997;52:M161–M168 [DOI] [PubMed] [Google Scholar]
- 17. Portegijs E, Sipila S, Alen M, et al. Leg extension power asymmetry and mobility limitation in healthy older women. Arch Phys Med Rehabil. 2005;86:1838–1842 [DOI] [PubMed] [Google Scholar]
- 18. Muir SW, Berg K, Chesworth B, et al. Balance impairment as a risk factor for falls in community-dwelling older adults who are high functioning: a prospective study. Phys Ther. 2010;90:338–347 [DOI] [PubMed] [Google Scholar]
- 19. Harrison A, Dunsmore L, Holt C, et al. Fall risk factors in adults with diabetic peripheral neuropathy. Abstract presented at: Combined Sections Meeting of the American Physical Therapy Association; February 17–20, 2010; San Diego, California [Google Scholar]
- 20. Frank JS, Earl M. Coordination of posture and movement. Phys Ther. 1990;70:855–863 [DOI] [PubMed] [Google Scholar]
- 21. Gahery Y. Associated movements, postural adjustments and synergies: some comments about the history and significance of three motor concepts. Arch Ital Biol. 1987;125:345–360 [PubMed] [Google Scholar]
- 22. Belen'kii VE, Gurfinkel VS, Pal'tsev EI. Control elements of voluntary movements [in Russian]. Biofizika. 1967;12:135–141 [PubMed] [Google Scholar]
- 23. Bouisset S, Zattara M. A sequence of postural movements precedes voluntary movement. Neurosci Lett. 1981;22:263–270 [Google Scholar]
- 24. Bouisset S, Zattara M. Biomechanical study of the programming of anticipatory postural adjustments associated with voluntary movement. J Biomech. 1987;20:735–742 [DOI] [PubMed] [Google Scholar]
- 25. Cordo PJ, Nashner LM. Properties of postural adjustments associated with rapid arm movements. J Neurophysiol. 1982;47:287–302 [DOI] [PubMed] [Google Scholar]
- 26. Lee WA. A control systems framework for understanding normal and abnormal posture. Am J Occup Ther. 1989;43:291–301 [DOI] [PubMed] [Google Scholar]
- 27. Fregly AR, Smith MJ, Graybiel A. Revised normative standards of performance of men on a quantitative ataxia test battery. Acta Otolaryngol. 1973;75:10–16 [DOI] [PubMed] [Google Scholar]
- 28. Simonsick EM, Newman AB, Nevitt MC, et al. Measuring higher level physical function in well-functioning older adults: expanding familiar approaches in the Health ABC study. J Gerontol A Biol Sci Med Sci. 2001;56:M644–M649 [DOI] [PubMed] [Google Scholar]
- 29. Muir SW, Berg K, Chesworth B, Speechley M. Use of the Berg Balance Scale for predicting multiple falls in community-dwelling elderly people: a prospective study. Phys Ther. 2008;88:449–459 [DOI] [PubMed] [Google Scholar]
- 30. Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39:142–148 [DOI] [PubMed] [Google Scholar]
- 31. Hergenroeder AL, Brach JS, Otto AD, et al. The influence of body mass index on self-report and performance-based measures of physical function in adult women. Cardiopulm Phys Ther J. 2011;22:11–20 [PMC free article] [PubMed] [Google Scholar]
- 32. Hergenroeder AL, Wert DM, Hile ES, et al. Association of body mass index with self-report and performance-based measures of balance and mobility. Phys Ther. 2011;91:1223–1234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Barker S, Craik R, Freedman W, et al. Accuracy, reliability, and validity of a spatiotemporal gait analysis system. Med Eng Phys. 2006;28:460–467 [DOI] [PubMed] [Google Scholar]
- 34. Brach JS, Berthold R, Craik R, et al. Gait variability in community-dwelling older adults. J Am Geriatr Soc. 2001;49:1646–1650 [DOI] [PubMed] [Google Scholar]
- 35. Cress ME, Schechtman KB, Mulrow CD, et al. Relationship between physical performance and self-perceived physical function. J Am Geriatr Soc. 1995;43:93–101 [DOI] [PubMed] [Google Scholar]
- 36. Fritz S, Lusardi M. White paper: “walking speed: the sixth vital sign” [erratum in: J Geriatr Phys Ther. 2009;32:110]. J Geriatr Phys Ther. 2009;32:46–49 [PubMed] [Google Scholar]
- 37. Studenski S. Bradypedia: is gait speed ready for clinical use? J Nutr Health Aging. 2009;13:878–880 [DOI] [PubMed] [Google Scholar]
- 38. Cesari M, Kritchevsky SB, Penninx BW, et al. Prognostic value of usual gait speed in well-functioning older people: results from the Health, Aging and Body Composition Study. J Am Geriatr Soc. 2005;53:1675–1680 [DOI] [PubMed] [Google Scholar]
- 39. Guralnik JM, Ferrucci L, Pieper CF, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci. 2000;55:M221–M231 [DOI] [PubMed] [Google Scholar]
- 40. Studenski S, Perera S, Patel K, et al. Gait speed and survival in older adults. JAMA. 2011;305:50–58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Imms FJ, Edholm OG. The assessment of gait and mobility in the elderly. Age Ageing. 1979;8:261–267 [DOI] [PubMed] [Google Scholar]
- 42. Imms FJ, Edholm OG. Studies of gait and mobility in the elderly. Age Ageing. 1981;10:147–156 [DOI] [PubMed] [Google Scholar]
- 43. Abellan van Kan G, Rolland Y, Andrieu S, et al. ; for the International Academy on Nutrition and Aging (IANA) Task Force. Gait speed at usual pace as a predictor of adverse outcomes in community-dwelling older people. J Nutr Health Aging. 2009;13:881–889 [DOI] [PubMed] [Google Scholar]
- 44. Kwan MM, Lin SI, Chen CH, et al. Sensorimotor function, balance abilities and pain influence Timed Up and Go performance in older community-living people. Aging Clin Exp Res. 2011;23:196–201 [DOI] [PubMed] [Google Scholar]
- 45. Bohannon RW. Reference values for the timed up and go test: a descriptive meta-analysis. J Geriatr Phys Ther. 2006;29:64–68 [DOI] [PubMed] [Google Scholar]
- 46. Bischoff HA, Stahelin HB, Monsch AU, et al. Identifying a cut-off point for normal mobility: a comparison of the timed “up and go” test in community-dwelling and institutionalised elderly women. Age Ageing. 2003;32:315–320 [DOI] [PubMed] [Google Scholar]
- 47. Powell LE, Myers AM. The Activities-specific Balance Confidence (ABC) Scale. J Gerontol A Biol Sci Med Sci. 1995;50:M28–M34 [DOI] [PubMed] [Google Scholar]
- 48. Myers AM, Fletcher PC, Myers AH, Sherk W. Discriminative and evaluative properties of the Activities-Specific Balance Confidence (ABC) Scale. J Gerontol A Biol Sci Med Sci. 1998;53:M287–M294 [DOI] [PubMed] [Google Scholar]
- 49. Myers AM, Powell LE, Maki BE, et al. Psychological indicators of balance confidence: relationship to actual and perceived abilities. J Gerontol A Biol Sci Med Sci. 1996;51:M37–M43 [DOI] [PubMed] [Google Scholar]
- 50. Wert DM, Brach JS, Hile E, et al. Meaningful change and responsiveness of psychological fall-related factors in older adults. Abstract presented at: Combined Sections Meeting of the American Physical Therapy Association; February 17–20, 2010; San Diego, California [Google Scholar]
- 51. Tinetti ME, Richman D, Powell L. Falls efficacy as a measure of fear of falling. J Gerontol. 1990;45:P239–P243 [DOI] [PubMed] [Google Scholar]
- 52. Vereeck L, Wuyts F, Truijen S, Van de Heyning P. Clinical assessment of balance: normative data, and gender and age effects. Int J Audiol. 2008;47:67–75 [DOI] [PubMed] [Google Scholar]
- 53. Lord SR, Clark RD, Webster IW. Postural stability and associated physiological factors in a population of aged persons. J Gerontol. 1991;46:M69–M76 [DOI] [PubMed] [Google Scholar]
- 54. Lord SR, Ward JA. Age-associated differences in sensori-motor function and balance in community dwelling women. Age Ageing. 1994;23:452–460 [PubMed] [Google Scholar]
- 55. Lord SR, Menz HB. Visual contributions to postural stability in older adults. Gerontology. 2000;46:306–310 [DOI] [PubMed] [Google Scholar]
- 56. Narayanan MR, Scalzi ME, Redmond SJ, et al. Evaluation of functional deficits and falls risk in the elderly: methods for preventing falls. Conf Proc IEEE Eng Med Biol Soc. 2009;2009:6179–6182 [DOI] [PubMed] [Google Scholar]
- 57. Michikawa T, Nishiwaki Y, Takebayashi T, Toyama Y. One-leg standing test for elderly populations. J Orthop Sci. 2009;14:675–685 [DOI] [PubMed] [Google Scholar]
- 58. Nardone A, Schieppati M. Postural adjustments associated with voluntary contraction of leg muscles in standing man. Exp Brain Res. 1988;69:469–480 [DOI] [PubMed] [Google Scholar]
- 59. Kouzaki M, Masani K. Reduced postural sway during quiet standing by light touch is due to finger tactile feedback but not mechanical support. Exp Brain Res. 2008;188:153–158 [DOI] [PubMed] [Google Scholar]
- 60. Tremblay F, Mireault AC, Dessureault L, et al. Postural stabilization from fingertip contact; I: variations in sway attenuation, perceived stability and contact forces with aging. Exp Brain Res. 2004;157:275–285 [DOI] [PubMed] [Google Scholar]
- 61. Tremblay F, Mireault AC, Dessureault L, et al. Postural stabilization from fingertip contact II: relationships between age, tactile sensibility and magnitude of contact forces. Exp Brain Res. 2005;164:155–164 [DOI] [PubMed] [Google Scholar]
- 62. Johannsen L, Guzman-Garcia A, Wing AM. Interpersonal light touch assists balance in the elderly. J Mot Behav. 2009;41:397–399 [DOI] [PubMed] [Google Scholar]
- 63. Johannsen L, Wing AM, Hatzitaki V. Contrasting effects of finger and shoulder interpersonal light touch on standing balance. J Neurophysiol. 2012;107:216–225 [DOI] [PubMed] [Google Scholar]
- 64. Rabin E, DiZio P, Ventura J, Lackner JR. Influences of arm proprioception and degrees of freedom on postural control with light touch feedback. J Neurophysiol. 2008;99:595–604 [DOI] [PubMed] [Google Scholar]
- 65. Rogers MW, Wardman DL, Lord SR, Fitzpatrick RC. Passive tactile sensory input improves stability during standing. Exp Brain Res. 2001;136:514–522 [DOI] [PubMed] [Google Scholar]
- 66. Corbeil P, Blouin JS, Begin F, et al. Perturbation of the postural control system induced by muscular fatigue. Gait Posture. 2003;18:92–100 [DOI] [PubMed] [Google Scholar]
- 67. Lord SR, Allen GM, Williams P, Gandevia SC. Risk of falling: predictors based on reduced strength in persons previously affected by polio. Arch Phys Med Rehabil. 2002;83:757–763 [DOI] [PubMed] [Google Scholar]
- 68. Vuillerme N, Burdet C, Isableu B, Demetz S. The magnitude of the effect of calf muscles fatigue on postural control during bipedal quiet standing with vision depends on the eye-visual target distance. Gait Posture. 2006;24:169–172 [DOI] [PubMed] [Google Scholar]
- 69. Butler AA, Lord SR, Rogers MW, Fitzpatrick RC. Muscle weakness impairs the proprioceptive control of human standing. Brain Res. 2008;1242:244–251 [DOI] [PubMed] [Google Scholar]
- 70. Rabin E, Bortolami SB, DiZio P, Lackner JR. Haptic stabilization of posture: changes in arm proprioception and cutaneous feedback for different arm orientations. J Neurophysiol. 1999;82:3541–3549 [DOI] [PubMed] [Google Scholar]
- 71. Bohannon R. Single limb stance times: a descriptive meta-analysis of data from individuals at least 60 years of age. Top Geriatr Rehabil. 2006;22:70–77 [Google Scholar]
- 72. Stemmons Mercer V, Sahrmann SA, Diggles-Buckles V, Abrams RA. Age group differences in postural adjustments associated with a stepping task. J Mot Behav. 1997;29:243–253 [DOI] [PubMed] [Google Scholar]
- 73. Speers RA, Ashton-Miller JA, Schultz AB, Alexander NB. Age differences in abilities to perform tandem stand and walk tasks of graded difficulty. Gait Posture. 1998;7:207–213 [DOI] [PubMed] [Google Scholar]