Abstract
It is of great interest to develop a pneumonic plague vaccine that would induce combined humoral and cellular immunity in the lung. Here we investigate a novel approach based on targeting of dendritic cells using the DEC-205/CD205 receptor (DEC) via the intranasal route as way to improve mucosal cellular immunity to the vaccine. Intranasal administration of Y. pestis LcrV (V) protein fused to anti-DEC antibody together with poly IC as an adjuvant induced high frequencies of IFN-γ secreting CD4+ T cells in the airway and lung as well as pulmonary IgG and IgA antibodies. Anti-DEC:LcrV was more efficient to induce IFN-γ/TNF-α/IL-2 secreting polyfunctional CD4+ T cells when compared to non-targeted soluble protein vaccine. In addition, the intranasal route of immunization with anti-DEC:LcrV was associated with improved survival upon pulmonary challenge with the virulent CO92 Y. pestis. Taken together, these data indicate that targeting dendritic cells via the mucosal route is a potential new avenue for the development of a mucosal vaccine against pneumonic plague.
Keywords: Dendritic cells, CD205/DEC-205, Y. pestis, LcrV, Cellular immunity, Mucosal
INTRODUCTION
Considering the rapid onset of the pneumonic plague disease, the induction of strong mucosal immunity is considered to be important for an efficient pneumonic plague vaccine. In contrast to other Gram-negative bacterial pneumonia, it is known that there is a delay in inflammatory cell recruitment to the lungs, as well as production of proinflammatory cytokines and chemokines in the first 48 hrs of Yersinia pestis (Y. pestis) infection, suggesting either evasion and/or suppression of the host innate immune response[1, 2]. Therefore, adequately designed vaccines should thwart such delayed responses at mucosal surfaces to accelerate bacterial clearance before systemic dissemination.
Various approaches have been examined to enhance mucosal immunity including different immunization routes and adjuvants. Intratracheal or intranasal administration of vaccines, as well as heterologous prime/boost strategies, have been shown to enhance mucosal immunity when compared to systemic administration[3-6]. In case of mucosal delivery, F1 and/or V subunit vaccines had been previously co-administered either with Cholera toxin B subunit, proteosome-based adjuvnats (ProtollinTM) or a Toll-like receptor 5 agonist, or flagellin[6-8]. Compared to free antigen delivery, either co-encapsulated antigens with microspheres or liposome-formulated delivery induce superior humoral immunity at mucosal surfaces. With these adjuvants, survival rates correlated with increased antibody titers in serum and lung washes[4, 6, 7]. Moreover, intratracheal delivery of monoclonal antibodies to F1 or V was sufficient to protect mice against aerosolized Y. pestis GB strain challenge[9]. Therefore, high antibody level is associated with protection against Y. pestis.
The role of cellular immunity for a successful plague vaccine has also been emphasized, particularly for primates, but at this point one requires methods to induce strong cell-mediated immunity in the lung. Treatment of mice with exogenous IFN-γ plus TNF-α inhibited the multiplication of Y. pestis in vivo, thereby conferring protection against intravenous challenge against 10 MLD (median lethal dose) of LcrV+ Y. pestis KIM[10]. Moreover, Stat-4 deficient mice, which have low levels of IFN-γ production, were poorly protected from Y. pestis GB by the s.c. route, despite producing high levels of serum antibody compared to wild type controls[11]. Recent studies by Smiley and colleagues demonstrated that naive B cell-deficient mice (μMT−/−) were protected against attenuated Y. pestis (KIM D27) intranasal challenge if the mice were adoptively transferred with Y. pestis-primed T cells. These cells were expanded in vitro with heat-killed Y. pestis, and protection was abolished upon removal of T cells, IFN-γ, or TNF-α[12, 13]. This investigation further showed that neutralizing TNF-α and IFN-γ reduced survival rate conferred by the suboptimal doses F1- or LcrV-specific mAb against 12LD50 intranasal challenge of Y. pestis CO92 strain[14]. In particular, B cell deficient mice primed and boosted with a live attenuated Y. pestis strain D27-pLpxL induced Th1 and Th17 cellular response, which protected against pulmonary D27 strain infection[15]. These results suggest that an effective pneumonic plague vaccine must prime strong responses in both humoral and cellular immunity not only systemically but also at mucosal surfaces.
In order to induce efficient cellular immunity against LcrV protein, we targeted the LcrV virulence protein to DEC-205/CD205 positive dendritic cells (DCs) systemically in the presence of poly IC and αCD40 as DC maturation stimuli. Under these conditions, we could induce broad splenic CD4+ Th1 type cellular immunity specific for several LcrV peptides presented by different MHC II haplotypes[16]. The DC-targeting strategy has been shown to improve plague vaccine efficacy against a human pathogen [17]. Here, we further utilized this targeting strategy combined with an intranasal delivery with the aim of inducing CD4+Th1 type cellular immunity, along with humoral immunity, at mucosal surfaces. We show that antigen targeting to DCs leads to greatly enhanced presentation to T cells when compared to non-targeted antigen at mucosal surfaces, and that this immunity is broad and accompanied by formation of mucosal IgG and IgA antibodies. Using a pulmonary challenge model, the intranasal route of immunization confers better protection as compared to the subcutaneous route.
MATERIALS & METHODS
Mice
C57BL/6 (H-2b), BALB/c (H-2d), and C3H/HeJ (H-2k) mice were purchased from Taconic, and DEC-205−/− mice (C57BL/6 background) from Jackson Laboratories. All mice were maintained under specific pathogen-free conditions and used at 5-7 wks of age according to the guidelines of our Institutional Animal Care and Use Committee.
Construction and production of fusion antibodies and protein
The fusion αDEC:LcrV antibody, a control Ig:LcrV antibody, and soluble LcrV protein were produced as described[16]. A recombinant F1-V protein from U.S. Army Medical Research Institute of Infectious Diseases (USAMRIID, Frederick, MD) has been described[18]. All proteins had <0.125 endotoxin units/mg using a Limulus Amebocyte Lysate assay, QCL-1000 (Bio Whittaker, Walkersville, MD).
Immunization
Mice were injected subcutaneously (s.c.) in the hind footpads, or intranasally (i.n.) in a total volume of 25 μl with the indicated doses of fusion antibody, control Ig antibody, or soluble LcrV protein along with 50 μg of poly IC (pIC, InVivogen, San Diego, CA) as adjuvant. F1-V recombinant protein was given in alhydrogel (2.0 % Alhydrogel, Superfos Biosector, Vedbaek, Denmark).
LcrV peptides
15-mer peptides spanning the entire LcrV sequence and overlapping by 11 amino acids (aa) were synthesized at the Rockefeller University Proteomics Facility. The library was divided into 8 pools of 11 peptides except peptide pool number 8, which was composed of 10 peptides, as described[16].
Intracellular cytokine staining (ICS) and surface staining
For ICS of pulmonary T cells, lungs were collected and single cell suspensions were prepared[19]. Briefly, perfusion was performed by injecting PBS containing 1 mM EDTA through the right ventricle. Lungs were harvested, dissected mechanically, and then digested enzymatically with Collagenase/DNase (Roche, Indianapolis, IN). The cells were washed, and stimulated with pools of peptides or individual reactive peptides (2 μM) or medium alone in the presence of a co-stimulatory anti-CD28 mAb (clone 37.51) for 6 hrs. Brefeldin A was added for the last 4 hrs to accumulate intracellular cytokines. Cells were then washed, incubated with anti-mouse-CD3, or CD4 mAbs for 20 min at 4°C after blocking Fcγ receptor with αCD16/CD23 antibody. Following fixation with Cytofix/Cytoperm PlusTM(BD PharMingen, San Jose, CA), cells were stained for intracellular IFN-γ, IL-2, or TNF-α for 15 min at room temperature. All mAbs were purchased from BD PharMingen. Data were collected using FACS Calibur and analyzed by FlowJo (Tree Star, Ashland, OR). In some experiments, splenocytes, mediastinal lymph nodes and airway lymphocytes were also collected and stained as described above.
ELISA for anti-LcrV antibodies
To detect LcrV specific antibody, high binding ELISA plates (BD Falcon, San Jose, CA) were coated with 5 μg/ml of LcrV protein overnight at 4°C. Plates were washed 3 times with PBST (PBS and Tween 20, 0.1 %) and blocked with PBST-BSA 5 % for 1 hr at 37°C. Serial dilutions of serum, bronchoalveolar lavage (BAL) fluid, or nasal washes were added and incubated 1 hr at 37°C. Various secondary goat anti-mouse Fc specific antibodies conjugated with horseradish peroxidase (Southern Biotech, Birmingham, AL) were then added and visualized with o-phenylenediamine (Sigma) tablets at room temperature for 15 min. The reported titers represent the highest dilution of sample showing an OD450 higher than 0.1, and the data was presented as the log antibody titer.
Y. pestis challenge and protection assay
Protection assays were performed at the Public Health Research Institute (PHRI, Newark, NJ). Each group of mice (n=10 per group) was inoculated i.n. with up to 25 μl to 105 colony forming units or ~ 100LD50 of CO92 strain of Y. pestis and the mice were observed daily for 14 days.
Statistics
Survival data were analyzed by log-rank tests. Differences in immunological responses were compared for significance using paired and unpaired Student’s t-test as appropriate.
RESULTS
Pulmonary immune responses are induced by a DEC-205+ DCs-targeted LcrV protein
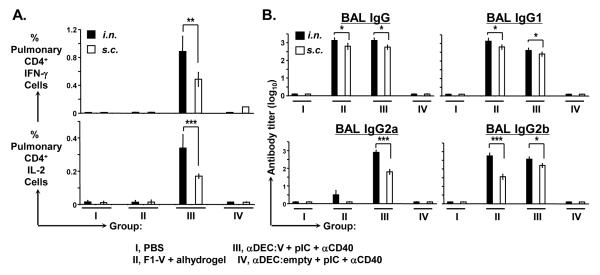
To investigate the ability of a DC-targeting approach to generate immunity at mucosal surfaces, mice were immunized by the intranasal (i.n.) route with αDEC:LcrV in the presence of adjuvants such as TLR3 ligand poly IC and agonistic αCD40. F1-V recombinant protein in alhydrogel was used as a reference[4-7]. Anti-DEC:empty, which does not carry any antigen and PBS were included as negative controls. Ten days after immunization, lungs were collected and antigen-specific pulmonary IFN-γ or IL-2 secreting CD4+ T cells were determined by intracellular cytokine staining (ICS) (Fig. 1A, see filled bars). The data showed that the i.n. route of immunization with αDEC:LcrV induced LcrV-specific IFN-γ/IL-2 secreting pulmonary CD4+ T cells. Next, subcutaneous (s.c.) immunizations were carried out to test whether parenteral vaccination induces mucosal response in addition to systemic immunity. Upon s.c. immunization, antigen-specific T cell responses were induced in the lungs in the group receiving αDEC:LcrV although the response was lower when compared to those immunized by the intranasal route (Fig.1A, see open bars). Importantly, we could not detect such T cell responses in the group immunized with F1-V recombinant protein by either routes, demonstrating the benefit of targeting DC.
Figure 1.
Immune responses at mucosal surfaces after αDEC:LcrV immunization in the presence of poly IC and αCD40 as adjuvants. (A) BALB/c mice were immunized with PBS, F1-V (10 μg) adsorbed in alum, αDEC:LcrV (10 μg), or αDEC:empty (10 μg) in the presence of adjuvants (50 μg of poly IC and 25 μg of αCD40 mAb) either i.n. or s.c. Ten days later, lungs were collected, restimulated with the LcrV reactive peptide LKIYSVIQAEINKHL, aa164-178, and ICS was performed. The frequency of IFN-γ+ (upper) or IL-2+ (lower) secreting CD3+/CD4+ pulmonary T cells was shown as percentage. (B) Anti-LcrV antibody titers for individual IgG isotypes in BAL. Immunization and injection routes were same as described in (A). Data are mean values from 3 independent experiments with similar results, using 3 mice per group. *p<0.05; **p<0.005; ***p<0.001
Antibodies in the airway can provide immediate protection against an aerosol infection with Y. pestis[9]. The data in Fig.1B showed that a single immunization of αDEC:LcrV in the presence of adjuvants induced antigen-specific antibodies in BAL not only upon i.n., but also upon s.c. immunization. Main isotypes were IgG1, IgG2b, and IgG2a. Interestingly, IgG2a (BALB/c), an isotype often associated with Th1 polarized response was only detected in the group immunized with αDEC:LcrV (Fig.1B, see group III). As previous studies have shown[20], the F1-V subunit vaccine was efficient at inducing strong humoral immunity (Fig. 1B, see group II).
Altogether, these data show that DC targeting strategy via the mucosal route is more efficient at inducing a combined humoral and cellular immunity at mucosal sites than a parenteral approach with soluble protein.
Targeting of LcrV protein to DEC-205+ DCs along with poly IC alone induces broad pulmonary CD4+ T cell immunity
A combination of a poly IC and αCD40 as adjuvants to induce strong immunity was used in previous studies [16] as well as in figure 1. As anti-CD40 reagent may not be easily amenable for use in humans in contrast to poly IC, 50 μg poly IC alone was tested as the adjuvant at time of priming and boosting, as described by Do et al [17].
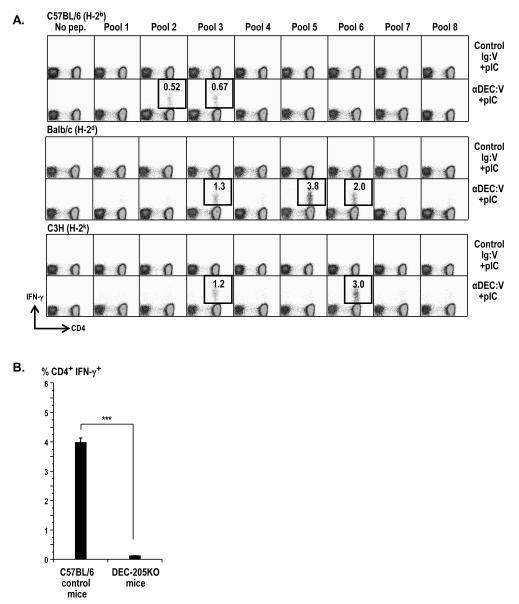
To test if this approach was effective for inducing Th1 type immunity at mucosal surfaces in different MHC haplotypes, H-2b(C57BL/6), H-2d(BALB/c), and H-2k (C3H/HeJ) mice were primed and boosted i.n. either with αDEC:LcrV or isotype control in the presence of poly IC. Measurement of antigen-specific IFN-γ production by T cells indicated that C57BL/6 and C3H/HeJ responded to at least two different peptides, while BALB/c recognized 3 pools (Fig 2A). In addition, we further checked that this was dependent on the expression of DEC-205 as DEC-205 KO mice did not mount an immune response against αDEC:LcrV(Fig. 2B).
Figure 2.
CD4+IFN-γ+ secreting pulmonary T cells following αDEC:LcrV immunization in three different strains of mice. (A) C57BL/6, BALB/c, and C3H/HeJ mice were primed and boosted i.n. with αDEC:LcrV (10 μg) or control Ig:LcrV (10 μg) in the presence of poly IC (50 μg). Six to 10 days later, lung cells were restimulated with peptide pools 1-8 and IFN-γ secreting CD4+ T cells were assessed by ICS (thick-lined boxes). This is one of several representative data sets having similar results (not shown). (B) C57BL/6 control and DEC-205−/− mice were primed and boosted with αDEC:LcrV (10 μg) in the presence of poly IC (50 μg) i.n., and 6-10 days later, lung cells were collected, restimulated, and IFN-γ secreting CD4+ T cells were assessed by ICS. Data are mean values from 2 independent experiments, using 2 mice per group. ***p<0.001
These data suggest that priming and boosting with DEC-targeted LcrV together with poly IC alone as the adjuvant induces broad pulmonary CD4+ T cell immunity.
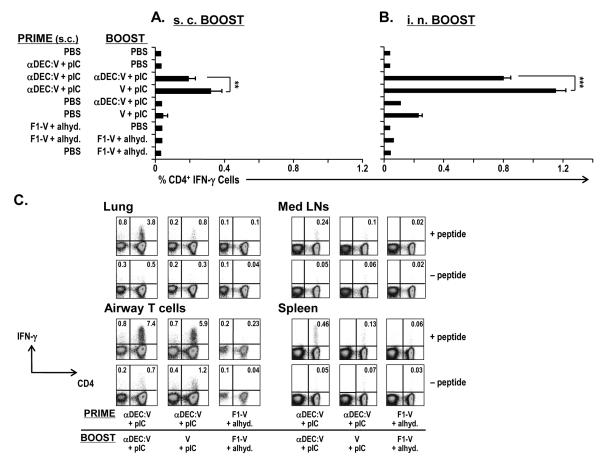
Targeting LcrV to DEC-205+ DCs in a prime/boost strategy along with poly IC induces strong mucosal CD4+ T cell immunity
In order to improve the mucosal vaccine response, different prime/boost regimens were assessed. Mice were first primed with αDEC:LcrV s.c. and boosted with either αDEC:LcrV or soluble LcrV s.c. Six to ten days later, lungs were collected and the antigen-specific IFN-γ+CD4+ T cells were measured by ICS (Fig. 3A). The s.c. prime-boost strategy induced detectable LcrV-specific pulmonary IFN-γ secreting CD4+ T cells, while both a single dose of immunization or prime-boost with F1-V plus alhydrogel did not (Fig. 3A).
Figure 3.
Cellular immunity at mucosal surfaces after αDEC:LcrV immunization in the presence of poly IC alone as an adjuvant in a prime/boost strategy. BALB/c mice were s.c. priming, and the mice were boosted either s.c. (A) or i.n. (B) as described at the left with antigen and adjuvants. Six to 10 days after the boost, lungs were collected, restimulated, and ICS was performed. The frequency of IFN-γ secreting CD3+/CD4+ pulmonary T cells are shown as percentages. The doses of LcrV protein were either 100 μg in case of s.c. (A) or 25 μg in case of i.n. (B) route of boost. Data are mean values from 3 independent experiments with similar results. (C) BALB/c mice were primed and boosted both by the i.n. route, as described at the bottom of each graph. Six to 10 days after the boost, T cells from lungs, mediastinal lymph nodes (Med LNs), BAL fluid, or spleens were restimulated, and IFN-γ secreting CD4+ T cells were assessed by ICS. Data in (C) is one of three similar experiments (tabulated in Table 1), using 3 mice per group. **p<0.005; ***p<0.001
We next studied mice primed with αDEC:LcrV s.c. that were boosted i.n., in an attempt to improve local immune response. The i.n. boost enhanced the frequency of LcrV-specific IFN-γ+CD4+ T cells in the lung by 4-fold relative to s.c. boosting (Fig. 3A and Fig. 3B).
To characterize the IFN-γ+ CD4+ T cell responses at various sites, we primed and boosted mice i.n. as shown in Fig. 3C, and analyzed cells from lung parenchyma, airways (bronchoalveolar lavage, BAL fluid), mediastinal lymph nodes (Med LNs), as well as the spleen. The level of antigen-specific IFN-γ+CD4+ T cells was 8-fold and 16-fold higher in lung parenchyma and BAL fluid, respectively as compared to that of spleen. Boosting with αDEC:LcrV was more effective than boosting with soluble LcrV protein (Fig. 3C). In contrast, immunisation with F1-V or a single immunization with αDEC:LcrV+poly IC did not induce detectable antigen-specific IFN-γ+CD4+ T cells (Table 1). Together the data indicate that a DEC-targeted protein vaccine induces strong mucosal immunity in the lung, particularly upon local administration of the vaccine.
Table 1.
IFN-γ+CD4+ T cell responses to LcrV protein following an i. n. route of immunization.
| PRIME | BOOST | SPLEEN | LUNG | MedLN | AIRWAY T CELLs |
|---|---|---|---|---|---|
| DEC-V | DEC-V | 0.41±0.03 | 2.46±0.6 | 0.21±0.01 | 6.0±0.9 |
| DEC-V | V | 0.07±0.03 | 0.57±0.27 | 0.05±0.04 | 4.56±1.2 |
| F1-V | F1-V | 0.01±0.03 | 0±0.03 | 0±0.01 | 0±0.01 |
| DEC-V | PBS | 0.01±0.01 | 0.01±0 | 0±0 | 0±0 |
| F1-V | PBS | 0.01±0 | 0±0 | 0.01±0 | 0±0 |
| PBS | DEC-V | 0.01±0.01 | 0±0.01 | 0.02±0.01 | 0.03±0.02 |
| PBS | V | 0.01±0 | 0±0.03 | 0±0.02 | 0.79±0.7 |
| PBS | F1-V | 0.01±0 | 0±0.01 | 0±0 | 0±0 |
DEC-V, αDEC:LcrV; V, LcrV
Adjuvant used: poly IC for αDEC:LcrV and LcrV protein immunization; alhydrogel for F1-V recombinant protein
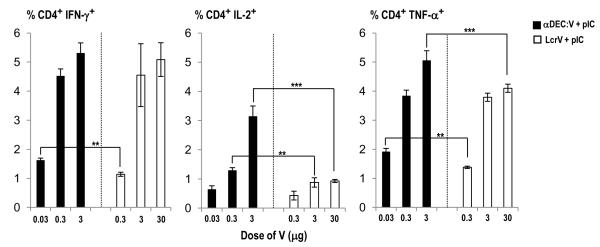
Targeting LcrV to DEC-205+ DCs more effectively induces strong mucosal immunity in comparison to non-targeted protein vaccine
To assess the value of targeted delivery of LcrV via αDEC, the responses to increased doses of αDEC:LcrV (0.1, 1, or 10 μg of the antibody per mouse is approximately equal amount of 0.03, 0.3, 3 μg of the LcrV protein per mouse, respectively) was compared to the response to soluble LcrV protein (0.3, 3, or 30 μg per mouse) in the presence of 50 μg of poly IC intranasally. Four to 6 wks later, the mice were boosted i.n. with the same doses and 6-10 days later, the lungs were harvested to detect antigen-specific IFN-γ /IL-2/TNF-α secreting CD4+ T cells (Fig. 4). At least 10-fold more soluble LcrV is required to achieve a similar T cell response than when it is fused to anti-DEC antibody. While the number of IL-2+/TNF-α+ T cells reaches a plateau when mice are immunized with 3 and 30 μg soluble LcrV, this number significantly increases in mice immunized with 0.3 and 3 μg of αDEC:LcrV. These data demonstrated the value of antigen targeting for increasing the efficiency of inducing LcrV-specific cellular immunity in the lungs. Consistent with previous finding, no IFN-γ+ IL-2+TNF-α+CD4+ T cell responses could be detected in the group primed and boosted with F1-V plus alhydrogel (data not shown).
Figure 4.
The targeting efficacy of the induction of LcrV-specific pulmonary cellular immunity. BALB/c were primed and boosted i.n. with different forms of LcrV protein of various dosages as shown at the bottom of the graphs. Six to 10 days later, lung cells were collected, restimulated, and IFN-γ or IL-2 or TNF-α secreting CD4+ T cells were assessed by ICS. Data are mean values from 2 independent experiments, using 2 mice per group. **p<0.005; ***p<0.001
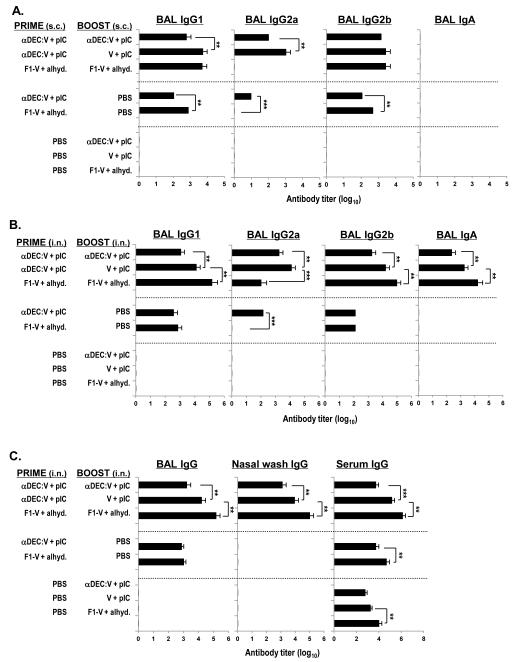
Targeting LcrV to DEC-205+ DCs primes for strong mucosal humoral immunity
To detect humoral immunity at mucosal surfaces, BAL fluid was collected and anti-LcrV antibody was measured by ELISA. A single s.c. immunization with αDEC:LcrV in the presence of poly IC induced detectable LcrV-specific antibodies in BAL fluid, but prime and boost immunization further enhanced the mucosal antibody responses about 10-fold (Fig. 5A). The titers of antibody in the BAL fluid were higher where the boost was performed with the soluble LcrV protein in comparison to the boost with αDEC:LcrV (Fig. 5A). A broad spectrum of IgG isotypes (IgG1, IgG2a, IgG2b) were detected following immunization with αDEC:LcrV, but IgG2a was not found in the BAL fluid from mice immunized with F1-V (Fig. 5A).
Figure 5.
Humoral immunity at mucosal surfaces, the lung, following αDEC:LcrV immunization. (A) BALB/c mice were primed and boosted s.c. as shown at the left side of the graphs. Six to 10 days after the boost, anti-LcrV antibody titers for individual IgG isotypes and IgA in BAL fluid were determined by ELISA. Data are mean values from one of three similar experiments. (B-C) BALB/c mice were primed and boosted i.n. as described at the left. Six to 10 days after the boost, anti-LcrV antibody titers for individual IgG isotypes and IgA were measured in BAL fluid (B) (C), and in nasal washes and serum (C) by ELISA. Data shown are mean values from three similar experiments, using 3 mice per group. *p<0.05; **p<0.005; ***p<0.001
Next, the humoral immune responses were examined in BAL fluid following an i.n. administration with αDEC:LcrV. The i.n. route increased the BAL antibody titres about 10-30 fold relative to the s.c. route (compare Fig. 5A and 5B), and the titers of anti-LcrV antibody were again higher in the group primed with αDEC:LcrV and then boosted with soluble LcrV protein in comparison to boosting with a DEC-targeted protein (Fig. 5B). Although we could not detect strong IFN-γ responses in the lung following i.n. immunization with F1-V plus alhydrogel, humoral immunity in BAL fluid was observed as shown in Fig. 5A and 5B. The isotypes of antibody were examined and IgG1 and 2b were consistently predominant while IgG2a isotype was the strongest in the DEC-targeted group. Interestingly, IgA responses were detected in BAL fluid following i.n. immunization (Fig. 5B) but not with s.c. immunization (Fig. 5A). This suggests that local immunization is required to promote mucosal-specific antibodies such as IgA.
We also determined anti-LcrV antibody in the upper respiratory tract by collecting and testing nasal washes by ELISA and observed IgG anti-LcrV antibody in DEC-targeted as well as F1-V immunized groups (Fig. 5C). IgA responses in nasal washes were detectable only in F1-V plus alhydrogel immunized mice (data not shown). When serum IgG responses were measured following i.n. immunization, the titers of anti-LcrV from the group primed with αDEC:LcrV and then boosted with soluble LcrV protein were again higher than those boosted with αDEC:LcrV. The highest antibody titers were detected in the F1-V plus alhydrogel immunized group (Fig. 5C). Taken together, these data showed that a DEC-targeted protein vaccine along with poly IC as adjuvant induces efficient humoral immunity at mucosal surfaces.
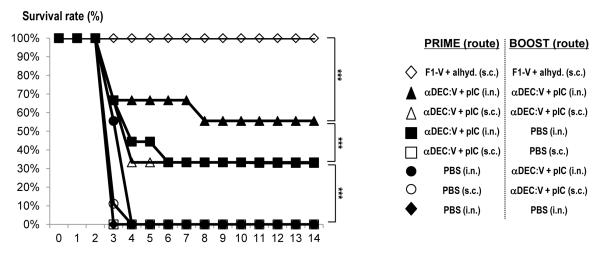
Targeting LcrV to DEC-205+ DCs via an intranasal route protected mice better than the targeting via a subcutaneous route against pneumonic plague
In order to study the efficacy of a mucosal DEC-targeted protein adjuvanted vaccine to protect from pulmonary plague, mice were primed and boosted with αDEC:LcrV plus poly IC either via an intranasal route or a subcutaneous route. Subcutaneously immunization with F1-V was included as a positive control. Six weeks after the boost, mice were challenged with 100 LD50 of virulent Y. pestis CO92 strain i.n. and their survival was carefully monitored for 14 days. As expected, immunization with F1-V conferred 100% protection while all mice immunized with saline did not survive the challenge (Fig. 6). Interestingly, an intranasal route of αDEC:LcrV with poly IC protected 56% of the mice while a subcutaneous route only protected 33% of the mice (Fig. 6A filled vs. unfilled triangle). Moreover, a single intranasal priming with αDEC:LcrV with adjuvant protected 33% while a single subcutaneous showed no impact on survival rate (Fig.6 filled vs. unfilled square). Although these data indicate that targeting DEC as a new approach does not confer better protection than the reference F1-V vaccine in these conditions, the data unequivocally showed that an intranasal route of immunization confers a protective advantage over parenteral immunization.
Figure 6.
Survival rates after challenge with 100 LD50 of CO92 Y. pestis. BALB/c mice (10/group) primed and boosted i.n. or s.c. as described at the right with antigen and adjuvants. Six weeks after the boost, CO92 Y. pestis was given i.n. and the survival of the mice monitored daily for 14 days. ***p<0.001
DISCUSSION
There have been substantial concerns and efforts to develop an efficient pneumonic plague vaccine not only due to its deadly contagiousness and lethality but also because of a high risk of aerosol dispersal of Y. pestis during a bioterror attack[21, 22]. The F1-V subunit vaccine provides protection against pneumonic plague in small animal models mainly through antibody response and most of the research on Y. pestis has focused on the induction of humoral immunity both systemically and at mucosal surfaces[20]. However, it so far fails to efficiently protect African green monkeys regardless of antibody titers suggesting that the induction of cellular immunity in addition to humoral immunity may be critical for better protection in humans[23].
In order to fulfill such requirements, we developed a novel approach based on the targeting the delivery of antigen into the most efficient cells at priming T cells, namely DC. We have previously shown a strong and broad LcrV-specific IFN-γ secreting CD4+ T cell immunity as well as humoral immunity including Th1-dependent antibody isotypes induced by αDEC:LcrV following parenteral administration[16]. In the setting of distinct DC subsets targeting, mice were protected against pulmonary fully virulent CO92 Y. pestis strain infection[17].
The present study further extends the value of using the DEC-205+ DC targeting strategy as a novel mucosal vaccine against pneumonic plague. When compared to a subcutaneous route of immunization, an intranasal route of DEC-targeted delivery increases the efficiency of Th1 cellular immunity as well as antibody responses at mucosal surfaces. A similar breadth of the response was also achieved as compared to parenteral delivery. The use of poly IC which signals via TLR3 receptor and MDA5, is likely to be key in stimulating local immunity as recently reported by Bei et al [24]. Our interests in poly IC as an adjuvant (in the absence of anti-CD40) were based on previous studies showing a good safety record in cancer patients and better potency as an adjuvant for responses to protein antigen in rhesus macaques when compared to other agonists [25, 26].
Different combinations of route in the prime/boost strategy were tested to compare the efficacy of mucosal immunity induced by a DEC-targeted LcrV protein. Prime and boost by a s.c. route of αDEC:LcrV is able to induce cellular and humoral immunity at mucosal surfaces (Fig. 3A and 5A). A prime by a s.c. route and then a boost by an i.n. route increase the frequency of IFN-γ secreting mucosal T cells (Fig. 3B). One explanation for this finding would be that an intranasal boost mimics a natural aerosol exposure to Yersinia and that therefore, a mucosal route for a boost is preferable. Prime and boost via the i.n. route might still be the optimal strategy for a vaccine as it induced the strongest antigen-specific cellular and humoral immunity at mucosal surfaces (Fig. 3C, 5B and C). Previous studies showed that a majority of activated T cells migrate into nonlymphoid tissues such as lung, liver, and kidney and we show here that a mucosal priming may be advantageous to support local immunity[27, 28]. Although the exact effector mechanisms of such protection are unclear, enhanced antigen presentation by pulmonary DCs to resident and /or recruited memory and naïve T cells might be important [28]. In addition, inflammatory chemokines from effector T cells are vital for the early recruitment of other immune cells including immature DCs and natural killer cells[27]. Interestingly, the data show that even a single parenteral immunization of DEC-targeted protein primes the immune system sufficiently to efficiently recall and activate antigen-specific T cells at mucosal surfaces. This is advantageous considering the hurdles of developing mucosal vaccines based on intranasal delivery. However, considering our current data, it may be beneficial to develop a mucosal delivery approach, using the DEC-targeted protein vaccine for example, to enhance T and B cell immunity at mucosal surfaces.
The data of survival rate using a virulent CO92 strain as pneumonic form of plague with high dose or 100LD50 also supported the benefit of the mucosal delivery of a DEC-targeted protein vaccine (Fig. 6). This data suggest potential roles of enhanced mucosal T and B cell immunity induced by the mucosal delivery of a DEC-targeted protein vaccine when compared to a subcutaneous delivery group since serum antibody titers following vaccination were similar between these two groups (data not shown). A further study should be focused on demonstrating a more direct involvement of mucosal T and B cell immunity against pneumonic plague. Although high serum antibody titers as much as a subcutaneous administration of F1-V with alhydrogel induces are necessary for providing 100% protection in a mouse model as previously known[17, 18, 20, 29], the value of the enhanced mucosal T cell immunity induced by a DEC-targeted vaccine might be appreciated better in nonhuman primates[23].
Another value of the DEC-205+ DC targeting strategy is that broader and stronger antigen-specific T cell responses are induced with lower amounts of antigen in comparison to standard non-targeted soluble protein vaccine (Fig.2A and 4). Additionally, the data suggest that poly IC, a clinically feasible adjuvant, is an effective mucosal adjuvant for a DEC-205+ DC targeted vaccine. While other adjuvants could be potentially tested, use of lipopolysaccharide from Escherichia coli 055:B5 as adjuvant offered a weaker activity relative to poly IC, with LPS being at least 10-fold less active in inducing Th1 immunity (data not shown). Another frequently used adjuvant, the TLR5 agonist flagellin, did not induce pulmonary cellular immunity, either with a DEC-targeted vaccine or F1-V protein vaccine treatments (data not shown). This is in agreement with other studies of flagellin showing a Th2 biased response to similar antigens [8]. Therefore, a DEC-targeted vaccine strategy with poly IC as adjuvant has potential to be utilized in future clinical applications with proven safety as well as antigen sparingness.
Taken together, this is the first study to demonstrate the efficacy of a DC-targeting strategy in the induction of combined pulmonary cellular and humoral immunity, which will be further developed as an efficient pneumonic plague vaccine for use in humans.
HIGHLIGHTS.
Y. pestis LcrV protein is targeted to dendritic cells via DEC-205 receptor.
Mucosal immunity is induced by the vaccine through both s.c. and i.n. routes.
Poly IC is an efficient mucosal adjuvant in the DEC-205 targeting strategy.
Efficacy of the targeting vaccine is demonstrated in mucosal T and B cell immunity.
ACKNOWLEDGEMENTS
We thank H. Zebroski of the Rockefeller University Proteomics Facility for synthesizing peptides, and J. Adams for help with the graphics. This work was supported by funds from the National Institutes of Health (#5 U54 AI057158-PI-Lipkin and AI13013, PI, RMS, and 1 R21 AI082331-01, PI, Y. Do). This study was also supported by Basic Science Research Program through the National Research Foundation of Korea(NRF) funded by the Ministry of Education, Science and Technology (2012-0003632), and a grant from the National R&D Program for Cancer Control, Ministry for Health and Welfare, Republic of Korea (1020120). A. Didilerlaurent was supported by a symposium bursary awarded by the Novartis Foundation. The opinions, interpretations, conclusions, and recommendations are those of the authors and are not necessarily endorsed by the U. S. Army.
Abbreviations
- Y. pestis
Yersinia pestis
- ICS
intracellular cytokine staining
- poly IC (pIC)
Polyinosinic:polycytidylic acid
Footnotes
Dr. Ralph M. Steinman died on 30 Sep. 2011.
CONFLICT OF INTEREST STATEMENT R. M. Steinman had been a consultant to Celldex, which is developing human DEC-205-based vaccines. Other authors have no commercial or financial conflict of interest.
AUTHOR CONTRIBUTIONS Conceived and designed the experiment: YD DA RMS. Performed the experiments: YD DA HK. Protection assay: SP DP. Analyzed the data: YD SR. Contributed reagents/materials/analysis tools: CGP BSP SR. Wrote the paper: YD DA RMS.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- [1].Lathem WW, Crosby SD, Miller VL, Goldman WE. Progression of primary pneumonic plague: a mouse model of infection, pathology, and bacterial transcriptional activity. Proc Natl Acad Sci U S A. 2005 Dec 6;102(49):17786–91. doi: 10.1073/pnas.0506840102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Bubeck SS, Cantwell AM, Dube PH. Delayed inflammatory response to primary pneumonic plague occurs in both outbred and inbred mice. Infect Immun. 2007 Feb;75(2):697–705. doi: 10.1128/IAI.00403-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Reed DS, Martinez MJ. Respiratory immunity is an important component of protection elicited by subunit vaccination against pneumonic plague. Vaccine. 2006 Mar 20;24(13):2283–9. doi: 10.1016/j.vaccine.2005.11.047. [DOI] [PubMed] [Google Scholar]
- [4].Eyles JE, Williamson ED, Spiers ID, Alpar HO. Protection studies following bronchopulmonary and intramuscular immunisation with yersinia pestis F1 and V subunit vaccines coencapsulated in biodegradable microspheres: a comparison of efficacy. Vaccine. 2000 Aug 1;18(28):3266–71. doi: 10.1016/s0264-410x(00)00128-6. [DOI] [PubMed] [Google Scholar]
- [5].Baca-Estrada ME, Foldvari MM, Snider MM, Harding KK, Kournikakis BB, Babiuk LA, et al. Intranasal immunization with liposome-formulated Yersinia pestis vaccine enhances mucosal immune responses. Vaccine. 2000 Apr 28;18(21):2203–11. doi: 10.1016/s0264-410x(00)00019-0. [DOI] [PubMed] [Google Scholar]
- [6].Eyles JE, Sharp GJ, Williamson ED, Spiers ID, Alpar HO. Intra nasal administration of poly-lactic acid microsphere co-encapsulated Yersinia pestis subunits confers protection from pneumonic plague in the mouse. Vaccine. 1998 Apr;16(7):698–707. doi: 10.1016/s0264-410x(97)00249-1. [DOI] [PubMed] [Google Scholar]
- [7].Jones T, Adamovicz JJ, Cyr SL, Bolt CR, Bellerose N, Pitt LM, et al. Intranasal Protollin/F1-V vaccine elicits respiratory and serum antibody responses and protects mice against lethal aerosolized plague infection. Vaccine. 2006 Mar 6;24(10):1625–32. doi: 10.1016/j.vaccine.2005.09.052. [DOI] [PubMed] [Google Scholar]
- [8].Honko AN, Sriranganathan N, Lees CJ, Mizel SB. Flagellin is an effective adjuvant for immunization against lethal respiratory challenge with Yersinia pestis. Infect Immun. 2006 Feb;74(2):1113–20. doi: 10.1128/IAI.74.2.1113-1120.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Hill J, Eyles JE, Elvin SJ, Healey GD, Lukaszewski RA, Titball RW. Administration of antibody to the lung protects mice against pneumonic plague. Infect Immun. 2006 May;74(5):3068–70. doi: 10.1128/IAI.74.5.3068-3070.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Nakajima R, Brubaker RR. Association between virulence of Yersinia pestis and suppression of gamma interferon and tumor necrosis factor alpha. Infect Immun. 1993 Jan;61(1):23–31. doi: 10.1128/iai.61.1.23-31.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Elvin SJ, Williamson ED. Stat 4 but not Stat 6 mediated immune mechanisms are essential in protection against plague. Microb Pathog. 2004 Oct;37(4):177–84. doi: 10.1016/j.micpath.2004.06.009. [DOI] [PubMed] [Google Scholar]
- [12].Parent MA, Berggren KN, Kummer LW, Wilhelm LB, Szaba FM, Mullarky IK, et al. Cell-mediated protection against pulmonary Yersinia pestis infection. Infect Immun. 2005 Nov;73(11):7304–10. doi: 10.1128/IAI.73.11.7304-7310.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Parent MA, Wilhelm LB, Kummer LW, Szaba FM, Mullarky IK, Smiley ST. Gamma interferon, tumor necrosis factor alpha, and nitric oxide synthase 2, key elements of cellular immunity, perform critical protective functions during humoral defense against lethal pulmonary Yersinia pestis infection. Infect Immun. 2006 Jun;74(6):3381–6. doi: 10.1128/IAI.00185-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Lin JS, Park S, Adamovicz JJ, Hill J, Bliska JB, Cote CK, et al. TNFalpha and IFNgamma contribute to F1/LcrV-targeted immune defense in mouse models of fully virulent pneumonic plague. Vaccine. 2010 Dec 16;29(2):357–62. doi: 10.1016/j.vaccine.2010.08.099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Lin JS, Kummer LW, Szaba FM, Smiley ST. IL-17 contributes to cell-mediated defense against pulmonary Yersinia pestis infection. J Immunol. 2011 Feb 1;186(3):1675–84. doi: 10.4049/jimmunol.1003303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Do Y, Park CG, Kang YS, Park SH, Lynch RM, Lee H, et al. Broad T cell immunity to the LcrV virulence protein is induced by targeted delivery to DEC-205/CD205-positive mouse dendritic cells. Eur J Immunol. 2008 Jan;38(1):20–9. doi: 10.1002/eji.200737799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Do Y, Koh H, Park CG, Dudziak D, Seo P, Mehandru S, et al. Targeting of LcrV virulence protein from Yersinia pestis to dendritic cells protects mice against pneumonic plague. Eur J Immunol. 2010 Oct;40(10):2791–6. doi: 10.1002/eji.201040511. [DOI] [PubMed] [Google Scholar]
- [18].Powell BS, Andrews GP, Enama JT, Jendrek S, Bolt C, Worsham P, et al. Design and testing for a nontagged F1-V fusion protein as vaccine antigen against bubonic and pneumonic plague. Biotechnol Prog. 2005 Sep-Oct;21(5):1490–510. doi: 10.1021/bp050098r. [DOI] [PubMed] [Google Scholar]
- [19].Didierlaurent A, Goulding J, Patel S, Snelgrove R, Low L, Bebien M, et al. Sustained desensitization to bacterial Toll-like receptor ligands after resolution of respiratory influenza infection. J Exp Med. 2008 Feb 18;205(2):323–9. doi: 10.1084/jem.20070891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Heath DG, Anderson GW, Jr., Mauro JM, Welkos SL, Andrews GP, Adamovicz J, et al. Protection against experimental bubonic and pneumonic plague by a recombinant capsular F1-V antigen fusion protein vaccine. Vaccine. 1998 Jul;16(11-12):1131–7. doi: 10.1016/s0264-410x(98)80110-2. [DOI] [PubMed] [Google Scholar]
- [21].Perry RD, Fetherston JD. Yersinia pestis--etiologic agent of plague. Clin Microbiol Rev. 1997 Jan;10(1):35–66. doi: 10.1128/cmr.10.1.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Inglesby TV, Dennis DT, Henderson DA, Bartlett JG, Ascher MS, Eitzen E, et al. Plague as a biological weapon: medical and public health management. Working Group on Civilian Biodefense. Jama. 2000 May 3;283(17):2281–90. doi: 10.1001/jama.283.17.2281. [DOI] [PubMed] [Google Scholar]
- [23].Pitt ML. Animal Models and Correlates of Protection for Plague Vaccines Workshop. Gaithersburg, MD: Oct 13 to 14, 2004. http://wwwfdagov/cber/minutes/workshop-minhtm. [Google Scholar]
- [24].Wang B, Zaidi N, He LZ, Zhang L, Kuroiwa JM, Keler T, et al. Targeting of the non-mutated tumor antigen HER2/neu to mature dendritic cells induces an integrated immune response that protects against breast cancer in mice. Breast Cancer Res. 2012 Mar 7;14(2):R39. doi: 10.1186/bcr3135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Robinson RA, DeVita VT, Levy HB, Baron S, Hubbard SP, Levine AS. A phase I-II trial of multiple-dose polyriboinosic-polyribocytidylic acid in patieonts with leukemia or solid tumors. J Natl Cancer Inst. 1976 Sep;57(3):599–602. doi: 10.1093/jnci/57.3.599. [DOI] [PubMed] [Google Scholar]
- [26].Stahl-Hennig C, Eisenblatter M, Jasny E, Rzehak T, Tenner-Racz K, Trumpfheller C, et al. Synthetic double-stranded RNAs are adjuvants for the induction of T helper 1 and humoral immune responses to human papillomavirus in rhesus macaques. PLoS Pathog. 2009 Apr;5(4):e1000373. doi: 10.1371/journal.ppat.1000373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Lefrancois L, Puddington L. Intestinal and pulmonary mucosal T cells: local heroes fight to maintain the status quo. Annu Rev Immunol. 2006;24:681–704. doi: 10.1146/annurev.immunol.24.021605.090650. [DOI] [PubMed] [Google Scholar]
- [28].Harris NL, Watt V, Ronchese F, Le Gros G. Differential T cell function and fate in lymph node and nonlymphoid tissues. J Exp Med. 2002 Feb 4;195(3):317–26. doi: 10.1084/jem.20011558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Williamson ED, Vesey PM, Gillhespy KJ, Eley SM, Green M, Titball RW. An IgG1 titre to the F1 and V antigens correlates with protection against plague in the mouse model. Clin Exp Immunol. 1999 Apr;116(1):107–14. doi: 10.1046/j.1365-2249.1999.00859.x. [DOI] [PMC free article] [PubMed] [Google Scholar]